Back to Journals » Patient Preference and Adherence » Volume 15
Differences in Lung Cancer Treatment Preferences Among Oncologists, Patients and Family Members: A Semi-Structured Qualitative Study in China
Authors He X, Zhang M, Wu J, Xu S , Jiang X, Wang Z, Zhang S, Xie F
Received 27 December 2020
Accepted for publication 16 March 2021
Published 15 April 2021 Volume 2021:15 Pages 775—783
DOI https://doi.org/10.2147/PPA.S299399
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Naifeng Liu
Xiaoning He,1,2 Mengqian Zhang,1,2 Jing Wu,1,2 Song Xu,3 Xiangli Jiang,4 Ziping Wang,5 Shucai Zhang,6 Feng Xie7,8
1School of Pharmaceutical Science and Technology, Tianjin University, Tianjin, People’s Republic of China; 2Center for Social Science Survey and Data, Tianjin University, Tianjin, People’s Republic of China; 3Department of Lung Cancer Surgery, Tianjin Key Laboratory of Lung Cancer Metastasis and Tumor Microenvironment, Lung Cancer Institute, Tianjin Medical University General Hospital, Tianjin, People’s Republic of China; 4Tianjin Medical University Cancer Institute & Hospital, Tianjin, People’s Republic of China; 5Department of Medical Oncology, Cancer Institute (Hospital), Chinese Academy of Medical Sciences & Peking Union Medical College, Beijing, People’s Republic of China; 6Department of Medical Oncology, Beijing Chest Hospital, Beijing, People’s Republic of China; 7Department of Health Research Methods, Evidence and Impact, McMaster University, Hamilton, ON, Canada; 8Centre for Health Economics and Policy Analysis, McMaster University, Hamilton, ON, Canada
Correspondence: Jing Wu
School of Pharmaceutical Science and Technology, Tianjin University, No. 92 Weijin Road, Nankai District, Tianjin, 300072, People’s Republic of China
Tel +862227405176
Fax +862287401830
Email [email protected]
Background: Cancer treatment decision-making often needs to balance benefits, harms, and costs. This study sought to identify the differences in cancer treatment preference among oncologists, patients and their family members in China.
Methods: A semi-structured face-to-face qualitative interview was conducted among oncologists, patients and their family members recruited in four tertiary hospitals in China. The interview guide was developed based on literature review and expert consultation. Participants were asked to indicate their preferences when making lung cancer treatment decisions. All interviews were audio-taped, transcribed verbatim, and thematic analyzed. The preferences were compared among three groups of participants.
Results: A total of 17 participants (5 oncologists, 6 dyads of patients and family members) were interviewed between June and July 2019. Five themes, namely, survival benefit, adverse effect/symptom, treatment process, treatment cost, and the impact on daily life were identified. The oncologists and family members gave highest priority on survival benefit, while the patients are concerned most about treatment cost and quality of life.
Conclusion: This study reveals different preferences for cancer treatment among oncologists, patients and their family members in China. Education is needed to empower patients and family members and promote share decision-making in this country.
Keywords: lung cancer, preference, qualitative interview, survival benefit, cost
Introduction
Lung cancer is the leading cause of cancer incidence and mortality, with 2.1 million new cases and causing 1.76 million deaths worldwide in 2018. In China, lung cancer accounts for 18.1% of new cancer cases and 24.1% of cancer deaths.1,2 The 5-year survival rate among patients with lung cancer was estimated at 19.8% in China.3 During the past 20 years, target therapies and immunotherapies have greatly improved the prognoses and outcomes of cancer patients.4,5 Nevertheless, these new therapies also impose significant burdens on patients including adverse events, mental stresses, and financial worries.6,7 When making treatment decisions, a trade-off between treatment benefits (eg, extended survival) and burdens (eg, adverse effect, cost) has to be made.
As we are thriving to establish a patient-centered healthcare system, clinical decision-making is shifting from the paternalistic model in which physicians dominated the treatment decision to shared decision-making between physicians and patients.8–10 However, many patients may still not feel comfortable of expressing their preference which limits the development and implementation of sharing decision-making.11 In China, family members are playing an important role in making treatment decisions.12 Moreover, family members may discuss the disease condition and treatment choice with oncologists,13 without involving the patient.14 As a result, some cancer patients are not even aware of the diagnosis.15 However, oncologists and family members may perceive the needs and preferences for treatments differently from the patient. Studies conducted in Italy and Australia reported that lung cancer patients were more willing to receive a treatment with small survival benefit than what their oncologists expected.16,17 Existing studies comparing the preferences between oncologists and lung cancer patients16–18 often focused on the attitudes/preferences for specific treatment regimens such as adjuvant chemotherapy, or treatment attributes such as overall survival (OS) and treatment convenience. No preference study has considered overall treatment benefits and risks for lung cancer. Moreover, little research has been conducted in China to understand the preferences of family members of cancer patients. In order to improve lung cancer treatment decision-making in China, we conducted a qualitative study to investigate and compare lung cancer treatment preferences among oncologists, patients and family members.
Methods
Qualitative face-to-face semi-structured interviews were conducted separately with lung cancer specialists, patients and their family members. Oncologists, patients and family members were asked to rank the factors mentioned at the end of the interview. A number of themes were developed through thematic analysis. The rank of different themes was concluded to ascertain preference differences.
Participants
Lung cancer patients, their attending oncologists and family members were recruited in four tertiary hospitals in Tianjin and Beijing, two large cities in China, between June and July 2019. The inclusion criteria for patients were age ≥18, diagnosed with lung cancer, currently on treatment, and without communication barriers. We used the quota sampling to ensure there was a reasonable diversity among participants in each group, for example, years of practice for oncologist, and disease stage and urban vs rural residents (the specific quota could be seen in Supplementary Table 1). The inclusion criteria for oncologists are having lung cancer treatment experience and meeting quotas in terms of gender and academic title. In order to meet the maximum variation principle,19 each quota should have at least one participant. One family member of each participating patients was invited to the interview as well.
Semi-Structured Interview
An interview guide was developed based on a literature review and feedback from pilot interviews with two specialists in lung cancer (full guide could be seen in Supplementary Materials). By following the guide, the interview consisted of three steps. First, basic demographic characteristics of the participants were collected. Second, open-ended questions were used to ask participants to talk about their communication process for treatment decision-making, factors they considered important when selecting treatment regimens, and their experiences and expectations of cancer treatments received. Third, the interviewer went over the information collected with the participant to ensure all was correct and accurate. And the participant was asked to rank the factors they mentioned from most to least important, and state the reasons.
Data Collection
Eligible oncologists in the participating hospitals were first approached. Through the referral of the oncologists, the patients and family members were contacted for interview when the patient received treatment in the hospital. All participants provided the informed consent prior to the interview. One-to-one interviews in Chinese were undertaken in the private rooms of the hospitals by two researchers (XH and MZ). The Institutional Review Board of Tianjin University and both participating hospitals approved this study. The interviews followed the principles of the Declaration of Helsinki.
Data Analysis
All interviews were audiotaped and transcribed verbatim in Chinese. Thematic analysis was used to analyze the data. The important factors in decision-making described by participants were coded from the electronic transcript. We also calculated the frequency of every code. Inductive themes were then identified. The overall ranking of factors was derived by averaging over the rankings made by all participants in each group. The codes and themes were translated into English and further audited by a bilingual reviewer. We compared the themes and corresponding rankings among the three groups.
Results
Characteristics of Participants
A total of 17 participants were interviewed, including five lung cancer oncologists, six dyads of lung cancer patients and their family members. Oncologists and patients met the prespecified quota requirements (Supplementary Table 2). As shown in Table 1, participating oncologists included resident physicians (n=2), attending physicians (n=2) and associate chief physician (n=1) in the surgical or medical oncology department, and their practicing years ranged from 5 to 22 years. Demographics of patients and family members are described in Table 2. The age of patient participants ranged from 35 to 66 years, with a median age of 56 years. Patients were in locally advanced stage (n=2) or advanced stage (n=4) of lung cancer, and their duration of illness varied from 0.5 to 24 months. Their monthly income ranged from ≤CNY2,000 (US$300) to >CNY10,000 (US$1501). Most patients live in urban areas (n=4) and have the Urban Employee Basic Medical Insurance (UEBMI)20 (n=5). Patients had received a wide range of treatments, including surgical resection, chemotherapy, targeted therapy and immune therapy. Participating family members are patients’ spouses (n=4) or adult children (n=2). The detailed information for each participant is shown in Supplementary Tables 3 and 4.
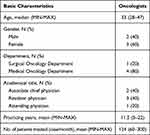 |
Table 1 Demographics of Oncologists |
 |
Table 2 Demographics of Patients and Family Members |
Themes Related to Treatment Preferences
A total of 84 codes were identified and grouped into five themes, namely, survival benefit, adverse effect/symptom, treatment process, treatment cost, and the impact on daily life. Table 3 shows the explanations of these themes and the codes with frequency. The survival benefit theme includes 14 codes and the most frequently mentioned was “overall survival/survival time (n=12)”. There are 54 codes related to adverse effect/symptom, which are grouped into sub-themes according to the site of adverse effects or symptoms occurred. The treatment process theme includes seven codes, where “mode of administration (n=8)” was the most frequently mentioned. The treatment cost theme has only two codes: “costs” and “cost-effectiveness”. Seven codes are related to the impact on daily life with “appetite (n=8)” being the most frequent one.
 |
Table 3 The Explanations of Every Theme and Their Codes with Frequency |
Difference in Treatment Preferences Among Oncologists, Patients and Family Members
Survival vs Cost
The oncologists and five family members all considered survival benefit as the first priority. One oncologist indicated that “From a medical point of view, the maximization of treatment effect is definitely the most important.” (D1), “Treatment effect is our key concern. The primary objective is to control the disease and prolong overall survival.” (D5). Family members expressed that “[When making decision] The most concern is survival. Nothing is more important than being alive for a cancer patient.” (R1), “I wish the treatment could control the disease and keep him alive.” (R5).
In contrast, survival benefit was considered most important by two patients versus cost by the remaining four patients. A patient stated that
Life is the first consideration. While under this circumstance, we are trading our savings for more life years. The treatment cost will impose a huge economic burden on my family that is the biggest concern for me. Personally, I prefer receiving no treatment and maintaining the status quo as long as possible. (P2)
“[For lung cancer treatment] My first consideration is cost. I will never allow my family fall into poverty because of this disease.” (P4). One patient mentioned “cost-effectiveness”. “[When choosing a treatment] Cost-effectiveness should be within a reasonable range, otherwise, this treatment would not be acceptable.” (P4).
The oncologists were less concerned about the cost and ranked it as the fourth important factor. An oncologist explained that
For targeted therapy, most drugs could be compensated by medical insurance, and almost 90% patients could afford. For new developed and high-priced immunotherapy, 30%-40% patients may not be able to afford. (O3)
Similar preferences were also expressed by the family members who ranked the cost as the second important factor.
Cost is not a big problem. If our salaries are not enough, we can sell our house property. Life is meaningless without your loved one. We will continue the treatment no matter how much it will spend. (F6)
Treatment cost is not a main factor for now. The drugs in first course of treatment will be covered by medical insurance. And the subsequent treatment could almost be afforded, even without the insurance coverage. (F4)
Adverse Events/Symptoms and Quality of Life
Adverse events/symptoms and quality of life are important factors for patients when making treatment decisions. One patient expressed his worry about adverse events before receiving treatment,
I am very concerned about the adverse effects. I was told that the [chemotherapy] treatment always has side effects, losing hair and weight. It is horrible to experience these and many people cannot bear. (P1)
Another patient who was sensitive to adverse events or symptoms expressed a stronger worry, “When I was in chemotherapy, I almost gave up. I went through four treatment cycles and the adverse events made me want to die.” (P5). This patient also described the impacts of treatments on his quality of life, “After a cycle of treatment, I couldn’t get out of bed nearly for three days. I cannot event take a sip of water, and nearly ate nothing for one week.” (P5). Patients would reject some effective but painful treatments, avoiding physical inconveniences, psychological discomfort, and dignity loss. One patient said
The second important consideration is the quality of my daily life. The length of life is determined by the quality of life. Better quality of life is more important than a longer survival. (P4)
For the oncologists, adverse events/symptoms and quality of life were ranked as the secondary and third considerations, while life-threatening adverse events were most concerning. An oncologist said that “From my perspective, I will focus on those serious adverse events or symptoms. Mild events are either transient or can be controlled by medications.” (O2). Another oncologist said “Quality of life is also an important indicator of treatment effect, which is however sometimes neglected by many physicians.” (D1).
Family members paid less attention to adverse events/symptoms and quality of life by ranking them as the fifth and fourth factors, respectively. One said that “occurrence of an adverse event is a probabilistic question. And it may not be predicted exactly.” (F4). Another family member mentioned that “I do not care adverse effects. My father is a very brave man. He also knowns potential adverse effects and he can bear.” (F1). Another family member expressed that
Among the options of 5 years survival with good quality of life and 10 years survival with poor quality of life, the latter one is definitely selected. Being alive is an essential precondition before we consider quality of life. (F1)
Treatment Process
Treatment process was also considered but ranked last consistently by all participants. An oncologist mentioned that “The length of hospital stay is under my consideration. ‘Quick recovery’ with shorter hospital stays will bring benefits to the patients.” (D1). One family member said “Medical care capacity is also under my consideration. Oncologists in high level hospitals may provide better treatment.” (C6).
Discussion
Our study found that cost, adverse effects/symptoms, and impact on quality of life are the most important factors for the patients compared with survival by oncologists and family members when considering cancer treatment in China. This qualitative study provides an in-depth understanding of the differences in treatment preferences between patients and their physicians and family members.
Survival benefit is the most important factor for selecting cancer treatments by the oncologists. There are similar findings from previous studies conducted in China, the USA, and Japan.21–23 This is shared by family members who hope their loved ones could live longer.24,25 Chinese culture is deeply shaped by Confucian philosophy in which family is the core element of society. Caring for elderly parents is a key definition in Chinese filial piety.26 Therefore, it is not surprising to observe this preference among family members.
Indeed, the rising cost of cancer treatments is imposing a significant burden on cancer patients worldwide.27,28 A study by the Association of Oncology Social Work indicates that 40% of cancer patients report that the cost of therapy in the last year used up all their savings.29 Lang found that the willingness to pay for lung cancer treatments by Chinese patients was lower than the actual price of the treatment.30 However, previous preference studies have been focusing on survival, adverse events and treatment process, rather than cost.18,31,32 But cost is an important factor in understanding the patient’s treatment preference in China due to varied public insurance coverage and the copayment by Chinese patients.
We found that quality of life is a key factor when making treatment decisions for Chinese patients. There were similar findings in western countries.33–35 Improvement in quality of life has been increasingly recognized as an important outcome in oncology randomized controlled trials (RCTs)36,37 and clinical guidelines.38
Difference in cancer treatment preferences between patients and their physicians and family members highlights the need and importance for promoting shared decision-making in China. The awareness of patient-centered model among Chinese health care professionals has been improved noticeably that they stated patient preference is more important in decision-making. Education is needed to make patients and family members aware of the difference in their preference and the importance of engaging patients in the decision-making. Physicians could play an important role in promoting this by encouraging patients and family members to actively participate in the decision-making. Social media could be another means to improve the awareness of the concept of shared decision-making among the general public.39
To promote shared decision-making, family members’ role also should be guided to change from the direct surrogates to helpers of patients. Their over-involvement may overstep and infringe upon the patient’s role in decision-making, despite with good intentions. As one patient in the interview claimed, “I am entitled to be informed all of the alternative treatments before they made the decision. This is my life”. Family members may also obscure or repress patients’ preference and unduly pressured patients to adopt their own preferences.40 Some patients would not express their real preference, in fear of letting down family members’ expectations or imposing burdens to the family.
The major limitation of this study is the small sample size. We experienced difficulty in recruiting patients and family members despite the effort. This small sample size also limited the representativeness even with the quota sampling. All of the participants in our study were recruited from tertiary hospitals in Beijing and Tianjin, which are both megacities with highly economic and medical development in north China. It is not clear how similar or different the treatment preferences are among those from less developed places.
Conclusion
This study reveals different preferences for cancer treatment between oncologists, patients and their family members in China. Education is needed to empower patients and family members and promote shared decision-making in this country.
Ethics Approval and Informed Consent
The study was performed in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study. Ethical approval was obtained by the Safety and Ethics Committee of School of Pharmaceutical Science and Technology in Tianjin University and all research hospitals (Tianjin Medical University General Hospital and Tianjin Medical University Cancer Institute & Hospital).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by the National Natural Science Foundation of China (No. 71673197 & No. 71804122).
Disclosure
The authors declare that they have no competing interests.
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68(6):394–424. doi:10.3322/caac.21492
2. World Health Organization. International agency for research on cancer. China fact sheets; 2018. Available from: https://gco.iarc.fr/today/data/factsheets/populations/160-china-fact-sheets.pdf.
3. Allemani C, Matsuda T, Di Carlo V, et al. Global surveillance of trends in cancer survival 2000–14 (CONCORD-3): analysis of individual records for 37 513 025 patients diagnosed with one of 18 cancers from 322 population-based registries in 71 countries. Lancet. 2018;391(10125):1023–1075.
4. Yang S, Zhang Z, Wang Q. Emerging therapies for small cell lung cancer. J Hematol Oncol. 2019;12(1):47. doi:10.1186/s13045-019-0736-3
5. Duma N, Santana-Davila R, Molina JR. Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin proc. 2019;94(8):1623–1640. doi:10.1016/j.mayocp.2019.01.013
6. Steven A, Fisher SA, Robinson BW. Immunotherapy for lung cancer. Respirology. 2016;21(5):821–833. doi:10.1111/resp.12789
7. Ricciardi S, Tomao S, de Marinis F. Toxicity of targeted therapy in non-small-cell lung cancer management. Clin Lung Cancer. 2009;10(1):28–35. doi:10.3816/CLC.2009.n.004
8. Barry MJ, Edgman-Levitan S. Shared decision making–pinnacle of patient-centered care. N Engl J Med. 2012;366(9):780–781. doi:10.1056/NEJMp1109283
9. Frosch DL, Kaplan RM. Shared decision making in clinical medicine: past research and future directions. Am J Prev Med. 1999;17(4):285–294. doi:10.1016/S0749-3797(99)00097-5
10. Emanuel EJ, Emanuel LL. Four models of the physician-patient relationship. JAMA. 1992;267(16):2221–2226. doi:10.1001/jama.1992.03480160079038
11. Ting X, Yong B, Yin L, Mi T. Patient perception and the barriers to practicing patient-centered communication: a survey and in-depth interview of Chinese patients and physicians. Patient Educ Couns. 2016;99(3):364–369. doi:10.1016/j.pec.2015.07.019
12. Rui D. A family-oriented decision-making model for human research in Mainland China. J Med Philos. 2015;40(4):400–417. doi:10.1093/jmp/jhv013
13. Lin ML, Huang CT, Chen CH. Reasons for family involvement in elective surgical decision-making in Taiwan: a qualitative study. J Clin Nurs. 2017;26(13–14):1969–1977. doi:10.1111/jocn.13600
14. Hobbs GS, Landrum MB, Arora NK, et al. The role of families in decisions regarding cancer treatments. Cancer. 2015;121(7):1079–1087. doi:10.1002/cncr.29064
15. Hahne J, Liang T, Khoshnood K, Wang X, Li X. Breaking bad news about cancer in China: concerns and conflicts faced by doctors deciding whether to inform patients. Patient Educ Couns. 2020;103(2):286–291. doi:10.1016/j.pec.2019.08.022
16. Pacchiana MV, Capelletto E, Carnio S, et al. Patients’ attitudes and physicians’ perceptions toward maintenance therapy for advanced non-small-cell lung cancer: a multicenter Italian survey. Clin Lung Cancer. 2017;18(4):381–387. doi:10.1016/j.cllc.2016.10.002
17. Blinman P, Hughes B, Crombie C, et al. Patients’ and doctors’ preferences for adjuvant chemotherapy in resected non-small-cell lung cancer: what makes it worthwhile? Eur j Cancer. 2015;51(12):1529–1537. doi:10.1016/j.ejca.2015.05.022
18. McMullen S, Hess LM, Kim ES, et al. Treatment decisions for advanced non-squamous non-small cell lung cancer: patient and physician perspectives on maintenance therapy. patient. 2019;12(2):223–233. doi:10.1007/s40271-018-0327-3
19. Teddlie C, Yu F. Mixed methods sampling. J Mix Methods Res. 2016;1:77–100. doi:10.1177/1558689806292430
20. Sun Y, Gregersen H, Yuan W. Chinese health care system and clinical epidemiology. Clin Epidemiol. 2017;9:167–178. doi:10.2147/CLEP.S106258
21. Sun H, Wang H, Shi L, et al. Physician preferences for chemotherapy in the treatment of non-small cell lung cancer in China: evidence from multicentre discrete choice experiments. BMJ Open. 2020;10(2):e032336. doi:10.1136/bmjopen-2019-032336
22. Gonzalez JM, Doan J, Gebben DJ, Boeri M, Fishman M. Comparing the relative importance of attributes of metastatic renal cell carcinoma treatments to patients and physicians in the united states: a discrete-choice experiment. PharmacoEconomics. 2018;36(8):973–986. doi:10.1007/s40273-018-0640-7
23. Bolt T, Mahlich J, Nakamura Y, Nakayama M. Hematologists’ preferences for first-line therapy characteristics for multiple myeloma in Japan: attribute rating and discrete choice experiment. Clin Ther. 2018;40(2):296–308.e292. doi:10.1016/j.clinthera.2017.12.012
24. Wieland J, Hoppe BS, Rausch-Osian SM, et al. Survivor and caregiver expectations and preferences regarding lung cancer treatment. Int j Part Ther. 2019;6(2):42–49. doi:10.14338/IJPT-19-00072.1
25. Jen W-Y, Yoong J, Liu X, Tan MSY, Chng WJ, Chee Y-L. Qualitative study of factors affecting patient, caregiver and physician preferences for treatment of myeloma and indolent lymphoma. Patient Prefer Adherence. 2020;14:301–308. doi:10.2147/PPA.S241340
26. Leng J, Lui F, Chen A, Huang X, Gany F. Adapting meaning-centered psychotherapy in advanced cancer for the Chinese immigrant population. J Immigrant Minority Health. 2017;20(11 Suppl):1–7.
27. Somers C, Chimonas S, McIntosh E, Kaltenboeck A, Briggs A, Bach P. Using nominal group technique to identify key attributes of oncology treatments for a discrete choice experiment. MDM Policy Pract. 2019;4(1):2381468319837925. doi:10.1177/2381468319837925
28. Lee JY, Kim K, Lee YS, et al. Treatment preferences of advanced ovarian cancer patients for adding bevacizumab to first-line therapy. Gynecol Oncol. 2016;143(3):622–627. doi:10.1016/j.ygyno.2016.10.021
29. Smith SK, Nicolla J, Zafar SY. Bridging the gap between financial distress and available resources for patients with cancer: a qualitative study. J Oncol Pract. 2014;10(5):e368–e372. doi:10.1200/JOP.2013.001342
30. Lang HC. Willingness to pay for lung cancer treatment. Value Health. 2010;13(6):743–749. doi:10.1111/j.1524-4733.2010.00743.x
31. Schmidt K, Damm K, Vogel A, et al. Therapy preferences of patients with lung and colon cancer: a discrete choice experiment. Patient Prefer Adherence. 2017;11:1647–1656. doi:10.2147/PPA.S138863
32. Muhlbacher AC, Bethge S. Patients’ preferences: a discrete-choice experiment for treatment of non-small-cell lung cancer. Eur J Health Econ. 2015;16(6):657–670. doi:10.1007/s10198-014-0622-4
33. Bridges J, Cruz M, Pavilack M. et al. Patient preferences for attributes of tyrosine kinase inhibitor treatments for EGFR mutation-positive non-small-cell lung cancer. Future Oncol;2019. 15. doi: 10.2217/fon-2019-0396
34. Tong BC, Wallace S, Hartwig MG, D’Amico TA, Huber JC. Patient preferences in treatment choices for early-stage lung cancer. Ann Thorac Surg. 2016;102(6):1837–1844. doi:10.1016/j.athoracsur.2016.06.031
35. Gerber DE, Hamann HA, Rasco DW, Woodruff S, Lee SJ. Patient comprehension and attitudes toward maintenance chemotherapy for lung cancer. Patient Educ Couns. 2012;89(1):102–108. doi:10.1016/j.pec.2012.04.013
36. Polanski J, Jankowska-Polanska B, Rosinczuk J, Chabowski M, Szymanska-Chabowska A. Quality of life of patients with lung cancer. Onco Targets Ther. 2016;9:1023–1028. doi:10.2147/OTT.S100685
37. Gralla RJ, Griesinger F. Interpreting clinical trials in lung cancer: impact of methodology and endpoints. J Thorac Oncol. 2007;2(Suppl 2):S51–S58. doi:10.1097/01.JTO.0000269734.27047.3e
38. Camps C, Del Pozo N, Blasco A, Blasco P, Sirera R. Importance of quality of life in patients with non-small-cell lung cancer. Clin Lung Cancer. 2009;10(2):83–90. doi:10.3816/CLC.2009.n.010
39. Longtin Y, Sax H, Leape LL, Sheridan SE, Donaldson L, Pittet D. Patient participation: current knowledge and applicability to patient safety. Mayo Clin proc. 2010;85(1):53–62. doi:10.4065/mcp.2009.0248
40. Ho A. Relational autonomy or undue pressure? Family’s role in medical decision-making. Scand J Caring Sci. 2008;22(1):128–135. doi:10.1111/j.1471-6712.2007.00561.x
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
