Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 9
Diarrheal status and associated factors in under five years old children in relation to implemented and unimplemented community-led total sanitation and hygiene in Yaya Gulele in 2017
Authors Degebasa MZ , Weldemichael DZ, Marama MT
Received 8 December 2017
Accepted for publication 17 April 2018
Published 17 October 2018 Volume 2018:9 Pages 109—121
DOI https://doi.org/10.2147/PHMT.S159366
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Professor Roosy Aulakh
Mamo Z Degebasa,1 Dawit Zenebe Weldemichael,2 Mokonnon T Marama3
1Department of Maternal and Child Health, Yaya Gulele Woreda, Fitan, Ethiopia; 2Department of Epidemiology, College of Health Sciences, Mekelle University, Mekelle, Ethiopia; 3Department of Midwifery, College of Health Sciences and Medicine, Wolaita Sodo University, Wolaita Sodo, Ethiopia
Purpose: The aim of this study was to assess the diarrheal status and associated factors of under five-years old children among implemented and unimplemented community-led total sanitation and hygiene (CLTSH) in Yaya Gulele district, Ethiopia, in 2017.
Methods: Community-based comparative cross-sectional study involving 380 households from each implemented and unimplemented CLTSH area was conducted from December 1 to June 30, 2017. Pretested structured questionnaire and a complete observational checklist were used to collect data. Qualitative data were collected via focused group discussions and analyzed manually. Data were checked and entered to Epi-info 3.5.4 and analyzed by SPSS version 20. Bivariate and multivariable logistic regression analyses were computed
Results: In this study, 88% implemented and 66% unimplemented CLTSH had latrine. Of households owning latrine, 85% in implemented and 75% in unimplemented CLTSH utilize latrine properly. In the study area, 12% in implemented and 34% in unimplemented CLTSH area practice open defecation. Two weeks period diarrhea prevalence was 13.4% (95% CI: 10.2–17.3%) in implemented CLTSH and 36.3% (95% CI: 31.7–41.6%) in unimplemented CLTSH. Having two or more children under five years old (adjusted odds ratio [AOR] = 2.33; 95% CI: 1.09–4.96), lack of clean water storage (AOR = 2.36; 95% CI: 1.16–4.80), negative attitude of mothers/caregivers toward diarrhea (AOR = 2.07; 95% CI: 1.06–4.04), presence of feces in the compound (AOR = 1.88; 95% CI: 1.10-3.22), and lack of hand washing facility in the compound (AOR = 2.64; 95% CI: 1.47–4.74) were associated factors of the outcome.
Conclusion: Implementation of CLTSH is the applicable tool to reduce diarrhea prevalence. Having two or more children under five years old, unclean water storage, negative attitude of mothers toward diarrhea, existence of feces in the compound, and lack of hand washing facility in the compound were associated factors to the diarrheal status of children under five years old. Health workers and local authorities inspire the community to clean water-storage facilities and the environment, to change mothers’ behavior toward diarrhea, as well as construct hand washing facility in the compound.
Keywords: CLTSH, diarrhea, under-five children, Yaya Gulele district
Introduction
The World Health Organization (WHO) defines diarrhea as the passage of three or more loose or watery stools within a day or unusual frequency of diarrhea episodes.1–3 Globally, about 1.7 billion cases of diarrheal disease occur annually. It is the second leading cause of death in children under five years old worldwide, mainly in developing countries. Eighteen percent of all the deaths of children under five years old is a result of diarrheal diseases. Of all the child deaths from diarrhea, 78% occur in the African and Southeast Asian regions. In Africa, diarrhea accounts for about four billion cases annually due to poor sanitation.4–7
Poor sanitation and unsafe drinking water have a grim impact on child mortality in particular and public health in general, which is associated with adverse nutritional outcomes, diarrhea, and tropical enteropathy.8,9
Inadequate and unsafe water, lack of sanitation, and poor hygiene practices is a complex issue for different diseases and accountable for the occurrence of 90% of diarrheal diseases. Approximately 1.5 to 2.2 million people die each year from diarrhea and related diseases due to poor sanitation. Open defecation (OD), lack of access to safe disposal of human excreta, lack of awareness of hygienic practices, and using contaminated water were strongly linked with these deaths.6,7,10–12
Since adoption of the Millennium Development Goals, access to improved sanitation has increased around the globe. Despite significant investments made during recent decades by governments, nongovernment organizations, bilateral and multilateral agencies to reduce diarrhea and sanitation problems, diarrhea remains a problem. Approximately 37% of the world’s population lacks approved sanitation. Eleven percent of the global population is not drinking safe water and 319 million of these people live in sub-Saharan Africa.6,13–15
Diarrhea is a preventable and treatable feco–oral disease and one of the prevention strategies is community-led total sanitation and hygiene (CLTSH). CLTSH is an important innovative approach to change collective behavior of the community. It is used to change the communities’ collective behavior to utilize emotions, participatory approaches, and visual tools based on the principle of triggering to enable communities to analyze their sanitation situations. In the year 2000, CLTSH was initiated in Bangladesh, and has since been implemented in 50 countries with at least 15 integrating the CLTSH into their national policy, including Ethiopia.3,10,13,16–18
In African countries, including Ethiopia, each child on average suffers from five episodes of diarrhea per year. The ranges of two weeks diarrhea prevalence from 10% to 40% in different parts of Ethiopia are the result of poor water, sanitation, and hygiene.12,20–22
The Ethiopian Ministry of Health has been struggling to control the morbidity and mortality of children due to poor sanitation, inadequate safe water, and poor hygiene practices by formulating and implementing different policies and strategies. In 2002/03, health service extension package strategies and, in 2006, CLTSH approach was adopted and linked to the national policy. Despite these continuous efforts, 50,000 to 112,000 children under five years of age perish annually due to diarrheal diseases related to poor environmental sanitation and hygiene practices.13,23,24
In study area, despite 50% of total kebeles implementing CLTSH and 90% rotavirus and measles vaccination achieved, diarrheal disease is the second among the top five causes of morbidity with 36.7% incidence (eHMIS annual report of Yaya Gulele district; unpublished data; 2016). Therefore, this study aimed to assess diarrheal status and associated factors among children under five years old in implemented and unimplemented CLTSH in Yaya Gulele district.
Methods
The study was conducted in Yaya Gulele “District” (district or the third-level administrative divisions of Ethiopia) which is purposely selected. Yaya Gulele is 114 kilometers away from Addis Ababa (capital city of the country) to the North direction. The district is found at geographical coordinates of 9°30′N latitude and 38°40′E longitude. This district has 16 rural and one urban kebeles (the smallest administration in Ethiopia) with four health centers and 16 health posts.25
The total estimated population of the district is 71,682 of whom 36,703 (51.2%) are males, based on 2014–2017 population projection of Ethiopia.26 Among the total population, 2,308 (3.22%) and 11,777 (16.43%) were under one and under five years old, respectively. The community has homogenous culture. The Yaya Gulele Woreda Report indicated that, latrine coverage was 89%, latrine utilization was 82%, and safe water coverage was 72% (eHMIS annual report of Yaya Gulele district; unpublished data; 2016).
Study design and period
Community-based comparative cross-sectional study design was triangulated with qualitative method of focus group discussions (FGD). The study was conducted from December 1 to June 30, 2017.
Study population
All households of Yaya Gulele district that had at least one child under five years old child who has resided there for more than 6 months composed the study population. The mothers/caregivers of the under-five years old child were the respondents in the households. However, mothers or caregivers who are mentally ill, seriously ill, had hearing and speaking problem were excluded from the study.
Sample size determination
The sample size was determined by using two-population proportion formula based on the assumptions: Significance level of 95% (α = 0.05), 11.1% and 21.6% the proportion of diarrhea in implemented and unimplemented CLTSH, respectively.27 Power of the study was 80% (β = 0. 2), 1:1 ratio and two-design effect and 10% of none response rate was considered. The computation resulted in 380 households recruited from each implemented and unimplemented CLTSH in this study.
Sampling techniques
Multistage sampling method was used to select study participants. The district was divided into implemented and unimplemented CLTSH kebeles. Four kebeles were selected from the total kebeles of implemented CLTSH and unimplemented CLTSH by a simple random sampling technique using lottery method as a primary sampling unit. Afterwards, sampling frame of the households who have at least one child under five years old was obtained from the monthly updated family folders in the health posts of respective kebeles. Finally, a total of 760 samples (380 households from implemented CLTSH and 380 households from unimplemented CLTSH) were allocated to all randomly selected kebeles proportionally based on population size (number of households who have at least one child under five years old) in the kebeles. Systematic sampling method was used to select study participants from each selected kebele as a secondary sampling unit. The total number of households (households with at least one child under five years old) in each kebele was divided by the allocated sample size to get sampling interval. The first participant picked by lottery method and the next was drawn (with the fifth interval in implemented CLTSH and eighth interval in unimplemented CLTSH) walking in the direction of the spinned sharp pen. One-time additional attempt was made to interview the participants who were not present during data collection. Schematic presentation of multistage sampling frame.
Data collection tools and techniques
Data were collected through face-to-face interview with the use of pretested interviewer-administered structured questionnaire and observational checklist. Variables included socio-demographic, environmental, behavioral factors, knowledge of mothers/caregivers toward diarrhea, and attitude of mothers/caregivers toward diarrhea and childhood diarrhea were incorporated into the questionnaires. Observational checklist was used to observe water container storage, availability and utilization of the latrine, sanitation of the compound, and absence or presence of hand washing facility. The questionnaire was adopted from WHO core questions for water and sanitation and by reviewing other materials related to the topic.7,16,28
Furthermore, four sessions of FGD (two from each implemented and unimplemented CLTSH area) were carried out to supplement the quantitative findings. There were eight participants involved in each FGD. Mothers/caregivers who had children under five years old and who did not take part in the questionnaire survey were the participants in this FGD. Purposive sampling technique was used to select the participants by considering age and residence (implemented CLTSH and unimplemented CLTSH) of the participants. The mothers/caregivers of the age group 25–35 years were selected, because they are considered to have some prior experiences of taking care of their children and could actively participate in the discussions to reveal additional interactions and insights. A semi-structured topic guide to understand the phenomena of mothers’ knowledge on the causes and prevention of diarrhea, the importance of having hand washing facility, and perception of hand washing to prevent diarrhea was used. These FGD were carried out by experts of the health office. Audio records via mobile and note taking were done throughout the process. Expert of maternal and child health department acted as moderator. The sessions were arranged based on the participants’ convenient time and place. Ten trained diploma nurses and two BSc Environmental Health professionals were employed for data collection and supervision, respectively.
Childhood diarrhea prevalence was measured using the WHO-recommended definition, namely if a child had three or more loose stools or watery diarrhea in 24 hours during the two weeks preceding the survey as reported by mothers/caregivers.29
Knowledge of the respondents toward diarrhea was measured via computed mean score. Each correct response scored as one whereas other responses such as “incorrect” or “don’t know” scored as zero.30 There were 22 variables in the knowledge section of the questionnaire. Using the mean score,7 respondents who scored below the mean were said to have poor knowledge and respondents who scored above the mean were considered as having good knowledge. Importance of hand washing has seven items. It was dichotomized into “know” was assigned if the respondents scored above the mean and not know when the respondents scored below the mean.7,31 Attitude of the mothers/caregivers toward diarrhea was measured by 10 questions. The questions were dichotomized to positive (strongly agree and agree) and negative (strongly disagree and disagree). Accordingly, respondents who scored above the mean were considered as positive and respondents who scored below the mean were considered to have a negative attitude toward diarrhea.32
Data quality assurance
Two days training was given to data collectors and supervisors on how to collect data from study participants and other technical procedures. To check the reliability of the tool, estimate time for this interview, and ensure understandability, the question was pretested on 5% (40) of the population who were not included in the study. Based on the findings of pretest, the necessary correction was made on the clarity of language, sequence of words and questions. The collected data were checked for completeness and consistency daily by supervisors and principal investigator before transferring into computer software. The questionnaire was originally written in English and then translated to “Afan Oromo” and back to English for consistency. Incomplete questionnaires were referred back for completion.
Data management and analysis
Data collected, were entered and cleaned using Epi Info version 3.5.4 and exported to Statistical Package for Social Sciences (SPSS) version 20 for data analysis. Continuous variables were coded, and some coded variables were recoded. Frequencies for all variables were counted and cross-tabulated using percentages. Bivariate logistic regression analyses were done for the explanatory variables with the dependent variable to select contender variables for multiple logistic regression models. Primarily variables that have p-value <0.2 in bivariate analysis were used to build the logistic model in order to identify predisposing factors that were linked with diarrhea. Multivariable analysis was done to find out whether the significant factors identified in bivariate analysis remain independently associated with the outcome variable.
Model fitness was checked via Hosmer–Lemeshow goodness of fit test when the p-value > 0.05 model is fit. Multicollinearity between independent variables was checked via calculation of variance inflation factor. The results were presented in the form of tables, figures, and summary statistics. Adjusted odds ratio (AOR) with its 95% confidence interval (CI) was used to report statistical significance at p-value < 0.05. Collected qualitative data were transcribed, coded, recoded, themes developed, and analyzed manually to augment quantitative findings.
Ethical consideration
Ethical approval was obtained from the ethical review board of Mekelle University College of Health Sciences. Official permission letters were obtained from the Oromia Regional Health Bureau before commencement of the study. The participants were informed of the purpose of the study and privacy during the interview. Informed verbal consent was obtained from each study participant prior to interviewing. The participants’ verbal informed consent process was approved by the Mekelle University College of Health Sciences ethical review board. Participants were made aware they had full right to participate or not in the study as well as to withdraw anytime during the interview. Confidentiality was also maintained through anonymity. In addition, they were also advised to take the child to the nearest health facility to get professional support.
Results
Socio demographic characteristics
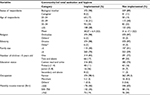
Seven hundred sixty (760) mothers/caregivers who have children under five years old were involved in this study with a 100% response rate. Among the study participants, 380 (50%) were from implemented CLTSH and the rest were from unimplemented CLTSH kebeles. The mean ages of the participants were 30.07 ± 6.4 (standard deviation [SD]) years old in implemented CLTSH and 31.6 ± 7.1 (SD) years old in unimplemented CLTSH kebeles. Orthodox Christianity was the predominant religion in both implemented (374 [98%]) and 370 (97%) in unimplemented CLTSH area (Table 1).
Childhood diarrhea prevalence
Two weeks period childhood diarrhea prevalence was 13.4% (95% CI: 10.2–17.3%) in implemented and 36.3% (95% CI: 31.7–41.6%) in unimplemented CLTSH area. The mean ages of the children with diarrhea were 29.9 ± 17.7 (SD) months in implemented and 28.8 ± 16.7 (SD) months in unimplemented CLTSH kebeles. The overall mean age of children was 29.01 ± 17.03 (SD) months (Table 2).
  | Table 2 Childhood diarrhea prevalence in implemented and not implemented community-led total sanitation and hygiene kebeles, Yaya Gulelle district, June 2017 |
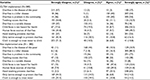
Environmental characteristics related to diarrhea
More than two-third of the participants, 333 (88%) in implemented and 280 (74%) unimplemented CLTSH area used protected water source. Two hundred eighty-nine (76%) in implemented and 247 (66%) unimplemented CLTSH kebeles got water supply by less than 30-minute walk from their home. Of the participants, 303 (91%) in implemented and 107 (43%) unimplemented CLTSH kebeles had improved pit latrine. More than half of the participants, 179 (54%) in implemented and 159 (63%) in unimplemented CLTSH kebeles had no hand-washing facility in or close to the latrine (Table 3).
  | Table 3 Environmental characteristics of community-led total sanitation and hygiene (CLTSH) implemented and CLTSH not implemented participants, Yaya Gulele district, June 2017 (N = 760) |
More than two-thirds of participants in implemented CLTSH mentioned latrine discomfort as the main reason for not having the latrine as compared to unimplemented CLTSH area, 3.1% (Figure 1). Of 760 participants, more than two-thirds of implemented CLTSH and 72% of unimplemented CLTSH described that they dispose wastes in an open pit in the compound, whereas 13.7% of implemented CLTSH and 15.3% of unimplemented CLTSH kebeles dump wastes in open field (Figure 2).
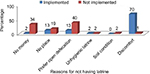  | Figure 1 Reason for not having latrine in CLTSH and not CLTSH implemented area, Yaya Gulele district, June 2017. Abbreviation: CLTSH, community-led total sanitation and hygiene. |
  | Figure 2 Place of solid waste disposal in CLTSH and not CLTSH implemented sites, Yaya Gulele district, June 2017. Abbreviation: CLTSH, community-led total sanitation and hygiene. |
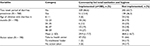
Behavioral characteristics related to diarrhea
Of the participants, 331 (87%) in implemented and 240 (63%) in unimplemented CLTSH kebeles treated their drinking water sources. Majority of participants, 377 (99%) in implemented and 320 (84%) in unimplemented CLTSH kebeles, stored their water in jerry can and practiced pouring method to draw water from the container. More than two-thirds of the participants, 283 (75%) in implemented and 282 (74%) in unimplemented CLTSH kebeles practiced incomplete hand washing at critical times. Nearly two-fifths of the participants, 146 (38%) in implemented and 161 (42%) in unimplemented CLTSH area, had poor knowledge toward diarrhea (Table 4).
Attitude of participants toward diarrhea
More than half of the participants, 205 (54%) in implemented and 291 (77%) in unimplemented CLTSH kebeles strongly agree that diarrhea is a harmful disease in the community. More than half of the participants, 201 (53%) in implemented and 248 (65%) in unimplemented CLTSH kebeles strongly agree that hand washing at the critical time can prevent diarrheal disease (Table 5). Overall, positive attitude of the respondents toward to diarrhea among implemented and unimplemented CLTSH was 48% and 22%, respectively (Table 6).
  | Table 6 Overall attitude of mothers/caregivers toward diarrhea in implemented and not implemented community-led total sanitation and hygiene (CLTSH) in Yaya Gulele district, June 2017 |
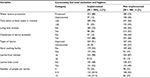
Factors associated with diarrhea among childrens under five years old
Variables in the bivariate analysis of socioeconomic status, environmental and behavioral characteristics, composition of knowledge toward diarrhea, attitude of mothers/caregivers toward diarrhea, and the importance of hand washing items that had a p-value ≤ 0.2 was further considered in the final multivariable logistic regression analysis via backward elimination methods. Variables such as having two or more children under five years old, not clean water container, and negative attitude of mothers/caregivers toward diarrhea in CLTSH as well as the presence of feces in the compound and not having hand washing facility in or adjacent to the latrine in unimplemented CLTSH were independently statistically significant in multivariable analysis.
The odds of developing diarrhea was two times higher among children whose parents had two or more children under five years old compared to the children whose parents had only one child in implemented CLTSH area (AOR = 2.33; 95% CI: 1.09–4.96). The children whose parents had no clean water storage were 2.36 times more likely to have diarrhea than those whose parents had clean water storage (AOR = 2.36; 95% CI: 1.16–4.80). The odds of children having diarrhea were two times higher among children whose mothers/caregivers had negative attitude toward diarrhea compared to children whose mothers/caregivers had positive attitude toward diarrhea in unimplemented CLTSH area (AOR = 2.07; 95% CI: 1.06–4.04).The children who lived in the compound where the feces were seen was 1.88 times more likely to have diarrhea than the children who lived where the feces was not seen in the compound (AOR = 1.88; 95% CI: 1.10–3.22). The odds of children developing diarrhea was 2.64 times higher among children whose parents didn’t have hand washing facility adjacent to the latrine as compared to those children whose parents had hand washing facility adjacent to the latrine (AOR = 2.64; 95% CI: 1.47–4.47). Overall, the likelihood of diarrhea among children under five years old was 68% less in implemented CLTSH than unimplemented CLTSH area (AOR = 0.32; 95% CI: 0.20–0.52) (Table 7).
Caregivers’ knowledge toward hand washing facility and latrine utilization
Challenges to prevent diarrhea disease
In the FGD some participants in both implemented and unimplemented CLTSH said that they faced challenges to prevent diarrheal disease. Thirty (30) years old mother who cannot read and write of FGD participant in not CLTSH implemented kebele said, “Most of the households who owned latrine have no hand washing facility adjacent to the latrine which raised raw material and water scarcity as the challenge. Households also use open field due to odor and discomfort of the latrine. The presence of bush and institutional latrine around their house is the great challenge which impairs the construction of their own latrine. Only adults go to the bush and institutional latrine to defecate, but the females and the children defecate in the garden and in the compound mostly at night time”. Also, the literate FGD participants of 28 years in implemented CLTSH support the idea that “soil condition is also one challenge to construct latrine and lead the people to defecate in the open which is the primary cause of diarrhea”.
This FGD indicates that presence of institutional latrine and bush/shrub around the house, scarcity of water for hand washing at hand washing facility, and soil condition which was a challenge to construct the latrine and led to defecating in the open field were the challenges to prevent diarrheal disease.
Knowledge and attitude of the mothers/caregivers toward diarrhea
Thirty-five (35) years old mother who cannot read and write, FGD participant in unimplemented CLTSH kebele, said, “…the health extension workers are now teaching us about the importance of hand washing facility. However, most of the households are inconvenient on the importance of hand washing facility next to the latrine and properly utilize it. Mostly they assume that if the children use the latrine they exposed to adult feces and may fall in the latrine via the hole of latrine”. Majority of FGD from implemented and unimplemented area raised the idea that “… Some households’ children defecate in open field adjacent to the house and the mothers perceive the infants and the child’s feces less dirty than adults because of less size and odorless”. Another participant of FGD in unimplemented CLTSH area also strengthens this one “…. I do not blame and influence my family to use the latrine, because of its odor and discomfort. My child developed diarrhea last week and I took to health facilities and paid forty-five birrs for this discomfort. There is a bush surrounding us. My family used that bush for defecation. Therefore, installing hand washing facility is not important because we do not use the latrine”. The result of this FGD indicates that the mothers/caregivers have a negative attitude toward the presence of a child feces in the compound no matter whether it is present or not related to diarrhea.
However, some FGD participants in both CLTSH and not CLTSH implemented kebeles explained that, “…. As we learnt from health extension workers, we are washing our hands and our children’s hand before feeding and after visit to the toilet. Since we apply education obtained from health extension workers about the importance of hand washing, our children are not suffering from diarrhea. Hence, having hand washing facility is one mechanism of diarrhea prevention”. This FGD reflects that the mothers have positive attitude toward hand washing and having hand washing facility to prevent diarrhea
An FGD participant of 30 years who cannot read and write in implemented CLTSH explained that “… When the children exposed to hot weather they may get diarrhea. For instance, since I am a farmer, I do the household responsibilities, including baking injera (local bread) in the kitchen, carrying my child on my back. Diarrhea not caused by germs. Therefore, if the child is exposed to hot weather he/she gets diarrhea”. Another 30 year old unable to read and write FGD participant in unimplemented CLTSH said “… diarrhea is caused when evil people’s eyes watch the child. When those people watch the child, they become sad and weak. Sometimes he/she suffers from headache, cries all the time, and cannot sleep. The stools are green, soft, and accompanied by vomiting. Thus, evil eyes cause under five years old childhood diarrhea”.
Discussion
Diarrheal diseases remain a major cause of morbidity and mortality in low-income countries such as Ethiopia.20 This study revealed that implementing CLTSH reduces childhood diarrheal illness. Two or more children under five years old in the family, no cleaned water container, negative attitude toward diarrhea in CLTSH, and presence of feces in the compound and lack of hand washing facility adjacent to the latrine in unimplemented CLTSH were associated factors for occurrence of diarrheal disease among children under five years old.
Results in previous literature on CLTSH in Ethiopia revealed that a substantial reduction in diarrheal incidences and nearly no acute watery diarrhea (AWD) incidences were present in the area where CLTSH was implemented.12 In this study, last two weeks period diarrhea prevalence during the study period was 13.4% (10.2–17.3%) in implemented CLTSH and 36.3% ( 31.7–41.6%) in unimplemented CLTSH area which reveals diarrhea prevalence in implemented was lower as compared to diarrhea prevalence in unimplemented CLTSH. This disparity might be due to increased latrine coverage and utilization with improved types of latrine and behavior change toward OD.
According to this study, two weeks period diarrhea prevalence in CLTSH was lower as compared to 19% in implemented CLTSH and 22.4% in unimplemented CLTSH in Jimma zone,20 32.6% in Burundi,33 22.5% in Eastern Ethiopia,34 and 27.3% in Somali Region, Jigjig district.35 This disparity might be due to study sample size, study period, coverage of latrine and utilization, access of safe water for drinking. However, the result of this study is consistent with study in implemented CLTSH in Kenya3, 12% in 2016 Ethiopian Demographic Health Survey (EDHS)22 and 15% in implemented CLTSH in Eastern Ethiopia.12 This consistence may be due to intervention of CLTSH and study period.
This study revealed that 12% in implemented CLTSH practiced OD as compared to 34% in unimplemented CLTSH area. This variation may be due to CLTSH influence to the community to analyse their local sanitation situation and its impact on their health. The results of this study revealed that 12% of households practice OD in implemented areas and 34% in unimplemented areas. However, the results are lower than those in an EDHS study done in 201622,36, which showed 37% and 38.1% were open defecate, respectively. This disparity may be due to sample size, sensitization of the community via CLTSH.
The children whose parents lived in implemented CLTSH were 68% less likely to develop diarrhea as compared to the children whose parents lived in unimplemented CLTSH area. This finding is consistent with study in Kenya.37 It is the reason why diarrhea is less likely developed in implemented CLTSH hygiene promotion and behavioral changes toward sanitation that prevent and reduce diarrhea via reduced environmental feco–oral contamination.
In this study, two or more children under five years old was statistically significant for the occurrence of diarrheal disease in implemented CLTSH and not significant in unimplemented area. As the number of children increased, the frequency of diarrhea increased significantly. This finding is supported by the studies done in Eastern, North-West, and Southern Ethiopia.23,34,38 When the number of children in the households increases, it is expected that children could be more vulnerable to contamination because the quality of care and attention from parents decreases. Furthermore, children who get diarrheal disease may easily transmit the disease to others who live in the same area. This might be due to crowding which worsens the hygiene condition and increases the chance of contact with pathogens and mothers/caregivers being incapable to care for a large number of children.
In this study, the children whose family had no clean water supply were more likely to develop diarrhea than children whose families had clean water storage in implemented CLTSH and not significant in unimplemented CLTSH area. This study is supported by a study in India19 and study in Nigeria39 which showed that transmission of diarrhea occurs easily when in-house water-storage facilities are contaminated. Despite the use of water from protected sources and water treatment practice, many people do not wash their hands before getting water from storage containers. This occurrence of diarrhea may be due to the drips of water from unwashed hand when getting water from the sources and dipping unwashed cup. During transportation water may also be contaminated in water container, which causes diarrheal disease.
Attitude of the mothers/caregivers toward diarrhea is statistically significant for developing diarrhea. Children whose mothers/caregivers had negative attitude toward diarrhea were more likely to have diarrhea than children whose mothers/caregivers’ attitude was positive. The result of FGD supports this finding. This result is consistent with a study done in Shebedino district, southern Ethiopia40 which reported that children whose mothers have misconception about diarrhea and sanitation are more affected by diarrhea. This may be due to misconception of mothers/caregivers toward diarrhea and educational background of the mothers/caregivers which causes the inability to identify factors which induce diarrhea and reduce exposure of contaminated environment.
Unavailability of hand washing facility adjacent to the latrine was positively associated with childhood diarrheal disease. In this study, children under five years old from households that had no hand-washing facilities were more likely to have diarrhea than the children from households that have hand-washing facilities adjacent to the latrine. The result of FGD support this finding, children under five years old affected by diarrhea because of water shortage and raw materials, lack of hand-washing facility adjacent to the latrine. This study is consistent with study in Jimma, Kersa district and Eastern Ethiopia,20,34 where the hand-washing facilities were not available, the person lacks the initiative to wash hands after toilet use and feeds the child with hands exposed to fecal matters which causes diarrhea. This may be due to educational background of the mothers/caregivers who have not learned the importance of hand washing after toilet use.
Presence of feces in the compound is an associated factor for diarrhea. This study showed that children who lived in the households where feces is present in the compound were more likely to have diarrhea as compared to those children who lived in households where feces was not present in the compound. The result was supported by FGD. The more the feces is in the compound, the more children suffered from diarrhea. This result is consistent with a study in Indonesia and Bangladesh,41,42 which reported that the child feces disposal events in open space adjacent to the households compound and in location designated for households waste fail the children on the risk of diarrhea which support the hypothesis that unsanitary environment leads to gastroenteritis. It seems universally true that mothers perceive that the feces of infants or children are less dirty than those of adults. It seems because of its less smell, its smaller size, and because of less likely to have food residuals43 though may possibly have a higher loading of pathogens. Unsanitary environmental conditions put children at increased risk of diarrhea including environmental enteropathy.42 Those children develop diarrhea where feces seen in open field may be due to the children either crawling or walking and putting in the mouth dirt or other contaminated objects while playing or eating.
The participants in this FGD indicated that diarrhea occurred due to exposure to weather condition and evil eyes, as well as germs not causing the diarrhea. This is supported by qualitative study in Benishangul Gumuz32 and North West Ethiopia.44 This may be due to misconception and negative attitude of the mothers/caregivers toward causes of diarrhea.
Recommendation
- Health workers and local authorities should inspire the community to change their behavior toward the construction of latrine with the full package (including hand-washing facility, soap/ash for hand-washing, functional superstructure and other components), give health education to the mothers/caregivers on the causes and prevention of diarrhea and importance of hand washing facility with cleansing agents.
- Further study with a robust research design such as cohort and randomized controlled trial, which would provide evidence of cause and effect, required to identify factors accounted for diarrhea occurrence should be conducted.
Conclusion
Generally, the overall two-week diarrhea prevalence was lower in implemented CLTSH compared to unimplemented CLTSH approach. Moreover, this study shows that having two or more children under five years old, not washing drinking water storage, negative attitude of mothers/caregivers toward diarrhea, presence of feces in the compound and lack of hand-washing facility adjacent to the latrine were the important associated factors for diarrhea occurrence. This finding indicates that despite the CLTSH approach implemented in several kebeles, the implemented kebeles did not practice OD. Thus, this result suggests that CLTSH implementation is an applicable approach on access to sanitation and to reduce diarrhea prevalence among children under five years old.
Acknowledgments
First and foremost, we are very grateful to the almighty God for giving us priceless health, well-being and support throughout our life. We would like to send sincere gratitude and invaluable acknowledgments to Mekelle University for sponsoring this research and to Dr Alemayehu Bayray for his scientific guidance, encouragement, comments and suggestions. Most importantly, we would like to thank the study participants. We are very grateful to Dr Carmen C Robles for her thorough English language evaluation.
Author contributions
Mamo Z Degebasa conceived the study, participated in the design of the study, performed statistical analysis and drafted the manuscript for important intellectual content. Dawit Zenebe Weldemichael directly participated in the planning of the research and guided all stages of the research, execution, and analysis of this study. Mokonnon T Marama was involved in the design and analysis of the study, helped to draft the manuscript, and revisited it critically for important intellectual content. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Farthing M, Salam MA, Lindberg G, et al. Acute diarrhea in adults and children: a global perspective. J Clin Gastroenterol. 2013;47(1):12–20. | ||
Diouf K, Tabatabai P, Rudolph J, Marx M. Diarrhoea prevalence in children under five years of age in rural Burundi: an assessment of social and behavioural factors at the household level. Glob Health Action. 2014;7. | ||
Mbutikimani H. Assessment of Diarrhoeal Disease Attributable to Water, Sanitation and Hygiene among Under Five in Kasarani, Nairobi, Kenya [master’s thesis]. Nairobi: Kenyatta University; 2013. | ||
Oklahoma State Department of Health. Global burden of diarrheal diseases. Previously available from: www.ok.gov/health2/documents/Global,Acute (Disease Service). Public Health Fact; 2014. | ||
Farthing M, Salam M, Lindberg G, et al; World Gastroenterology Organisation. Global guidelines. Acute diarrhea in adults and children; 2012. Available from: https://www.guidelinecentral.com/summaries/world-gastroenterology-organisation-global perspective. Accessed September 4, 2018. | ||
Gebru T, Taha M, Kassahu W. Risk factors of diarrhoeal disease in under-five children among health extension model and non-model families in Sheko district rural community, Southwest Ethiopia. BMC Public Health. 2014;14:395. | ||
Mashoto OK, Malebo MH, Msisiri E. Prevalence, one week incidence and knowledge on causes of diarrhea: Household survey of under-fives and adults in Mkuranga district, Tanzania. BMC Public Health. 2014;14:985. | ||
Mamo A, Hailu A. Assessment of prevalence and related factors of diarrheal diseases among under-five year’s children in Debrebirehan Referral Hospital, Debrebirehan town, North Shoa Zone, Amhara Region, Ethiopia. OA Lib J. 2014;1:1–14. | ||
WHO, UNICEF. Progress on Sanitation and Drinking Water: 2015 Update and MDG Assessment. Geneva: WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation (JMP); 2015. | ||
Lanata CF, Fischer-Walker CL, Olascoaga AC, Torres CX, Aryee MJ. Global causes of diarrheal disease mortality in children under 5 years of age: a systematic review. PLoS ONE. 2013;8(9):e72788. | ||
Assefa M, Kumie A. Assessment of factors influencing hygiene behaviour among school children in Mereb-Leke District, Northern Ethiopia. BMC Public Health. 2014;14:1000. | ||
Tessema RA. Assessment of the implementation of community-led total sanitation, hygiene, and associated factors in Diretiyara district, Eastern Ethiopia. PLoS ONE. 2017;12(4):e0175233. | ||
Crocker J, Geremew A, Atalie F, Yetie M, Bartram. Teachers and sanitation promotion: an assessment of community-led total sanitation in Ethiopia. Environ Sci Technol. 2016;50(12):6517–6525. | ||
James A, Fuller E, Clasen TH, M H, Joseph NS. Shared sanitation and the prevalence of diarrhea in young children: evidence from 51 countries. Am J Trop Med Hyg. 2014;91(1):173–180. | ||
Cha S, Kang D, Tuffuor B, et al. The effect of improved water supply on diarrhea prevalence of children under five in the Volta Region of Ghana. Int J Environ Res Public Health. 2015;12(10):127–143. | ||
Perez E, Cardosi J, Coombes Y, Devine J, Grossman A. Scaling up rural sanitation. What does it take to scale up rural sanitation? Paris: World Bank; 2012. | ||
Sanan D, Moulik GS. Water and sanitation programme. Community-led total sanitation in rural areas [government report]. In: S, ed. Rural Women’s Studies Association (RWSA). Noida, India: PS Press Services Pvt. Ltd; 2007:78–89. | ||
Cheng JJ, Schuster-Wallace JC, Watt S NK, Mente A. An ecological quantification of the relationships between water, sanitation and infant, child, and maternal mortality. J Environ Health. 2012;11(1):4. | ||
Clasen T, Boisson S, Routray P, et al. Effectiveness of a rural sanitation programme on diarrhoea, soil transmitted helminth infection, and child malnutrition in Odisha, India. Lancet Glob Health. 2014;2(11):645–653. | ||
Eshete N, Beyene A, Terefe G. Implementation of community-led total sanitation and hygiene approach on the prevention of diarrheal disease in Kersa District, Jimma Zone, Ethiopia. Sci J Pub Health. 2015;3(5):669–676. | ||
Central Statistical Agency [Ethiopia] and ICF International. Ethiopia Demographic and Health Survey. Addis Ababa, Ethiopia: CSA; 2012. | ||
Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey: Key Indicators Report. Addis Ababa, Ethiopia: CSA; 2016. | ||
Sinmegn MT, Alemie AG, Shimeka TA. Determinants of childhood diarrhea among underfive children in Benishangul Gumuz Regional State, North West Ethiopia. BMC Pediatr. 2014;14:102. | ||
Federal Ministry of Health [FMOH] [Ethiopia]. Implementation Guideline for CLTSH Programming. Addis Ababa, Ethiopia: FMOH; 2012. | ||
Wikipedia. Yaya Gulele Demography [updated 2014]. Available from: https://en.wikipedia.org/wiki/Yaya_Gulele. Accessed November 30, 2016. | ||
Central Statistical Agency (CSA) [Ethiopia]. Population Projection of Ethiopia for All Regions at Wereda Level from 2014 – 2017. Addis Ababa, Ethiopia: CSA; 2013. | ||
Makotsi N, Kaseje D, Mumma J, Opiyo J, Lukorito L. Association of community led total sanitation to reduced household morbidity in Nyando District. Int J Sci Basic Appl Res. 2016;6(22):224–576. | ||
WHO/UNICEF. Core Questions on Drinking-Water and Sanitation for Household Surveys. Geneva, Switzerland: WHO/UNICEF Joint Monitoring Programme for Water Supply and Sanitation; 2006. | ||
UNICEF/WHO. Diarrhoea: Why Children are Still Dying and What Can Be Done. Geneva, Switzerland: World Health Organization; 2009. | ||
Awodele O, Adeyomoye AA, Awodele DF, Kwassh IO, Awodele IO, 504 DD. A study on cervical cancer screening amongst nurses in Lagos University Teaching Hospital, Lagos, Nigeria. J Cancer Educ. 2011;26(3):497–504. | ||
Azage M, Kumie A, Worku A, Bagtzoglou CA. Childhood diarrhea in high and low hotspot districts of Amhara Region, northwest Ethiopia. J Health Popul Nutr. 2016;35(13). | ||
Merga N, Alemayehu T. Knowledge, perception, and management skills of mothers with under-five children about diarrhoeal disease in indigenous and resettlement communities in Assosa District, Western Ethiopia. J Health Popul Nutr. 2015;33(1):20–30. | ||
Kakulu RK. Diarrhea among Under-Five Children and Household Water Treatment and Safe Storage Factors in Mkuranga District, Tanzania [master’s thesis]. Dar es Salaam: Muhimbili University of Health and Allied Sciences; 2012. | ||
Mengistie B, Berhane Y, Worku A. Prevalence of diarrhea and associated risk factors among children under-five years of age in Eastern Ethiopia. Open J Prev Med. 2013;3(7):446–453. | ||
Hashi A, Kumie A, Gasana J. Prevalence of diarrhoea and associated factors among under-five children in Jigjiga District, Somali Region, Eastern Ethiopia. Open J Prev Med. 2016;6(10):233–246. | ||
Plan, UNC Water Institute. Testing CLTS Approaches for Scalability, Community-led Total Sanitation in Ethiopia: Findings from a Situational Assessment [research summary]. Chapel Hill: Carolina University; 2015. | ||
Njuguna J. Effect of eliminating open defecation on diarrheal morbidity: improving sanitation and sustainable. An ecological study of Nambale sub-country, Kenya. BMC Public Health. 2016;16:712. | ||
Addisu KA. The prevalence of diarrheal disease in under five children and associated risk factors in Wolitta Soddo Town, Southern Ethiopia. ABC Res Alert. 2015;3(2):2–11. | ||
Oloruntoba O E, Folarin BT, Ayede IA. Hygiene and sanitation risk factors of diarrhoeal disease among under-five children in Ibadan, Nigeria. Afr Health Sci. 2014;14(4):1001–1011. | ||
Tamiru B. Predictors of child diarrheal diseases in CLTSH and PHAST approach done implemented areas in shebedino district, Sidama zone, south Ethiopia [master’s thesis]. Addis Ababa: Addis Ababa University; 2013:1–78. | ||
Aidan A.C, Sebayang SK, Torlesse H, Nandy R. Association of safe disposal of child feces and reported diarrhea in Indonesia: need for stronger focus on a neglected risk. Int J Environ Res Pub Health. 2016;13(310):1–13. | ||
George CM, Oldja L, Biswas SH, et al. Unsafe child feces disposal is associated with environmental enteropathy and impaired growth. J Pediatr. 2016;176:43–49. | ||
Brown J, Cairncross S, Ensink JHJ. Water, sanitation, hygiene and enteric infections in children. Arch Dis Child. 2013;98:629–634. | ||
Amare D, Dereje B, Kassie B, Tessema M, Mullu G. Maternal knowledge and practice towards diarrhoea management in under five children in Fenote Selam Town, West Gojjam Zone, Amhara Regional State, Northwest Ethiopia. J Infect Dis Ther. 2014;2(6):182. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.