Back to Journals » Patient Preference and Adherence » Volume 17
Disease-Related Knowledge and Need for Revision of Care for Patients with Atrial Fibrillation: A Cross Sectional Study
Authors Erlingsdottir HY , Ketilsdottir A , Hendriks JM , Ingadottir B
Received 1 July 2023
Accepted for publication 29 September 2023
Published 24 October 2023 Volume 2023:17 Pages 2621—2630
DOI https://doi.org/10.2147/PPA.S428444
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Helga Yr Erlingsdottir,1,2 Audur Ketilsdottir,1,2 Jeroen M Hendriks,3,4 Brynja Ingadottir1,5
1Faculty of Nursing and Midwifery, School of Health Sciences, University of Iceland, Reykjavik, Iceland; 2Cardio-Vascular and Cancer Center, Landspitali – The National University Hospital of Iceland, Reykjavik, Iceland; 3Caring Futures Institute, College of Nursing and Health Sciences, Flinders University, Adelaide, SA, Australia; 4Centre for Heart Rhythm Disorders, University of Adelaide and Royal Adelaide Hospital, Adelaide, SA, Australia; 5Office of Chief Nursing Officer, Landspitali – The National University Hospital of Iceland, Reykjavik, Iceland
Correspondence: Helga Yr Erlingsdottir, Cardio-Vascular and Cancer Center, Landspitali – The National University Hospital of Iceland, Hringbraut, 101, Reykjavik, Iceland, Tel +354 865 7764, Email [email protected]
Purpose: To evaluate the disease-related knowledge of outpatients with atrial fibrillation (AF), and the relationship with health literacy and other background variables.
Patients and Methods: In this cross-sectional survey study, conducted in Iceland, patients with AF scheduled for an electrical cardioversion or AF catheter ablation were recruited from a hospital outpatient clinic. They completed the validated Atrial Fibrillation Knowledge Scale (AFKS), a 11-item instrument (with possible score 0– 10, 10 being the best knowledge) which evaluates knowledge pertaining to AF in general, AF symptom detection and AF treatment. Health literacy was assessed with the 16 item European Health Literacy Survey Questionnaire (HLS-EU-Q) and patients answered questions about their background. Data was analysed with parametric tests.
Results: In total, 185 participants completed the questionnaire (mean age 63 ± 10), 77% were male, 74% with previous electrical cardioversion and 76% were on non-vitamin K antagonist oral anticoagulants (NOAC) medication. The mean score on the AFKS was 6.5 (± 1.8). The best knowledge was concerning oral anticoagulation therapy (96% answered correctly) and the least knowledge was regarding responses to AF episodes (17% answered correctly). Patients with sufficient health literacy (52%) had better knowledge of AF (M 6.8 ± 1.7 vs M 6.3 ± 1.9, p = 0.05). Age, educational level, health literacy and AF pattern explained 22% of the variance in AF knowledge.
Conclusion: Patients with AF have inadequate knowledge of their condition, potentially as a result of insufficient health literacy. AF knowledge may be improved using integrated management where patients are actively involved in the care and health literacy is considered in the provided patient education.
Keywords: atrial fibrillation, health literacy, patient education, patient knowledge, self-care
Introduction
Atrial fibrillation (AF) is the most prevalent cardiac arrhythmia and if not treated appropriately it can have severe consequences, eg heart failure, cardiomyopathy, or stroke as well as dementia, depression and impaired quality of life.1,2 The arrhythmia is classified by presentation, regardless of treatment: first diagnosed, paroxysmal (terminates within seven days of onset), persistent (sustained beyond seven days), long-standing persistent (continuous longer than 12 months) and permanent (when no further attempts to restore sinus-rhythm will be attempted).3 Although patients may be asymptomatic, possible symptoms include dyspnoea, palpitations, fatigue, and dizziness.1,4 The risk factors for AF are increasing age, hypertension, coronary artery disease (CAD), heart failure, obesity, diabetes mellitus (DM), chronic kidney disease, obstructive sleep apnoea, smoking and excessive alcohol consumption.1 Hypertension is the most prevalent risk factor for AF, being present in up to 71%, followed by CAD which has been found to be present in up to 38% of AF patients5 but AF has also been shown to promote CAD.6 Patients hospitalized for myocardial infarction complicated with AF have a risk of adverse prognostic implications and also long-term mortality7 and CAD can significantly increase the risk of paroxysmal AF recurring after catheter ablation.8 This complex relationship has to be considered when managing AF.9
Anticoagulation therapy is a significant part of AF management to prevent incidences of stroke. In the last decade, the therapy has shifted from vitamin K antagonists (VKA) to non-vitamin K antagonist oral anticoagulants (NOAC) treatment.2,10
Due to the aging of the world’s population, increased incidence, and the burden of risk factors, the prevalence of AF is increasing globally.2 This also applies to Iceland, with the prevalence expected to increase from 2% to 3.5% in the next 30 years.11 To achieve comprehensive treatment, the 2020 ESC guidelines for the diagnosis and management of AF propose an integrated ABC approach, namely: Anticoagulation/Avoid stroke for prevention of thromboembolism; Better symptom management for rate and rhythm control; and Cardiovascular and Comorbidity optimisation for modification of precipitating causes such as risk factors related to unhealthy lifestyle.2 For optimal results it is important that the patients are involved in the decision-making concerning management of their AF, along with an interdisciplinary collaboration between health care professionals.2
Sufficient knowledge is a prerequisite for patient’s decision-making, active participation and self-care.12 Patients therefore need to receive education for multi-dimensional knowledge of their condition and its treatment.13–15 Several studies have reported insufficient disease-related knowledge among patients with AF.16,17 Factors related to AF knowledge have been identified where lower age and higher educational level positively contribute to AF knowledge16,18–20 whereas factors such as being recently diagnosed with AF or having a diagnosis of heart failure or diabetes are negatively associated with AF knowledge.16,19
In this context, health literacy is relevant and is becoming an increasing concept of interest within patient education. Health literacy has been defined as the
knowledge, motivation and competences to access, understand, appraise and apply health information in order to make judgements and take decisions in everyday life concerning health care, disease prevention and health promotion to maintain or improve quality of life during the life course. (p. 3)21
Health literacy needs to be considered when educating patients, and clinical AF guidelines emphasise patient-centred education about AF and self-care.2,14,22
Effective patient education may require repetition with a follow-up after hospital discharge providing opportunity to ask questions and get more detailed information.13 Patients who receive education about AF, symptoms and treatment and follow-up from nurse specialists have been shown to have significantly better knowledge of their disease.18
In Iceland, neither the effect of provided patient education nor the disease-related knowledge of patients with AF has been studied before. A preparatory work is being conducted before starting an interdisciplinary, integrated AF outpatient service. This service will aim to meet patients’ needs, support self-care, include them in care development and ultimately improve their outcomes. As part of that work, it is important to explore patient knowledge and understanding of their condition. Therefore, the aim of this study was to evaluate the disease-related knowledge of patients with AF and its relationship with health literacy and background.
Materials and Methods
Participants and Procedure
In this cross-sectional survey study data was collected with posted questionnaires. Eligible for participation were all adult (≥18 years) patients diagnosed with AF and scheduled for electrical cardioversion (n = 41) or AF catheter ablation (n = 237) at Landspitali-The National University Hospital of Iceland in October 2018. Excluded were patients who could not understand Icelandic.
A questionnaire, an information letter and a pre-stamped envelope were posted to eligible patients on the waiting list, and they could choose between answering the questionnaire by returning the printed copy or answering an online version through a provided URL. Online data were collected and managed using Research Electronic Data Capture (REDCap) tools hosted at the University of Iceland.23 A reminder phone call was made two weeks later to those patients who had not responded.
The current procedure is that patients are placed on the waiting list for catheter ablation after either the first or repeated episodes of AF not responding to medical treatment. The time from the onset of AF varies between patients and they can be referred to the waiting list following admission to hospital or by cardiologists working in private clinics. The patients receive a phone call from a nurse when the procedure has been scheduled with admission information and basic information about the procedure but no specific information about AF. An information leaflet is added to the verbal information about the procedure.
Measures
AF Knowledge
Knowledge of AF was evaluated with the Icelandic version of the AF Knowledge Scale (AFKS), developed in the Netherlands by Hendriks et al, to evaluate general knowledge about AF among patients and to tailor the patient’s education according to the results.24 The AFKS consists of 11 items divided into three categories: AF in general, AF symptom detection, and AF treatment. Each item has three response options, of which only one is correct. One point is awarded for the correct answer, but no deduction is made for incorrect answers, thus possible scores are 0–11, with 0 indicating the worst knowledge, and 11 indicating excellent knowledge (for questions see Supplementary Figure 1). The questionnaire is not designed to detect dementia in AF but could provide signs/triggers to further investigate dementia, once it becomes obvious that patients have difficulties completing the questionnaire.24 The questionnaire’s reliability and validity have previously been evaluated as well as its sensitivity to the patient knowledge and the utilisation value of the instrument in the treatment of AF. The original items were reduced from 14 to 11 to increase the validity of the measuring instrument after a pre-test for a group of patients, cardiologists, and cardiac nurses. For reliability, the Cronbach’s alpha coefficient was calculated and proved to be 0.5824 which was considered acceptable due to a rather short instrument and regarding sensitivity the scale differentiates between minimal, moderate and high score. The Cronbach’s alpha in the current study was 0.67.
The English version of the AFKS was first translated into Icelandic by a certified translator and a nurse, independently. These two versions were reviewed and merged by the researchers and subsequently back-translated into English by a native English-speaking person. Thereafter it was submitted to five individuals with AF for further assessment, which led to changes before the final Icelandic version was ready. The translation process revealed that question 11, which asks about the thrombosis centre where the previously most common warfarin treatment is traditionally monitored and managed, was not relevant to many patients. The explanation for this may be that the need for thrombosis centres is becoming less due to more general use of NOAC. Through consultation with the instrument’s author the researchers decided to make item 11 only applicable to those patients who were prescribed warfarin and leave it out in the total score sum. Therefore, ten questions were used to calculate the total score, with a possible range being 0 to 10.
Health Literacy
Health literacy was evaluated with the European Health Literacy Survey Questionnaire (HLS-EU-Q)25 which consists of 16 items concerning access, understanding, and skills in utilisation of health information. Each item has four response options (very difficult, fairly difficult, fairly easy, very easy) and the answers are dichotomised so that very difficult and fairly difficult are scored as zero (0) and easy and fairly easy as one (1). A possible total score is 0–16 and scores can be categorised further into inadequate (score 0–8), problematic (score 9–12) and sufficient (score 13–16). The HLS-EU-Q has been validated in several European languages and the Icelandic version has been found to have acceptable psychometric properties.26
Background
Based on the literature on patients’ disease-related knowledge and recommendations from the German AF competence NETwork (AFNET) and the European Heart Rhythm Association (EHRA),27 background questions were created. Patients were asked to mark which description of AF applied best to them. The purpose was to assess the patients’ awareness of their condition which is important for their disease management and understanding of the disease. The response options were five and it was possible to choose more than one option: 1) AF present for seven days or less (paroxysmal), 2) Sustained AF for more than one week (persistent), 3) Continuous episodes of AF for 12 months or longer (long-standing persistent, 4) Chronic AF for longer than 12 months (permanent), 5) Don´t know. In addition, patients were asked to write up their prescribed medication, about comorbidities (open questions on other diseases/conditions they had), and their age, sex, highest educational level, employment, marital status, number of household members, and if they had previously had electrical conversion (yes or no).
Statistical Analysis
Descriptive statistics are presented as mean ±SD or n (%). Characteristics were compared using t-tests, chi-squared tests, and analysis of variance (ANOVA) depending on the level of measurement. Before data analysis the health literacy data was dichotomised into insufficient (score 0–12) and sufficient (score 13–16) health literacy. Linear, stepwise, regression was used to determine independent predictors of knowledge from sociodemographic and clinical characteristics.
In all tests, the level of statistical significance was set at ≤0.05. Electronic responses and data from printed questionnaires were transferred coded into SPSS version 26 (IBM Corp., Armonk, NY, USA) which was used for data analysis.
Ethical Considerations
The study conforms with the principles outlined in the Declaration of Helsinki.28 It was approved by the Ethical Committee of Landspitali – The National University Hospital of Iceland (38/2018) and the hospital management. Patients were informed that returning the questionnaire would be interpreted as consent to participation.
Results
Of 278 patients waiting for electrical conversion and/or AF catheter ablation, 259 were eligible for inclusion and were invited to participate in the study. In total, 187 patients participated (72%), of which 59% returned printed versions. Two questionnaires were not usable because they were not properly filled out, resulting in 185 analysed questionnaires. The mean age of the participants was 63 ±10 with men representing 77%. Most of the participants described their AF as paroxysmal AF (39%), 24% had permanent AF, 6% had persistent AF and 3% had long-standing persistent AF. Almost three-quarters (74%) had undergone electrical conversion before and 76% were taking NOACs as an anticoagulation treatment. Half of the participants (51%) had other health problems than AF as well, such as arthritis (35%), hypertension (23%), DM 2 (13%), sleep apnoea (13%) and coronary artery disease (4%). Of the participants, 84% were in a relationship and 34% had university degree. Patient characteristics are presented in Table 1.
 |
Table 1 Characteristics of the Participants (N = 185) |
The mean score on the AFKS was 6.5 ± 1.8. Two participants (1%) answered all 10 questions correctly, 20 participants (11%) scored nine or more, and 28% scored seven out of 10 (Figure 1). The best knowledge pertained to oral anticoagulation therapy (96% answered correctly) and the least knowledge concerned reactions to AF (17% answered correctly).
 |
Figure 1 Percentage distribution of the number of correctly answered questions to the AFKS by the participants. |
The mean score on the HLS-EU-Q was 12.3 (SD 3.1) and 12% of patients had inadequate health literacy, 37% had problematic health literacy and 52% had sufficient health literacy (Figure 2).
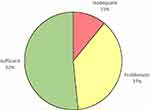 |
Figure 2 Health literacy of the AF patients in Iceland. |
Older participants were more likely to have less knowledge than younger participants (rp=−0.34, p < 0.001). No difference in knowledge was found between men and women but participants with a university degree had significantly better knowledge than other participants (F(2,17)=13.98, p < 0.001).
The participants with paroxysmal AF had significantly better knowledge of AF than the participants who did not know what AF pattern they had. There was not a significant difference between the other groups.
Participants with sufficient health literacy had better knowledge of AF than patients with insufficient health literacy (t(178)=1.95, p = 0.05). The relationship between AF knowledge and background factors is presented in Table 2.
 |
Table 2 Relationship Between Background Variables and AF Knowledge (AFKS) |
All six background variables (age, education, AF pattern, health literacy, number of household members and employment) found to be related to AF knowledge (p ≤ 0.05, Table 2) in a one-way ANOVA were included in a multiple regression analysis. The final model showed that age, education, health literacy and AF pattern explained 22% of the variance in AF knowledge, with other variables being equal (Table 3). Education and health literacy contributed positively to the AF knowledge where there was a gradual increase in the average knowledge with participants with university degrees compared to participants with other levels of education and participants with sufficient health literacy had better AF knowledge compared to those with insufficient health literacy. Older age and not knowing AF pattern negatively affected knowledge where there was a gradual decrease in the average AF knowledge with increasing age and those who had paroxysmal AF had significantly better knowledge than those who did not know their AF pattern.
 |
Table 3 Relationship Between Knowledge on AF and Background Variables Using Multiple Regression Analysis (N = 167) |
Discussion
This study contributes to the emerging evidence of patient knowledge and its importance in the management of AF. The results imply that patients’ knowledge of AF is suboptimal, especially concerning self-care and only half of the patients had sufficient health literacy. We found that education, age, AF pattern and health literacy are independent contributing factors to explaining the variance in disease-related knowledge.
Insufficient patient knowledge is in accordance with previous international studies which report patient knowledge ranging from 40% to 70% of the optimal.18,19,29,30 The patients had good knowledge about anticoagulation treatment and 96% knew the purpose of anticoagulation medications. This corresponds to other studies19,20 and reflects well the emphasis on anticoagulation in the treatment of AF. However, only 55% could correctly answer the question about the adverse effects of alcohol on anticoagulation treatment which could indicate that other important issues, such as interaction with other substances, need to be explained better.
Knowledge about necessary self-care, ie monitoring symptoms and responding to them31 was insufficient, and it was interesting that 36% of participants answered that AF was life-threatening, whereas it does not need to be if treated properly. The causes and consequences of the symptoms of AF, ie shortness of breath and palpitations, can be unclear and some symptoms subtle, like irregular heart rate.31 This supports the importance of patient-centred education, for example on signs and symptoms patients should react to and what self-care is needed and when, as emphasised in the 2020 ESC guidelines.2
Patient knowledge was negatively correlated with age, similar to what has been reported in other studies16–20 and is a cause of concern because the oldest group is also the one at the highest risk of having a stroke because of AF.20 It is not clear what explains the effect of age on knowledge, but multimorbidity, which is associated with decreased cognitive functioning32 as well as insufficient patient education may explain that relationship.
Most patients defined themselves as having paroxysmal AF, and they had better knowledge than those who did not know their pattern. Paroxysmal AF is more common in the early stages of the disease and these patients may have received subsequent disease-related patient education more recently, explaining their better knowledge.2
A higher level of education increases the probability of good patient knowledge about AF. It is possible that individuals with a higher education level have a better capability to seek practical information and to find useful patient information, ie that they have better health literacy.
Patient knowledge about AF also improved with better health literacy but half of the patients had insufficient health literacy, similar to what is reported in other countries.33 The importance of health literacy is becoming more evident12 and insufficient health literacy is thought to be one of the factors hindering patients with AF, similar to other patient populations, from participating and making decisions concerning their AF treatment.34 To meet these challenges, healthcare organisations have been tasked to become health literate, ie to make it easier for people to navigate, understand, and use information and services to take care of their health.35
In order to sustain and increase knowledge, patients need education provided by competent healthcare professionals based on the best available evidence36 where repetition is regarded very important.18,20,29,30,37 This study suggests that patients with AF are in need for such education but their hospital stay is often brief, with limited time for education.20 The holistic ABC approach in the 2020 ESC guidelines recommends person-centred management where patient education is a crucial element of self-care and lifestyle modification. A holistic approach implies that diverse groups are considered and therefore individualised and repeated education is important.2 Novel care approaches (integrated care) with multidisciplinary team have been successful in increasing patient knowledge18 and improving patients’ quality of life18,38,39 and such care models have indeed been advised in the ESC guidelines.40 The results of this study support that the implementation of integrated care is warranted, including in Iceland. Furthermore, the AFKS is a practical measurement tool that is useful in the assessment of educational needs, the development of individualised educational plans and in assessing the outcomes of patient-education.24,37,40
Finally, the fact that most participants (76%) were prescribed NOACs as an anticoagulation therapy but only 6% were taking warfarin, reflects the fast transition that has occurred in medical care, from warfarin to NOACs.10,19,20,29 This supports the decision to exclude item 11 in our analysis of patient knowledge as it was only applicable to the minority of patients.
This study is not without limitations. The researchers acknowledge that the study sample was limited to patients scheduled for rhythm control by cardioversion and ablation, and the results may therefore not be generalizable to all patients with AF. As no registry is existent in Iceland on patients diagnosed with AF this was the only option available to recruit patients. The fact that 28% of the participants responded that they did not know or chose more than one option when asked about their AF pattern may indicate that the wording of the question was not clear enough. We also acknowledge the limitations of self-report which may cause biases and inaccurate data for example, on comorbidities and AF pattern.
Conclusion
Patients with AF have inadequate knowledge of their condition, potentially as a result of insufficient health literacy. AF knowledge may be improved using integrated management where patients are actively involved in the care and health literacy is considered in the provided patient education.
Acknowledgments
We thank Ms Lilja Thorsteinsdottir and Dr. Hlynur Bárðarson for assistance with data collection and processing.
Funding
We acknowledge financial support from the Icelandic Nurses’ Research and Science Fund.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Virani SS, Alonso A, Aparicio HJ, et al. Heart disease and stroke statistics—2021 update. Circulation. 2021;143(8):e254–e743. doi:10.1161/CIR.0000000000000950
2. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2021;42(5):373–498. doi:10.1093/eurheartj/ehaa612
3. Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–2962. doi:10.1093/eurheartj/ehw210
4. Gleason KT, Nazarian S, Dennison Himmelfarb CR. Atrial fibrillation symptoms and sex, race, and psychological distress. J Cardiovasc Nurs. 2018;33(2):137–143. doi:10.1097/JCN.0000000000000421
5. Greene HL. Baseline characteristics of patients with atrial fibrillation: the AFFIRM study. Am Heart J. 2002;143(6). doi:10.1067/mhj.2002.122875
6. Sharma YP, Batta A, Makkar K, et al. Angiographic profile and outcomes in persistent non-valvular atrial fibrillation: a study from tertiary care center in North India. Indian Heart J. 2022;74(1). doi:10.1016/j.ihj.2021.12.010
7. Schmitt J, Duray G, Gersh BJ, Hohnloser SH. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009;30(9):1038–1045. doi:10.1093/eurheartj/ehn579
8. Cui YK, Dong JZ, Du X, et al. Outcome of catheter ablation for paroxysmal atrial fibrillation in patients with stable coronary artery disease. PACE Pacing Clin Electrophysiol. 2022;45(9):1032–1041. doi:10.1111/pace.14571
9. Batta A, Hatwal J, Batta A, Verma S, Sharma YP. Atrial fibrillation and coronary artery disease: an integrative review focusing on therapeutic implications of this relationship. World J Cardiol. 2023;15(5):229–243. doi:10.4330/wjc.v15.i5.229
10. Güzel T, Aktan A, Kılıç R, et al. Oral anticoagulant use and long-term follow-up results in patients with non-valvular atrial fibrillation in Turkey AFTER-2 study. Anatol J Cardiol. 2022;26(7):567–576. doi:10.5152/AnatolJCardiol.2022.1597
11. Stefansdottir H, Aspelund T, Gudnason V, Arnar DO. Trends in the incidence and prevalence of atrial fibrillation in Iceland and future projections. EP Europace. 2011;13(8):1110–1117. doi:10.1093/europace/eur132
12. Magnani JW, Mujahid MS, Aronow HD, et al. Health literacy and cardiovascular disease: fundamental relevance to primary and secondary prevention: a scientific statement from the American Heart Association. Circulation. 2018;138(2). doi:10.1161/CIR.0000000000000579
13. Cutugno CL. Atrial fibrillation: updated management guidelines and nursing implications. Am J Nurs. 2015;115(5):26–38. doi:10.1097/01.NAJ.0000465028.05223.39
14. January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: executive summary. J Am Coll Cardiol. 2014;64(21):2246–2280. doi:10.1016/j.jacc.2014.03.021
15. Leino-Kilpi H, Johansson K, Heikkinen K, Kaljonen A, Virtanen H, Salantera S. Patient education and health-related quality of life: surgical hospital patients as a case in point. J Nurs Care Qual. 2005;20(4):307–308. doi:10.1097/00001786-200510000-00005
16. Desteghe L, Engelhard L, Raymaekers Z, et al. Knowledge gaps in patients with atrial fibrillation revealed by a new validated knowledge questionnaire. Int J Cardiol. 2016:223. doi:10.1016/j.ijcard.2016.08.303
17. Frankel DS, Parker SE, Rosenfeld LE, Gorelick PB. HRS/NSA 2014 survey of atrial fibrillation and stroke: gaps in knowledge and perspective, opportunities for improvement. Heart Rhythm. 2015;12(8):e105–e113. doi:10.1016/j.hrthm.2015.04.039
18. Hendriks JML, Vrijhoef HJM, Crijns HJGM, Brunner-La Rocca HP. The effect of a nurse-led integrated chronic care approach on quality of life in patients with atrial fibrillation. Europace. 2014;16(4):491–499. doi:10.1093/europace/eut286
19. Janion-Sadowska A, Sadowski M, Konieczyńska M, et al. Polish regional differences in patient knowledge on atrial fibrillation and its management as well as in patterns of oral anticoagulant prescription. Kardiol Pol. 2019;77(4):437–444. doi:10.5603/KP.a2019.0036
20. McCabe PJ, Schad S, Hampton A, Holland DE. Knowledge and self-management behaviors of patients with recently detected atrial fibrillation. Heart Lung. 2008;37(2):79–90. doi:10.1016/j.hrtlng.2007.02.006
21. Sørensen K, Van den Broucke S, Fullam J, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. 2012;12(1):80. doi:10.1186/1471-2458-12-80
22. Excellence NI for H and C. Atrial fibrillation: management | guidance | NICE; 2014. Available from: Https://WwwNiceOrgUk/Guidance/Cg180.
23. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)-A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi:10.1016/j.jbi.2008.08.010
24. Hendriks JML, Crijns HJGM, Tieleman RG, Vrijhoef HJM. The atrial fibrillation knowledge scale: development, validation and results. Int J Cardiol. 2013;168(2):1422–1428. doi:10.1016/j.ijcard.2012.12.047
25. Sørensen K, Van den Broucke S, Pelikan JM, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health. 2013;13(1):948. doi:10.1186/1471-2458-13-948
26. Gustafsdottir SS, Sigurdardottir AK, Arnadottir SA, Heimisson GT, Mårtensson L. Translation and cross-cultural adaptation of the European health literacy survey questionnaire, HLS-EU-Q16: the Icelandic version. BMC Public Health. 2020;20(1):61. doi:10.1186/s12889-020-8162-6
27. Kirchhof P, Auricchio A, Bax J, et al. Outcome parameters for trials in atrial fibrillation: executive summary: recommendations from a consensus conference organized by the German Atrial Fibrillation Competence NETwork (AFNET) and the European Heart Rhythm Association (EHRA). Eur Heart J. 2007;28(22):2803–2817. doi:10.1093/eurheartj/ehm358
28. World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/jama.2013.281053
29. Desteghe L, Engelhard L, Vijgen J, et al. Effect of reinforced, targeted in-person education using the Jessa Atrial fibrillation Knowledge Questionnaire in patients with atrial fibrillation: a randomized controlled trial. Eur J Cardiovasc Nurs. 2019;18(3):194–203. doi:10.1177/1474515118804353
30. Clarkesmith DE, Pattison HM, Lip GYH, Lane DA, ten Cate H. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One. 2013;8(9):e74037. doi:10.1371/journal.pone.0074037
31. Riegel B, Jaarsma T, Lee CS, Strömberg A. Integrating symptoms into the middle-range theory of self-care of chronic illness. Adv Nurs Sci. 2019;42(3):206–215. doi:10.1097/ANS.0000000000000237
32. Kadambi S, Abdallah M, Loh KP. Multimorbidity, function, and cognition in aging. Clin Geriatr Med. 2020;36(4):569–584. doi:10.1016/j.cger.2020.06.002
33. Sorensen K, Pelikan JM, Rothlin F, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health. 2015;25(6):1053–1058. doi:10.1093/eurpub/ckv043
34. Aronis KN, Edgar B, Lin W, Martins MAP, Paasche-Orlow MK, Magnani JW. Health literacy and atrial fibrillation: relevance and future directions for patient-centred care. Euro Cardiol Rev. 2017;12(1):52. doi:10.15420/ecr.2017:2:2
35. Brach C, Keller D, Hernandez LM, et al. Ten attributes of health literate health care organizations. participants in the workgroup on attributes of a health literate organization of the IOM Roundtable on health literacy. NAM Perspect. 2012;02(6). doi:10.31478/201206a
36. Health Care Education Association. Patient education practice guidelines for health care professionals. Available from: https://www.hcea-info.org/patient-education-practice-guidelines-for-health-care-professionals.
37. Ferguson C, Hendriks J. Partnering with patients in shared decision-making for stroke prevention in atrial fibrillation. Eur J Cardiovasc Nurs. 2017;16(3):178–180. doi:10.1177/1474515116685193
38. Angaran P, Mariano Z, Dragan V, et al. The atrial fibrillation therapies after ER visit: outpatient care for patients with acute AF - the AFTER3 study. J Atr Fibrillation. 2015;7(5). doi:10.4022/jafib.1187
39. Yaeger A, Cash NR, Parham T, et al. A nurse‐led limited risk factor modification program to address obesity and obstructive sleep apnea in atrial fibrillation patients. J Am Heart Assoc. 2018;7(23). doi:10.1161/JAHA.118.010414
40. Hendriks JML, Heidbüchel H. The management of atrial fibrillation: an integrated team approach – insights of the 2016 European Society of cardiology guidelines for the management of atrial fibrillation for nurses and allied health professionals. Eur J Cardiovasc Nurs. 2019;18(2):88–95. doi:10.1177/1474515118804480
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
