Back to Journals » Clinical Interventions in Aging » Volume 16
Discrepancies Between Community-Dwelling Individuals with Dementia and Their Proxies in Completing the Cornell Scale for Depression in Dementia: A Secondary Data Analysis
Authors Leung WY , Bhar S , Reilly A, Pedell S
Received 30 October 2020
Accepted for publication 24 December 2020
Published 16 February 2021 Volume 2021:16 Pages 281—289
DOI https://doi.org/10.2147/CIA.S289595
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Wing-Yin Leung,1 Sunil Bhar,1 Ann Reilly,2 Sonja Pedell3
1Department of Psychological Sciences, Swinburne University of Technology, Melbourne, Victoria, Australia; 2Client Services Department, Dementia Australia, Melbourne, Victoria, Australia; 3Centre for Design Innovation, Swinburne University of Technology, Melbourne, Victoria, Australia
Correspondence: Sunil Bhar
Department of Psychological Sciences, Swinburne University of Technology, H99, PO Box 218, Hawthorn, Victoria, 3122, Australia
Tel +1 613 9214 8371
Fax +1 613 9819 6857
Email [email protected]
Background: Depressive symptoms are common in people with dementia.
Purpose: This study examined the discrepancies in the ratings of depressive symptoms between people with dementia and their family caregivers, and the extent to which these discrepancies varied according to the functional status of people with dementia.
Participants and Methods: This study is a cross-sectional secondary analysis. Twenty-five people living with dementia (“participants”) and their family caregivers (“proxies”) participated as pairs in the study (participant mean age = 71.36, SD = 8.63; proxy mean age = 67.54, SD = 11.46). Data were collected in Victoria, Australia between May 2018 and May 2019. Participants were administered a semi-structured interview comprising the Cornell Scale for Depression in Dementia (CSDD). Proxies independently completed the CSDD and the Functional Activities Questionnaire (FAQ). A paired sample t-test was used to investigate differences in CSDD scores between participants and proxies. Kendall’s tau-b correlation was used to examine the relationship between FAQ scores and discrepancy scores of CSDD. Participants were then classified into either low or high functional impairment. Mann–Whitney U-test was used to examine whether the discrepancy scores of CSDD were similar between these two groups. Intraclass correlation coefficients were calculated to indicate the level of agreement between participants and proxies in each group.
Results: The CSDD scores of participants were significantly lower than proxies. The size of the discrepancy in CSDD scores was positively correlated with FAQ scores. The “high functional impairment” group had larger discrepancy scores and a lower level of agreement than the “low functional impairment” group.
Conclusion: The findings highlighted that relying on proxy CSDD scores may not reflect estimates of depressive symptoms by people with dementia. Hence, both perspectives need to be taken into account, particularly when the level of functional impairment in dementia is advanced.
Keywords: cognitive impairment, function, measurement, informants, instrumental activity of daily living, pilot study
Introduction
Globally, 50 million people are estimated to be living with dementia, with projections that there will be 152 million people with this diagnosis by 2050.1 Depressive symptoms are significant in 20% to 30% of people with dementia.2 Such symptoms can impair their quality of life and health, as well as lead to increased rates of health care utilization and costs.3 Hence, assessment and treatment of such symptoms are important for dementia care.
The self-report assessment of depressive symptoms is based on an individual’s capacity to make judgments about their own well-being. Assessments of depressive symptoms are complicated in people with dementia, who may have impaired capacity for such self-ratings. They may have poor insight about internal states, poor short-term recall, high levels of confusion or difficulties with communication – symptoms common to many forms of dementia. Whether they can provide reliable self-report of depressive symptoms remains a controversial issue.4 In the literature, it is recommended that observer or proxy evaluation supplements subjective accounts of depressive symptoms in dementia.5
The Cornell Scale for Depression in Dementia (CSDD) is one of the most widely used screening measures for depressive symptoms in people living with cognitive impairment.6 This measure incorporates information from those diagnosed with dementia and from their proxies (such as nursing staff or family caregivers). According to the instructions for administering the CSDD, the clinician interviews both parties to score items on the CSDD.7 If there are discrepancies in the scores generated from these perspectives, the interviewer is instructed to meet with both parties again, and then to score items based on the interviewer’s clinical judgment.7 Although this approach is recommended by the scale’s authors, some recent studies have used the CSDD as a proxy-based scale only (eg, Blytt et al,8 Michelet et al,9 and Young et al10). This practice leads to the question of how well proxy scores on CSDD reflect those that would be provided by the person with dementia.
Discrepancies between CSDD scores based on interviews with proxies and with people with dementia have been reported in several studies. Burrows et al11 found that interviews with nurses produced higher scores on the CSDD than interviews with people with dementia in the residential aged care facility (RACF). In contrast, Towsley et al4 found that CSDD ratings provided by nurses were lower than ratings provided by RACF residents themselves. Wongpakaran et al12 did not find differences in the overall scores on the CSDD from the perspective of the RACF staff and residents. However, subscale scores differed between these cohorts; compared to residents’ responses, mood-related signs were scored higher while cyclic functions and ideational disturbances were rated lower by the RACF staff.12
Some researchers suggest that discrepancies in ratings of depressive symptoms are dependent on the characteristics of the proxy and person with dementia.13 Studies that have compared the CSDD ratings of people with dementia and their proxies have employed RACF populations and staff;4,11,12 hence, we do not know if the discrepancies found for overall and subscale scores on the measure extends to community populations with dementia where proxies are family caregivers, rather than RACF staff. It is possible that family caregivers are more familiar than RACF staff with the person with dementia, and therefore provide scores that are not discrepant from the person with dementia. However, it is also possible that compared with RACF staff, family caregivers have lower knowledge of mental health issues, and hence may inaccurately estimate levels of depressive symptoms for the person with dementia. In both cases, discrepancies may exist if the person with dementia has impaired insight into their symptoms.
The extent to which people with dementia have insight into their depressive symptoms is unclear. Ott and Fogel14 suggest that people in the early to mild dementia states retain awareness of having depressive symptoms. For such individuals, good agreement has been found between people with dementia and their proxies on the ratings of depressive symptoms.14 When dementia becomes more severe, such insight may be impaired, which has been found to result in less agreement between people with dementia and their proxies on the ratings of depressive symptoms.14 However, such findings are not consistent. In contrast to Ott and Fogel,14 Towsley et al4 found that the cognitive capacity of a person with dementia was not associated with the discrepancy between the ratings of people with dementia and their proxies in CSDD. Hence, more research is needed to understand the relationship between capacity and self-proxy discrepancies on the CSDD.
The capacity of people with dementia to accurately rate depressive symptoms may also depend on their functional status. As dementia progresses, the ability to perform instrumental activities of daily living (IADLs) deteriorates.15 Although the deterioration in functional ability is not synonymous with cognitive decline, some studies have found that functional and cognitive impairment are associated.16,17 Hence, measures of functional impairment may be used as a reference for potential cognitive decline in dementia, and signal an impaired ability to report on levels of one’s own depressive symptoms. The relationship between functional impairment and discrepancy in participant-proxy scores on CSDD remains to be investigated.
The purpose of this study was to explore whether the CSDD scores differ when completed by people with dementia who were living in their own homes, compared to their family caregivers. It also explored if observed discrepancies varied by the level of functional impairment in dementia. Given that some studies employ proxy ratings only, this study was conducted to clarify the extent to which researchers could regard proxy ratings as substitutes for self-rated depressive symptoms at different levels of functional impairment.
Participants and Methods
Design and Procedure
This study was a secondary analysis of a larger project that examined the outcomes of a range of highly customized technology solutions for people with dementia (referred to as “participants”) and their family caregivers (referred to as “proxies”). In this larger study, assessments occurred repeatedly for over 9 months. Data were collected between May 2018 and May 2019. This study used baseline data only. Written informed consent was obtained from both the participants and their proxies. Participants were interviewed by research assistants; they were provided the following instructions: “I am going to ask some questions about how you have been feeling during the past week.” Proxies were asked to complete self-report measures without assistance.
Sample
To be eligible for this study, participants were required to (a) have a diagnosis of dementia, according to self-report or specialist referral; (b) have sufficient English to complete study tasks; (c) be able to answer questions by an interviewer about their depressive symptoms; (d) have a family caregiver involved in the study; and (e) be living in the community (not in RACFs). Proxies were eligible to participate if they were: (a) a family member of the person with dementia; (b) at least 18 years old; (c) sufficiently proficient in English in order to participate in study procedures; and (d) medically and cognitively able to participate in study procedures. Participants were recruited through circulars and emails sent by Dementia Australia to their consumer networks. Potential participants were also approached directly by staff at Dementia Australia. Twenty-five pairs of participants and their proxies participated in this study.
Measures
The Cornell Scale for Depression in Dementia (CSDD) is a 19-item measure of depressive symptoms in people with dementia.5 The CSDD comprises five subscales: (1) mood-related signs, which includes anxiety, sadness, lack of reactivity to pleasant events, and irritability; (2) behavioral disturbance, which includes agitation, retardation, multiple physical complaints, and loss of interest; (3) physical signs, which includes appetite loss, weight loss, and lack of energy; (4) cyclic functions, which includes diurnal variation of mood, difficulty falling asleep, multiple awakenings during sleep, and early-morning awakening; (5) ideational disturbance, which includes suicide, poor self-esteem, pessimism, and mood-congruent delusions.5
The CSDD was formatted as a semi-structured interview when conducted with participants; each question was verbally administered by the researcher. The researcher probed for relevant phenomena using scripted questions. For example, for the item measuring anxiety, the researcher asked the participants
Have you been feeling anxious this past week? Have you been worrying about things you may not ordinarily worry about, or ruminating over things that may not be that important?
Items were scored by the researcher based on a discussion with the participants about their mood symptoms in the past week.
The CSDD was formatted as a brief self-report form for proxies. This version of the CSDD presented only the headings of items, without elaborated explanations. For example, the item measuring anxiety was presented as “Anxiety: anxious expression, ruminations, worrying”. Each item was rated for severity on a scale of 0 (“absent”) to 2 (“severe”). The item scores were added to provide a total score ranging from 0 to 38. According to the manual for CSDD,7 a total score below 6 is associated with the absence of significant depressive symptoms, between 6 and 10 indicates “minor depression”, above 10 indicates a “probable major depression”, and above 18 indicates a “definite major depression”. The CSDD has good interrater reliability (0.64 to 0.99), concurrent validity (r = 0.83), and internal consistency (alpha = 0.84).5 Cronbach’s alpha for people with dementia and their proxies were 0.84 and 0.86, respectively.12
The Functional Activities Questionnaire (FAQ) is a proxy-based measure that comprises 10 IADLs such as “shopping alone for clothes, household necessities, or groceries”, “playing a game of skill, working on a hobby”, “preparing a balanced meal”, and “keeping track of current events”.18 Each activity is rated by the family caregiver using a Likert scale ranging from 0 (“normal”) to 3 (“dependent”). Item scores are added to create a total score ranging from 0 to 30, with higher scores indicating higher degrees of functional impairment. The FAQ has high interrater reliability (r = 0.97).18
Demographic information about participants and proxies was collected. Information was collected about participants’ age, gender, country of birth, language, education, type of dementia, location and living arrangement, and relationship of proxy to participant.
Ethical Considerations
Ethics approval was obtained from the Swinburne University Human Research Ethics Committee (HREC 2018/022). This study was conducted in accordance with the Declaration of Helsinki.
Data Analyses
Data were analyzed with SPSS® version 27. Descriptive statistics for all variables were calculated. Means, standard deviations (SDs) and frequencies were computed. Missing item scores were replaced by the mean of the scale, as long as no more than a third of item scores were missing. When more than a third of item scores were missing for the scale or subscale, total scores for the relevant scale or subscale were not calculated.
To investigate whether there was a significant discrepancy between participant and proxy scores on the CSDD, a paired sample t-test was used. CSDD scores were normally distributed for participants (W(25) = 0.92, p = 0.052) and proxies (W(23) = 0.96, p = 0.42). The discrepancy scores of CSDD (ie, proxies’ scores – participants’ scores) were also normally distributed (W(23) = 0.92, p = 0.059). The power of the sample was 67% to detect a medium effect (d >0.50), and 97% to detect a strong effect (d >0.80), when employing paired sample t-tests at an alpha of 0.05.
Kendall’s tau-b correlation was performed to investigate the relationship between FAQ scores and discrepancy scores of CSDD. In addition, participants were classified into two categories of functional impairment according to the median of the FAQ score range. Participants with FAQ total scores between 0 to 15 were classified into the “low functional impairment” group, whereas participants with FAQ total scores between 16 to 30 were classified into the “high functional impairment” group. Due to the small sample size, nonparametric Mann–Whitney U-test was used to examine whether the discrepancy scores of CSDD were similar between these two groups. Rank-biserial correlation coefficient (r) was calculated as an estimate of the effect size of this non-parametric test.
Finally, in order to indicate the level of agreement between participants and proxies in each category of functional impairment, intraclass correlation coefficients (ICCs) were calculated for absolute agreement by two-way mixed methods (single measure).19 ICC values <0.5 indicate a poor level of agreement, between 0.5 and 0.75 indicate a moderate level of agreement, between 0.75 and 0.9 indicate good agreement and >0.9 indicate excellent agreement.20,21 The alpha level was set at p ≤ 0.05 for all analyses in this study.
Results
Sociodemographic Data of the Sample
Table 1 shows the percentage of missing data for CSDD and FAQ. Of the 25 pairs of participants and proxies, less than 24 provided data that allowed for a calculation of CSDD discrepancies, and for an examination of the relationship between such discrepancies and FAQ. Demographic characteristics of the participants and proxies are presented in Table 2. Of the 25 participants, most had a diagnosis of dementia due to Alzheimer’s disease, lived with a spouse or partner, and lived in metropolitan Victoria, Australia. Most participants were born in Australia. The mean age of participants with dementia was 71.36 (age ranged from 59 to 88, SD = 8.63), and just over half the sample was male. All spoke English and one spoke a language in addition to English. Approximately, a third had completed a university degree. The mean age of proxies was 67.54 (age ranged from 40 to 89, SD = 11.46). Most self-identified as spouses or partners of participants with dementia. More than half had completed a university degree.
 |
Table 1 Percentage of Missing Data for CSDD and FAQ |
 |
Table 2 Baseline Demographic Characteristics of the Sample |
Comparison of Participant and Proxy Scores
The means and SDs of proxies and participants CSDD scores are shown in Table 3. Proxy CSDD scores were significantly higher than participant CSDD scores with a large effect size (d = 0.96). On average, participants rated themselves as experiencing an “absence of significant depressive symptoms”, while their family proxies rated them as having “minor depression”. Proxies also had significantly higher scores than participants in the mood-related signs subscale (d = 0.58), behavioral disturbance subscale (d = 0.75), and cyclic functions subscale (d = 0.62). No significant differences in participant-proxy ratings were found in physical signs and ideational disturbance subscales.
 |
Table 3 Comparison of CSDD Between Participants and Proxies |
Discrepancy Scores and Functional Impairment
Table 4 shows the results of correlation analysis between the FAQ and CSDD discrepancies scores. The discrepancy scores of CSDD (mean = 3.52, SD = 4.07) were significantly correlated with FAQ scores (mean = 18.9, SD = 6.60). This positive correlation indicates that the discrepancy between participant and proxy CSDD scores increased as the severity of functional impairment in dementia increased. No significant relationship was observed, however, between discrepancy scores of CSDD subscales and FAQ scores.
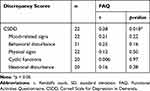 |
Table 4 Correlations Between FAQ Scores and CSDD Discrepancies Scores |
Eight participants were classified into “low functional impairment” group and 15 participants were classified into “high functional impairment” group; two participants were not classified because of missing FAQ scores. The “high functional impairment” group had significantly larger discrepancy scores (mean = 5.13, SD = 3.00) than “low functional impairment” group (mean = 1.71, SD = 2.69) (U = 18.5, z = −2.41, p = 0.016), with a large effect size (r = 0.51).22
Further, for the “low functional impairment” group, participant and proxy ratings on the CSDD were in moderate agreement (ICC = 0.67). For the “high functional impairment” such ratings were in poor agreement in CSDD (ICC = 0.27).
Discussion
The aims of this study were to examine if ratings of depressive symptoms provided by people with dementia and their family caregivers were discrepant, and if so, whether the magnitude of discrepancy was associated with functional status in dementia. This study found that the level of depressive symptoms of people with dementia was perceived as less severe by those people compared to their family caregivers. The discrepancy in participant and proxy scores increased as functional impairment worsened.
Ratings of depressive symptoms were significantly lower when rated by people with dementia compared to proxy ratings by their family caregivers. Participants rated themselves as falling in the category “absence of significant depressive symptoms” (the mean score was below 6), while their family proxies rated them as having “minor depression” (the mean score was in the range of 6–10) in this study. This pattern of scores is consistent with other studies that have found participants to report their own level of depressive symptoms as lower than do their proxies.11,23
The discrepancy between participant and proxy ratings in depressive symptoms may be due to proxies’ attentional bias towards negative information or to the poor insight amongst people with dementia for reporting depressive symptoms. Family caregivers may have been overly attentive to difficulties experienced by their family member with dementia.24,25 Caregivers may be prompted by CSDD items to recall negative experiences rather than healthy behavior. In addition, or instead, people with dementia may underestimate their level of depressive symptoms due to poor insight into their mood states. As will be discussed later, there is some evidence for this hypothesis – given the level of agreement between participant and proxy ratings was higher when functional impairment in dementia was lower.
The discrepancy between participant and proxy ratings was observed for three of the five subscales of the CSDD: mood-related signs, behavioral disturbance and cyclic functions. However, the discrepancy in ratings was not observed for subscales measuring physical signs and ideational disturbance. The low level of participant-proxy discrepancy for physical signs may reflect the relative visibility of the symptoms to the caregiver. As suggested by Snow et al,13 larger discrepancies between participant and proxy ratings were most likely to be found when rating less visible constructs. “Physical signs” was the most observable construct measured in the CSDD. For instance, appetite loss and weight loss were directly observable. The lack of discrepancy between participant and proxy ratings on ideational disturbance may conversely reflect the difficulties in rating this construct where both proxies and people with dementia under-report suicide ideation and delusional thinking.26
The discrepancy between participant and proxy ratings on CSDD was not consistent across levels of functional impairment in dementia. Higher discrepancies in CSDD ratings were found at higher levels of functional impairment. This finding was consistent with the inference from previous studies that function decreases with cognitive decline,16,17 and therefore, people with poorer function may be less reliable in reflecting about, and remembering internal states,14 resulting in under-reporting of depressive symptoms. As shown in this study, greater agreement in ratings was found when people with dementia were in the category of low functional impairment versus the high functional impairment category.
This study is the first to examine the discrepancies in CSDD ratings between people with dementia and their family caregivers in the community. Previous studies have not examined such discrepancies in community-dwelling people with dementia, but rather have focused on RACF residents.4,11,12 Such studies have focused on proxy ratings by RACF staff, rather than family caregivers.4,11,12
The findings of this study have implications for future research. The findings suggest that proxy ratings of depressive symptoms could not be regarded as a substitute for ratings by people with dementia about their own levels of depressive symptoms. Each reflects a different perspective. Family caregivers rate the person with dementia as having a higher level of depressive symptoms than is rated by the person themselves. Such a response pattern is most obvious for constructs that are less observable such as physical signs or infrequently endorsed such as suicidal and delusional ideation. The question of which perspective is more accurate is unresolved. It is equally possible that family caregivers over-estimate depressive symptoms or that persons with dementia under-report depressive symptoms. The suggestion made in the CSDD manual to take into account both persons with dementia and proxy perspectives is supported by this study,7 as either perspective in isolation may provide a distorted and subjective account of depressive symptoms in dementia.
There are four limitations of the current study. The current study explored only one moderator – functional impairment. However, a number of other moderators may predict discrepancies in ratings – such as proxies’ level of knowledge of mental health symptoms, level of closeness with participants, or their own mental health status. It is possible that proxies may have mistaken symptoms of dementia as depressive symptoms, or have distorted views of their family member’s levels of depressive symptoms because of a poor knowledge of the person with dementia or because of their current levels of distress. Family caregivers with greater levels of mental health literacy, greater familiarity with the person with dementia and more stable mental health may be less prone to biased estimations. Further studies can explore a wider range of potential moderators for the participant-proxy discrepancies in CSDD scores.
Second, the study sample was small and was clinically heterogeneous. The sample was not adequately powered to detect significant small or medium effect sizes. The sample did not reflect a homogenous group of patients with a specific type of dementia or with a specific severity of dementia or depressive symptoms. By recruiting a larger and more homogenous sample, further studies can focus on detecting smaller but significant discrepancies in CSDD ratings between proxies and people with dementia. Such a large sample would also allow for researchers to explore the extent to which discrepancies in such ratings would vary with different types of dementia and severity levels of dementia and depressive symptoms.
Third, the impact of the mode of administering the CSDD on ratings can be further explored. In this study, proxies were administered the CSDD as a self-report scale while participants with dementia were administered a semi-structured interview. This difference in administration mode may have accounted for discrepancies in ratings by proxies and people with dementia. It is unlikely that such administration mode fully accounted for such discrepancies but this hypothesis remains to be empirically tested.
Finally, participants’ ratings in this study were based exclusively on reports elicited during an interview and were not based on the interviewer’s direct observation of the participants’ behavior. Ratings based on such observations are recommended in the CSDD manual.7 Hence, it is possible that hybrid ratings based on both participant and observer perspectives may have also changed CSDD ratings. Further studies should explore if there are differences in self-versus-interviewer administrations of CSDD, when such observer ratings are taken into account.
Conclusion
This study suggests that family caregiver proxy ratings on the CSDD overall tend to be significantly higher than ratings provided by the person with dementia. These discrepancies were significantly greater when people with dementia were living with higher levels of functional impairment compared to lower levels of functional impairment. However, people with dementia and their family caregivers provided similar ratings on those features of depression that were visible – such as physical signs, or less frequently endorsed – such as suicidal and delusional ideation. For other symptoms, proxy ratings could not be regarded as substitutes for ratings provided by the person with dementia about their depressive symptoms. Hence, both perspectives need to be taken into account, particularly when the level of functional impairment in dementia is advanced, or when rating depressive symptoms that are less visible or prevalent.
Acknowledgments
All authors approved the final manuscript. We wish to acknowledge funding by the Department of Health (Dementia and Aged Care Services Fund) to support this project. We also wish to acknowledge the assistance provided by Mulu Woldegiorgis with respect to project management.
Disclosure
The authors report no conflicts of interest in this work.
References
1. World Health Organization. Dementia: fact sheets. Available from: https://www.who.int/news-room/fact-sheets/detail/dementia.
2. Enache D, Winblad B, Aarsland D. Depression in dementia: epidemiology, mechanisms, and treatment. Curr Opin Psychiatry. 2011;24(6):461–472. doi:10.1097/YCO.0b013e32834bb9d4
3. Meeks TW, Vahia IV, Lavretsky H, Kulkarni G, Jeste DV. A tune in “a minor” can “b major”: a review of epidemiology, illness course, and public health implications of subthreshold depression in older adults. J Affect Disord. 2011;129(1–3):126–142. doi:10.1016/j.jad.2010.09.015
4. Towsley G, Neradilek MB, Snow AL, Ersek M. Evaluating the cornell scale for depression in dementia as a proxy measure in nursing home residents with and without dementia. Aging Ment Health. 2012;16(7):892–901. doi:10.1080/13607863.2012.667785
5. Alexopoulos GS, Abrams RC, Young RC, Shamoian CA. Cornell scale for depression in dementia. Biol Psychiatry. 1988;23(3):271–284. doi:10.1016/0006-3223(88)90038-8
6. Mellow AM, Kales HC, Maixner SM. Depression and anxiety in late life. In: Mellow AM, editor. Geriatric Psychiatry. Vol. chap 1. American Psychiatric Association Publishing; 2008:1–34.
7. Alexopoulos GS. The Cornell Scale for Depression in Dementia: Administration & Scoring Guidelines. New York: Cornell Institute of Geriatric Psychiatry; 2002:1–11.
8. Blytt KM, Bjorvatn B, Husebo B, Flo E. Clinically significant discrepancies between sleep problems assessed by standard clinical tools and actigraphy. BMC Geriatr. 2017;17(1):253. doi:10.1186/s12877-017-0653-7
9. Michelet M, Lund A, Strand BH, Engedal K, Selbaek G, Bergh S. Characteristics of patients assessed for cognitive decline in primary healthcare, compared to patients assessed in specialist healthcare. Scand J Prim Health Care. 2020;38(2):107–116. doi:10.1080/02813432.2020.1753334
10. Young DK, Ng PY, Kwok T. Predictors of the health-related quality of life of Chinese people with major neurocognitive disorders and their caregivers: the roles of self-esteem and caregiver’s burden. Geriatr Gerontol Int. 2017;17(12):2319–2328. doi:10.1111/ggi.13065
11. Burrows AB, Satlin A, Salzman C, Nobel K, Lipsitz LA. Depression in a long-term care facility: clinical features and discordance between nursing assessment and patient interviews. J Am Geriatr Soc. 1995;43(10):1118–1122. doi:10.1111/j.1532-5415.1995.tb07011.x
12. Wongpakaran N, Wongpakaran T, van Reekum R. Discrepancies in Cornell Scale for Depression in Dementia (CSDD) items between residents and caregivers, and the CSDD’s factor structure. Clin Interv Aging. 2013;8:641–648. doi:10.2147/CIA.S45201
13. Snow AL, Cook KF, Lin PS, Morgan RO, Magaziner J. Proxies and other external raters: methodological considerations. Health Serv Res. 2005;40(5):1676–1693. doi:10.1111/j.1475-6773.2005.00447.x
14. Ott BR, Fogel BS. Measurement of depression in dementia: self vs clinician rating. Int J Geriatr Psychiatry. 1992;7:899–904. doi:10.1002/gps.930071209
15. Stern Y, Hesdorffer D, Sano M, Mayeux R. Measurement and prediction of functional capacity in alzheimer’s disease. Neurology. 1990;40:8–14. doi:10.1212/wnl.40.1.8
16. Rajan KB, Hebert LE, Scherr PA, Mendes de Leon CF, Evans DA. Disability in basic and instrumental activities of daily living is associated with faster rate of decline in cognitive function of older adults. J Gerontol Ser a Biol Sci Med Sci. 2013;68(5):624–630. doi:10.1093/gerona/gls208
17. Helvik AS, Hogseth LD, Bergh S, Saltyte-Benth J, Kirkevold O, Selbaek G. A 36-month follow-up of decline in activities of daily living in individuals receiving domiciliary care. BMC Geriatr. 2015;15(47):1–13. doi:10.1186/s12877-015-0047-7
18. Pfeffer RI, Kurosaki TT, Harrah CH, Chance JM, Filos S. Measurement of functional activities in older adults in the community. J Gerontol. 1982;37(3):323–329. doi:10.1093/geronj/37.3.323
19. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979;86(2):420–428. doi:10.1037//0033-2909.86.2.420
20. Portney LG, Watkins MP. Foundations of Clinical Research: Applications to Practice.
21. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. doi:10.1016/j.jcm.2016.02.012
22. Cohen J. Statistical Power Analysis for the Behavioral Sciences.
23. Snow AL, Kunik ME, Molinari VA, et al. Accuracy of self‐reported depression in persons with dementia. J Am Geriatr Soc. 2005;53(3):389–396. doi:10.1111/j.1532-5415.2005.53154.x
24. Kanouse DE, Hanson LR. Negativity in evaluations. In: Jones EE, Kanouse DE, Kelley HH, Nisbett RE, Valins S, Weiner B, editors. Attribution: Perceiving the Causes of Behavior. General Learning Press; 1972:47.
25. Tversky A, Kahneman D. Judgement under uncertainty: heuristics and biases. Scis. 1974;185(4157):1124–1131. doi:10.1126/science.185.4157.1124
26. Snowdon J, Rosengren D, Daniel F, Suyasa M. Australia’s use of the cornell scale to screen for depression in nursing homes. Australas J Ageing. 2011;30(1):33–36. doi:10.1111/j.1741-6612.2010.00450.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
