Back to Journals » Patient Preference and Adherence » Volume 15
Disparities in Unmet Needs in Indigenous and Non-Indigenous Australians with Cirrhosis: An Exploratory Study
Authors Bernardes CM , Clark PJ, Brown C, Stuart K, Pratt G, Toombs M, Hartel G , Powell EE, Valery PC
Received 4 October 2021
Accepted for publication 9 November 2021
Published 24 November 2021 Volume 2021:15 Pages 2649—2658
DOI https://doi.org/10.2147/PPA.S341566
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Christina M Bernardes,1 Paul J Clark,2 Cath Brown,1 Katherine Stuart,3 Gregory Pratt,1 Maree Toombs,4 Gunter Hartel,1 Elizabeth E Powell,3,5,* Patricia C Valery1,*
1QIMR Berghofer Medical Research Institute, Herston, QLD, Australia; 2Department of Gastroenterology and Hepatology, Mater Hospitals, Brisbane, QLD, Australia; 3Department of Gastroenterology and Hepatology, Princess Alexandra Hospital, Brisbane, QLD, Australia; 4Rural Clinical School, Faculty of Medicine, University of Queensland, Toowoomba, QLD, Australia; 5Centre for Liver Disease Research, Translational Research Institute, Faculty of Medicine, The University of Queensland, Brisbane, QLD, Australia
*These authors contributed equally to this work
Correspondence: Patricia C Valery Tel +61 07 3362 0376
Email [email protected]
Purpose: Understanding and responding to the supportive care needs of people with cirrhosis is essential to quality care. Indigenous Australians, Aboriginal and Torres Strait Islander people, are overrepresented amongst patients with cirrhosis. This study documented the nature and extent of supportive care needs of Indigenous Australians with cirrhosis, in comparison with non-Indigenous Australians.
Patients and Methods: The supportive care needs of adult patients diagnosed with cirrhosis attending public hospitals in Queensland were assessed through the Supportive Needs Assessment tool for Cirrhosis (SNAC). Patients indicated how much additional help they needed on four subscales: 1. psychosocial issues; 2. practical and physical needs; 3. information needs; and 4. lifestyle changes. We examined the rate of moderate-to-high unmet needs based on Indigenous status (Poisson regression; incidence rate ratio (IRR)).
Results: Indigenous (n=20) and non-Indigenous (n=438) patients included in the study had similar sociodemographic and clinical characteristics except for a lower educational level among Indigenous patients (p< 0.01). Most Indigenous patients (85.0%) reported having moderate-to-high unmet needs with at least one item in the SNAC tool. Following adjustment for key sociodemographic and clinical factors, Indigenous patients had a greater rate of moderate-to-high unmet needs overall (IRR=1.5, 95% CI 1.31– 1.72; p< 0.001), and specifically for psychosocial issues (IRR=1.7, 95% CI 1.39– 2.15; p< 0.001), and practical and physical needs subscales (IRR=1.5, 95% CI 1.22– 1.83; p< 0.001), compared to non-Indigenous patients.
Conclusion: Indigenous Australians with cirrhosis more frequently had moderate-to-high unmet supportive care needs than non-Indigenous patients. Specific targeting of culturally appropriate supportive care for psychosocial, practical and physical needs may optimize cirrhosis care and improve the quality of life for Indigenous Australians with cirrhosis.
Keywords: chronic liver disease, patient reported outcomes, perceived needs, unmet needs, Indigenous Australians
Introduction
Cirrhosis, an advanced stage of chronic liver disease, is an increasing cause of morbidity and mortality worldwide.1 Cirrhosis is a dynamic process, which is often asymptomatic in the early stages of disease progression until clinical decompensation occurs, including events of ascites, sepsis, variceal bleeding, hepatic encephalopathy and non-obstructive jaundice.1
In Australia, chronic liver disease affects more than 6 million people and the prevalence is expected to increase to more than 8 million in 2030.2 With cirrhosis, both physical functioning and mental health well-being may be affected, and quality of life is often compromised even in uncomplicated cases.3,4
Aboriginal and Torres Strait Islander people (hereafter respectfully referred to collectively as Indigenous Australians) experience a higher burden of disease with almost every major cause of mortality and morbidity over-represented amongst the most disadvantaged, and are less likely to access health care.5–7 Indigenous Australians diagnosed with cirrhosis have increased hospital readmissions for cirrhosis (1.35 times) and lower overall survival (17% vs 27%; unadjusted hazard ratio (HR) = 1.16 95% CI 1.06–1.27) compared to non-Indigenous Australians.8 Indigenous Australians with cirrhosis are also younger (<50 years) than non-Indigenous Australians with cirrhosis, live in some of the most economically disadvantaged areas and present more frequently with decompensation events, such as ascites.8 Living with cirrhosis at a younger age has been found to be associated with a greater decline in quality of life than living with cirrhosis at an older age.4 However, little is currently known about the supportive care needs of Indigenous Australians with cirrhosis.
The complexity of the clinical management associated with the functional impact of cirrhosis on activities of daily living and quality of life may result in patients with unmet practical and psychological needs.9–11 The assessment and management of supportive care needs is an essential component of quality care for people diagnosed with cirrhosis.11,12 Assessment provides a direct measure of the patient’s perception of need for help, as well as the magnitude of their desire for help with those needs, which may be influenced by cultural factors and service delivery factors (eg organization and delivery of services). Cross-cultural and international comparisons of unmet supportive care needs have shown that different populations tend to prioritize needs belonging to different domains (eg Japanese cancer patients reported higher needs in psychological and health system information domains, while Taiwanese and Hong Kong patients reported higher needs in health systems information and Patient Care and support).13
Understanding the specific needs of Indigenous Australians with cirrhosis will facilitate improvements to the quality and appropriateness of supportive care provided to this population. Extending our previous research into supportive care needs of patients with cirrhosis, here we document the type and level of supportive care needs of Indigenous Australians with cirrhosis, and compare the data with that of non-Indigenous Australians.
Materials and Methods
Setting and Patients
In this study, we included Indigenous and non-Indigenous Australians with cirrhosis who participated in the previously described CirCare study.12 Briefly, consecutive adult patients diagnosed with cirrhosis attending a liver specialist clinic or admitted to one of five hospitals in Brisbane and Logan, Queensland between the period of June 2016 to December 2018 were eligible to be involved in the study. Patients’ eligibility was assessed by a study nurse and the treating clinician. Patients who were unable to communicate in English and those with cognitive or physical impairment that could interfere with the ability to make an informed choice to be involved in the study were excluded. Patients were invited to take part in the study while waiting for their appointment with the liver specialist or while they were admitted to hospital.
Data Collection and Measures
Patient interviews were conducted face-to-face at recruitment in the clinic. Sociodemographic data was self-reported at recruitment, and clinical data was obtained from the patients’ medical records by clinicians. Place of residence was categorised according to Rurality of Residence and the Index of Relative Socioeconomic Advantage and Disadvantage (IRSAD).14
The Supportive Needs Assessment tool for Cirrhosis (SNAC)12 was used to assess needs. Exploratory factor analysis of the tool identified 4 factors (39 items considered to be clinically relevant items by the expert multidisciplinary panel) that accounted for 49.2% of the total variance. The 39-item SNAC met the requirements of a needs assessment tool and identified a range of needs important to patients with cirrhosis. Moreover, differences in SNAC total scores according to disease stage and patient’s age supported known group validity. The tool has four subscales, namely: 1. Psychosocial issues; 2. Practical and physical needs; 3. Information needs; and 4. Lifestyle changes. Cronbach’s alpha values for the four subscales ranged from 0.64 to 0.92. This tool asks patients to rate their need for help with each item over the past month. Responses to each item are broken down to a “yes/no” initial response to the opening question (“In the past month, did you … ”), followed by 4 possible answers (“None”, “A little”, “Some”, and “A lot”) to the subsequent question (“How much additional help did/do you need?”). The SNAC response categories to the opening question and the subsequent question were banded together and re-scored using a 5-point response scale in which 0 indicates no issue with that item, no need for help; 1 indicates an issue with that item and “no” help required; 2 indicates an issue with that item and “A little” help required; 3 indicates an issue with that item and “Some” help required; and 4 indicates an issue with that item and “A lot” of help required. The mean score for each subscale and the overall SNAC mean score (average of the four subscales) can range from 0 (indicating no issue with all items in the SNAC tool) to a potentially maximum value of 4, with higher values indicating higher levels of unmet needs.
Cirrhosis severity was assessed by the Child-Pugh class around the time of recruitment and by absence (“compensated” cirrhosis) versus presence (“decompensated”) of cirrhosis complications (eg ascites, hepatic encephalopathy, gastroesophageal variceal bleeding and jaundice). The prevalence of coexistent conditions present around the time of recruitment was assessed as a measure of comorbidity burden.
Data Collection and Measures
Analyses were conducted using Stata/SE (Version 15; Stata Corporation, College Station, TX). Descriptive analyses are presented as frequency (percentages, %), mean (standard deviation, SD) or median (interquartile range, IQR) value depending on data distribution. The chi-square test was used to compare categorical variables (Fisher's exact test was used for sparse tables), Student’s t-test to compare continuous variables normally distributed and Wilcoxon rank-sum test for not normally distributed data. Linear regression analysis (bi-variable) was performed to study the influence of each independent variable on the level of needs (summary scales of the overall SNAC score and the scores for each subscale). As in the previous study, marital status and live alone were combined and categorised as “Have a partner, do not live alone”, “No partner, do not live alone”, “No partner, live alone”.
In multiple regression analysis, the need scores were used as dependent variables, and independent variables included demographic and clinical factors. The final multivariable model included Indigenous status as well as Child-Pugh class, age group, recruitment hospital, combined variable marital/live alone, place of residence, diabetes, and primary diagnosis. The final model (reported in the previous study)12 was determined based on the results of the bi-variable analysis, taking into account our understanding of the relationships and dependencies among variables as well as their clinical relevance. The variance inflation factors (VIFs) for the independent variables included in the model were <2 indicating that the variables are not highly collinear. Multivariable linear regression analysis reported in terms of coefficients with associated 95% confidence intervals (CIs) was used to assess the differences in SNAC scores by independent factors.
Perceived supportive needs for each item were grouped as “moderate-to-high” if patients reported that they needed “Some” or “A lot” of additional help with that item. The rates of moderate-to-high unmet need items were calculated using the total number of items in each subscale or overall as denominator. Using Poisson regression, we compared the rate of moderate-to-high unmet need items by Indigenous status; incidence rate ratios (IRR) and 95% CI were reported. Using multivariable logistic regression, we measure the association between the categorical dependent variable “having at least one moderate-to-high unmet need item” and Indigenous status. Statistical significance was set at alpha = 0.05, and all p-values were 2-sided.
Results
Participants Characteristics
A total of 746 patients were invited to participate in the study (581 completed the survey and 165 declined to participate in the study; 78% response). Completers (n=581) and non-consenters (n=165) were similar in key demographic charateristics, such as age (p=0.10), gender (p=0.73) and whether patients were an inpatient or outpatient (p=0.20) at the time they were invited to take part in the study. SNAC data was available for 465 patients12 recruited in the CirCare study. After excluding seven patients with chronic liver disease who did not have cirrhosis, 458 patients were included in this analysis (20 Indigenous and 438 non-Indigenous). The characteristics of the study sample are shown in Table 1. Indigenous and non-Indigenous patients had, in general, similar sociodemographic and clinical characteristics. The majority of patients in both groups were male, had no partner, were unemployed at the time of recruitment, and lived in a major city area. The average age of Indigenous and non-Indigenous patients were similar (58 +12.52 years, vs 59 +10.91 years, respectively). A higher proportion of non-Indigenous compared to Indigenous patients had higher education level (Senior high school or more; 58.5% vs 26.3%; p<0.01). Other relevant sociodemographic variables of note that did not meet statistical criteria for significance were socioeconomic disadvantage (50.0% for Indigenous vs 33.0% for non-Indigenous patients; p=0.15) and place of residence, with the latter reflecting the recruitment sites for the CirCare study, namely hospitals located in major city areas.
 |
Table 1 Patient’s Demographic and Clinical Characteristics at Recruitment According to Indigenous Status |
Clinically, the two most common primary causes of liver disease for both groups were alcohol-related liver disease and chronic hepatitis C. The majority of Indigenous and non-Indigenous patients had Child-Pugh class A cirrhosis at recruitment, and portal hypertension was the most common complication. The most frequent comorbidities were diabetes (55.0% of Indigenous and 41.6% of non-Indigenous patients; p=0.23) and obesity (60.0% of Indigenous and 44.3% of non-Indigenous patients; p=0.43).
Prevalence of Supportive Needs
The majority of patients (90.0% of Indigenous and 87.7% of non-Indigenous patients; p=0.999) reported needing additional help (“a little,” “some,” or “a lot”) with at least one item; and 85.0% and 81.1% respectively, had at least one moderate-to-high unmet need item (p=0.999). Overall, the rate of moderate-to-high unmet need items was 1.5 times higher for Indigenous than non-Indigenous patients (IRR=1.5, 95% CI 1.31–1.72; p<0.001) (Table 2). Following adjustment for key sociodemographic and clinical factors, Indigenous patients had 50% more moderate-to-high unmet need items (IRR=1.7, 95% CI 1.39–2.15; p<0.001) in the psychosocial issues subscale and 30% more moderate-to-high unmet need items in the practical and physical needs subscale (IRR=1.5, 95% CI 1.22–1.83; p<0.001) compared to non-Indigenous patients. The results of bi-variable analysis were similar to the aforementioned multivariable analysis (the rate of moderate-to-high unmet needs according to Indigenous status and unadjusted IRRs are provided in Supplementary Table 1).
 |
Table 2 Comparison of the Rate of Moderate-to-High Unmet Supportive Care Needs and the 20 Most Frequent Items Reported by Patients with Cirrhosis According to Indigenous Status |
When the 20 most frequent items with moderate-to-high unmet needs were ranked, practical and physical needs and psychosocial issues subscales were the most commonly reported by both groups (Table 2). However, of the 39 items in SNAC, 32 were reported as moderate-to-high unmet needs items (prevalence of 20% or higher) among the Indigenous patients, compared to only 14 items for non-Indigenous patients. Fifteen moderate-to-high unmet need items were reported in over 34% of Indigenous patients.
Half or more of Indigenous patients reported lack of energy, poor sleep and anxiety and depression. Over a third of Indigenous patients with cirrhosis reported feeling down or depressed, lonely or worried and reported difficulties with daily tasks and mobility. More than one in five Indigenous patients with cirrhosis felt they needed more information about lifestyle interventions/self-help, treatment options and assistance to access further supports or counselling. The prevalence of moderate-to-high unmet needs of all 39 items of the SNAC tool according to Indigenous status is provided in Supplementary Table 2.
The Supportive Needs Assessment Tool for Cirrhosis Scores
SNAC scores (overall and by subscale) can range between 0 and 4, with higher values indicating a higher need. Overall, SNAC sub-score for psychosocial needs were higher for Indigenous patients with a two-fold higher median score than that of non-Indigenous patients (median=1.5, IQR 0.7–2.3 vs median=0.6, IQR 0.2–1.4, respectively; p=0.018). While the overall SNAC score was 50% higher for Indigenous relative to non-Indigenous patients (median=1.2, IQR 0.7–1.6 vs 0.8, IQR 0.4–1.4; p=0.072), this did not meet statistical significance (Figure1).
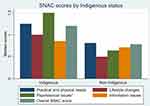 |
Figure 1 Median SNAC scores according to Indigenous status. Note: *p-value <0.005 (Wilcoxon rank-sum test). |
In multivariate regression analysis after adjustment for age, recruiting hospital, marital/live alone status, place of residence, diabetes, Child-Pugh class, and primary liver disease aetiology (as per main analysis previously reported),15 As reflected by a positive β value, being Indigenous was associated with higher levels of unmet needs in the psychosocial issues subscale (a positive β value denotes an increase in SNAC score for Indigenous vs non-Indigenous patients). The SNAC score for psychosocial issues was increased by 0.44 for Indigenous patients (β=0.44, 95% CI 0.03–86; p=0.036) compared to non-Indigenous patients. SNAC scores for practical and physical needs (β=0.32, 95% CI −0.02–0.66; p=0.063), lifestyle changes (β=0.15, 95% CI −0.36–0.66; p=0.565), information needs (β=−0.02, 95% CI −0.43–0.38; p=0.911), and overall (β=0.22, 95% CI −0.08–0.52; p=0.145) did not vary significantly according to Indigenous status (see Supplementary Table 3 for linear regression coefficients for all variables included in the model).
Discussion
Findings from this exploratory study comparing Indigenous and non-Indigenous Australians with cirrhosis suggest that Indigenous patients are more likely to have medium or high supportive care needs, predominantly in the domains of psychological issues and physical and practical needs subscales. Although both patient cohorts demonstrated high needs on these subscales, high-level need was more frequent for Indigenous patients. Half of the Indigenous cohort reported moderate-to-high level of unmet needs in lack of energy, poor sleep, anxiety, and depression, and an additional 15 moderate-to-high unmet need items were reported in more than one-third of Indigenous patients.
This study did not address why patient needs are not met; however, a number of factors have been found to contribute to unmet needs for Indigenous people with chronic illness,16 including a lack of needs assessment in the liver clinics, lack of access to appropriate resources, or not feeling culturally safe.6,17,18 The delivery of optimal care to Indigenous Australians should be culturally safe and person-family and community centred.19–21 Inaccessibility and lack of cultural safety impair the engagement of Indigenous Australians for treatment or support.6,17,18
Indigenous patients indicated a moderate-to-high need for help with common, debilitating symptoms of cirrhosis. Needing help with lack of energy, poor sleep, and feeling unwell were needs at moderate-to-high levels. The cause of fatigue in cirrhosis is multifactorial and is associated with reduced motivation, cognitive difficulties, altered mood, neuromuscular dysfunction, and altered central neurotransmission.22 Moreover, fatigue in cirrhosis has a strong social component and is often associated with depression, anxiety,22 and poor sleep. While fatigue has been successfully managed with exercise in the cancer setting,23,24 the absence of evidence-based specific therapies for chronic liver disease makes management of fatigue in patients with cirrhosis challenging. Supportive management focusing on educating patients to better manage fatigue and controlling contributing factors (eg nocturnal pain, pruritus or nocturia) are useful clinical strategies.22 Lifestyle changes, including gradual increase in physical activity, can play a key role in managing fatigue and poor sleep, and it is vital that patients are empowered to address their symptoms. Together with their health care provider, patients need to learn strategies for self-management25 of fatigue.
Compared with non-Indigenous Australians with cirrhosis, Indigenous patients had a greater need for help with psychosocial issues. Mental illness contributes to more than one-third of Indigenous Australians' non-fatal burden of disease.26–28 Moreover, anxiety and depression may affect many aspects of care (e.g. adherence to medications and medical appointments), and engagement with social risk behaviours (e.g. alcohol misuse).29,30 The legacy of dispossession, social disruption and intergenerational trauma has led to higher rates of common mental disorders, such as anxiety, substance abuse and alcohol misuse among Indigenous Australians.26,28,31 Alcohol misuse and substance abuse are commonly used by victims of intergenerational trauma to cope with feelings of anxiety and despair.28 A cross-sectional study26 involving 544 Indigenous Australians reported that the prevalence of mental health disorders was four times higher than that of the general Australian population, while Indigenous Australians living on traditional lands had lower rates (50% less) of common mental health disorders than those living in mainstream communities. Embedding mental health and social workers in the multidisciplinary care of Indigenous patients with cirrhosis and using culturally appropriate targeted intervention programs for this patient group may help to address these difficult unmet needs.
For Indigenous patients with cirrhosis, reporting a higher rate of unmet needs is not an unexpected finding, as differences in health outcomes between Indigenous and non-Indigenous Australians have been well documented in cirrhosis and other chronic diseases.8,32,33 Previous studies involving the assessment of needs among cancer patients found that physical and psychological domains were important issues for Indigenous cancer patients.34,35
For most Indigenous patients included in this study, the education level was Junior High school or less, and over half of the patients had at least one comorbidity (eg diabetes, hypertension and obesity). Lower education rates directly impact health literacy, and health services must adapt to the changes in patient health literacy needs. The management of multiple comorbidities is challenging and can be aggravated by a low level of health literacy.36 Over 20% of the Indigenous patients reported moderate-to-high unmet needs with SNAC items about information to manage cirrhosis and its complications. This demonstrates that irrespective of health literacy level, Indigenous patients with cirrhosis have the same need to be informed about their illness, its prognosis and options for treatment as non-indigenous, but these needs are not sufficiently met by existing support services.
These findings are important in the context of increasing recognition of the burden of comorbidities for Indigenous people and the significance of chronic disease prevention and management for maintaining health, reducing morbidity, and increasing lifespan.37
Limitations of the study include the cross-sectional design and a small number of Indigenous patients. In addition, the assessment tool has not been specifically developed to be used by Indigenous people. However, this study used a reliable source of clinical data, including assessment of disease severity and aetiology by hepatologists. Patients were recruited from five large hospitals in Queensland, including a referral centre for the state-wide liver transplant service. Nevertheless, the study findings may not be directly generalizable to all patients with cirrhosis in Australia or other English-speaking countries.
Conclusion
Indigenous Australians with cirrhosis have higher levels of unmet needs in psychological issues and physical and practical needs subscales than non-Indigenous Australians with cirrhosis. A systematic assessment of patient needs is critical to optimise care,34 and the use of the SNAC tool in patients with cirrhosis may reliably identify high-need patients who require more complex care. Timely interventions or referral to appropriate services may improve outcomes for people diagnosed with cirrhosis. Indigenous Australians are disproportionately affected by cirrhosis,38,39 and liver diseases are among the most common contributors to the mortality gap between Indigenous and non-Indigenous Australian adults.40 A “one size fits all” approach to supporting patients with cirrhosis does not meet the increased supportive care need for Indigenous patients with higher rates of psychosocial, practical and physical needs. Further research is needed to extend and complement information about the supportive care needs of Indigenous Australians with cirrhosis, in particular exploring the needs experienced by this patient group through a qualitative study. To “Close the Gap” on health outcomes for Indigenous Australians with cirrhosis, coordinated and culturally appropriate services across the health system that are co-designed with the Indigenous Australian community are needed to meet the supportive needs of Indigenous patients. Delivery of culturally appropriate interventions that achieve community acceptance and “buy in” from Indigenous patients has the potential to optimize cirrhosis care and improve the quality of life of this patient group.
Ethics Approval and Informed Consent
Approval for the study was obtained from the Human Research Ethics Committees of the Metro South Health (HREC/16/QPAH/628) and QIMR Berghofer Medical Research Institute (P2207). Written informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
We thank the staff and patients of the participating hospitals for their assistance and cooperation in performing the current study.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tsochatzis EA, Bosch J, Burroughs AK. Liver cirrhosis. Lancet. 2014;383(9930):1749–1761. doi:10.1016/S0140-6736(14)60121-5
2. Deloitte Access Economics. The Economic Cost and Health Burden of Liver Diseases in Australia. The Gastroenterological Society of Australia/Australian Liver Association; 2013.
3. Marchesini G, Bianchi G, Amodio P, et al. Factors associated with poor health-related quality of life of patients with cirrhosis. Gastroenterology. 2001;120(1):170–178. doi:10.1053/gast.2001.21193
4. McPhail SM, Amarasena S, Stuart KA, et al. Assessment of health-related quality of life and health utilities in Australian patients with cirrhosis. JGH Open. 2021;5(1):133–142. doi:10.1002/jgh3.12462
5. Australian Institute of Health and Welfare. Bainbridge R, McCalman J, Clifford AKT. Cultural competency in the delivery of health services for Indigenous people. Produced for the Closing the Gap Clearinghouse. Cat No. AIHW. 2015;157(13). doi:10.25816/5ec4ba84d1241
6. Durey A, Thompson SC. Reducing the health disparities of indigenous Australians: time to change focus. BMC Health Serv Res. 2012;12(1):151. doi:10.1186/1472-6963-12-151
7. Wotherspoon C, Williams CM. Exploring the experiences of aboriginal and torres strait islander patients admitted to a metropolitan health service. Aust Health Rev. 2019;43(2):217–223. doi:10.1071/AH17096
8. Valery PC, Clark PJ, Pratt G, et al. Hospitalisation for cirrhosis in Australia: disparities in presentation and outcomes for indigenous Australians. Int J Equity Health. 2020;19(1):27. doi:10.1186/s12939-020-1144-6
9. Low JTS, Rohde G, Pittordou K, et al. Supportive and palliative care in people with cirrhosis: international systematic review of the perspective of patients, family members and health professionals. J Hepatol. 2018;69(6):1260–1273. doi:10.1016/j.jhep.2018.08.028
10. Valery PC, Clark PJ, McPhail SM, et al. Exploratory study into the unmet supportive needs of people diagnosed with cirrhosis in Queensland, Australia. Intern Med J. 2017;47(4):429–435. doi:10.1111/imj.13380
11. Valery PC, Powell E, Moses N, et al. Systematic review: unmet supportive care needs in people diagnosed with chronic liver disease. BMJ Open. 2015;5(4):e007451. doi:10.1136/bmjopen-2014-007451
12. Valery PC, Bernardes CM, Stuart KA, et al. Development and evaluation of the Supportive Needs Assessment Tool for Cirrhosis (SNAC). Patient Prefer Adherence. 2020;14:599–611. doi:10.2147/PPA.S236818
13. Fielding R, Lam WW, Shun SC, et al. Attributing variance in supportive care needs during cancer: culture-service, and individual differences, before clinical factors. PLoS One. 2013;8(5):e65099. doi:10.1371/journal.pone.0065099
14. Australian Bureau of Statistics (ABS). Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2006. Canberra, Australia: ABS; 2008.
15. Valery PC, Bernardes CM, McKillen B, et al. The patient’s perspective in cirrhosis: unmet supportive care needs differ by disease severity, etiology, and age. Hepatol Commun. 2021;5(5):891–905. doi:10.1002/hep4.1681
16. McMullen S, Grootemaat P, Winch S, et al. Perspectives on Chronic Disease in the Australian Indigenous Population: A Review of Literature. Centre for Health Service Development, Australian Health Services Research Institute, University of Wollongong; 2015.
17. Gruen RL, Weeramanthri TS, Bailie RS. Outreach and improved access to specialist services for indigenous people in remote Australia: the requirements for sustainability. J Epidemiol Community Health. 2002;56(7):517–521. doi:10.1136/jech.56.7.517
18. Hayman N. Strategies to improve indigenous access for urban and regional populations to health services. Heart Lung Circ. 2010;19(5–6):367–371. doi:10.1016/j.hlc.2010.02.014
19. Cancer Australia. National aboriginal and torres strait islander cancer framework 2015. Surry Hills, NSW; 2015. Available from: https://canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/national-aboriginal-and-torres-strait-islander-cancer-framework.
20. Cancer Australia. Optimal Care Pathway for Aboriginal and Torres Strait Islander People with Cancer. Surry Hills, NSW: Cancer Australia; 2018. Available from: https://www.canceraustralia.gov.au/publications-and-resources/cancer-australiapublications/optimal-care-pathway-aboriginal-and-torres-strait-islanderpeople-cancer.
21. The Wardliparingga Aboriginal Research Unit of the South Australian Health and Medical Research Institute. National Safety and Quality Health Service Standards User Guide for Aboriginal and Torres Strait Islander Health. Sydney: Australian Commission on Safety and Quality in Health Care; 2017. Available from: https://www.safetyandquality.gov.au/sites/default/files/migrated/National-Safety-and-Quality-Health-Service-Standards-User-Guide-for-Aboriginal-and-Torres-Strait-Islander-Health.pdf.
22. Swain MG, Jones DEJ. Fatigue in chronic liver disease: new insights and therapeutic approaches. Liver Int. 2019;39(1):6–19. doi:10.1111/liv.13919
23. Brown JC, Huedo-Medina TB, Pescatello LS, Pescatello SM, Ferrer RA, Johnson BT. Efficacy of exercise interventions in modulating cancer-related fatigue among adult cancer survivors: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2011;20(1):123–133. doi:10.1158/1055-9965.EPI-10-0988
24. Hayes SC, Newman B. Exercise in cancer recovery: an overview of the evidence. Cancer Forum. 2006;30(1):13–17.
25. Blackburn P, Freeston M, Baker CR, Jones DE, Newton JL. The role of psychological factors in the fatigue of primary biliary cirrhosis. Liver Int. 2007;27(5):654–661. doi:10.1111/j.1478-3231.2007.01500.x
26. Nasir BF, Toombs MR, Kondalsamy-Chennakesavan S, et al. Common mental disorders among Indigenous people living in regional, remote and metropolitan Australia: a cross-sectional study. BMJ Open. 2018;8(6):e020196. doi:10.1136/bmjopen-2017-020196
27. Queensland Health. The Burden of Disease and Injury in Queensland’s Aboriginal and Torres Strait Islander People 2017 (Reference Year 2011) Main Report. Brisbane: Queensland Health; 2017.
28. Toombs M, Hamptom R, Ward R. Impact of substance abuse, violence and self-harm in indigenous communities. In: Hamptom R, Toombs M, editor. Indigenous Australians and Health: The Wombat in the Room. Victoria, Australia: Oxford University Press; 2013:225–245.
29. Buganza-Torio E, Mitchell N, Abraldes JG, et al. Depression in cirrhosis - a prospective evaluation of the prevalence, predictors and development of a screening nomogram. Aliment Pharmacol Ther. 2019;49(2):194–201. doi:10.1111/apt.15068
30. Rabiee A, Ximenes RO, Nikayin S, et al. Factors associated with health-related quality of life in patients with cirrhosis: a systematic review. Liver Int. 2021;41(1):6–15. doi:10.1111/liv.14680
31. Parker R. Australia’s aboriginal population and mental health. J Nerv Ment Dis. 2010;198(1):3–7. doi:10.1097/NMD.0b013e3181c7e7bc
32. Australian Institute of Health and Welfare (AIHW). Aboriginal and Torres Strait Islander Health Performance Framework 2020 -Summary Report; 2020.
33. Dudgeon P, Walker R, Scrine C, Shepherd C, Calma T, Ring I. Effective Strategies to Strengthen the Mental Health and Wellbeing of Aboriginal and Torres Strait Islander People: Issues Paper No. 12 Produced for the Closing the Gap Clearinghouse. AIHW; 2014.
34. Bernardes CM, Beesley V, Martin J, et al. Unmet supportive care needs among people with cancer: a cross-cultural comparison between indigenous and non-indigenous Australians. Eur J Cancer Care. 2019;28(5):e13080. doi:10.1111/ecc.13080
35. Bernardes CM, Diaz A, Valery PC, et al. Unmet supportive care needs among indigenous cancer patients across Australia. Rural Remote Health. 2019;19(3):4660.
36. Ramaswamy R. Complex care: treating an older patient with multiple comorbidities. Am Fam Physician. 2014;89(5):392–394.
37. Broe GT, Radford K. Multimorbidity in Aboriginal and non-Aboriginal people. Med J Aust. 2018;209(1):16–17. doi:10.5694/mja18.00348
38. Australian Institute of Health and Welfare (AIHW). Cancer in Aboriginal & Torres Strait Islander People of Australia. Canberra: AIHW; 2018.
39. Powell EE, Skoien R, Rahman T, et al. Increasing hospitalization rates for cirrhosis: overrepresentation of disadvantaged Australians. EClinicalMedicine. 2019;11:44–53. doi:10.1016/j.eclinm.2019.05.007
40. Commonwealth of Australia. Closing the Gap Report 2020. Canberra, Australia:: Commonwealth of Australia; 2020.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
