Back to Journals » Clinical Interventions in Aging » Volume 13
Differences of patients’ perceptions for elective diagnostic coronary angiography and percutaneous coronary intervention in stable coronary artery disease between elderly and younger patients
Authors Rittger H , Frosch B, Vitali-Serdoz L, Waliszewski M
Received 24 June 2018
Accepted for publication 3 August 2018
Published 10 October 2018 Volume 2018:13 Pages 1935—1943
DOI https://doi.org/10.2147/CIA.S178129
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Walker
Harald Rittger,1 Barbara Frosch,1 Laura Vitali-Serdoz,1 Matthias Waliszewski2,3
1Medizinische Klinik 1, Klinikum Fürth, Fürth, Germany; 2Medical Scientific Affairs, B. Braun Melsungen AG, Berlin, Germany; 3Department of Internal Medicine and Cardiology, Charité – Universitätsmedizin Berlin, Campus Virchow, Berlin, Germany
Aims: There is limited evidence of the differences in expectations between elderly (≥80 years) and younger patients (<80 years) regarding treatment success of percutaneous coronary interventions (PCI). We conducted a survey in patients undergoing diagnostic coronary angiography (DA) and/or intervention (PCI) to identify differences in patient perceptions between elderly and younger patients.
Methods and results: This is an all-comers study of consecutive patients who underwent DA and/or PCI. Patients were asked to fill out a questionnaire prior to DA/PCI. This questionnaire consisted of ten questions with potential patient expectations based on an increasing scale of importance from 0 to 5 which were related to the procedure (eg, extend life, decrease symptoms etc.) and the value of “hard” cardiac endpoints like death, stroke, acute myocardial infarction and target lesion revascularization for the patient. Among 200 patients (mean age 76.6±9.3 years, 60.5% male, ejection fraction 63.7%±13.2%), 100 patients (50%) were ≥80 years. For these elderly patients the questions “to remain independent,” “to maintain mobility, so that I can maintain my current life,” and “to prevent myocardial infarction” were rated highest. Regarding “hard” cardiac endpoints “to avoid PCI in the future” was rated lowest in younger and in elderly patients. Significant differences were found between the age groups with the items “to avoid myocardial infarction,” “avoid heart insufficiency,” “to extend my life” and “to maintain mobility so that I can maintain my current life” (P<0.001).
Conclusions: In our survey we found significant differences in patient expectations between elderly and younger patients regarding the outcome of DA/PCI.
Keywords: patient perceptions, coronary angiography, percutaneous coronary intervention, elderly
Introduction
Existing data provide evidence that an elective PCI can be performed safely and with a high success rate not only in an overall population, but also in an elderly patient group.1–4 In contrast to younger patients who may have higher expectations to restore their myocardial perfusion, the strategy to perform percutaneous coronary intervention (PCI) may be different in older patients who are probably associated with a more sedentary life style. Lower pain levels,5–7 which have been reported for an older population, and a reduction in physical activity might implicate, that pain relief as the main indication for PCI does not play a major role in this patient group. It therefore competes with medical treatment, because physical activity is often reduced in this patient group. Furthermore, in the light of a limited remaining life span, one might expect that there is a different emphasis on the goals of a procedure. There is only limited evidence regarding patient expectations in patients who have to undergo coronary angiography or intervention8–10 and no evidence about differences in patients’ expectations between elderly and younger patients concerning treatment success. But research regarding this issue is extremely important. Firstly, in an attempt to determine adequate outcome measurements for elderly patients (death, myocardial infarction [MI], stroke vs improvement of functional capacity or to maintain mobility) it is necessary to know patients’ wishes and expectations with regard to the intervention. Secondly, to determine factors, which may be more effective and more suitable to predict outcomes after coronary interventions. These reveal functional, cognitive and behavioral deficits, which may play a decisive role since the evidence to perform such procedures is based on conventional endpoints (death, MI, target lesion revascularization) in this patient group.11 Not least important, as already mentioned there is no study that has been conducted to evaluate patients’ wishes regarding outcomes in patients with advanced age.
We conducted the current survey to determine possible differences in patients’ perceptions regarding the value of coronary angiography/intervention and to identify differences in patient perceptions between elderly and younger patients.
Methods
Patient population
From September 2015 to April 2016, 200 consecutive patients, in whom coronary angiography and/or intervention was indicated, were invited to participate in a questionnaire in our center. This entailed a structured interview to assess their expectations for the procedure. Informed and consented patients for DA and PCI were asked to participate in the survey prior to the intervention for patient quality assurance. To ensure consecutive recruitment each patient ≥80 years and every third consecutive patient <80 years were included.
Patients >18 years with stable angina pectoris or silent ischemia as detected by a stress test were eligible for inclusion. To focus on patients with stable coronary artery disease, we excluded those patients with primary or emergent PCI due to ST-elevation myocardial infarction (STEMI), Non-ST-elevation myocardial infarction (NSTEMI) and unstable angina (UA). Accordingly, we restricted our analysis to patients with stable coronary artery disease. Further exclusion criteria were patient transferal from another hospital, the inability to give informed consent (e.g. dementia) and the inability to perform the questionnaire and the interview. There were no exclusions due to age or comorbidity. All data were routinely collected. The study complied with the provisions of the Declaration of Helsinki in its most current form and all patients gave written informed consent for the procedure. The ethics committee of the University of Erlangen-Nuremberg, Germany agreed to the survey within the routine framework of quality management at our institution.
Study procedures and questionnaire
Within the routine framework of quality management at our institution, the primary measurement was a grading (0–5) of a list for potential benefits from the procedure. These items were evaluated in a 2-year survey, in which patients were asked to report their expectations on a voluntary basis prior to invasive diagnostic or therapy in our department. After comparison with the existing literature, these expectations were summarized in a questionnaire consisting of ten patient expectations of the procedure:8,10,12–14
1) to avoid angina; 2) to avoid myocardial infarction in the future; 3) to avoid dyspnea; 4) to avoid heart failure; 5) to avoid further hospital stays in the future; 6) to regain/maintain physical resistance; 7) to extend my life; 8) to remain independent; 9) to maintain mobility so that I can maintain my current life; and 10) to take less co-medication.
In a second step the expectations relative to adverse events were evaluated: 1) to avoid death; 2) to avoid myocardial infarction; 3) to avoid stroke; 4) to avoid further interventions (PCI or CABG) in the future; and 5) to have sufficient quality of life were evaluated.
The value of the different items was rated between 0 and 5 (0=not important and 5=very important).
To avoid an interaction with these predetermined questions, an interview was conducted prior to filling out the questionnaire, in which the patients were asked to express their own perceptions of the procedure.
At the same time, we collected data of the demographic and clinical characteristics, including sex, marital status, smoking status, medical history (prior MI, percutaneous coronary intervention, and coronary artery bypass grafting) as well as other cardiac risk factors (hypertension, diabetes, obesity, hyperlipidemia and family history of CAD). After the procedure all procedural aspects were collected.
Statistical analysis and primary and secondary endpoints
For dichotomous variables either the two-sided Fisher’s exact test or the chi-squared statistic were used whenever applicable. In case of continuous variables, the unpaired t-test was typically used. In case the Shapiro-Wilk test revealed a strong deviation from a normal distribution, the Mann–Whitney U test was preferred. To compare the perception scores, the independent samples Mann–Whitney U test was used to account for non-Gaussian distributions. The significance level α of 0.05 was used for all tests. To estimate the sample size, a difference in perception scores of 0.4 was assumed with at least one age group having a perception score of 4.0 and a SD of 0.8 in both subgroups. A sample size of 64 in each group would then have 80% power to detect a difference of 0.4 in perception scores. For all descriptive statistical analyses SPSS version 24.0 (IBM, Munich, Germany) was used whereas nQuery/nTerim version 2.0 (Statistical Solutions Ltd. Cork, Ireland) was preferred for sample size estimates.
Results
A total of 200 consecutive patients with planned coronary angiography/intervention were included. Of these, 100 were <80 years and 100 were ≥80 years, the mean age was 76.6±9.3 years (69.5±7.9 vs 83.7±3.9).
Baseline clinical and angiographic characteristics were very similar in the two age groups (Figure 1). There were more women in the group of patients >80 years (72/100, 72.0% vs 49/100, 49.0%, P<0.001) and a higher frequency of patients with a history of smoking (39/100, 39.0% vs 13/100, 13.0%, P<0.001) and hyperlipidemia (77/100, 77.0% vs 64/100, 64.0%, P=0.044) in the younger patient group. Renal insufficiency was more common in elderly patients (7/100, 7.0% vs 25/100, 25.0%, P<0.001). A PCI was done in 85 patients (85/200, 42.5%).
  | Figure 1 Differences of patients’ expectations on a 5-point scale according to age. |
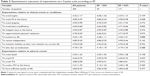
Overall rankings of the specific items were very high (Table 1). Of all patients the item “to avoid death” (3.93±1.32) was rated lowest followed by “to take less medication” (4.18±1.20). The item “to maintain mobility so that I can maintain my current life” was ranked highest (4.93±0.28), followed by “to remain independent” (4.89±0.43) and “to avoid MI in the future” (4.89±0.39). Regarding common cardiac endpoints “to avoid PCI in the future” (3.41±1.39) was rated lowest and “to avoid stroke” (4.86±0.58) was rated highest, before the item “to have sufficient quality of life” (4.84±0.47).
There were significant differences found between age groups in six of the ten proposed items (Table 1, Figure 1). All proposed items were rated lower in patients ≥80 years than in younger patients. The following parameters were significantly different between age groups: 1) to avoid myocardial infarction in the future (P<0.001); 2) to avoid heart insufficiency (P=0.002); 3) to regain/maintain physical resistance (P=0.022); 4) to extend my life (P=0.009); and 5) to maintain mobility so that I can maintain my current life (P=0.010). Item 10 “to take less co-medication” was rated lowest by the elderly patients group (4.37±1.08 vs 3.99±1.29, P=0.026).
In the younger group “to avoid MI in the future” (4.99±0.10), followed by “to maintain mobility, so that I can maintain my current life” (4.98±0.14) were ranked highest. In contrary to that, elderly patients did rank the same item highest, but “to maintain mobility to maintain my current life”, was ranked highest.
Regarding “hard cardiac endpoints” two items were significantly different (Table 1, Figure 2): “to avoid death” 4.21±1.23 vs 3.65±1.36 (P=0.001) and “to avoid MI” 4.76±0.65 vs 4.52±0.84 (P=0.006). In contrary to differences between age groups, in all other subgroups: male and female (Table 2), patients with normal or reduced ejection fractions (Table 3) and prior history of CAD (Table 4) there were basically no significant differences. Except for one comparison in the gender subgroup analysis which revealed that women would like to remain more independent (4.99±0.13 vs 4.83±0.54, P=0.010).
An analysis of patients with PCI and angiography only, was also conducted which did not reveal any significant differences in patients’ perceptions.
Discussion
Patient perceptions regarding the most beneficial expected effects of invasive cardiac procedures differed significantly between age groups but not between other subgroups such as gender or history of prior PCI and between patients with normal or reduced EF.
The most recent guidelines on myocardial revascularization (Windecker et al11) point out the importance of the process of medical decision making and patient information under consideration of institutional and, especially patient-related factors. They recommend, that “treatment decisions should not be based solely on research results …, since active patient participation in the decision making process may yield better outcomes” and further, “patients may have limited understanding of their disease … and sometimes unreasonable expectations with regard to the outcomes of a proposed intervention.” Therefore a profound knowledge of patients’ perceptions, especially in the elderly, and the fact that we are facing a growing aging population, it is essential to find out how patients before CA/DA have to be advised.
A quick glance at the differences between the younger and the elderly patients reveals, that overall, the perception scores were numerically lower in the elderly. This means that most likely, the elderly had a tendency to score lower. Hence, this attitude in the elderly age group may also have contributed to the observed differences.
Overall it was obvious that similar perceptions were present, with a more powerful emphasis in the younger patient group in all items. In an attempt to figure out different perceptions of elderly patients, which would help to define alternative endpoints for elderly patients, patient expectations did not show differences in estimated outcomes for this patient group.
This is the first study to investigate differences in perceptions between elderly and younger patients receiving cardiac interventions. Therefore, a comparison with the literature is not possible. Interestingly all other subgroups did not show any significant differences. Regarding the total population, our findings are not completely consistent with other studies. Some questions, which were rated to be most important in other studies8 such as improved survival and prevention of a MI, were not rated highest in our survey. In another study,12 71% of the participants expected that the intervention would extend their life and 75% that it would prevent a heart attack. In a multicenter study, conducted by Whittle et al,10 83% of the participants thought that the PCI would extend their life. The most recent study, conducted by Rothberg et al,13 found that 82% of 153 patients with stable CAD thought that the intervention would reduce the risk for MI. There are several possible reasons for this finding. Firstly, expectations depend mainly on the information the patients receive prior to the procedure. This is basically the process of receiving informed consent. Secondly, they are also related to the contact between patient and general practitioner, who initiates the referral of the patient to the hospital. Furthermore, the patient does not know cardiac endpoints commonly used by cardiologists when conducting studies in this setting. This is reflected by the ranking attributed to “hard” cardiac endpoints, when the most important issue was not a prolongation of life but quality of life. Interestingly, this was the case in all subgroups, with the lowest emphasis in elderly patients. Therefore, the value of evidence-based benefits of PCI as prevention of myocardial infarction and of common cardiac endpoints, ie, cardiac death and stroke for the patient remains unclear. Holmboe et al12 conducted a study in which many patients expected that pain relief would be the most likely consequence of the intervention. Furthermore, they found no correlation between age and the belief that PCI would prolong life. In a study investigating the effect of decision making the authors found that the single most important consideration was whether a given treatment would increase life expectancy.12 Patients had high expectations for their chosen treatment regarding a prolonged life and the prevention of future MIs. This finding, that patients overestimate the benefits of coronary intervention is consistent with other studies.10–14 Kureshi et al8 found that patients predominantly believed that the procedure would extend their life and prevent a heart attack. In the same study two thirds of the patients noted symptom relief as a benefit of the procedure and only 1% identified this as the only benefit of the procedure.
In our study we did not observe the informed consent process or the discussions the primary physician had with the patient. This precluded us from knowing how the decision was made. Even though complaints of the patients were evaluated during the admission process and differed in an elderly population compared to younger counterparts, perceptions in the elderly were the same only on a lower level. Based on this finding, it would be worthwhile to further elucidate the question why these lower perception scores were observed. This, however, leads us into the arena of geriatric psychology which will be difficult to discuss in an adequate manner. Hirsch et al15 for instance studied optimism and pessimism as potential moderators for depression in older primary care patients. Therefore, without being trained in psychological methods, our perception scores can only be a “bird’s eye view” on the clinical landscape of PCI patients.
To define factors, which may be more effective and more suitable to predict outcomes after coronary procedures in elderly patients, patient perceptions are not deemed to be helpful in this respect, and other items regarding outcomes like the reduction of functional decline and frailty may be more effective, to define different outcome measures in elderly patients.
Limitations
This survey was conducted at a single center and our results may differ from other cardiac centers. Furthermore, patients’ differing levels of medical knowledge and/or the level of education may have introduced some bias. Moreover, the differences in how the informed consent process was interpreted could also have affected the results as compared to findings of various authors. According to the protocol we performed a comparison of patients with prior coronary angiography and/or PCI and those who had not experienced such an examination. We did not perform a comparison of patients with angina pectoris and silent ischemia. This remains a limitation. Since evidence for the evaluation of patients’ perceptions is rare, plenty of possible adequate citations are missing. The reason to add the item expectation relative to adverse events was, however, the assumption that the patients’ view was not necessarily comparable to the value of a commonly accepted cardiac endpoint from the perspective of the physician.
Conclusion
In our survey we found significant differences in patient expectations between elderly and younger patients regarding the outcome of coronary angiography/coronary intervention. Future research, especially in the elderly should aim to identify patient expectations in any therapy of coronary artery disease so that the patients’ wishes and expectations can be respected.
Disclosure
The authors report no conflicts of interest in this work.
References
Peterson ED, Alexander KP, Malenka DJ, et al. American Heart Association Chronic CAD Working Group. Am Heart J. 2004;148(3):486–492. | ||
Weintraub WS, Veledar E, Thompson T, Burnette J, Jurkovitz C, Mahoney E. Percutaneous coronary intervention outcomes in octogenarians during the stent era (National Cardiovascular Network). Am J Cardiol. 2001;88(12):1407–1410. | ||
Hassani SE, Wolfram RM, Kuchulakanti PK, et al. Percutaneous coronary intervention with drug-eluting stents in octogenarians: characteristics, clinical presentation, and outcomes. Catheter Cardiovasc Interv. 2006;68(1):36–43. | ||
Rittger H, Hochadel M, Behrens S, et al. Interventional treatment and outcome in elderly patients with stable coronary artery disease. Results from the German ALKK registry. Herz. 2014;39(2):212–218. | ||
Rittger H, Rieber J, Breithardt OA, et al. Influence of age on pain perception in acute myocardial ischemia: a possible cause for delayed treatment in elderly patients. Int J Cardiol. 2011;149(1):63–67. | ||
Ambepitiya G, Roberts M, Ranjadayalan K, Tallis R. Silent exertional myocardial ischemia in the elderly: a quantitative analysis of anginal perceptual threshold and the influence of autonomic function. J Am Geriatr Soc. 1994;42(7):732–737. | ||
Tresch DD, Brady WJ, Aufderheide TP, Lawrence SW, Williams KJ. Comparison of elderly and younger patients with out-of-hospital chest pain. Arch Intern Med. 1996;156(10):1089–1093. | ||
Kureshi F, Jones PG, Buchanan DM, Abdallah MS, Spertus JA. Variation in patients’ perceptions of elective percutaneous coronary intervention in stable coronary artery disease: cross sectional study. BMJ. 2014;349:g5309. | ||
Liao L, Jollis JG, Delong ER, Peterson ED, Morris KG, Mark DB. Impact of an interactive video on decision making of patients with ischemic heart disease. J Gen Intern Med. 1996;11(6):373–376. | ||
Whittle J, Conigliaro J, Good CB, Kelley ME, Skanderson M. Understanding of the benefits of coronary revascularization procedures among patients who are offered such procedures. Am Heart J. 2007;154(4):662–668. | ||
Windecker S, Kolh P, Alfonso F, et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014;35(37):2541–2619. | ||
Holmboe ES, Fiellin DA, Cusanelli E, Remetz M, Krumholz HM. Perceptions of benefit and risk of patients undergoing first-time elective percutaneous coronary revascularization. J Gen Intern Med. 2000;15(9):632–637. | ||
Rothberg MB, Sivalingam SK, Ashraf J, et al. Patients’ and cardiologists’ perceptions of the benefits of percutaneous coronary intervention for stable coronary disease. Ann Intern Med. 2010;153(5):307–313. | ||
Lee JH, Chuu K, Spertus J, et al. Patients overestimate the potential benefits of elective percutaneous coronary intervention. Mo Med. 2012;109(1):79–84. | ||
Hirsch JK, Walker KL, Wilkinson RB, Lyness JM. Family criticism and depressive symptoms in older adult primary care patients: optimism and pessimism as moderators. Am J Geriatr Psychiatry. 2014;22(6):632–635. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.