Back to Journals » Patient Preference and Adherence » Volume 17
Disease Burden and Treatment Preferences Amongst Postmenopausal Women with Severe Osteoporosis in Greece
Authors Souliotis K , Golna C, Poimenidou C, Drakopoulou T, Tsekoura M, Willems D, Kountouris V, Makras P
Received 7 August 2022
Accepted for publication 5 November 2022
Published 10 January 2023 Volume 2023:17 Pages 107—118
DOI https://doi.org/10.2147/PPA.S385351
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Kyriakos Souliotis,1,2 Christina Golna,2 Christina Poimenidou,2 Tatiana Drakopoulou,3 Memi Tsekoura,2 Damon Willems,4 Vasileios Kountouris,5 Polyzois Makras6
1Department of Social and Education Policy, University of Peloponnese, Corinth, Greece; 2Research Department, Health Policy Institute, Maroussi, Greece; 3Greek Bone Health Association “Petalouda”, Perama, Greece; 4Market Access Lead, UCB Pharma, Brussels, Belgium; 5External Engagement Lead, UCB Pharma, Athens, Greece; 6Department of Endocrinology and Diabetes and Department of Medical Research, 251 Hellenic Air Force & VA General Hospital, Athens, Greece
Correspondence: Kyriakos Souliotis, Email [email protected]
Objective: The objectives of this study were to elicit self-reported health status, quantify osteoporosis-related burden, and understand preferences for treatment attributes among postmenopausal women with severe osteoporosis in Greece.
Methods: Postmenopausal women with self-reported severe osteoporosis, defined as having suffered at least one osteoporotic fracture and reporting a T-score of ≤− 2.5, were asked to evaluate their health status, osteoporosis management, and disease-related physical, emotional, and financial burden. Participants were also asked to rate a series of treatment attributes and state their preference for unlabeled anabolic treatments, based on scenarios describing key treatment characteristics.
Results: Approximately one third (31%) of the 186 participants who responded to the survey in full had been living with severe osteoporosis for more than 10 years. Three quarters of participants (72%) considered their overall quality of life (QoL) to be worse than it had been 10 years prior, and the vast majority (89%) attributed this deterioration to osteoporosis. Direct, out of pocket, disease-related costs of at least € 100 per month were reported by 86% of participants. Patients attached the greatest value to a treatment that would decrease probability of future fractures, followed by increase in bone density, safety, and mode and frequency of administration. When asked to select their preferred treatment scenario between two anabolic treatments, 70% of participants opted for the scenario that shared treatment characteristics with romosozumab over a scenario that shared treatment characteristics with teriparatide.
Conclusion: Our study revealed that osteoporosis placed a considerable burden on QoL for postmenopausal women with severe osteoporosis in Greece. Patients reported valuing treatment efficacy, measured through reduction in future fractures and increase in bone density, and safety, as key treatment attributes.
Keywords: osteoporosis, patient preference, burden of disease, quality of life
Plain Language Summary
This study aimed to describe patient-reported health status and quality of life in postmenopausal women with severe osteoporosis in Greece, and to understand patient preferences for osteoporosis therapies. Postmenopausal women with self-reported severe osteoporosis evaluated their health status, osteoporosis management, and disease-related physical, emotional, and financial burden. They also rated a series of treatments attributes and stated their preference for one out of two unlabeled osteoporosis treatments. Three quarters of the participants reported that their quality of life had reduced over the last 10 years, and most of these participants reported that this was due to their osteoporosis. When asked about treatment preferences, patients valued a treatment that would decrease probability of future fractures, followed by increase in bone density, safety, mode of administration, and frequency of administration. Our study revealed that osteoporosis can place a considerable burden on QoL for postmenopausal women with severe osteoporosis in Greece. Overall, patients valued the treatment that was more effective and safer.
Introduction
Osteoporosis is becoming increasingly prevalent worldwide and can place a substantial burden on patients in terms of quality of life (QoL) and disability. A systematic analysis of the Global Burden of Disease 2019 reported 178 million (95% uncertainly interval [UI] 162–196) new cases of fracture, 445 million (428–484) prevalent fractures, and 25.8 million (17.8–35.8) years of healthy life lost due to disability (YLDs) due to fractures. Between 1990 and 2019, the absolute number of incident cases increased by 33.4% and of prevalent cases by 70.1%, despite a decrease in age standardized rate of total incident and prevalent fractures. These findings reflect the increase in fractures with age and the rapidly growing global shift towards an ageing society.1 Further, and according to the most recent SCOPE report, the annual number of osteoporotic fractures in the EU27+2 is expected to increase by 1.06 million, from 4.28 million in 2019 to 5.34 million in 2034.2
Osteoporosis is managed with pharmacological treatment. Patients consider attributes of their treatment, such as treatment efficacy, safety, mode/frequency of administration, and cost as very important.3 Early diagnosis and access to care are critical to the management of osteoporosis, by increasing bone mineral density and reducing fracture risk. Global clinical guidelines focus on fracture risk assessment, diagnosis, pharmacological treatment, and follow-up to achieve better disease control and improved public health outcomes. Incorporating patient preferences and perceptions in the management of osteoporosis, including health research, treatment guidelines, and regulatory processes, has been shown to inform healthcare resource allocation and is considered best practice by the World Health Organization (WHO) and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO).4 This is particularly important when drafting osteoporosis treatment guidelines, which traditionally overlook or underplay patient values and preferences.5
In Greece, approximately 99,000 new fragility fractures, or 272 fractures per day, were estimated to have occurred in 2019, an increase of 1.8 fractures/1,000 individuals compared with 2010. The annual number of deaths associated with a fracture event was estimated at 130 per 100,000 individuals aged 50 years or over. Lifetime probability of hip fracture (%) at 50 years of age in men and women was 8.0% and 15.8%, respectively. Direct costs of incident fractures in Greece in 2019 were €694.7 million, to which another €203.5 million should be added for the cost of long-term disability resulting from fractures that occurred before 2019. Additionally, the cost of pharmacological interventions was €80.5 million. Thus, total direct costs for 2019 (excluding the value of QALYs lost) amounted to €980 million.6 Due to this high burden, osteoporosis is considered a public health challenge in Greece. The healthcare system covers the cost of diagnosis and access to care, including pharmaceutical treatments. Additionally, updated clinical guidelines for the diagnosis and treatment of osteoporosis in Greece have been recently published by the Hellenic Society for the Study of Bone Metabolism (HSSBM),7 which have been endorsed by the Central Health Council and published by the Ministry of Health.8
This comprehensive policy framework has to date, to the best of our knowledge, not been assessed against evidence on the QoL or financial burden of patients with osteoporosis, including severe osteoporosis, which is the most resource-intensive type of osteoporosis, or their preference for specific treatment attributes. Therefore, evidence on current patient challenges or preferences in those with severe osteoporosis is lacking and further information is required in order to inform future healthcare decisions for the optimal management of severe osteoporosis in Greece.
This study aimed to elicit self-reported health status, quantify severe osteoporosis-related burden, and understand the preferences of postmenopausal women with severe osteoporosis for anabolic therapies in Greece. Anabolic therapies have the same reimbursement status in Greece and are excluded from any patient co-payment for severe osteoporosis (all other treatment options have an out-of-pocket co-payment rate of 25%). This removes any cost considerations from the preference analysis.
Methods
This was a descriptive, observational, cross-sectional study with a convenience sample. Data were collected through an online patient survey during a 2-month period, between May and July 2021.
Study Population and Procedures
The study sample consisted of postmenopausal women with severe osteoporosis, defined as those who reported having experienced at least one osteoporotic fracture and a formal diagnosis of a Dual-energy X-ray absorptiometry (DXA) T-score of ≤−2.5 at either lumbar spine and/or hip. Women who were neither postmenopausal nor suffering from self-reported severe osteoporosis, as defined above, were excluded from the study. All participants were members of, or associated with, the Greek Bone Health Association “Petalouda”. As sample size requirements are difficult to predict in patient preference studies,9 purposive sampling was used to select the study sample as it is a non-probability sampling method, in which participants are selected with a purpose (a criterion of selection) in mind.10 The study protocol and instrument were sent to and approved by the Board of Directors of “Petalouda”, who agreed to participate in the study. Subsequently, “Petalouda” sent an email to members/associated parties containing an invitation to participate, an informed consent form, information regarding the study and a link to the questionnaire. Based on current legislation regarding the General Data Protection Regulation (GDPR), “Petalouda” was not aware of the medical history of each member and/or friend, therefore the total number of eligible subjects was not known. Upon initiating the survey, participants were asked to self-declare whether they had severe osteoporosis, as defined above. Only patients with self-reported severe osteoporosis were allowed to proceed and participate in the survey.
Research Tool
The survey contained the following sections:
Participant Characteristics
This section recorded anonymized participant demographics (age, place of residence, educational level, and household composition) and source of income.
Patient Reported Health-Related Quality of Life (HR-QoL)
HR-QoL was recorded and measured via the QoL Questionnaire (QUALEFFO-41) instrument,11 as validated in Greek, and the Osteoporosis Quality of Life Questionnaire (OQLQ) instrument.12 QUALEFFO-41 was selected due to its disease-specific content, since it was developed by the European Foundation for Osteoporosis, and is validated in Greek. OQLQ was selected as it correlates well with generic measures and fractures and can detect health improvements or disabilities.13
Osteoporosis Management Paradigm and Burden
This section recorded participants’ current health status and disease burden, in terms of physical and mental health, and financial costs.
Importance of Treatment Attributes
Participants were asked to rate the importance of specific treatment attributes, namely efficacy, safety, mode of administration, and frequency of administration. Treatment attributes included in this section were selected based on a recent review of 26 studies reporting the values and preferences towards osteoporosis treatments of 15,348 women and were validated in the pilot study as described below.3
Risk-Benefit Trade off Table
The questionnaire was followed by a risk-benefit trade-off table (Table 1) to measure patients’ preferences between two unlabelled anabolic treatments for severe osteoporosis (teriparatide and romosozumab). The risk-benefit trade-off table structure followed the optimal decision support tool for postmenopausal osteoporotic women recently reported in Carrissa Abigail Roxas et al.14 The different considerations reported as important to patients in this study were efficacy, method and frequency of administration, side effects, and cost. Of those, our study did not evaluate the importance to patients of treatment cost, as social insurance in Greece covers 100% of the cost of both teriparatide and romosozumab. Treatment brand names or International Non-Proprietary Names (INNs) were not revealed in the trade-off table. Patients were provided with data for both options on each of the following parameters: BMD change at the hip, femoral neck and lumbar spine, fracture frequency within a 12-month treatment period, method and duration of treatment administration, incidence of adverse events, and incidence of serious adverse events. Participants were then asked to select a preference for one of the two scenarios. Data used in the trade-off table were derived from the STRUCTURE study.15 STRUCTURE was a randomized, Phase 3, open-label, active-controlled study run at 46 sites over a 12-month period in North America, Latin America, and Europe. Eligible patients were women aged between 55 and 90 years with postmenopausal osteoporosis who had taken an oral bisphosphonate for at least 3 years before screening and alendronate the year before screening, an areal BMD T score of −2.5*SD or lower at the total hip, femoral neck, or lumbar spine, and a history of fracture. Patients were randomly assigned (1:1) to receive subcutaneous romosozumab (210 mg once monthly) or subcutaneous teriparatide (20 μg once daily). The primary endpoint was percentage change from baseline in areal BMD by dual-energy x-ray absorptiometry at the total hip through Month 12 (mean of Months 6 and 12), using a linear mixed effects model for repeated measures which represented the mean treatment effect at Months 6 and 12. All randomized patients with a baseline measurement and at least one post-baseline measurement were included in the efficacy analysis. Data on adverse events (AEs) were also elicited from the STRUCTURE study.
 |
Table 1 Trade-off Table |
Pilot Study
The survey questionnaire was pre-tested with a Greek endocrinologist and two patient representatives of “Petalouda” to evaluate the suitability of the survey in answering the research question, the validity of content, clarity of language, and ease of understanding. Feedback was incorporated into the final survey questionnaire. Responses provided during this phase were excluded from the final sample and analysis.
Statistical Analysis
Cronbach’s alpha was calculated to assess internal consistency. Means and standard deviations (SD) were reported for continuous normally distributed variables. If non-normality was observed, medians were also reported. To evaluate the normality of the data, a Shapiro–Wilk test was performed along with graphical representation (QQ plot). An independent samples t-test was used to determine whether there was a statistically significant difference in patient characteristics between the means of the group that opted for treatment option 1 (romosozumab characteristics) vs the group that opted for treatment option 2 (teriparatide characteristics) in the risk-benefit trade off table (Table 1).
Results
A total of 350 invitations for the survey were sent via email and 283 (81%) women responded; of these, 186 (66%) completed the survey in full and were included in the analysis. Patient characteristics, osteoporosis disease history and current management, and osteoporosis burden are presented below and in Table 2.
 |
Table 2 Patient Sociodemographic Characteristics, Osteoporosis Disease History, Current Management and Burden |
Patient Characteristics
All participants were female, 72% were aged between 61 and 80 years, and 49% were living in an urban setting. There was a good distribution across all Greek provinces, with almost half (42%) of participants based in Attica, and 58% in the rest of Greece. Almost one third of survey respondents held a graduate or postgraduate degree. Approximately 40% of respondents were retired, 34% were housewives, and 22% were currently employed. Overall, 58% were married with children and 29% were widowed with children.
Osteoporosis Disease History and Current Management
The majority (69%) of participants reported being diagnosed with severe osteoporosis over the past 10 years, 20% over the past 11 to 20 years, and 11% were diagnosed more than 20 years ago. Vertebral fracture was the first osteoporotic fracture in 31% of participants, forearm fracture in 26%, ankle fracture in 22%, and hip fracture in 17%. Almost half (45.2%) of participants reported additional fractures since their first osteoporotic fracture. The majority (61%) of participants reported an average recovery time from the fracture, defined as the time taken to recover from the physical impact of fracture, of at least three months. In total, 81% of participants reported receiving some type of pharmaceutical treatment for their osteoporosis, beyond calcium and vitamin D.
Osteoporosis Burden
The majority (68%) of participants considered their general health to be below average for their age, 22% reported their general health as satisfactory or average, and only 10% considered their health to be good or very good. Almost three quarters (72%) of all study participants considered their overall QoL to be worse compared with 10 years ago, with 89% (119/134) attributing this deterioration to their osteoporosis. Of these participants, 60 (50%) had experienced a refracture since their first fracture.
HR-QoL: Pain and Discomfort
Most participants reported experiencing back pain at least 2–3 days per week, with only 7% reporting that they never experienced back pain. Participants also scored a mean of 3 (SD=1.21) on the pain/discomfort scale included in the QUALEFFO-41 questionnaire (where 1=extreme distress or discomfort and 6=no distress or discomfort).11 Approximately 38% of participants reported experiencing high levels of pain in general. Almost half (43%) of the participants experienced high levels of distress or discomfort due to pain from carrying things and due to pain from standing for long periods of time (44%).
HR-QoL: Mobility
On the mobility scale included in the QUALEFFO-41 questionnaire11 (where 1=only with help and 5=without difficulty), participants scored a mean of 2.83 (SD=1). Over half of the respondents (56%) reported experiencing high levels of difficulty (defined as a response of 1 or 2) when kneeling. A total of 50% reported experiencing high levels of difficulty when climbing stairs to the next floor of a house, while 40% reported difficulty walking 100 meters.
HR-QoL: Mental Health and Stress
On the mental health/stress scale included in the OQLQ questionnaire12 (where 1=all the time and 7=never), participants scored a mean of 3.46 (SD=1.41). The majority reported experiencing a very frequent fear of fractures and a very frequent fear of falling (65% and 66%, respectively). Approximately half of the participants were very angry about having an illness at a time of their life when they planned to enjoy themselves, and 48% reported feeling very frustrated.
Financial Burden
On average, 86% of participants spent at least €100 per month in personal or family costs related to their osteoporosis. The majority (84.4%) reported out of pocket costs for medication to manage their pain/discomfort and 63% reported paying for rehabilitation services (e.g., physiotherapy or gym classes). Almost 35% of participants reported paying out of pocket costs for hospitalization and/or other medical services, and approximately 25% reported paying for caring for their family and/or household. With respect to indirect costs due to missed workdays, the vast majority (95%) of respondents, who were employed, reported having missed work due to their osteoporosis; most of them once every 3 (40%) or 6 (33%) months, for multiple days on each occasion.
Preferences for Treatment Attributes
On a scale of 1=unimportant to 10=extremely important where 5=average, almost all participants (93%) ranked a decrease in the probability of sustaining a fracture at above average importance (mean=8.71, SD=1.67), followed by an increase in bone density (89% of participants, mean=8.31, SD=1.83), probability of severe adverse events (88% of participants, mean=8.13, SD=2.04), mode of administration (75% of participants, mean=7.24, SD=2.26), and frequency of administration (70.4% of participants, mean=6.83, SD=2.37) (Table 3). The majority (68%) of participants reported a preference for oral osteoporosis treatments, while 23% preferred subcutaneous treatment, and 5% preferred intravenous treatment administration. The remaining 4% of participants did not express an opinion on this matter or stated that they would follow their doctor’s recommendation. The majority (53%) preferred having their osteoporosis treatment administered once every 6 months or even less frequently. Around half of participants (58%) would consider their osteoporosis treatment to be effective if it led to a 50% reduction in future fracture risk, 10% would consider their osteoporosis treatment to be effective only if it led to an 80% reduction in risk, and almost 20% only if it led to at least a 90% reduction in risk. Furthermore, the vast majority (90%) of participants would consider their osteoporosis treatment to be effective if it led to an increase of at least 15% in their bone mineral density (BMD), almost half (57%) would consider treatment effective if it led to a 15–20% increase in BMD, and 33% only considered treatment to be effective if it led to at least a 20% increase in BMD. Almost all (94%) participants reported that their preference for an osteoporosis treatment was influenced by their knowledge of the probability of severe AEs.
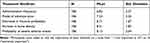 |
Table 3 Osteoporosis Treatment Attribute Mean Scores and Standard Deviation* |
Risk-Benefit Trade-off Table
Participants were asked to select one of two unlabeled options from the risk-benefit trade-off table (Table 1); treatment option one shared attributes with romosozumab, whereas treatment option two shared attributes with teriparatide. Overall, 70% opted for treatment option one. There were no statistically significant differences in levels of pain/discomfort, level of mobility, or financial burden between the group that selected treatment option one compared with those who selected treatment option two. Patients who selected treatment option one experienced a fear of fractures more frequently (mean=3.09, SE=0.11) than those who chose treatment option two (mean=3.50, SE=0.18), t(184)=−2.02, p <0.05. Additionally, respondents who selected treatment option one experienced a fear of falling more frequently (mean=3.08, SE=0.12) than those who chose option two (mean =3.55, SE=0.19), t(184)=−2.18, p <0.05.
Participants who opted for treatment option one rated a decrease in fracture probability as more important (mean=8.88, SE=0.14) than those who selected option two (mean=8.32, SE=0.24), t(184)=2.10, p <0.05. Similarly, patients who chose treatment option one rated the probability of severe AEs as a more important treatment attribute (mean=8.45, SE=0.17), compared with those who chose treatment option two (mean=7.39, SE=0.29), t(184)=3.32, p <0.01.
Discussion
This is the first study assessing self-reported quality of life and perceived disease burden amongst postmenopausal women with severe osteoporosis in Greece. Study participants largely reported a below average QoL, with the vast majority attributing this to their osteoporosis. Respondents in this study consistently reported pain and discomfort, mobility issues and mental health/distress challenges, all related to the presence of osteoporosis.
These findings on impaired HR-QoL confirm previous findings from other studies. A study by de Oliveira Ferreira et al reported that women with osteoporosis experienced impaired QoL, as assessed with the QUALEFFO-41 and the SF-36 scales in all domains studied, but especially relating to the physical, psychological, and social domains.16 Other work by Cohen-Solal and de Vernejoul reported the long-term physical, psychological, and social consequences of osteoporosis that affect QoL, impair social and leisure activities, and potentially alter emotional status to the extent of causing depression amongst patients with osteoporosis.17 Finally, hip and vertebral fractures in osteoporotic women have been shown to impact quality adjusted life years (QALYs) by Tosteson et al.18 Their study reported mean QALY values, where 1=perfect health and 0=death, of 0.82 (95% CI: 0.76, 0.87) among 114 women with one or more vertebral fracture and 0.63 (95% CI: 0.52, 0.74) among 67 women with hip fracture compared with 0.91 (95% CI: 0.88, 0.94) among 201 women without fracture.
Our study indicates that postmenopausal women with severe osteoporosis in Greece are burdened with substantial disease-related out of pocket costs of at least €100 per month, primarily for medication to manage pain, rehabilitation, and other medical services. This finding is in line with previously reported data on out-of-pocket payments in Greece, a country with one of the highest private healthcare expenditures. Giannouchos et al reported informal healthcare payments (median=€150) in more than half (63%) of all healthcare incidents (n=3494 healthcare incidents were reported by 3183 household representatives) in a sample of the general population in 2016–2017.19 In another study conducted in Australia, which evaluated out-of-pocket expenses for women with osteoporosis, participants had a mean of 6.8 consultations with healthcare practitioners for their osteoporosis in the previous 12 months, and 46% of participants used three or more types of complementary medicine products/practices in the same period. Overall, participants incurred an arithmetic mean of AU$594 (median=$350; inter-quartile range=$450) in out-of-pocket expenditure for healthcare use over the 12-month period.20
Additionally, in our study, severe osteoporosis appeared to impact on participants’ ability to work, with 40% of employed respondents reporting having missed work due to their osteoporosis once every 3 months, 32.5% once every 6 months and 12.5% at least once every 2 months. Fragility fractures have previously been associated with indirect costs attributable to absenteeism from paid or unpaid/voluntary work following a fracture; in a Dutch study of 116 patients who prospectively completed cost diaries every 3 months for 1 year after a hip fracture, absenteeism, both for paid and voluntary work, accounted for half of the total costs of fracture.21
Our study indicates that patients with severe osteoporosis place the greatest importance on treatment efficacy and safety, followed by mode and frequency of administration. These findings are in line with a recent review of 26 studies reporting the values and preferences regarding osteoporosis treatments of 15,348 women (mean age=66 years).3 This review revealed that women valued both effectiveness and adverse events, followed by convenience of taking the medication and its effect on daily routine (less frequent dosing was preferred, and administration by injection was preferred over oral administration if given less frequently). Key attributes evaluated in our study are also confirmed by another recent review of patient preferences and satisfaction with osteoporosis treatment.22 Our results relating to treatment attribute preferences appear to be in line with a recent discrete choice experiment among 188 patients with osteoporosis in the Netherlands.23 Though different in methodology, the hypothetical treatment options in this study were also characterized by three attributes: treatment efficacy, side effects, and mode/frequency of administration.
Another discrete choice experiment conducted in Belgium, France, Ireland, the Netherlands, Spain, Switzerland, and the UK asked participants to choose repeatedly between two hypothetical unlabeled drug treatments (and an opt-out option) that varied with respect to four attributes: efficacy in reducing the risk of fracture, type of potential common side effects, and mode and frequency of administration.24 In all countries, patients preferred treatments with higher effectiveness, and 6-monthly subcutaneous injection was always preferred over weekly oral tablets. These findings, i.e., a greater importance placed on effectiveness and a preference for less frequent dosing, are in line with our results.
Our findings of a preference for less frequent dosing are also confirmed in a review by Hiligsmann et al.25 This review underlined variations in the preferences of patients in most studies, highlighting the importance of considering individual preference in decision making to improve osteoporosis care. Finally, when participants in this study were asked to select their preferred treatment scenario between two unlabeled anabolic treatments, 70% opted for the scenario that shared treatment characteristics with romosozumab over a scenario that shared treatment characteristics with teriparatide.
This is, to the best of our knowledge, the first patient preference survey using a risk-benefit trade-off table to compare characteristics of unlabeled treatment scenarios between anabolic therapies in severe osteoporosis.
Limitations
Although this study followed good research practices and was designed and conducted by experienced clinicians and researchers, some limitations are to be considered in the interpretation of the results. This study was conducted via e-mail, therefore patients without an email address registered to “Petalouda” would not have received an invitation to complete the questionnaire. This may have introduced sampling bias and generalizability limitations, as patients lacking access to the internet or with limited computer skills are unlikely to have been able to participate. Furthermore, patients were included in the study based on their self-reported status of severe osteoporosis. QoL and disease severity were also self-reported in the context of osteoporosis alone, disallowing for any additional comorbidities, including COVID-19, which may have had an impact on overall patient QoL at the time of the study. The characteristics of both treatments were based on a single trial (STRUCTURE), which may not fully represent the totality of clinical evidence available for both treatments as differently selected treatment characteristics could have led to varying preference outcomes. Finally, despite patient preference research being widely used, it has the inherent limitation that respondents are stating their hypothetical preferences, which may differ from their preferences in real-life treatment decision-making.26
Conclusion
Our study evaluated the burden of severe osteoporosis on self-reported QoL of postmenopausal women in Greece and elicited patient preferences for treatment attributes. Patients valued treatment efficacy, measured through reduction in future fractures and increase in bone density, and safety, as key treatment attributes. When asked to select their preferred treatment scenario between two unlabeled anabolic treatments, 70% opted for the scenario that shared treatment characteristics with romosozumab over a scenario that shared treatment characteristics with teriparatide. This is the first study in Greece to report QoL, financial burden, and preferences for treatment attributes of postmenopausal women with severe osteoporosis. This study may help to inform future treatment protocols and prescription guidelines to further optimize osteoporosis treatment outcomes.
Data Sharing Statement
The authors are committed to sharing the full survey with qualified external researchers. The requests are to be made to the corresponding author and will be appraised based on scientific merit.
Ethics Approval and Consent to Participate
The study was approved by the Ethics Committee of the Health Policy Institute, Maroussi, Greece, and was conducted in line with the ethical standards set by the Declaration of Helsinki. Participation was voluntary, anonymized, and informed consent was requested and obtained from all participants.
Funding
This work was funded by UCB Pharma and Amgen Inc.
Disclosure
K Souliotis has received advisory boards’ fees from Boehringer Ingelheim, Βristol Myers Squibb and Pfizer; research grants from Sanofi and Roche outside the submitted work. C Golna, C Poimenidou, T Drakopoulou, M Tsekoura report no potential conflicts of interest for this work. D Willems and V Kountouris are employees and shareholders of UCB Pharma. P Makras has received lecture fees/advisory boards from Amgen, ELPEN, Farmaserv, Galenica, Genesis, Lilly, Pfizer, Rapharm, Takeda, UCB Pharma, UniPharma, and VIANEX; research grant from Amgen. The authors report no other conflicts of interest in this work.
References
1. Cauley JA. The global burden of fractures. Lancet Healthy Longevity. 2021;2:e535. doi:10.1016/S2666-7568(21)00183-5
2. Kanis JA, Norton N, Harvey NC, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos. 2021;16(1):82. PMID: 34080059; PMCID: PMC8172408. doi:10.1007/s11657-020-00871-9
3. Barrionuevo P, Gionfriddo MR, Castaneda-Guarderas A, et al. Women’s values and preferences regarding osteoporosis treatments: a systematic review. J Clin Endocrinol Metab. 2019;104(5):1631–1636. PMID: 30907968; PMCID: PMC7296202. doi:10.1210/jc.2019-00193
4. de Wit M, Cooper C, Tugwell P, et al. Practical guidance for engaging patients in health research, treatment guidelines and regulatory processes: results of an expert group meeting organized by the World Health Organization (WHO) and the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Aging Clin Exp Res. 2019;31(7):905–915. PMID: 30993659; PMCID: PMC6589151. doi:10.1007/s40520-019-01193-8
5. Sale JEM, Marwah A, Naeem F, Yu W, Meadows L. Evidence of patient beliefs, values, and preferences is not provided in osteoporosis clinical practice guidelines. Osteoporos Int. 2019;30(7):1325–1337. PMID: 30859238. doi:10.1007/s00198-019-04913-y
6. Willers C, Norton N, Harvey NC, et al. SCOPE review panel of the IOF. Osteoporosis in Europe: a compendium of country-specific reports. Arch Osteoporos. 2022;17(1):23. PMID: 35079919; PMCID: PMC8789736. doi:10.1007/s11657-021-00969-8
7. Makras P, Anastasilakis AD, Antypas G, et al. The 2018 Guidelines for the diagnosis and treatment of osteoporosis in Greece. Arch Osteoporos. 2019;14(1):39. PMID: 30877479. doi:10.1007/s11657-019-0584-3
8. Ministry of Health, Clinical guidelines for the diagnosis and management of osteoporosis; 2020. Available from: https://www.moh.gov.gr/articles/kentriko-symboylio-ygeias-ndash-kesy/kateythynthries-odhgies/8208-kateythynthries-odhgies-diagnwshs-kai-therapeias-ths-osteoporwshs-2020.
9. Lepkowski JM. Sampling the difficult-to-sample. J Nutr. 1991;121(3):416–423. PMID: 2002412. doi:10.1093/jn/121.3.416
10. Lancsar E, Louviere J. Conducting discrete choice experiments to inform healthcare decision making: a user’s guide. Pharmacoeconomics. 2008;26(8):661–677. doi:10.2165/00019053-200826080-00004
11. International Osteoporosis Foundation, Quality of Life Questionnaire (Qualeffo-41), Greek. Available from: https://www.osteoporosis.foundation/sites/iofbonehealth/files/2020-01/IOF-Qualeffo41-questionnaire-Greece.pdf.
12. Osteoporosis Quality of Life Study Group. Measuring quality of life in women with osteoporosis. Osteoporos Int. 1997;7(5):478–487. PMID: 9425507. doi:10.1007/PL00004151
13. Madureira MM, Ciconelli RM, Pereira RM. Quality of life measurements in patients with osteoporosis and fractures. Clinics. 2012;67(11):1315–1320. PMID: 23184210; PMCID: PMC3488992. doi:10.6061/clinics/2012(11)16
14. Carrissa Abigail Roxas M, Jimeno C, Palileo-Villanueva L, Macalalad-Josue AA, Sandoval MA, Fernandez JA. Development of a patient decision aid for the treatment of osteoporosis among Filipino postmenopausal women. J ASEAN Fed Endocr Soc. 2020;35(1):93–101. PMID: 33442174; PMCID: PMC7784105. doi:10.15605/jafes.035.01.15
15. Langdahl BL, Libanati C, Crittenden DB, et al. Romosozumab (sclerostin monoclonal antibody) versus teriparatide in postmenopausal women with osteoporosis transitioning from oral bisphosphonate therapy: a randomised, open-label, phase 3 trial. Lancet. 2017;390(10102):1585–1594. PMID: 28755782. doi:10.1016/S0140-6736(17)31613-6
16. de Oliveira Ferreira N, Arthuso M, da Silva R, Pedro AO, Pinto Neto AM, Costa-Paiva L. Quality of life in women with postmenopausal osteoporosis: correlation between QUALEFFO 41 and SF-36. Maturitas. 2009;62(1):85–90. PMID: 19100693. doi:10.1016/j.maturitas.2008.10.012
17. Cohen-Solal ME, de Vernejoul M-C. Quality of life in osteoporosis. Medicographia. 2002;24(4):349–352.
18. Tosteson AN, Gabriel SE, Grove MR, Moncur MM, Kneeland TS, Melton LJ. Impact of Hip and vertebral fractures on quality-adjusted life years. Osteoporos Int. 2001;12(12):1042–1049. PMID: 1184633. doi:10.1007/s001980170015
19. Giannouchos TV, Vozikis A, Koufopoulou P, Fawkes L, Souliotis K. Informal out-of-pocket payments for healthcare services in Greece. Health Policy. 2020;124(7):758–764. PMID: 32475739. doi:10.1016/j.healthpol.2020.04.005
20. Adams J, Bayes J, Hosseini M, Sibbritt D. Annual out-of-pocket expenditure associated with healthcare use among Australian older women with osteoporosis: a cross-sectional study. Arch Osteoporos. 2021;16(1):148. PMID: 34606032. doi:10.1007/s11657-021-01021-5
21. Eekman DA, van Helden SH, Huisman AM, et al. Optimizing fracture prevention: the fracture liaison service, an observational study. Osteoporos Int. 2014;25(2):701–709. PMID: 24030287. doi:10.1007/s00198-013-2481-8
22. Canals-Ruiz L, Comellas M, Lizán L. Preferences, satisfaction and decision-making processes in osteoporosis treatment: a systematic review of the literature. J Comp Eff Res. 2021;10(8):629–645. PMID: 33880940. doi:10.2217/cer-2020-0216
23. Cornelissen D, Boonen A, Bours S, Evers S, Dirksen C, Hiligsmann M. Understanding patients’ preferences for osteoporosis treatment: the impact of patients’ characteristics on subgroups and latent classes. Osteoporos Int. 2020;31(1):85–96. PMID: 31606825; PMCID: PMC6946725. doi:10.1007/s00198-019-05154-9
24. Hiligsmann M, Dellaert BG, Dirksen CD, et al. Patients’ preferences for anti-osteoporosis drug treatment: a cross-European discrete choice experiment. Rheumatology. 2017;56(7):1167–1176. PMID: 28398547; PMCID: PMC5563450. doi:10.1093/rheumatology/kex071
25. Hiligsmann M, Bours SP, Boonen A. A review of patient preferences for osteoporosis drug treatment. Curr Rheumatol Rep. 2015;17(9):61. PMID: 26286178; PMCID: PMC4540772. doi:10.1007/s11926-015-0533-0
26. Laba TL, Brien JA, Fransen M, Jan S. Patient preferences for adherence to treatment for osteoarthritis: the Medication Decisions in Osteoarthritis Study (MEDOS). BMC Musculoskelet Disord. 2013;14:160. doi:10.1186/1471-2474-14-160
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
