Back to Journals » Clinical Ophthalmology » Volume 17
Different Modalities for Management of Pediatric Epiphora
Authors Abd-El Hakeem MT , Abdallah A, Abdelmoneim R, Khaleel A, Abdallah R
Received 20 February 2023
Accepted for publication 5 April 2023
Published 19 April 2023 Volume 2023:17 Pages 1193—1201
DOI https://doi.org/10.2147/OPTH.S406836
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mostafa Talaat Abd-El Hakeem,1 Adel Abdallah,1 Rasha Abdelmoneim,1 Ahmed Khaleel,1 Raafat Abdallah2
1Otorhinolaryngology Department, Faculty of Medicine, Minia University, Minia, Egypt; 2Ophthalmology Department, Faculty of Medicine, Minia University, Minia, Egypt
Correspondence: Mostafa Talaat Abd-El Hakeem, Email [email protected]
Objective: This study assessed the efficacy and safety of different modalities for managing nasolacrimal duct obstruction and epiphora in children over one year.
Methods: We performed a non-randomized prospective study on 98 children (149 eyes) with epiphora and no history of lacrimal operation. The selected candidates attended the ENT and ophthalmology outpatient clinics of Minia University Hospital, seeking to treat epiphora that may or may not be associated with sinonasal pathology. Nasolacrimal operations involved a joint approach involving an otorhinolaryngologist and an ophthalmologist.
Results: Ninety-eight children (149 eyes) were identified. Ages varied from 1 to 12 years old. Conservative measures were successful in 32.6% of children. Silicone stents were used in 27.5% of the interventions with a mean time to removal of 3– 6 months. The success rate for dacryocystorhinostomy (DCR) was 85.7%. Revision surgery was performed in 10% of probing cases, 8% of intubation cases, and 14.3% of DCR patients. The concomitant chronic sinonasal problems were evident in 62.2% of patients.
Conclusion: Conservative measures, probing, endonasal nasolacrimal intubation, endoscopic DCR, and external DCR are safe and effective procedures for epiphora in children. Also, correcting concomitant nasopharyngeal or sinonasal diseases in epiphora patients is crucial for successful management, overcoming recurrence, and minimizing morbidity.
Keywords: pediatric epiphora, pediatric dacryocystorhinostomy, endonasal nasolacrimal intubation, sinonasal pathology
Introduction
Congenital epiphora affects up to 20% of all newborns. It usually results from the incomplete development of the lower end of the tear duct with persistent web membrane at the site of Hasner’s valve or bony abnormalities, known collectively as congenital nasolacrimal duct obstruction (CNLDO). The reported rate of spontaneous resolution is 90% within the first year of life.1
For cases where obstruction does not resolve spontaneously, conservative measures such as lacrimal sac massage and medical treatment proved effective in many children.2 Fortunately, many cases unresolved by conservative measures in the first year of age benefit from nasolacrimal endoscopic assisted probing and irrigation. However, the success rate of this maneuver is inversely related to the age of the child.3,4
Lacrimal intubation has become a widely used procedure for congenital nasolacrimal duct obstruction that does not improve by conservative medical treatment or unsuccessful probing.5,6
When NLDO is unresponsive to less invasive lines of treatment, such as probing and intubation, or when associated with recurrent dacryocystitis, pediatric DCR is instituted. Previously, such cases received external DCR. However, endoscopic DCR has become more common nowadays.7,8
In the current work, we investigated the correlation between sinonasal pathologies and nasolacrimal disorders in patients with uni- or bilateral NLDO.9,10 We evaluated the prevalence of sinonasal abnormalities of anatomical, inflammatory, or infectious etiology, such as polyps, nasal allergy, and adenoid hypertrophy observed.
Aim of This Study
We aimed to evaluate the outcomes of collaborative ophthalmological and ENT endonasal procedures for managing persistent epiphora with or without associated sinonasal disease in pediatric candidates. Besides, we sought to establish a clear plan for managing pediatric epiphora.
Patients and Methods
This study followed a prospective design comprising 98 children selected from Minia University Hospital outpatients after full ENT and ophthalmological assessment. Eyes diagnosed with epiphora (n = 149), plus or minus sinonasal manifestations, were included. Of the 98 children, 61 presented with sinonasal problems (Table 1). Children were evaluated between December 2020 and September 2022 and received medical and/or surgical treatment for persistent nasolacrimal system obstruction. A successful outcome was indicated by symptomatic relief.
 |
Table 1 Associated Nasopharyngeal or Sinonasal Pathology |
Informed written consent was obtained from the parents of the patients after carefully explaining the details of the study.
*Inclusion criteria:
– Excessive eye watering in children aged 1 to 12 years (unilateral or bilateral).
– Possible presence of sinonasal symptoms such as nasal obstruction, snoring, allergic manifestations (sneezing/itching/rhinorrhea), and/or nasal discharge.
*Exclusion criteria:
– Children less than one year of age.
– Eye conditions, such as punctal maldevelopment, congenital ectropion, blepharitis, congenital glaucoma, and conjunctivitis.
– Children who underwent nasolacrimal operations such as probing, intubation, or DCR surgery.
– Cases of lacrimal fistula and dacryocystitis.
Conservative and Medical Measures
All 98 cases received conservative medical treatment, including Crigler’s lacrimal sac massage. Besides, in conjunction with eye measures, 61 patients received decongestants, antihistaminics, and nasal or systemic steroids for treating their sinonasal complaints. Parents were encouraged to apply topical antibiotic eye drops whenever an infected discharge appeared in a child’s eye. All cases were regularly evaluated every two weeks for clinical improvement and relief of seasonal symptoms.
These conservative medical measures continued for at least six weeks in all cases unless spontaneous recovery of epiphora was achieved or when probing was decided for cases showing no improvement. In the current study, spontaneous recovery was observed in 15 cases of isolated epiphora and 17 cases of epiphora associated with nasal allergy.
Invasive Treatment of NLDO
The cases that failed to respond to conservative measures underwent invasive treatment by endoscopy-guided probing, silicone tube intubation, or dicryocystorhinostomy (DCR).
The first-line invasive procedure: endoscopy-guided probing and syringing of the lacrimal passages with surgical correction of nasal or nasopharyngeal disease, if present, was performed in 30 children older than one year and younger than four. Twenty of these children were associated with nasal allergy (treated conservatively) or nasopharyngeal adenoid hypertrophy, which was treated with combined technique adenoidectomy (at the same operative session).
Endoscopy guidance improved the detection and handling of variations in the submucosal entry, the elastic membrane at the Hasner’s valve, and the presence of tight inferior concha. Thus, endoscopy-assisted probing achieved better success rates than the unguided technique, especially in complicated cases suffering from NLDO associated with nasal or posterior nasal pathology not resolved by treatment (Figure 1). On the other hand, the blind probing procedure can lead to complications such as false passages, bleeding, infection, and fibrosis of NLD. Failure of probing is identified by the recurrence of symptoms after primary probing, often within six weeks. Factors contributing to unsuccessful probing outcomes include improper maneuvering, narrowing of the opening leading to recurrence, probing at older ages, bilateral NLDO cases, and variations in the nasolacrimal anatomy.
 |
Figure 1 Endoscopic-assisted probing. |
The second line of invasive treatment, silicone tube intubation, was performed in three cases that failed to respond to probing beside 24 additional children aged 2–7 (Figure 2). Seventeen of these 24 cases presented with nasal allergy, nasopharyngeal adenoid hypertrophy, deviated nasal septum, or unilateral choanal atresia. These concomitant defects were simultaneously corrected at the same operative session in the affected patients as follows:
– 4 cases with associated nasal allergy received conservative treatment.
– 5 cases with nasopharyngeal adenoid hypertrophy were treated with combined technique adenoidectomy (transoral/transnasal).
– 5 children with deviated nasal septum were treated by endoscopic septoplasty.
– 3 cases with unilateral choanal atresia were treated by endoscopic canalization and stenting.
 |
Figure 2 Endoscopic guided nasolacrimal silicone intubation. |
silicone intubation is an invasive maneuver where a bi- or mono-canalicular silicone stent is inserted and left in place for 3–6 months. The success rate of probing and intubation is inversely related to the child’s age. The morbidities of intubation include punctal damage, tube extrusion, and local granuloma formation.
The third line of invasive treatment, dacryocystorhinostomy (DCR), was performed in 2 cases that failed to resolve after silicone intubation and in 12 patients suffering from recurrent or chronic dacryocystitis (4–12 years old), Figure 3.
 |
Figure 3 Insertion of eagle tube under vision after opening of lacrimal sac in endoscopic DCR. |
The external DCR, the “gold standard” maneuver, was carried out in seven cases that had isolated epiphora. The other seven patients, who had epiphora accompanied by sinonasal disorder, received Endonasal DCR as follows:
– Two cases had nasopharyngeal adenoid hypertrophy: treated with combined technique adenoidectomy (transoral/transnasal).
– Two children had deviated nasal septum: treated by endoscopic septoplasty.
– One case had unilateral choanal atresia: treated by endoscopic canalization with stenting.
– One case had a unilateral antro-choanal polyp: treated by endoscopic removal with wide middle meatal antrostomy.
– One case had allergic fungal rhinosinusitis: treated by functional endoscopic sinus surgery.
The degree of recovery from previous complaints determines the clinical success of DCR. The most typical problem of pediatric endonasal DCR is the early extrusion of the silicone tube. Although it does not usually lead to further complications, premature tube loss may increase the possibility of long-term failure. Nonetheless, endoscopic DCR has success rates approaching those of external DCR in the pediatric population.
Data Analysis and Statistics
The SPSS software (version 22) was used for data entry and statistical analyses. Descriptive statistics were used to illustrate the study findings. Quantitative variables were presented as the mean and standard deviation, while qualitative data were illustrated as frequencies and percentages. Figures were drawn with the help of Microsoft Excel 2010.
Results
Demographic Data
Ninety-eight children (50 girls and 48 boys; 149 eyes) with excessive tearing were involved in this study. The mean age was 5.62 ± 1.7 years, and the age range was 1 to 12 years (Table 2).
 |
Table 2 Sociodemographic Data of Studied Children |
Sixty-one (62.2%) of the 98 children had associated nasopharyngeal or sinonasal pathologies as follows:
– 28 cases had associated nasal allergy.
– 20 patients had associated nasopharyngeal adenoid hypertrophy.
– 7 cases had deviated nasal septum.
– 4 patients had unilateral choanal atresia.
– 1 child had an antro-choanal polyp.
– 1 patient had unilateral allergic fungal rhinosinusitis.
Thirty-seven cases (40 eyes) presented with isolated epiphora with no accompanying sinonasal comorbidity (Table 3 and Table 4).
 |
Table 3 Distribution of Studied Patients According to Disease |
 |
Table 4 Frequencies of Associated Nasopharyngeal or Sinonasal Pathology Among Studied Cases |
Following only the conservative and medical measures, the epiphora of 32 patients improved spontaneously, with a success rate of 32.6% of the total number of patients.
On the other hand, endoscopically guided probing and syringing of the lacrimal passages with correction of nasal or nasopharyngeal disease (when present) resulted in 90% success (27 of 30 cases) in children aged 1–4 (Figure 4). Three patients who were unresponsive to probing showed clinical improvements after silicone intubation.
 |
Figure 4 Success and failure percentage of probing among studied cases. |
Moreover, silicone nasolacrimal intubation in children between 2 and 7 years old resulted in 90% success in resolving isolated epiphora in nine of 10 cases with no associated sinonasal disease. Besides, 17 of these 24 cases (94.1%) showed improved excessive watering of the eye, which was related to sinonasal comorbidity, upon nasolacrimal intubation (Figure 5).
 |
Figure 5 Success and failure percentage of intubation among studied cases. |
Besides the 12 cases with recurrent or chronic dacryocystitis (aged 4–12), DCR has been carried out in 2 cases that failed to resolve after nasolacrimal intubation. The surgical procedure was performed either as an open DCR (7 patients with isolated epiphora) or as an Endonasal DCR (7 cases of epiphora plus sinonasal disorder). The two methods showed the same success rate of 85.7%, with only two patients requiring revision surgery (Figure 6).
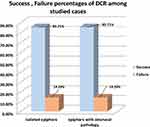 |
Figure 6 Success and failure percentage of DCR among studied cases. |
The successful outcomes were defined as the relief of symptoms of NLDO ± syringing in co-operative older children to see the fluid coming through the new ostium by endoscopy and improvement of sinonasal manifestations in the affected patients.
Discussion
Congenital nasolacrimal duct obstruction (CNLDO) is the most common cause of epiphora in infants and young children. This condition resolves spontaneously in 85–96% of cases by the age of 1 year.11,12 Chronic rhinosinusitis and other sinonasal comorbidities induce excessive eye tearing due to inflammation of the lower part of the nasolacrimal duct.13 In the current study, we investigated the outcomes of different interventions on clinical outcomes in 98 children aged 1–12 with excessive tearing of 1 or both eyes. All patients received conservative medical measures. For unresolved epiphora, different surgical procedures were performed by an expert team of ophthalmology/ENT surgeons. Patients were regularly evaluated to ensure the relief of manifestations and to confirm the patency of the lacrimal passage by postoperative endoscopy. The results showed that the success rate in children with non-isolated nasolacrimal obstruction was comparable to that in isolated epiphora, possibly because the sinonasal pathology was diagnosed and corrected simultaneously with epiphora.14
Endoscopic-guided NLD probing is a safe and feasible option as a primary management strategy for epiphora. However, the failure rate of probing increases with age—previous studies associated worse outcomes with age over two years.15,16
Nasolacrimal intubation performed by the operative team is rapid and has minimal complications. The optimum tensioning of the tube is essential to prevent cheese wiring through the puncta (when the tube is too tight) or the tube from getting out of the puncta (when the tube is too loose). Although optimizing tube tension requires a certain level of skill by the surgeon, cheese wiring did not change the cure rate. On the other hand, the prolapse of the silicone tube was annoying to the parents; it often necessitated early tube removal, and it could lead to a failed procedure. Thus, a question arises about the appropriate duration for the retention of tubes. In our study, the silicone intubation stent was maintained in situ for 3–6 months.5,17
The DCR procedure is reserved for intubation-resistant NLDO cases and recurrent or chronic dacryocystitis patients. Usually, doctors prefer to postpone the surgery until the child reaches 3 to 4 years to avoid any undesirable effects on the growth of nasal bones.18
Our study results confirmed the safety and feasibility of endoscopic DCR as a good option for epiphora in children. Endoscopic DCR has many advantages: it is more cosmetic (no skin incision), it preserves the medial canthus, it does not affect the physiology of the lacrimal system, it offers better control of intraoperative epistaxis, and its recovery time is faster.19 In addition, sinonasal or nasopharyngeal pathologies can be treated in the same operative session and take a shorter time than the external technique.20
In children, some important technical points are different from those in adults. In children, identifying anatomical landmarks is difficult because of the different pneumatization of agger nasi, and, unlike in adults, the lacrimal eminence and uncinate process may be hidden. The nonendoscopic (external) DCR procedure has a comparable success rate to the endoscopic maneuver but without disadvantages such as the high cost and required surgical experience.21,22
Conclusions
Conservative measures, probing, endonasal nasolacrimal intubation, endoscopic DCR, and external DCR are safe and effective procedures for dealing with epiphora in children. Besides, correction of possibly present nasopharyngeal or sinonasal diseases in epiphora patients is very important for successful management, overcoming recurrence, and minimizing morbidity.
Ethical Approval
Approval number 697:12/2020. We officially notify you that our “Faculty of Medicine, Research Ethics Committee (FMREC)”, Minia University, has reviewed and approved your submitted protocol, which has been entitled as mentioned above (approval number 697:12/2020). The study was adherent to the tenets of the Declaration of Helsinki.
Funding
This research has not received grants from any public, commercial, or not-for-profit agency.
Disclosure
The authors declare that they have no competing interests.
References
1. Macewen CJ. Congenital nasolacrimal duct obstruction. Compr Ophthalmol Update. 2006;7(2):79–87.
2. Nelson LB, Calhoun JH, Menduke H. Medical management of congenital nasolacrimal duct obstruction. Ophthalmology. 1985;92(9):1187–1190. doi:10.1016/S0161-6420(85)33878-2
3. Honavar SG, Prakash VE, Rao GN. Outcome of probing for congenital nasolacrimal duct obstruction in older children. Am J Ophthalmol. 2000;130(1):42–48. doi:10.1016/S0002-9394(00)00388-3
4. Kashkouli MB, Beigi B, Parvaresh MM, Kassaee A, Tabatabaee Z. Late and very late initial probing for congenital nasolacrimal duct obstruction: what is the cause of failure? Br J Ophthalmol. 2003;87(9):1151–1153. doi:10.1136/bjo.87.9.1151
5. Aggarwal RK, Misson GP, Donaldson I, Willshaw HE. The role of nasolacrimal intubation in the management of childhood epiphora. Eye. 1993;7(6):760–762. doi:10.1038/eye.1993.177
6. Cunningham MJ. Endoscopic management of pediatric nasolacrimal anomalies. Otolaryngol Clin North Am. 2006;39(5):1059–1074. doi:10.1016/j.otc.2006.07.004
7. Abozaid M, Othman Y. External versus endoscopic dacryocystorhinostomy for congenital nasolacrimal duct obstruction. J Egypt Ophthalmol Soc. 2015;108(3):148–152. doi:10.4103/2090-0686.168718
8. Struck HG, Weidlich R. Indikation und Prognose der Dakryozystorhinostomie im Kindesalter Eine klinische Studie 1970–2000 [Indications and prognosis of dacryocystorhinostomy in childhood. A clinical study 1970–2000]. Ophthalmologe. 2001;98(6):560–563. German. doi:10.1007/s003470170119
9. Borges Dinis P, Oliveira Matos T, Ângelo P. Does sinusitis play a pathogenic role in primary acquired obstructive disease of the lachrymal system? Otolaryngol Head Neck Surg. 2012;148(4):685–688. doi:10.1177/0194599812471615
10. Habesoglu M, Eriman M, Habesoglu TE, et al. Co-occurrence and possible role of sinonasal anomalies in primary acquired nasolacrimal duct obstruction. J Craniofac Surg. 2013;24(2):497–500. doi:10.1097/SCS.0b013e31827c83ea
11. Olitsky SE. Update on congenital nasolacrimal duct obstruction. Int Ophthalmol Clin. 2014;54(3):1–7. doi:10.1097/IIO.0000000000000030
12. Schnall BM. Pediatric nasolacrimal duct obstruction. Curr Opin Ophthalmol. 2013;24(5):421–424. doi:10.1097/ICU.0b013e3283642e94
13. Annamalai S, Kumar NA, Madkour MB, Sivakumar S, Kubba H. An association between acquired epiphora and the signs and symptoms of chronic rhinosinusitis: a prospective case–control study. Am J Rhinol. 2003;17(2):111–114. doi:10.1177/194589240301700209
14. Olver J, Minasian M. Nasal endoscopy for ophthalmologists. CME J Ophthalmol. 1998;2:73–77.
15. Abd El Ghafar AE. Endoscopic-guided probing for the management of congenital nasolacrimal duct obstruction. Delta J Ophthalmol. 2015;16(2):93–96. doi:10.4103/1110-9173.168539
16. Petris C, Liu D. Probing for congenital nasolacrimal duct obstruction. Cochrane Database Syst Rev. 2017;7. doi:10.1002/14651858.CD011109.pub2
17. Pediatric Eye Disease Investigator G. Primary treatment of nasolacrimal duct obstruction with nasolacrimal duct intubation in children younger than 4 years of age. J Am Assoc Pediatr Ophthalmol Strabismus. 2008;12(5):445–450. doi:10.1016/j.jaapos.2008.03.005
18. Komínek P, Červenka S, Matoušek P, Pniak T, Zeleník K. Primary pediatric endonasal dacryocystorhinostomy—a review of 58 procedures. Int J Pediatr Otorhinolaryngol. 2010;74(6):661–664. doi:10.1016/j.ijporl.2010.03.015
19. Komínek P, Červenka S. Pediatric endonasal dacryocystorhinostomy: a report of 34 cases. Laryngoscope. 2005;115(10):1800–1803. doi:10.1097/01.mlg.0000175678.73264.88
20. Nussbaumer M, Schreiber S, Yung MW. Concomitant nasal procedures in endoscopic dacryocystorhinostomy. J Laryngol Otol. 2006;118(4):267–269. doi:10.1258/002221504323011996
21. Bothra N, Wani RM, Ganguly A, Tripathy D, Rath S. Primary nonendoscopic endonasal versus external dacryocystorhinostomy in nasolacrimal duct obstruction in children. Indian J Ophthalmol. 2017;65(10):1004–1007. doi:10.4103/ijo.IJO_188_17
22. Grover AK. Management of nasolacrimal duct obstruction in children: how is it changing? Indian J Ophthalmol. 2017;65(10):910–911. doi:10.4103/ijo.IJO_719_17
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
