Back to Journals » Pharmacogenomics and Personalized Medicine » Volume 16
Association Between CTSK Gene Polymorphisms and Response to Alendronate Treatment in Postmenopausal Chinese Women with Low Bone Mineral Density
Authors Yuan H, Wang C, Liu L, Wang C, Zhang Z, Qu S
Received 30 June 2023
Accepted for publication 16 October 2023
Published 28 October 2023 Volume 2023:16 Pages 925—932
DOI https://doi.org/10.2147/PGPM.S425357
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Hu Yuan,1,* Caihong Wang,2,* Li Liu,3 Chun Wang,3 Zhenlin Zhang,3 Shen Qu4
1Department of Endocrinology, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, Gusu School, Nanjing Medical University, Suzhou, 215001, People’s Republic of China; 2Department of Cardiology, The Affiliated Suzhou Hospital of Nanjing Medical University, Suzhou Municipal Hospital, Gusu School, Nanjing Medical University, Suzhou, 215001, People’s Republic of China; 3Shanghai Clinical Research Center of Bone Disease, Department of Osteoporosis and Bone Disease, Shanghai Jiaotong University Affiliated Sixth People’s Hospital, Shanghai, 200233, People’s Republic of China; 4Department of Endocrinology and Metabolism, Shanghai Tenth People’s Hospital, Clinical Medical College of Nanjing Medical University, Shanghai, 200072, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Zhenlin Zhang; Shen Qu, Email [email protected]; [email protected]
Purpose: The aim of this study was to explore the association between CTSK polymorphisms and the response to alendronate treatment in postmenopausal Chinese women with low bone mineral density.
Patients and Methods: In this study, 460 postmenopausal women from Shanghai were included. All of them were treated with weekly oral alendronate 70 mg, daily calcium 600 mg and vitamin D 125 IU for a year. Four tag single nucleotide polymorphisms (SNPs) in CTSK gene were genotyped. Bone mineral densities of lumbar spine (L1-L4), femoral neck and total hip were measured at baseline and after 12 months of treatment, respectively.
Results: After 1-year of treatment, there was no significant differences in BMI between baseline and follow-up. After alendronate treatment, the BMD of L1– 4, femoral neck and total hip all increased significantly (all P < 0.001), with average increases of 4.33 ± 6.42%, 1.85 ± 4.20%, and 2.36 ± 3.79%, respectively. There was no significant difference in BMD at L1-L4, the femoral neck and total hip between different genotype groups at baseline (P> 0.05). After 1-year treatment with alendronate, rs12746973 and rs10847 were associated with the % change of BMD at L1-L4 (P=0.038) and % change of BMD at femoral neck (P=0.038), respectively. Furthermore, rs10847 was associated with BMD response at femoral neck (P=0.013). However, the associations were not significant after Bonferroni correction.
Conclusion: We concluded that the common variations of CTSK gene were potentially associated with the therapeutic response to alendronate treatment in Chinese women with low bone mineral density. However, further validation is needed.
Keywords: CTSK gene, alendronate, postmenopausal, low bone mineral density, osteoporosis
Introduction
Osteoporosis is a complex disease characterized by reduction of bone mass and strength, destruction of bone microstructure, increase in bone brittleness and susceptibility to fractures. It is generally believed to be caused by genetic and environmental factors. It tends to occur in postmenopausal and older women. A minor trauma or daily activities can lead to fracture of hip, vertebral body, distal radius and proximal humerus, which is called fragility fracture.1 The hip fracture is the most important cause of disability and death in the elderly, and the disability rate within a year is 50% and the mortality rate is 20%. In China, the elderly population over 60 years has exceeded 210 million and the population over 65 years is nearly 140 million, making China the country with the largest elderly population in the world.2
Early diagnosis and effective treatment of osteoporosis, improving bone density and quality, thereby reducing the risk of fracture, are critical for the prevention and treatment of osteoporotic fractures. There are three types of drugs to treat osteoporosis. The first inhibits osteoclast function and reduces bone resorption. The second promotes the function of osteoblasts and increases bone formation. The third promotes bone formation and inhibits bone absorption.3 The World Health Organization (WHO) and national guidelines recommend bisphosphonate, a drug that belongs to the first type, for the prevention and treatment of osteoporosis and alendronate is most commonly used. Many trials have suggested that treatment with 70 mg of alendronate weekly for at least one year can reduce bone resorption markers by 50% and increase bone mineral density (BMD) in lumbar spine and hip by 5–8% and 3–5%, respectively.4–7 However, the efficacy and safety of alendronate vary greatly among individuals, with about 5–10% of patients having poor efficacy, no response, or even adverse reactions.4–7
The differences in the responses to alendronate may be related to differences in genetic background between individuals. Some scholars have detected the coding genes of seven key enzymes in the mevalonate pathway, including Mevalonate kinase (MK), Phosphomevalonate kinase (PMVK), Mevalonate decarboxylase (MVD), Isopentenyl pyrophosphate isomerase (IPI), Geranylgeranyl pyrophosphate synthase 1 (GGPS1), Farnesyl pyrophosphate synthase (FDPS) and Farnesyl-Diphosphate Farnesyltransferase 1 (FDFT1), and three genes of OPG/RANKL/RANK system, a total of 67 tag SNPs, and found that the response to alendronate is significantly associated with the patient’s genetic background.6–11 Some enzymes in other pathways of bone metabolism also showed high correlation, such as SOST.6
Cathepsins are lysosomal cysteine proteases and papain family members. There are 11 different types of cathepsins (B, C, F, H, K, L, O, S and W, V, X). Cathepsin K (CTSK) is highly expressed in osteoclasts, and is the key bone resorption protease. It is most active in degrading collagen, including collagen type I and collagen type II.12–14 Osteoporosis and some other diseases of the bones are associated with genetic changes in CTSK.14–16 Seven genes encoding CTSK were found to be mutated in eight families with pycnodysostosis.17–19 These mutations can inhibit the degradation of collagen type I so as to increase BMD. In animal studies, mice with deficiency of the CTSK gene presented with osteosclerosis.14,20
Alendronate is a representative drug for bone resorption. Whether its variance in therapeutic effect is associated with the polymorphisms of the CTSK gene is uncertain. Our aim was to study the allelic association of CTSK polymorphisms and the response to alendronate treatment in postmenopausal Chinese women with low BMD. This study provides an important basis for the implementation of individualized drug regimen according to different genotypes, so as to achieve the best curative effect for osteoporosis patients, improve the safety and effectiveness of individual drug regimen, which can achieve the therapeutic purpose and also save resources, and has great clinical and social significance.
Materials and Methods
Subjects
All participants were recruited by the department of Osteoporosis and Bone Disease in Shanghai Jiaotong University Affiliated Sixth People’s Hospital. A total of 460 women were enrolled in this study. All study subjects were postmenopausal women (Han nationality), aged 45–80 years, from Shanghai, with natural menopause for at least one year. All subjects were followed up once a month and assigned drugs. The procedures used during the study were in accordance with the guidelines of the Helsinki Declaration for human studies. This study was approved by the Ethics Committee of the Shanghai Jiao Tong University affiliated to Sixth People’s Hospital. All study participants provided written informed consent.
Inclusion and Exclusion Criteria
Criteria for inclusion (meeting either of the below criteria): (1) Lumbar spine 1–4 or femoral neck or total hip BMD lower than the peak BMD of young women 2.5SD; (2) brittle fracture (fractures from minor trauma).
Criteria for exclusion: (1) other metabolic or inherited bone mineral diseases such as hypoparathyroidism, hyperparathyroidism, deformans osteitis, osteogenesis imperfecta, osteomalacia; (2) Cushing’s syndrome, hyperthyroidism, diabetes mellitus; (3) chronic liver disease, chronic obstructive pulmonary disease and chronic kidney disease with blood creatinine >177 mol/L; (4) Rheumatoid arthritis or took steroids or anticonvulsant for >6 months or other drugs affecting bone metabolism; (5) suffered from gastric ulcer, Crohn’s disease and chronic dysentery in recent two years; (6) non-hereditary nerve or muscle disease affecting BMD; (7) sequelae of heart or brain disease affecting limb movements; (8) fracture of non-brittle fracture sites (nose, toes, skull, mandible and phalanges) and fracture resulting from severe trauma; (9) all malignancies; (10) bilateral oophorectomy before 45 years of age; (11) menopause before 40 years of age; (12) brittle fracture with no accurate medical history and X-ray image; (13) previous treatment with calcium, vitamin D, active vitamin D, bisphosphonate, sodium fluoride, calcitonin, sodium fluoride, a selective estrogen receptor modulator, strontium ranelate, or the recombinant form of PTH or current use of hormone replacement therapy; (14) Active gastric or duodenal ulcer, reflux esophagitis or any other disease contraindicated for alendronate use; (15) unable to stand or sit for half an hour; (16) BMI <18 kg/m2 or >30 kg/m2; (17) hypocalcemia (serum calcium (Ca) < 2.08 mmol/l) or hypophosphatemia 130 (serum phosphorus (P) < 0.80 mmol/l); (18) increased serum parathyroid hormone (PTH) levels (normal values: 15–65 pg/mL); (19) inability to understand and follow-up regularly.
Drug Treatment and Observation in Study Subjects
A total of 460 participants were treated with alendronate (Fosamax, 70 mg/tablet, produced by MSD Hangzhou) one tablet per week and Caltrate D (contains 600 mg of calcium and 125 IU of vitamin D, produced by Pfizer) one tablet daily for one year. The participants were followed-up once every three months and their basic information including height, weight, diet (daily intake of calcium and vitamin D), smoking, alcohol intake, activity volume, fall history, adverse reactions to drugs, fracture and comorbid diseases were recorded.
BMD Measurements
Lunar prodigy dual-energy X-ray absorptiometry (DXA) densitometer (GE Healthcare, Madison, WI, USA) was used to measure the BMD and size of lumbar spine1-4 (L1-4), proximal part of the femur including the total hip, femoral neck, trochanter and inter-trochanter at baseline and after one year of treatment. BMD was expressed as g/cm2 and bone size was expressed as cm2. The machine was calibrated daily, and the coefficient of variability values of the dual energy X-ray absorptiometry measurements (obtained from triplicate measurements of the same 15 individuals) at L1-4, the total hip and the femoral neck were 1.39%, 0.70% and 2.22%, respectively.21 The long-term reproducibility of the DXA instrument during the trial based on weekly repeated phantom measurements was 99.55%. The least significant change in BMD at L1-4, total hip and femoral neck were 3.85%, 1.94% and 6.15%.21 Weight and height were measured using a calibrated balance beam scale and a calibrated stadiometer. The BMI was defined as weight/height2 in kg/m2.
Genomic DNA Extraction and SNP Testing
Four tag SNPs in CTSK gene (rs12085336, rs12746973, rs4379678 and rs10847) were selected from dbSNP (http://www.ncbi.nlm.nih.gov/snp/) and HapMap (http://hapmap.ncbi.nlm.nih.gov/). All of them were chosen based on the following criteria: (1) minor allele frequency (MAF) > 0.05 and (2) pairwise linkage disequilibrium (LD) exceeding the threshold of 0.8 (r2 > 0.8).
Briefly, 2 mL of peripheral blood was collected from the selected subjects, and genomic DNA was extracted using an automatic genomic DNA instrument. After extraction, the DNA content was determined, and then stored at −80 degrees after unified numbering. All the SNP sites in this study were detected by fluorescence quantitative PCR using the TaqMan probe’s 5’ nucleotide SNP detection technology. Real-time quantitative PCR was performed on Mx 3000P type instrument (Stratagene, USA), and the primers and probes were designed using Primer Express software and TaqMan® SNP genotyping design (Applied Biosystems, CA, USA) provided by ABI.
Statistical Analyses
Multivariate regression method and the nonparametric test were used to analyze the relationship of BMD and bone conversion between the haploid type with the baseline and after one year treatment. Non-parametric tests (chi-square test, etc.) were used to analyze the therapeutic effect. The primary outcome was the change in BMD in the lumbar spine, hips and femoral neck. Another outcome, the response to treatment, was also observed and the least significant change (LSC) was used to define response, as per the standards and guidelines22 established by ISCD 2007 Adult and Pediatric Official Positions.
Hardy-Weinberg equilibrium (HWE) was tested for each SNP. The linkage disequilibrium (LD) coefficient r2 among all pairs of biallelic loci was tested using Haploview (version 4.2; www.broad.mit.edu/mpg/hapview/). Clinical data were expressed as the mean ± SD for continuous variables with symmetrical distributions.
Linear regression analysis was used to test the effects of the qualified SNPs on % change in BMD under the additive genetic model using PLINK (http://pngu.mgh.harvard.edu/~purcell/plink/), with adjustment for age and BMI. While for the therapeutic response to alendronate treatment, the association analysis was performed with multi-variable logistic regression models. Odds ratios (ORs) and 95% confidence intervals (CIs) were estimated by using the demographic characteristics, including age and BMI, as covariates. P-values less than 0.05 were defined as nominal significance, P-value less than 0.0125 were defined as Bonferroni-corrected significance (0.05/4).
Results
Characteristics of the Study Subjects
A total of 460 subjects were included and completed the evaluation of biochemical and BMD measurements at baseline and after 1-year treatment, respectively.
At baseline, mean age was 63.55 ± 12.2 years, mean BMI was 22.81 ± 3.03 kg/m2 and mean BMD of L1-4, the femoral neck, total hip was 0.804 ± 0.197 g/cm2, 0.687 ± 0.103 g/cm2 and 0.725 ± 0.11 g/cm2. After 1-year of treatment, mean BMI was 22.89 ± 3.05 kg/m2 and mean BMD of L1-4, the femoral neck, total hip was 0.858 ± 0.150 g/cm2, 0.701 ± 0.103 g/cm2 and 0.749 ± 0.133 g/cm2. After 1-year of treatment, there was no significant differences in BMI between baseline and follow-up. After alendronate treatment, the BMD of L1-4, femoral neck and total hip all increased significantly (all P < 0.001), with average increases of 4.33 ± 6.42%, 1.85 ± 4.20%, and 2.36 ± 3.79%, respectively (Table 1).
 |
Table 1 Characteristic Changes of 460 Postmenopausal Women in This Study |
Allele Frequencies and Haplotype Structures
Four tag SNPs in CTSK gene were genotyped in all participants. All tag SNPs were successfully genotyped. In the study, the population distribution of rs12085336 deviated from HWE (P < 0.05) and were excluded from further analysis. The other 3 SNPs (rs12746973, rs4379678 and rs10847) were compatible with HWE (Table 2). There was no haplotype block constructed from the four SNPs after linkage disequilibrium (LD) analysis.
 |
Table 2 Information on the 4 SNPs of CTSK Gene in the Study |
Association Between SNPs and the Therapeutic Response to Alendronate Treatment
There was no significant difference in BMD at L1-L4, the femoral neck and total hip between different genotype groups at baseline (P>0.05). After 1-year treatment with alendronate, the results showed that rs12746973 was associated with the % change of BMD at L1-L4 (P=0.038); and rs10847 was associated with the % change of BMD at femoral neck (P=0.038). However, the associations were not significant after Bonferroni correction (P>0.0125) (Table 3).
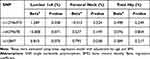 |
Table 3 The Association Between 3 SNPs of CTSK Gene and the % Change in BMD |
In order to estimate the efficacy of treatment, we divided all participants into the responders group and the non-responders group according to the least significant change (LSC) in BMD (the standards and guidelines21 established by ISCD 2007 Adult and Pediatric Official Positions). Only rs10847 showed association with the BMD response at femoral neck (P=0.013), but this association was not significant (P>0.0125) after Bonferroni correction (Table 4).
 |
Table 4 The Association Between 3 SNPs of CTSK Gene and BMD Response |
Discussion
Alendronate is one of the first-line anti-resorption drugs commonly used in postmenopausal patients with osteoporosis or bone defects, which can increase BMD and reduce the risk of brittle fractures.23 However, the response to anti-osteoporosis treatment, including alendronate, is different in different individuals, and is known to be associated with genetic differences. Genetic polymorphisms in the mevalonate pathway are associated with the different responses.8 Wang et al24 also found that polymorphisms of SOST gene were associated with the response to alendronate.
CTSK, encoded by cathepsin K gene (CTSK), is a protein composed of 329 amino acids, including three parts: amino terminus region composed of 15 amino acids, pro-peptide consisting of 99 amino acids, and catalytic unit composed of 215 amino acids.25 In stationary osteoclasts far from the bone resorption lacunae, CTSK was present as an inactive proenzyme. In the acidic environment, the enzyme was activated after the n-terminal signal peptide was lysed. In the activated osteoclasts, the high level of activase polarization cell fold edge was fused with lysosomal sac and CTSK was released into the extracellular space. In the bone pit, acidic environment is formed by the CLCN7 and TCIRG1, and the pH value is less than 4.5. CTSK can degrade collagen I and II in the acidic environment, especially type I collagen. Because of the important role of CTSK in bone resorption, it has become an important target for the development of drugs to treat osteoporosis.26,27
Many studies have investigated the relationship between CTSK and bisphosphonate in postmenopausal women with osteoporosis. Meier et al28 found that serum Cathepsin K was significantly elevated in postmenopausal women with osteoporosis and decreased after the patients were treated with bisphosphonates. Jahn et al29 also found that the levels of Cathepsin K were significantly reduced after three to six months treatment with zoledronic acid (P < 0.05), and the level returned to baseline after one year. Recent study has shown that nitrogen-containing bisphosphonates downregulate CTSK in osteoclasts cultured in vitro.30
As far as we know, this is the first research reported a population-based association analysis of CTSK gene polymorphism and response to alendronate treatment in postmenopausal Chinese women. In this study, we investigated the CTSK gene as a candidate gene to explore the relationship between genetic factors and therapeutic response to alendronate. There was no association between SNP and BMD at baseline. Gao et al31 also found no significant relationship between serum cathepsin K and age, BMI, BMD or bone metabolic markers (all P > 0.05) after adjustment for age and BMI. After 12-months treatment with alendronate, the BMD at L1-L4, total hip and femoral neck was measured and large difference in the % change in BMD among all participants was observed as expected. Then, the association between % change in BMD and four SNPs was analyzed. There were correlations between rs12746973 and the % change of BMD at L1-L4, rs10847 and the % change of BMD at femoral neck. However, after Bonferroni correction, the correlation was not significant.
Furthermore, we examined BMD response as the % change cannot depict the therapeutic effect. According to the standards and guidelines14 established by ISCD 2007 Adult and Pediatric Official Positions, we analyzed the LSC to eliminate the error effect. All subjects were divided into the responders group and the non-responders group depending on the LSC at L1-4, total hip and femoral neck. Only rs10847 at femoral neck appeared more frequently in responders, but this association disappeared after Bonferroni correction. Hence, it was concluded that there was no association between CTSK gene polymorphisms and response to alendronate treatment in postmenopausal Chinese women with low BMD. Maybe it was due to the inadequate sample size. And it is necessary to confirm the relationship between SNP variations and efficacy of alendronate therapy by expanding samples size.
The present study also had some limitations. First, bone turnover markers were not considered, which is a sensitive index to evaluate the therapeutic effect.32 Second, the participants were only followed-up for one year, which is a short period for treating low BMD. Measuring more indices to reflect the improvement of bone metabolism and longer follow-up durations may be necessary to demonstrate the interaction between genotype and treatment in future studies.
Conclusion
In summary, genetic background is considered to be important for individualized anti-reabsorption therapy. This study provided some evidence that the common variation variants of CTSK gene were potentially associated with does not contribute to the therapeutic response to alendronate treatment in Chinese women with low bone mineral density. However, further validation is needed.
Acknowledgments
This study was supported by the National Key Research and Development Program of China (2018YFA0800801), National Natural Science Foundation of China (NSFC) (81974123 and 81770871).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Gao C, Xu Y, Li L, et al. Prevalence of osteoporotic vertebral fracture among community-dwelling elderly in Shanghai. Chin Med J. 2019;132(14):1749–1751. doi:10.1097/CM9.0000000000000332
2. National Bureau of Statistics of China. China Statistical Yearbook. China Statistics Press; 2015.
3. The Chinese Medical Association of Osteoporosis and Bone Mineral Disease. Guidelines for the diagnosis and management of primary osteoporosis (2017). Chin J Osteoporos Bone Miner Res. 2019;25(3):281–309.
4. Cremers S, Drake MT, Ebetino FH, Bilezikian JP, Russell RGG. Pharmacology of bisphosphonates. Br J Clin Pharmacol. 2019;85(6):1052–1062. doi:10.1111/bcp.13867
5. Haider IT, Simonian N, Saini AS, Leung FM, Edwards WB, Schnitzer TJ. Open-label clinical trial of alendronate after teriparatide therapy in people with spinal cord injury and low bone mineral density. Spinal Cord. 2019;57(10):832–842. doi:10.1038/s41393-019-0303-3
6. Li M, Zhang Z, Xue Q, et al. Efficacy of generic teriparatide and alendronate in Chinese postmenopausal women with osteoporosis: a prospective study. Arch Osteoporos. 2022;17(1):103. doi:10.1007/s11657-022-01131-8
7. Calvo-Gallego JL, Pivonka P, Ruiz-Lozano R, Martínez-Reina J. Mechanistic PK-PD model of alendronate treatment of postmenopausal osteoporosis predicts bone site-specific response. Front Bioeng Biotechnol. 2022;10:940620. doi:10.3389/fbioe.2022.940620
8. Wang C, Zheng H, He JW, et al. Genetic polymorphisms in the mevalonate pathway affect the therapeutic response to alendronate treatment in postmenopausal Chinese women with low bone mineral density. Pharmacogenomics J. 2015;15(2):158–164. doi:10.1038/tpj.2014.52
9. Zhou PR, Xu XJ, Zhang ZL, et al. SOST polymorphisms and response to alendronate treatment in postmenopausal Chinese women with osteoporosis. Pharmacogenomics. 2015;16(10):1077–1088. doi:10.2217/pgs.15.76
10. Wang JY, Zhou PR, Liu Y, et al. The analysis of DKK1 polymorphisms in relation to skeletal phenotypes and bone response to alendronate treatment in Chinese postmenopausal women. Pharmacogenomics. 2016;17(3):209–217. doi:10.2217/pgs.15.167
11. Zheng H, Wang C, He JW, Fu WZ, Zhang ZL. OPG, RANKL, and RANK gene polymorphisms and the bone mineral density response to alendronate therapy in postmenopausal Chinese women with osteoporosis or osteopenia. Pharmacogenet Genomics. 2016;26(1):12–19. doi:10.1097/FPC.0000000000000181
12. Kafienah WE, Brömme D, Buttle DJ, Croucher LJ, Hollander AP. Human cathepsin K cleaves native type I and II collagens at the N-terminal end of the triple helix. Int J Exp Pathol. 1998;331(3):727–732.
13. Dai R, Wu Z, Chu HY, et al. Cathepsin K: the action in and beyond bone. Front Cell Dev Biol. 2020;8:433. doi:10.3389/fcell.2020.00433
14. Troen BR. The regulation of cathepsin K gene expression. Ann N Y Acad Sci. 2006;1068(1):165–172. doi:10.1196/annals.1346.018
15. Yuan J, Gao YS, Liu DL, et al. PINK1-mediated mitophagy contributes to glucocorticoid-induced cathepsin K production in osteocytes. J Orthop Translat. 2022;38:229–240. doi:10.1016/j.jot.2022.11.003
16. Bonnet N, Douni E, Perréard Lopreno G, Besse M, Biver E, Ferrari S. RANKL-induced increase in Cathepsin K levels restricts cortical expansion in a periostin-dependent fashion: a potential new mechanism of bone fragility. J Bone Miner Res. 2021;36(8):1636–1645. doi:10.1002/jbmr.4307
17. Xiong F, Gao J, Li J, et al. Noncanonical and canonical splice sites: a novel mutation at the rare noncanonical splice-donor cut site (IVS4+1A>G) of SEDL causes variable splicing isoforms in X-linked spondyloepiphyseal dysplasia tarda. Eur J Hum Genet. 2009;17(4):510–516. doi:10.1038/ejhg.2008.219
18. Hung CC, Lee CN, Chang CH, et al. Genotyping of the G1138A mutation of the FGFR3 gene in patients with achondroplasia using high-resolution melting analysis. Clin Biochem. 2008;41(3):162–166. doi:10.1016/j.clinbiochem.2007.08.014
19. Kannan P, Hadeefa Begum A, Madhana Priya N, et al. Unravelling the Relacatib activity against the CTSK proteins causing pycnodysostosis: a molecular docking and dynamics approach. J Biomol Struct Dyn. 2023;31:1–12. doi:10.1080/07391102.2023.2218927
20. El-Makawy AI, Ibrahim FM, Mabrouk DM, Abdel-Aziem SH, Sharaf HA, Ramadan MF. Efficiency of turnip bioactive lipids in treating osteoporosis through activation of Osterix and suppression of Cathepsin K and TNF-α signaling in rats. Environ Sci Pollut Res Int. 2020;27(17):20950–20961. doi:10.1007/s11356-020-08540-7
21. Gao G, Zhang ZL, Zhang H, et al. Hip axis length changes in 10,554 males and females and the association with femoral neck fracture. J Clin Densitom. 2008;11(3):360–366. doi:10.1016/j.jocd.2008.04.005
22. Lewiecki EM, Gordon CM, Baim S, et al. International Society for Clinical Densitometry 2007 adult and pediatric official positions. Bone. 2008;43(6):1115–1121. doi:10.1016/j.bone.2008.08.106
23. Cummings SR, Santora AC, Black DM, Russell RGG. History of alendronate. Bone. 2020;137:115411. doi:10.1016/j.bone.2020.115411
24. Wang WJ, Fu WZ, He JW, Wang C, Zhang ZL. Association between SOST gene polymorphisms and response to alendronate treatment in postmenopausal Chinese women with low bone mineral density. Pharmacogenomics J. 2019;19(5):490–498. doi:10.1038/s41397-018-0059-8
25. LaLonde JM, Zhao B, Janson CA, et al. The crystal structure of human procathepsin K. Biochemistry. 1999;38(3):862–869. doi:10.1021/bi9822271
26. Zhu G, Chen W, Tang CY, et al. Knockout and Double Knockout of Cathepsin K and Mmp9 reveals a novel function of Cathepsin K as a regulator of osteoclast gene expression and bone homeostasis. Int J Biol Sci. 2022;18(14):5522–5538. doi:10.7150/ijbs.72211
27. Liu F, Zhou ZF, An Y, et al. Effects of cathepsin K on Emdogain-induced hard tissue formation by human periodontal ligament stem cells. J Tissue Eng Regen Med. 2017;11(10):2922–2934. doi:10.1002/term.2195
28. Meier C, Meinhardt U, Greenfield JR, et al. Serum cathepsin K concentrations reflect osteoclastic activity in women with postmenopausal osteoporosis and patients with Paget’s disease. Clin Lab. 2006;52(1–2):1–10.
29. Jahn O, Wex T, Klose S, Kropf S, Adolf D, Piatek S. Cathepsin K in treatment monitoring following intravenous zoledronic acid. Biomed Rep. 2014;2(6):915–917. doi:10.3892/br.2014.360
30. Bautista-Carbajal A, Villanueva-Arriaga RE, Páez-Arenas A, Massó-Rojas F, Frechero Molina N, García-López S. Nitrogen-containing bisphosphonates downregulate Cathepsin K and upregulate annexin V in osteoclasts cultured in vitro. Int J Dent. 2023;2023:2960941. doi:10.1155/2023/2960941
31. Gao LH, Li SS, Yue H, Zhang ZL. Associations of serum Cathepsin K and polymorphisms in CTSK gene with bone mineral density and bone metabolism markers in postmenopausal Chinese women. Front Endocrinol. 2020;11:48. doi:10.3389/fendo.2020.00048
32. Brown JP, Don-Wauchope A, Douville P, Albert C, Vasikaran SD. Current use of bone turnover markers in the management of osteoporosis. Clin Biochem. 2022;109–110:1–10. doi:10.1016/j.clinbiochem.2022.09.002
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
