Back to Journals » Open Access Emergency Medicine » Volume 15
Diagnosis of Acute Appendicitis: A Cross-sectional Study on Alvarado’s Score from a Low Income Country
Authors Gebreselassie H, Zeleke H, Ashebir D
Received 10 March 2023
Accepted for publication 9 June 2023
Published 16 June 2023 Volume 2023:15 Pages 253—258
DOI https://doi.org/10.2147/OAEM.S410119
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Hana Gebreselassie,1 Henok Zeleke,2 Daniel Ashebir2
1Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia; 2Department of Surgery, Addis Ababa University, College of Health Sciences, Addis Ababa, Ethiopia
Correspondence: Hana Gebreselassie, Department of Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, Email [email protected]
Background: Alvarado score is the most widely used scoring system for diagnosing acute appendicitis, globally. There have been concerns regarding the diagnostic accuracy of this score as it was shown to have lower sensitivity in certain populations like Blacks and Asians. Despite its wide clinical use in the Ethiopian set up, the diagnostic accuracy of this score remained largely unexamined in this population.
Methodology: A prospective cross-sectional study was conducted and all adult patients who presented with right lower quadrant abdominal pain and evaluated with a clinical impression of acute appendicitis were enrolled in the study. Data was collected by trained surgical residents over a period of six months (August 2019– January 2020) and analysed using SPSS version 25.
Results: A total of 235 patients were enrolled in this study among whom two thirds were males. The majority of the study participants (61.7%) had an Alvarado score of ≥ 7 while almost a quarter of them had a score of < 4. The mean Alvarado score in this study was 7 ± 1.8 whereas the median and the mode were 7 and 9 respectively. The overall sensitivity, specificity, positive predictive value and negative predictive value of Alvarado score were 99.1%, 55.6%, 98.2% and 62.5% respectively. The sensitivity and specificity of this score was superior in males compared to females (99.3% vs 97.6% and 80% vs 25%). A score of ≥ 5 was found to have a sensitivity of 98.4%.
Conclusion: Alvarado score was found to have good sensitivity and positive predictive value in this study. A score of ≥ 5 can be used to “rule in” the diagnosis of acute appendicitis. Hence, the use of Alvarado score’s in the Ethiopian setup is to be encouraged.
Keywords: Alvarado score, acute appendicitis, sensitivity, specificity
Background
Acute appendicitis is the most common gastrointestinal pathology requiring urgent surgical intervention.1–4 Although population-based data is lacking in the Ethiopian setup, acute appendicitis has been shown to be the most common indication for emergency surgical intervention in several facility-based reports.5–9 Despite its common occurrence, its clinical diagnosis remained challenging.
Clinical evaluation of a patient who is suspected to have acute appendicitis through a meticulous history and physical examination has remained the mainstay of diagnosis.2,10 Although a number of diagnostic tools, including imaging modalities and biochemical tests, have been developed some reports have shown that, at a population level, the diagnosis of acute appendicitis has not improved with the availability of advanced diagnostic testing.11
The ideal evaluation of a patient with acute appendicitis aims to make an accurate diagnosis once the patient comes to the emergency department. The reported negative appendectomy rates vary between 11–40% in literature.12–18 A rate of 15–20% has been accepted as appropriate to reduce the incidence of perforation in the past but this figure is being challenged these days due to the high post-operative morbidity in patients who have undergone a negative appendectomy.19–24
This diagnostic difficulty has led to the need for developing objective ways of evaluating patients with suspected acute appendicitis by using scoring systems. More than ten scoring systems for the diagnosis of acute appendicitis have been described in the literature so far, with variable results in different setups. Among these, Alvarado’s score, which uses eight predictive factors with a total score of ten, is the most well described and widely used one.11,25,26
In prior studies done about Alvarado’s score sensitivity for the diagnosis of acute appendicitis, varied and conflicting results have been reported and racial difference has been mentioned as one factor for this difference. Some of the studies have found out that it has got a high sensitivity and recommended its routine use while the rest of the literature had an opposing report.27–32
In a low-income country setup like Ethiopia where imaging modalities such as ultrasound and computed tomography scan are neither widely available nor cost-effective, the diagnosis of acute appendicitis is mainly guided by clinical evaluation. Thus, it is crucial to have an effective clinical scoring system in order to minimize delayed intervention and unnecessary appendectomies as well.
This study will be helpful to provide objective data about the sensitivity of the widely used Alvarado’s score in the Ethiopian setup. Since the reliability of this score in our population is not yet tested, this facility-based study will serve as a stepping point to evaluate this scoring system in our context and also serves as a baseline for further population based study.
Methodology
This study was conducted in Menelik II Referral Hospital which is the first public Hospital in Ethiopia established in 1896 by Emperor Menelik II. The hospital serves many patients from the metropolis and surrounding towns.
A prospective observational study was conducted and all patients who presented to the adult emergency department with right lower quadrant acute abdominal pain and evaluated with a clinical suspicion of acute appendicitis were included in the study. Sample size was calculated by using the single population proportion formula using a P of 0.83 which is taken from a similar Indian study.
Data was collected for a period of six months by trained surgical residents using a questionnaire developed for the purpose of this study. Data coding and analysis was done using SPSS 25 (Statistical Packages for Social Sciences). Alvarado’s score was calculated for each patient using the clinical and laboratory parameters (Table 1). Frequencies and percentages were used to describe categorical variables. For continuous variables, mean was calculated. Sensitivity, specificity, positive predictive value and negative predictive value of Alvarado’s score were calculated using the respective formulas.
 |
Table 1 Components of Alvarado Score |
A written consent was taken from each study participant after the objective of this study is clearly explained to them. Ethical clearance was also obtained from the research and ethical board of the College of Health Sciences of Addis Ababa University. All research procedures were done in accordance with the Declaration of Helsinki.
Result
In the study period, 235 patients with acute abdominal pain were assessed in our institution with a clinical diagnosis of acute appendicitis and Alvarado’s score was calculated for each patient. Based on the clinical evaluation, a decision was made whether to proceed with surgical exploration or to follow the patients conservatively.
Socio Demographic Characteristics
Among the 235 patients, 150 (63.8%) were males with a male to female ratio of 1.8:1. The mean age of the study participants was 27.5 ± 8.5 years while the median and mode were 25 years and 27 years respectively. As to the age distribution, the youngest study participants, aged 18–25 years, accounted for 50.2% of the study population while those aged >40 years accounted for only 8.5%. The great majority of patients (88.5%) were residents of Addis Ababa.
Alvarado’s Score
The Alvarado score was calculated for all patients and it was ≥7 in 145 (61.7%) of the study population while 23 (9.8%) had a score of 4 or less. The mean Alvarado’s score of the study population was 7 ± 1.8 with a median of 7 and mode of 9. Among the 235 patients evaluated, 5 were kept in the emergency department for serial examination using the following parameters: worsening or improvement of symptoms, vital signs, abdominal exam and Alvarado’s score. They were not given any medications (neither analgesics nor antibiotics) and were just observed conservatively and discharged improved. The Alvarado score of these patients were five and less.
A grossly normal appendix was found intra operatively in 4 (1.7%) patients. As pathology service is not available in our Hospital, these specimens were not subjected to such examination. All of these patients had a score of five or less. All patients with Alvarado score of seven and above were operated on and had acute appendicitis of various stages intra operatively (Table 2).
 |
Table 2 Alvarado Score versus Intra Operative Finding |
The overall sensitivity and specificity of Alvarado score was 99.1% and 55.6% respectively. The sensitivity and specificity of this score was found to be lower in females compared to males (97.6% vs 99.3% and 25% vs 80% respectively) (Table 3). The positive predictive value of Alvarado score in this study was 98.2% while the negative predictive value was 62.5%.
 |
Table 3 Alvarado Score in Males vs Females |
The negative predictive value of Alvarado score, while using a score of 4 as a cut-off point, was 60% whereas it was found to be 100% at a cut-off point of 7 (Table 4). Hence, the later cut-off point was found to be reliable to rule out the diagnosis of acute appendicitis in this study.
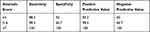 |
Table 4 Sensitivity, Specificity, Positive Predictive Value and Negative Predictive Value of Alvarado Score at Different Cut off Points |
Discussion
Even though acute appendicitis is the most common cause of an acute surgical abdomen, making an accurate and timely diagnosis of it remained challenging. Several clinical scores have been developed to this end and they have been especially useful in low income countries set up where modern imaging modalities are inaccessible and/or unaffordable to the public.
According to the Jerusalem guideline which was devised by the World Society of Emergency Surgery in 2020, clinical scores alone seem sufficiently sensitive to identify low-risk patients and decrease the need for imaging and negative surgical explorations in patients with suspected acute appendicitis.33 Another recent review also demonstrated that three scores for acute appendicitis including the Alvarado score, are sensitive enough to exclude appendicitis and decreased the need for imaging and the negative appendectomy rate.34
Among others, Alvarado’s score is the most well-known and widely used clinical scoring system for the diagnosis of acute appendicitis.11,22–24 In a recent review done by Alfredo Alvarado himself, Alvarado score was compared to other scoring methods for acute appendicitis and it was found to be associated with the lowest negative appendectomy rate and missed perforation rate.35
In the current study, 235 adult patients who presented to our emergency department with acute abdominal pain and evaluated with a clinical suspicion of acute appendicitis were included. The predominance of men seen in this study is also reflected in other reports.36–42 Our patients were found to be relatively young when compared to other study participants in studies done elsewhere while other scholars reported a comparable mean age with our patients.38–40,42,43
The mean Alvarado score in this study was found to be similar with a study from Qatar while it was higher compared to reports from India and Pakistan.40,42,43 The majority of our study participants (61.7%) had an Alvarado score of seven and above which was much lower than a report from Morocco (91%). On the other hand, this finding is significantly higher when compared to other studies in which less than half of the study participants (36.6–48%) had such a score.34–37 On the other hand, the percentage of patients who had a score of four and less was smaller in our study compared to other reports.36–39
The overall sensitivity of Alvarado score in this study was found to be similar with a result from one systematic review and another report from Morocco but significantly higher when compared to reports from Jordan, Tunisia, and Pakistan.37,40,44–46 On the other hand, the overall specificity of this score in our study (55.6%) was lower when compared to other reports in which it was in the range of 75–92.3%.37,40,43 In this study, the positive and negative predictive value of Alvarado's score were comparably higher than other reports.37,40,43
In this study, all patients with an Alvarado score of seven and above were operated on and had a confirmed acute appendicitis intraoperatively. Out of patients with a score of 5 or more, only one patient had a negative appendectomy. The sensitivity of Alvarado score at a score of 5 or more was 98.4% which is replicated in one systematic review and even higher than reports from Brazil, Qatar and Samoa.38,41,42,45 Hence, this cut off point can be recommended for “ruling in” the diagnosis of acute appendicitis based on this result.
A score of 4 or less was reported to be reliable to “rule out” the diagnosis of acute appendicitis in a study from Tunisia.46 This was contrary to our findings in that two thirds of our patients with such a score had acute appendicitis intraoperatively and also the negative predictive value of Alvarado score at this cut off point in this study was 60%. Therefore, we cannot safely recommend a score of 4 or less as a safe tool to rule out the diagnosis of acute appendicitis based on these findings.
From the results of this study we can conclude that Alvarado score is a good tool to diagnose acute appendicitis. Its use is especially significant in a set up like ours where modern diagnostic imaging modalities are not widely available or not cost-effective. This hospital based study can be used as a stepping stone to do a population based study in Ethiopia in order to get a better picture about the use of this scoring system at a larger scale as its validity has been questioned in the black population by some literatures.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Ammal Korpi HE, Mentula P, Leppaniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis - a prospective study. BMC Gastroenterol. 2014;14(1):114. doi:10.1186/1471-230X-14-114
2. Wagner M, John Tubre D, Asensio JA. Evolution and current trends in the management of acute appendicitis. Surg Clin North Am. 2018;98:1005–1023. doi:10.1016/j.suc.2018.05.006
3. Sartelli M, Baiocchi GL, Di Saverio S, et al. Prospective Observational Study on acute Appendicitis Worldwide (POSAW). World J Emerg Surg. 2018;13(1):19. doi:10.1186/s13017-018-0179-0
4. Baird DL, Simillis C, Kontovounisios C, Rasheed S, Tekkis PP. Acute appendicitis. BMJ. 2017;357:j1703. doi:10.1136/bmj.j1703
5. Kotiso B, Abdurahman Z. Pattern of acute abdomen in adult patients in Tikur Anbessa Teaching Hospital, Addis Ababa, Ethiopia. East Cent Afr J Surg. 2007;12(1):47–52.
6. Hagos M. Acute abdomen in adults: a two year experience in Mekelle, Ethiopia. Ethiop Med J. 2015;53(1):19–24.
7. Melkie A, Alemayehu T. Eyobe tarekegn; pattern of acute abdomen in Dil Chora Referral Hospital, Eastern Ethiopia. Int J Collab Res Intern Med Public Health. 2016;8(11):607–615.
8. Deneke A, Tadesse B. Pattern and clinical presentation of acute 360 appendicitis in adults in Zewditu memorial hospital. Ethiop J Health Sci. 2003;13(2):8.
9. Hanks L, Lin CP, Tefera G, Seyoum N. Abdominal surgical emergencies at Tikur Anbessa Specialized Hospital in Ethiopia; a shifting paradigm. East Cent Afr J Surg. 2014;19(1):90.
10. Petroianu A. Diagnosis of acute appendicitis. Int J Surg. 2012;10(3):115e11. doi:10.1016/j.ijsu.2012.02.006
11. Bhangu A, Søreide K, Di Saverio S, Hansson Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386(10000):1278–1287. doi:10.1016/S0140-6736(15)00275-5
12. Andersson RE, Hugander AP, Ghazi SH, et al. Diagnostic value of disease history, clinical presentation, and inflammatory parameters of appendicitis. World J Surg. 1999;23(2):133. doi:10.1007/PL00013174
13. Davies GM, Dasbach EJ, Teutsch S. The burden of appendicitis-related hospitalizations in the United States in 1997. Surg Infect. 2004;5(2):160–165. doi:10.1089/sur.2004.5.160
14. Pooria A, Pourya A, Gheini A. Appendicitis: clinical implications in negative appendectomy. Int J Surg. 2021;29:45–49.
15. Ahmed HO, Muhedin R, Boujan A, et al. A five-year longitudinal observational study in morbidity and mortality of negative appendectomy in Sulaimani teaching Hospital/Kurdistan Region/Iraq. Sci Rep. 2020;10(2028). doi:10.1038/s41598-020-58847-1
16. Sammalkorpi HE, Mentula P, Savolainen H, Leppäniemi A. The introduction of adult appendicitis score reduced negative appendectomy rate. Scand J Surg. 2017;106(3):196–201. doi:10.1177/1457496916683099
17. Raja AS, Wright C, Sodickson AD, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology. 2010;25:6.
18. Nyamuryekung’E MK, Athar A, Patel MR, et al. Negative appendectomy rate in urban referral hospitals in Tanzania: a cross-sectional analysis of associated factors. Ann Afr Surg. 2021;18(2):109–114. doi:10.4314/aas.v18i2.9
19. Gelpkea K, Hammingaa JTH, van Bastelaarb JJ, et al. Reducing the negative appendectomy rate with the laparoscopic appendicitis score; a multicenter prospective cohort and validation study. Int J Surg. 2020;79:257–264. doi:10.1016/j.ijsu.2020.04.041
20. Tamini N, Santurro L, Chiappetta MF, et al. Morbidity after negative appendectomy: a single-centre experience on 627 cases. Eur J Trauma Emerg Surg. 2020;46(4):859–864. doi:10.1007/s00068-019-01138-w
21. Geon Jeon B. Predictive factors and outcomes of negative appendectomy. Am J Surg. 2019;217:1094e1098.
22. Allaway MGR, Eslick GD, Cox MR. The unacceptable morbidity of negative laparoscopic appendicectomy. World J Surg. 2019;43:405–414. doi:10.1007/s00268-018-4784-6
23. Colson M, Skinner KA, Dunnington G. High negative appendectomy rates are no longer acceptable. Am J Surg. 1997;174(6):723e726. doi:10.1016/S0002-9610(97)00183-9
24. Lewis FR, Holcroft JW, Boey J, Dunphy EA. A critical review of diagnosis and treatment in 1000 cases. Arch Surg. 1975;110(5):677–684.
25. Snyder MJ, Guthrie M, Cagle S. Acute appendicitis: efficient diagnosis and management. Am Fam Physician. 2018;98(1):25–33.
26. Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15(5):557–579. doi:10.1016/S0196-0644(86)80993-3
27. Tahsin Tekeli M, Ilhan E, Ureyen O, et al. How much reliable is Alvarado scoring system in reducing negative appendectomy? Indian J Surg. 2017;79(2):106–110. doi:10.1007/s12262-015-1433-2
28. Kalliakmanis V, Pikoulis E, Karavokyros IG, et al. Acute appendicitis: the reliability of diagnosis by clinical assessment alone. Scand J Surg. 2005;94(3):201–206. doi:10.1177/145749690509400305
29. Munir K, Iqbal J, Mushtaq U, Ishaque I, Jabeen M, Khalid A. Modified Alvarado scoring system in the diagnosis of acute appendicitis. Ann Punjab Med Coll. 2008;2(2):91–94.
30. Hashemy AM, Seleem MI. Appraisal of the modified Alvarado score for acute appendicitis in adults. Saudi Med J. 2004;25(9):1229–1231.
31. Al-Hashemy AM, Seleem MI. Appraisal of the modified Alvarado score for acute appendicitis in adults. Saudi Med J. 2004;25(9):106–110.
32. Khan I, Ur Rehman A. Application of Alvarado scoring system in diagnosis of acute appendicitis. J Ayub Med Coll Abbottabad. 2005;17:41–44.
33. Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020;15(27). doi:10.1186/s13017-020-00306-3
34. Podda M, Pisanu A, Sartelli M, et al. Diagnosis of acute appendicitis based on clinical scores: is it a myth or reality? Acta Biomed. 2021;92(4):e2021231. doi:10.23750/abm.v92i4.11666
35. Alvarado A. Improved Alvarado score (MANTRELS) for the early diagnosis of acute appendicitis. Int J Surg Res Pract. 2019;6:098. doi:10.23937/2378-3397/1410098
36. Kong VY, Van der linde S, Aldous C, Handley JJ, Clarke DL. The accuracy of the Alvarado score in predicting acute appendicitis in the black South African population needs to be validated. Can J Surg. 2014;57(4):121–125. doi:10.1503/cjs.023013
37. Musa Al Awayshih M, Nabih Nofal M, Jad Yousef A. Evaluation of Alvarado score in diagnosing acute appendicitis. Pan Afr Med J. 2019;34(34):15. doi:10.11604/pamj.2019.34.15.17803
38. Do Nascimento RR, Souza JC, Alexandre VB, Kock KD, Kestering DD. Association between the Alvarado score and surgical and histopathological findings in acute appendicitis. Rev Col Bras Cir. 2018;45(5):e1901. doi:10.1590/0100-6991e-20181901
39. Ouedraogo NA, Ouedraogo S, Kambou BM, Ouedraogo A, Sanou A. Diagnosis of acute appendicitis in Sub-Saharan Africa. Open J Med Imaging. 2018;8:1–9. doi:10.4236/ojmi.2018.81001
40. Memon SN, Abro S, Pathan MR, et al. Diagnostic accuracy of ripasa and Alvarado score in detecting acute appendicitis. J Liaquat Uni Med Health Sci. 2022;1–10. doi:10.22442/jlumhs.2022.00912
41. Pifeleti S, Hansell D, Kaspar A. Sensitivity and specificity of the Alvarado score for the timely differential diagnosis of acute appendicitis for a case series in Samoa. Ann Med Surg. 2022;73:103219. doi:10.1016/j.amsu.2021.103219
42. Al-Tarakji M, Zarour A, Singh R, et al. The role of Alvarado score in predicting acute appendicitis and its severity in correlation to histopathology: a retrospective study in a Qatar population. Cureus. 2022;14(7):e26902. doi:10.7759/cureus.26902
43. Pasumarthi V, Madhu CP. A comparative study of RIPASA score and ALVARADO score in diagnosis of acute appendicitis. Int Surg J. 2018;5(3):796–801. doi:10.18203/2349-2902.isj20180430
44. El Hattabi K, Bouali M, El Berni Y, et al. Value of Alvarado scoring system in diagnosis of acute appendicitis. Ann Med Surg. 2022;77:103642. doi:10.1016/j.amsu.2022.103642
45. Ohle R, O’Reilly F, O’Brien KK, Fahey T, Dimitrov BD. The Alvarado score for predicting acute appendicitis: a systematic review. BMC Med. 2011;9:139. doi:10.1186/1741-7015-9-139
46. Maghrebi H, Maghraoui H, Makni A, et al. Role of the Alvarado score in the diagnosis of acute appendicitis. Pan Afr Med J. 2018;29:56. doi:10.11604/pamj.2018.29.56.14011
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
