Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 16
Differences in Demographic and Clinical Characteristics Among Subtypes of Female Pattern Hair Loss
Authors Sakpuwadol N , Tejapira K , Kositkuljorn C, Pomsoong C , Suchonwanit P
Received 21 May 2023
Accepted for publication 30 July 2023
Published 7 August 2023 Volume 2023:16 Pages 2073—2082
DOI https://doi.org/10.2147/CCID.S422335
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jeffrey Weinberg
Nawara Sakpuwadol, Kasama Tejapira, Chaninan Kositkuljorn, Cherrin Pomsoong, Poonkiat Suchonwanit
Division of Dermatology, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Poonkiat Suchonwanit, Division of Dermatology, Department of Medicine, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Ratchathewi, Bangkok, 10400, Thailand, Tel +66-2-2011141, Fax +66-2-201-1211 ext 4, Email [email protected]
Background: Female pattern hair loss (FPHL) is the most common hair loss disorder in women that can be classified into three patterns, including Ludwig, Olsen, and Hamilton-Norwood subtypes. Information regarding the comparison of demographics, clinical characteristics, and associated comorbidities among subtypes of FPHL is scarce and contradictory.
Objective: To evaluate and compare the epidemiology, clinical manifestations, and comorbid conditions of FPHL subtypes and determine their associated factors.
Methods: This retrospective study included patients who were diagnosed with FPHL between January 2000 and November 2021. Participants were classified into three subtypes, namely Ludwig, Olsen, and Hamilton-Norwood, and were statistically compared. Variables significantly associated with each FPHL subtype were identified using multivariable multinomial logistic regression analysis.
Results: Among the 519 patients with FPHL, the Ludwig subtype was the most prevalent (51.1%), followed by the Olsen (32.9%) and Hamilton-Norwood (16%) subtypes. The Hamilton-Norwood subtype revealed significantly higher frequencies of early disease onset (61.4%), menstrual irregularity (22.9%), polycystic ovary syndrome (PCOS, 18.1%), and seborrhea (30.1%) but lower frequencies of overweight (24.1%) and type 2 diabetes mellitus (DM, 2.4%). Multivariable multinomial regression analysis demonstrated that the Hamilton-Norwood subtype was a predictor for early disease onset and PCOS compared to Ludwig (early onset: odds ratio (OR) = 2.14, 95% confidence interval (CI) = 1.39– 4.22, P = 0.02; PCOS: OR = 2.02, 95% CI = 1.55– 4.84, P = 0.03), and Olsen (early onset: OR = 1.89, 95% CI = 1.03– 3.92, P = 0.04; PCOS: OR = 2.24, 95% CI = 1.89– 5.31, P = 0.01). In contrast, the Hamilton-Norwood pattern was at decreased risk for type 2 DM compared to Ludwig (OR = 0.51, 95% CI = 0.03– 0.82, P = 0.02), and Olsen (OR = 0.68, 95% CI = 0.04– 0.79, P = 0.03).
Conclusion: The Ludwig pattern was found to be the most prevalent FPHL subtype among Thai patients. Moreover, the Hamilton-Norwood subtype was associated with early disease onset and PCOS, whereas the Ludwig and Olsen subtypes were associated with type 2 DM.
Keywords: AGA, androgenetic alopecia, comorbidity, FPHL, non-scarring alopecia, subtype
Introduction
Female pattern hair loss (FPHL) is the most common non-scarring alopecia in women,1 affecting approximately 50% of them during their lifetime.2 The prevalence of FPHL increases with age.3 Hair cycle changes, including progressive transformation of terminal hair to miniaturized hair, anagen phase shortening, and increasing kenogen numbers, are characteristic follicular alterations of FPHL, resulting in clinically apparent hair thinning.4,5 Although similarities exist between FPHL and male androgenetic alopecia (AGA) for follicular miniaturization, the pathogenesis of FPHL remains inconclusive.6,7 Unlike AGA, the relationship between FPHL and androgens is controversial, as evidence reveals normal hormone levels in most affected women and relatively poor treatment outcome by anti-androgen therapy.8–11 FPHL has been observed to coexist with several comorbidities, including hyperandrogenism, polycystic ovary syndrome (PCOS), metabolic syndrome, coronary artery diseases, type 2 diabetes mellitus (DM), and hypertension.12–17
FPHL can be clinically classified into three patterns, namely, Ludwig, Olsen, and Hamilton-Norwood, each with a specific severity grading.1 The Ludwig subtype is characterized by diffuse hair thinning of the centroparietal scalp with frontal hairline preservation (Figure 1A), and its severity is graded using the 3-stage Ludwig and 5-stage Sinclair scales.4 The Olsen subtype presents with diffuse centroparietal hair thinning with breaching of frontal hairline, resembling Christmas tree (Figure 1B), while the Hamilton-Norwood subtype presents recession of frontal hairline in bitemporal pattern and vertex hair thinning (Figure 1C).1 The severity of Olsen and Hamilton-Norwood patterns is assessed using the 3-stage Olsen and 7-stage Hamilton-Norwood severity scales, respectively.1
Despite the clinical relevance of distinguishing FPHL subtypes, limited data comparing the epidemiological characteristics, clinical manifestations, and associated comorbidities among FPHL subtypes are available in the literature. Previous studies reported conflicting results regarding the prevalence of hirsutism and acne among different FPHL subtypes; while Özkoca et al showed that these were more prevalent in Ludwig and Hamilton-Norwood patterns,18 Tandon et al found that both conditions were more common in Ludwig and Olsen subtypes.19 Due to this inconclusive evidence and potential significance of identifying coexisting disorders, this study aimed to investigate and compare prevalence, demographics, clinical characteristics, and co-occurring conditions among FPHL subtypes and determine their associated factors.
Materials and Methods
Study Design
This study was conducted in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the Mahidol University Institutional Review Board for Ethics in Human Research (MURA2022/778). This is a retrospective study in which all included participants were categorized based on FPHL subtypes according to the Ludwig, Olsen, and Hamilton-Norwood classifications. The requirement for informed consent was waived, and the data were anonymized before analysis.
Study Participants and Data Collection
We included patients clinically and/or histopathologically diagnosed with FPHL between January 2000 and November 2021 at the outpatient dermatology clinic at Ramathibodi Hospital, Bangkok, Thailand; a minimum follow-up time of one year was required. Data regarding age, age at onset, duration of FPHL, family history of AGA obtained from the patients (defined as having AGA or FPHL in any of the family members), FPHL subtypes, and severity according to Ludwig (with 3 stages), Olsen (with 3 stages), and Hamilton-Norwood scales (with 7 stages), and comorbidities were collected from electronic medical records from January 2000 to November 2022. Patients with incomplete medical records or coexisting hair or scalp disorders were excluded.
For analytical purposes, a modified severity grading was applied to the Hamilton-Norwood pattern: scales I–III as grade I, IV–V as grade II, and VI–VII as grade III. Participants with age at disease onset <40 years were defined as having early onset FPHL.1 Body mass index (BMI) ≥25 kg/m2 was considered overweight. Comorbidities were diagnosed based on previous specialist examinations. PCOS was diagnosed based on the Rotterdam criteria, requiring at least 2 out of the 3 following criteria: (1) ovulatory dysfunction; (2) biological or clinical signs of hyperandrogenism; and (3) the presence of polycystic ovarian morphology observed in ultrasonography. Hirsutism was assessed using the modified Ferriman-Gallwey score, evaluating nine body areas (ie, upper lip, chin, chest, upper back, lower back, upper abdomen, lower abdomen, upper arms, and thighs) for terminal hair growth with a scale of 0–4 at each site, and a score of 8 or higher indicated hirsutism. To ensure diagnostic validity, we limited the participants to those with a diagnosis confirmed by specialists and at least two visits to our clinic. Patient demographics and clinical characteristics were compared among the FPHL subtypes, and multivariable analysis was performed to identify the factors associated with each FPHL pattern.
Statistical Analysis
Statistical analyses were performed using SPSS Statistics software (version 18.0; SPSS Inc., Chicago, IL, USA). The sample size was calculated based on data from a previous study on the prevalence of FPHL.20 At least 168 participants were required to detect a statistical power of 95% and a two-sided significance level of 5%. Categorical variables were expressed as proportions, and continuous variables were reported as mean ± standard deviation (SD) or median (interquartile range, IQR). Differences between FPHL among subtypes were determined using chi-square test with Yate’s correction, Kruskal–Wallis test, or analysis of variance (ANOVA), as appropriate.
Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated to estimate risks and describe associations. Univariate analysis was performed to estimate the associations between the variables of interest and FPHL subtypes by comparing demographics, clinical characteristics, and comorbidities. Multinomial logistic regression adjusted for variables with P-value ≤ 0.1 in univariate analysis and relevant potential confounding factors was performed to evaluate relationships between variables and each FPHL subtype. Two-sided P-values < 0.05 were considered statistically significant and analyzed without proper adjustment for multiple comparisons.
Results
Demographics and Clinical Characteristics
A total of 519 patients with FPHL were identified from our database. The most prevalent FPHL subtype was the Ludwig pattern, which was observed in 265 patients (51.1%), followed by the Olsen (n = 171, 32.9%) and Hamilton-Norwood (n = 83, 16%) patterns. The mean age at disease onset was 45.2 ± 14.3, 43.8 ± 12.9, and 41.5 ± 13.1 years for Ludwig, Olsen, and Hamilton-Norwood subtypes, respectively, with a significantly lower age observed in the Hamilton-Norwood group (P = 0.03). When stratifying the age at onset into early (<40) and late (≥40) onset groups, the Hamilton-Norwood subtype continued to have the highest prevalence in the early onset group (61.4%, P = 0.005). Patients with the Ludwig pattern showed the longest median disease duration (7 [1–10] years) and the highest proportion of grade III severity (25.3%) compared with the others; however, no statistically significant differences were detected among the patterns. Significant differences were observed in menstrual regulation among the three groups (P = 0.036), with irregularity in 22.9% of Hamilton-Norwood subjects, 13.5% of Olsen subjects, and 11.7% of Ludwig subjects.
A total of 387 (74.5%) patients reported a positive family history of AGA, with no statistically significant differences among the subtypes. The Ludwig and Olsen groups had higher proportions of maternal AGA than paternal AGA history, described by 28.7% and 28.6% of maternal AGA and 25.3% and 22.8% of paternal AGA in the Ludwig and Olsen groups, respectively. In contrast, the Hamilton-Norwood group showed a higher prevalence of a paternal AGA background, with 31.3% reporting paternal AGA and 24.1% reporting maternal AGA, respectively. Other characteristics, including infertility, menopause, alcohol consumption, and smoking, were not significantly different among the three groups. Table 1 presents the demographic and clinical characteristics of each FPHL subtype.
 |
Table 1 Comparison of Demographics and Clinical Characteristics Among Subtypes of Female Pattern Hair Loss |
Comorbidities Among Subtypes of FPHL
A statistically significant difference was observed in the BMI among the three patterns (P = 0.039). Overweight (BMI ≥ 25 kg/m2) was predominant in the Olsen (n = 68, 39.8%) and Ludwig (n = 100, 37.8%) patterns, whereas the Hamilton-Norwood subtype showed a lower proportion with only 20 participants (24.1%). Hypertension and type 2 DM showed similar trends to overweight, with 19 (11.1%), 20 (7.5%), and 3 (3.6%) cases of hypertension in the Olsen, Ludwig, and Hamilton-Norwood groups, respectively, and 20 (11.7%), 28 (10.6%), and 2 (2.4%) patients with type 2 DM in those same groups respectively. However, only type 2 DM showed a statistically significant difference among the categories (P = 0.047).
Being the most prevalent, 15 patients (18.1%) in the Hamilton-Norwood group had PCOS with a significantly higher proportion compared to the others (P = 0.02), as only 9.4% (n = 25) and 7.0% (n = 12) of patients with Ludwig and Olsen patterns, respectively, had PCOS. Seborrhea was more frequent in the Hamilton-Norwood pattern (30.1%) than in the Ludwig (19.6%) and Olsen (16.9%) patterns (P = 0.045). Acne was found in 36.1%, 25.3%, and 23.9% of Hamilton-Norwood, Ludwig, and Olsen patients, respectively. Hirsutism was reported in 14.5%, 7.6%, and 6.8% of patients according to the Hamilton-Norwood, Olsen, and Ludwig subtypes, respectively. Table 2 summarizes the comorbidities associated with each FPHL subtype.
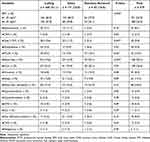 |
Table 2 Comparison of Comorbidities Among Subtypes of Female Pattern Hair Loss |
Factors Associated with Each FPHL Subtype
Multinomial logistic regression analyses were performed to study the associations between FPHL subtypes associated with the variables examined, as well as to calculate the odds of pairwise comparisons between each FPHL subgroup. The multivariable model implemented adjustments for potential confounders, including variables that met the criteria in the univariate analysis (P ≤ 0.1) and disease severity according to a previous study.18 In line with the previous results, Hamilton-Norwood subtype demonstrated significantly earlier age of disease onset compared to Ludwig and Olsen, with ORs of 2.14 (95% CI = 1.39–4.22, P = 0.02) and 1.89 (95% CI = 1.03–3.92, P = 0.04), respectively. In addition, the Hamilton-Norwood pattern was also reported to have significantly lower odds in type 2 DM compared to Ludwig (OR = 0.51, 95% CI = 0.03–0.82, P = 0.02), and Olsen (OR = 0.68, 95% CI = 0.04–0.79, P = 0.03). In contrast, this subtype revealed higher odds of PCOS, with ORs of 2.02 (95% CI = 1.55–4.84, P = 0.03) compared to Ludwig and 2.24 (95% CI = 1.89–5.31, P = 0.01) compared to Olsen (Table 3).
 |
Table 3 Multinomial Logistic Regression Analysis for Demographics, Clinical Characteristics, and Associated Comorbidities of Each Subtype of Female Pattern Hair Loss |
Discussion
Previous studies have reported the demographics, clinical characteristics, and increased risk of several comorbidities in patients with FPHL. However, limited information exists regarding the differences among FPHL subtypes. Our study which included a relatively large number of subjects demonstrated that the Ludwig subtype was the most prevalent FPHL pattern among Thai patients. Additionally, the Hamilton-Norwood subtype showed significantly higher proportions of early disease onset, menstrual irregularity, seborrhea, and PCOS but lower proportions of overweight and type 2 DM. Multivariable analysis revealed that the Hamilton-Norwood pattern was an indicator of early disease onset and PCOS, while the Ludwig and Olsen subtypes were more likely to develop type 2 DM.
The prevalence of each clinical subtype of FPHL reported in the literature has shown inconsistencies. The Ludwig pattern has been identified as the most common subtype by Blumeyer et al and Özkoca et al,18,21 whereas Olsen found the Olsen pattern to be the most frequent subtype.1 Conversely, most previously published articles have indicated the Hamilton-Norwood pattern as the least common subtype,21–24 except for Özkoca et al, which reported it as the second most common.18 In line with most prior studies, our findings demonstrated the Ludwig pattern as the most prevalent (51.4%) and Hamilton-Norwood as the least common subtype (16%). The conflicting findings regarding the frequencies of FPHL subtypes could be explained by racial and methodological differences among the conducted studies.
The age at FPHL onset may play a significant role in clinical manifestations and associated comorbidities; however, this factor has not been fully elucidated. Our study revealed that participants with the Hamilton-Norwood pattern experienced an earlier disease onset and had approximately a 2-fold higher odds of having early onset FPHL (age < 40 years). This finding is in accordance with the study by Su et al, who also reported that the Hamilton-Norwood subtype had the youngest age at onset.25 Notably, our study demonstrated that the Hamilton-Norwood group had significantly higher frequencies of menstrual irregularity and seborrhea, which are symptoms associated with hyperandrogenism. Furthermore, this group exhibited an association with PCOS, a relatively hyperandrogenic condition that primarily develops in the 30s. Therefore, these findings suggest a potential relationship among the Hamilton-Norwood subtype, early onset FPHL, and hyperandrogenism.
FPHL is known to be a progressive disorder, with disease duration correlating positively with hair loss severity.26 Consistent with our findings, although statistically insignificant, the Ludwig pattern exhibited the longer duration and highest proportion of grade III severity, while the Hamilton-Norwood subtype had the shortest duration and lowest severity. The age at FPHL onset may have contributed to this correlation, as the Ludwig subtype had the highest age at onset, whereas the Hamilton-Norwood subtype had the lowest. Özkoca et al reported a similar relationship specifically in the Olsen subtype, suggesting variations in different disease progression rates among FPHL subtypes.18 Currently, information regarding the progression characteristics of each FPHL subtype remains limited in the literature, warranting further studies to elucidate these aspects.
Our study reported a family history of AGA or FPHL in 74.5% of the participants, which was not significantly different among the FPHL subtypes, indicating that the genetics do not show much overlap between the two hair loss phenotypes. These results were compatible with those of a previous study that demonstrated 81.7% of patients with a family history of AGA independent of clinical subtypes.18 Prior studies of FPHL from India and Korea demonstrated lower proportions of 46% and 45.2%, respectively.19,20 High frequency of a family history of AGA could indicate the role of genetics in the pathogenesis of FPHL; however, the mode of inheritance is yet to be well elucidated. Males with AGA demonstrated a higher prevalence of paternal rather than maternal family history.27,28 In contrast, FPHL was linked to maternal inheritance, similar to our study.26,28 Specifically, our study reported that the Hamilton-Norwood subtype was more likely to have paternal inheritance, suggesting the influence of paternally inherited genes.
Androgens play an important role in the pathogenesis of male AGA; however, this relationship remains inconclusive in FPHL because emerging evidence suggests that the majority of patients with FPHL present with normoandrogenia and poor response to anti-androgen therapy.24,29,30 Previous studies have reported a high prevalence of FPHL-associated hyperandrogenism in the Ludwig or Olsen subtypes.31,32 In contrast, our study revealed that the Hamilton-Norwood subtype had higher frequencies of hyperandrogenic-related presentations, including menstrual irregularity, infertility, seborrhea, acne, hirsutism, and PCOS. This disagreement could be attributed to the multifactorial etiology of androgen-related conditions and ethnic variations among the study populations. In addition, our findings may reveal the link between the Hamilton-Norwood subtype and hyperandrogenism. We observed a high prevalence of hyperandrogenic-related manifestations in the Hamilton-Norwood subtype, particularly in patients who experienced early onset of the disease, a relatively lower androgen-to-estrogen ratio period compared to older patients.33,34 Notably, the menopausal status and presence of hyperandrogenism were comparable across all subtypes, and the occurrence of androgen excess in postmenopausal women with FPHL is rarely reported.35 We hypothesize that androgens may play a role in FPHL pathogenesis by specifically affecting androgen-prone hair follicles that distribute in Hamilton-Norwood pattern on scalp of genetically predisposed females.
Women with PCOS were found to have a higher incidence of hyperandrogenism and FPHL.36,37 Prevalence of FPHL in patients with PCOS is up to 30% without any age preferences.36 A study by Tandon et al reported no differences in the prevalence of PCOS among FPHL subtypes;19 however, our study yielded contrasting results; indicating that individuals with Hamilton-Norwood subtype were at increased risk of PCOS. This discordance can be likely be attributed to the small sample size of the study by Tandon et al.19 Given the high prevalence of PCOS in women with FPHL and the increased likelihood of developing various comorbidities such as type 2 DM, hypertension, and endometrial cancer in patients with PCOS, individuals with FPHL, especially those with the Hamilton-Norwood pattern, should be screened for PCOS.
The presence of FPHL comorbidities is well documented in the literature. Yi et al identified components of metabolic syndrome, including increased waist circumference, type 2 DM, and hypertension, as main coexisting conditions of FPHL.14 These findings were also observed in the patients with FPHL included in our study; BMI ≥ 25 kg/m2 (overweight), type 2 DM, and hypertension were significantly more frequent in Ludwig and Olsen subtypes compared to Hamilton-Norwood subtype. The advanced age commonly seen in the Ludwig and Olsen subtypes could explain these results because advanced age is a known risk factor for overweight, type 2 DM, and hypertension. After adjusting for confounding factors, our analysis revealed that the Ludwig and Olsen subtypes were associated with only type 2 DM compared to the Hamilton-Norwood pattern, consistent with previous studies by Matilainen et al and Özkoca et al, respectively.18,38 The analysis also revealed no significant association between overweight and different FPHL subtypes, in agreement with the study by Tandon et al.19 Moreover, Özkoca et al revealed a high proportion of hypertension in the Ludwig subtype.18 Although hypertension was prevalent in the Olsen pattern in our cohort, our multivariable analysis failed to demonstrate a relationship between hypertension and any FPHL subtypes.
The strength of our study was its relatively large sample size. Nevertheless, it had some limitations. First, some data were unavailable due to the retrospective design of the study. Second, different follow-up durations among the FPHL participants may have introduced detection bias, potentially leading to an underestimation of variable prevalence. Third, laboratory investigations for hormonal profiles were not performed in all participants. Fourth, the results refer specifically to differences among women with different FPHL subtypes due to no comparative non-hair loss control group. Finally, the study was conducted at a single tertiary referral center in a homogeneous population, which may limit the generalizability of the findings. Future prospective, multicenter, longitudinal studies in a larger number of subjects with complete hormonal investigations are recommended to confirm our findings and better identify the associations among FPHL subtypes, clinical characteristics, and comorbidities.
Conclusion
Our study compared the prevalence, clinical characteristics, and associated comorbidities of each FPHL subtype in Thai patients. The Ludwig subtype was most prevalent in our cohort. After adjusting for confounding factors, the Hamilton-Norwood subtype was more likely to present with early disease onset and PCOS. In contrast, patients with the Ludwig and Olsen subtypes showed an increased risk for type 2 DM. Although the retrospective design may limit our study quality, physicians should carefully review the medical history, conduct thorough physical examinations, and consider appropriate investigations for comorbidities in patients with FPHL, particularly in those with specific subtypes.
Abbreviations
AGA, Androgenetic alopecia; ANOVA, Analysis of variance; BMI, Body Mass Index; CI, Confidence interval; DM, Diabetes mellitus; FPHL, Female pattern hair loss; IQR, Interquartile range; OR, Odds ratio; PCOS, Polycystic ovary syndrome; SD, Standard deviation.
Data Sharing Statement
The data sets used to support the findings of this study are available from the corresponding author upon request.
Ethics Approval and Consent to Participate
This retrospective study was conducted in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the Mahidol University Institutional Review Board for Ethics in Human Research (MURA2022/778). Concerning the included participants, the requirement for informed consent was waived, and the data were anonymized before analysis.
Disclosure
The authors declare that this manuscript was prepared in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Olsen EA. Female pattern hair loss. J Am Acad Dermatol. 2001;45(3 Suppl):S70–80. doi:10.1067/mjd.2001.117426
2. Gan DC, Sinclair RD. Prevalence of male and female pattern hair loss in Maryborough. J Investig Dermatol Symp Proc. 2005;10(3):184–189. doi:10.1111/j.1087-0024.2005.10102.x
3. Leerunyakul K, Suchonwanit P. Evaluation of hair density and hair diameter in the adult Thai population using quantitative trichoscopic analysis. Biomed Res Int. 2020;2020:2476890. doi:10.1155/2020/2476890
4. Rojhirunsakool S, Suchonwanit P. Parietal scalp is another affected area in female pattern hair loss: an analysis of hair density and hair diameter. Clin Cosmet Investig Dermatol. 2018;11:7–12. doi:10.2147/ccid.S153768
5. Natpracha W, Sukanjanapong S, Chanprapaph K, Suchonwanit P. Characterization and classification of different female hairline patterns in the Thai population. J Cosmet Dermatol. 2021;20(3):890–896. doi:10.1111/jocd.13642
6. Iamsumang W, Leerunyakul K, Suchonwanit P. Finasteride and its potential for the treatment of female pattern hair loss: evidence to date. Drug Des Devel Ther. 2020;14:951–959. doi:10.2147/dddt.S240615
7. Khunkhet S, Chanprapaph K, Rutnin S, Suchonwanit P. Histopathological evidence of occipital involvement in male androgenetic alopecia. Front Med. 2021;8:790597. doi:10.3389/fmed.2021.790597
8. Suchonwanit P, Iamsumang W, Rojhirunsakool S. Efficacy of Topical Combination of 0.25% Finasteride and 3% Minoxidil Versus 3% Minoxidil Solution in Female Pattern Hair Loss: a Randomized, Double-Blind, Controlled Study. Am J Clin Dermatol. 2019;20(1):147–153. doi:10.1007/s40257-018-0387-0
9. Suchonwanit P, Iamsumang W, Leerunyakul K. Topical finasteride for the treatment of male androgenetic alopecia and female pattern hair loss: a review of the current literature. J Dermatolog Treat. 2022;33(2):643–648. doi:10.1080/09546634.2020.1782324
10. Chanprapaph K, Sutharaphan T, Suchonwanit P. Scalp biophysical characteristics in males with androgenetic alopecia: a comparative study with healthy controls. Clin Interv Aging. 2021;16:781–787. doi:10.2147/cia.S310178
11. Suchonwanit P, Triyangkulsri K, Ploydaeng M, Leerunyakul K. Assessing biophysical and physiological profiles of scalp seborrheic dermatitis in the Thai population. Biomed Res Int. 2019;2019:5128376. doi:10.1155/2019/5128376
12. Vañó-Galván S, Saceda-Corralo D, Blume-Peytavi U, et al. Frequency of the types of alopecia at twenty-two specialist hair clinics: a multicenter study. Skin Appendage Disorders. 2019;5(5):309–315. doi:10.1159/000496708
13. Arias-Santiago S, Gutiérrez-Salmerón MT, Castellote-Caballero L, Buendía-Eisman A, Naranjo-Sintes R. Androgenetic alopecia and cardiovascular risk factors in men and women: a comparative study. J Am Acad Dermatol. 2010;63(3):420–429. doi:10.1016/j.jaad.2009.10.018
14. Yi SM, Son SW, Lee KG, et al. Gender-specific association of androgenetic alopecia with metabolic syndrome in a middle-aged Korean population. Br J Dermatol. 2012;167(2):306–313. doi:10.1111/j.1365-2133.2012.10978.x
15. Liamsombut S, Pomsoong C, Kositkuljorn C, Leerunyakul K, Tantrakul V, Suchonwanit P. Sleep quality in men with androgenetic alopecia. Sleep Breath. 2023;27(1):371–378. doi:10.1007/s11325-022-02618-x
16. Suchonwanit P, Kositkuljorn C, Mahasaksiri T, Leerunyakul K. A comparison of the efficacy and tolerability of three corticosteroid treatment regimens in patients with alopecia areata. J Dermatolog Treat. 2022;33(2):756–761. doi:10.1080/09546634.2020.1773384
17. Suchonwanit P, McMichael AJ. Alopecia in Association with Malignancy: a Review. Am J Clin Dermatol. 2018;19(6):853–865. doi:10.1007/s40257-018-0378-1
18. Özkoca D, Aşkın Ö, Engin B. The comparison of demographics and comorbidities of female pattern hair loss according to the clinical subtype and stage. J Am Acad Dermatol. 2022;87(4):779–783. doi:10.1016/j.jaad.2021.11.027
19. Tandon S, Arora P, Gautam RK, Bhardwaj M, Garga U, Sharma N. Correlation between Clinical Features, Biochemical Parameters, and Histopathological Findings in Women with Patterned Baldness: a Study from North India. J Cutan Aesthet Surg. 2019;12(1):42–48. doi:10.4103/jcas.Jcas_30_18
20. Paik JH, Yoon JB, Sim WY, Kim BS, Kim NI. The prevalence and types of androgenetic alopecia in Korean men and women. Br J Dermatol. 2001;145(1):95–99. doi:10.1046/j.1365-2133.2001.04289.x
21. Blumeyer A, Tosti A, Messenger A, et al. Evidence-based (S3) guideline for the treatment of androgenetic alopecia in women and in men. J Dtsch Dermatol Ges. 2011;9(6):S1–57. doi:10.1111/j.1610-0379.2011.07802.x
22. Norwood OT. Male pattern baldness: classification and incidence. South Med J. 1975;68(11):1359–1365. doi:10.1097/00007611-197511000-00009
23. Hamilton JB. Patterned loss of hair in man; types and incidence. Ann N Y Acad Sci. 1951;53(3):708–728. doi:10.1111/j.1749-6632.1951.tb31971.x
24. Ramos PM, Miot HA. Female Pattern Hair Loss: a clinical and pathophysiological review. An Bras Dermatol. 2015;90(4):529–543. doi:10.1590/abd1806-4841.20153370
25. Su LH, Chen LS, Chen HH. Factors associated with female pattern hair loss and its prevalence in Taiwanese women: a community-based survey. J Am Acad Dermatol. 2013;69(2):e69–77. doi:10.1016/j.jaad.2012.09.046
26. Salman KE, Altunay IK, Kucukunal NA, Cerman AA. Frequency, severity and related factors of androgenetic alopecia in dermatology outpatient clinic: hospital-based cross-sectional study in Turkey. An Bras Dermatol. 2017;92(1):35–40. doi:10.1590/abd1806-4841.20175241
27. Khumalo NP, Jessop S, Gumedze F, Ehrlich R. Hairdressing and the prevalence of scalp disease in African adults. Br J Dermatol. 2007;157(5):981–988. doi:10.1111/j.1365-2133.2007.08146.x
28. Lee WS, Lee HJ. Characteristics of androgenetic alopecia in asian. Ann Dermatol. 2012;24(3):243–252. doi:10.5021/ad.2012.24.3.243
29. Herskovitz I, Tosti A. Female pattern hair loss. Int J Endocrinol Metab. 2013;11(4):e9860. doi:10.5812/ijem.9860
30. Redler S, Messenger AG, Betz RC. Genetics and other factors in the aetiology of female pattern hair loss. Exp Dermatol. 2017;26(6):510–517. doi:10.1111/exd.13373
31. Starace M, Orlando G, Alessandrini A, Piraccini BM. Female Androgenetic Alopecia: an Update on Diagnosis and Management. Am J Clin Dermatol. 2020;21(1):69–84. doi:10.1007/s40257-019-00479-x
32. Rossi A, D’Arino A, Pigliacelli F, et al. The diagnosis of androgenetic alopecia in children: considerations of pathophysiological plausibility. Australas J Dermatol. 2019;60(4):e279–e283. doi:10.1111/ajd.13079
33. Leerunyakul K, Suchonwanit P. Asian Hair: a Review of Structures, Properties, and Distinctive Disorders. Clin Cosmet Investig Dermatol. 2020;13:309–318. doi:10.2147/ccid.S247390
34. Randolph JF, Zheng H, Sowers MR, et al. Change in follicle-stimulating hormone and estradiol across the menopausal transition: effect of age at the final menstrual period. J Clin Endocrinol Metab. 2011;96(3):746–754. doi:10.1210/jc.2010-1746
35. Carmina E, Azziz R, Bergfeld W, et al. Female Pattern Hair Loss and Androgen Excess: a Report From the Multidisciplinary Androgen Excess and PCOS Committee. J Clin Endocrinol Metab. 2019;104(7):2875–2891. doi:10.1210/jc.2018-02548
36. Feng JG, Guo Y, Ma LA, Xing J, Sun RF, Zhu W. Prevalence of dermatologic manifestations and metabolic biomarkers in women with polycystic ovary syndrome in north China. J Cosmet Dermatol. 2018;17(3):511–517. doi:10.1111/jocd.12387
37. Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25. doi:10.1016/j.fertnstert.2003.10.004
38. Matilainen V, Laakso M, Hirsso P, Koskela P, Rajala U, Keinänen-Kiukaanniemi S. Hair loss, insulin resistance, and heredity in middle-aged women. A population-based study. J Cardiovasc Risk. 2003;10(3):227–231. doi:10.1097/01.hjr.0000070200.72977.c6
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

