Back to Journals » Clinical Ophthalmology » Volume 18
DEXTENZA versus Topical Steroid or Antihistamine Therapy for Treatment of Allergic Conjunctivitis
Authors Reich S, Lopez M, Leff J, Herman J
Received 20 November 2023
Accepted for publication 19 January 2024
Published 14 February 2024 Volume 2024:18 Pages 473—480
DOI https://doi.org/10.2147/OPTH.S440840
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Shani Reich,1 Maria Lopez,2,* Jacqueline Leff,3,* Jordan Herman1
1Clinical Research Center of Florida, Pompano Beach, FL, USA; 2New England Eye Center/Tufts Medical Center, Boston, MA, USA; 3Touro Osteopathic School of Medicine, Touro University, New York, NY, USA
*These authors contributed equally to this work
Correspondence: Shani Reich, Tel +1 305 984 7785, Fax + 1 305 570 2642, Email [email protected]
Purpose: To compare clinical outcomes and patient preference for the dexamethasone intracanalicular insert (DEX) versus topical loteprednol (LOT) or olopatadine (OLO) for the treatment of allergic conjunctivitis in a real-world model of allergen exposure.
Methods: This was a prospective comparative trial. Adults with testing-confirmed bilateral allergic conjunctivitis received DEX in the more symptomatic eye and either LOT 2 times daily or OLO once daily for 30 days in the fellow eye. The primary outcome was patient preference for treatment. Clinical outcomes included ocular itching and hyperemia, lid swelling, and watering/tearing. Safety outcomes included intraocular pressure (IOP).
Results: Thirty patients participated and completed the study. All received DEX in the eye with worse symptoms and 15 received LOT and the other 15 received OLO in the other eye. Patients preferred DEX (10/15; 66.7%) over LOT (4/15; 26.7%), with one patient having no preference (p = 0.0103). Patients had no preference between DEX (8/15; 53.3%) and OLO (6/15; 40%), with one patient having no preference (p = 0.1044). In the DEX/LOT cohort, ocular itching and hyperemia improved more with DEX than LOT (p ≤ 0.009), while in the DEX/OLO cohort, the DEX eyes showed greater improvement in conjunctival hyperemia (p < 0.0001) but not itching (p = 0.074). No between-group differences were seen in eyelid swelling or tearing/watering in either cohort. Mean change in IOP was similar between the DEX and LOT eyes (p = 0.4921), and mean IOP rose more in the DEX eyes than the OLO eyes (by < 1 mmHg; p = 0.0403).
Conclusion: Overall, this real-world study demonstrated that the dexamethasone intracanalicular insert was as effective as a topical antihistamine/mast cell stabilizer and more effective than topical steroids in relieving the signs and symptoms of allergic conjunctivitis. This insert should be considered as an alternative to topical therapy for the treatment of allergic conjunctivitis.
Keywords: dexamethasone, dextenza, allergic conjunctivitis
Introduction
Allergic conjunctivitis is a common cause of ocular itching, conjunctival hyperemia, and watering and can be triggered by both seasonal and perennial allergens. Its prevalence has been estimated at up to 40%.1 The condition negatively impacts quality of life and work productivity.2
The pathophysiology of allergic conjunctivitis involves immune responses mediated by histamine and mast cells.3 Treatment consists of antihistamines for immediate relief and mast-cell stabilizers for long-term control. Corticosteroids can be used for short periods to manage acute flares but safety issues such as elevated intraocular pressure (IOP) and cataract formation limit long-term use.3 Recently, Dextenza, a 0.4 mg dexamethasone intracanalicular insert (Ocular Therapeutix, Bedford, MA) has been approved for the treatment of ocular itching associated with allergic conjunctivitis; it is also approved for the treatment of ocular inflammation and pain following ocular surgery.4 The dexamethasone intracanalicular insert is a rod-shaped depot of 0.4 mg preservative-free dexamethasone encapsulated within polyethylene glycol-based hydrogel that expands after contact with fluid to occlude the punctum and secure its placement.5 Fluorescein is conjugated to the hydrogel to enable visualization. The insert delivers a sustained and tapered dose of dexamethasone to the ocular surface for up to 30 days and resorbs completely.5,6
In Phase 2 and 3 clinical trials, the dexamethasone insert relieved ocular itching associated with allergic conjunctivitis more effectively than placebo when evaluated using a modified conjunctival allergen challenge model.7,8 To date, no real-world studies have evaluated the insert’s effectiveness in managing signs and symptoms of clinical allergic conjunctivitis, nor have any studies included comparisons to other treatments for allergic eye disease. We have conducted a randomized trial comparing the dexamethasone insert to loteprednol—a topical corticosteroid—and to olopatadine—a topical antihistamine/mast cell stabilizer—in reducing the signs and symptoms of allergic conjunctivitis.
Methods
This was a prospective, randomized, active-controlled clinical trial. The trial was registered at ClinicalTrials.gov (NCT04708821) on January 14, 2021, and the protocol and consent form were reviewed and approved by the Advarra institutional review board on May 5, 2021. All subjects provided written consent to participate. The trial was conducted in accordance with the tenets of the Declaration of Helsinki. The investigators will consider appropriate requests for data sharing.
Eligible subjects were adults aged 18 years or older with best-corrected visual acuity (BCVA) ≥50 ETDRS letters (Snellen equivalent 20/100) in both eyes. All subjects had a history of bilateral ocular allergic symptoms. Key exclusion criteria included concurrent use of anti-inflammatory medications (including systemic, inhaled, or nasal steroids; ocular or topical nonsteroidal anti-inflammatory agents [NSAIDs]; and immunotherapeutic agents), use of systemic antihistamines or decongestants, lid scrubs for lid disease, or monoamine oxidase inhibitors, any abnormalities of the punctum that would prevent proper insertion of the implant, as well as any contraindications to study medications.
At a screening visit, potential subjects underwent an ocular examination that included assessment of BCVA, external and slit lamp evaluation of the anterior segment and ocular adnexa, and intraocular pressure (IOP) by Goldmann tonometry. Ocular hyperemia was graded by the investigator on a 0–4 scale (none, mild, moderate, severe, extremely severe) and eyelid swelling on a 0–3 scale (none, mild, moderate, severe). After slit lamp exam was completed, patients underwent allergy testing with DoctoRx’s Allergy Formula Ocular Allergy Diagnostic System (OADS). Patient-reported outcomes included subjective grading of ocular and nasal allergy symptoms including itching using a 9-point scale 0–4 in 0.5 increments from none to incapacitating, as well as watering/tearing using a 5-point scale 0–4 from none to extremely severe. A visual analog scale (VAS) consisting of a 100-mm line (0 = absent, 100 = maximal) was utilized to assess pain, photophobia, blurred vision, and lacrimation; subscores were summed for a total symptom score (TSS) ranging from 0 to 400.
Qualifying subjects attended a treatment visit within 2 weeks; all assessments described above except ocular allergy testing were repeated. Also, the Eye Allergy Patient Impact Questionnaire (EAPIQ) was administered. This validated instrument assessed the severity of ocular allergy symptoms, treatment, impact of symptoms on daily activities and emotions, and satisfaction with therapy;9,10 the latter section was not administered at the treatment visit. Following these assessments, subjects received the dexamethasone intracanalicular insert (the DEX group) in the self-reported most symptomatic eye and either the corticosteroid loteprednol 0.2% (Alrex, Alcon, the LOT group) 2 times daily or the antihistamine/mast cell stabilizer olopatadine (Pazeo, Alcon, the OLO group) once daily in the fellow eye for 30 days. The treatment assigned to the fellow eye was alternated between LOT and OLO 1:1. After insertion, DEX position was assessed by slit lamp examination. Adherence with topical therapy was assessed by the use of a patient dosing diary. Subjects were re-evaluated at days 3, 8, 15, and 30. BCVA, IOP, Slit lamp examination, patient grading of ocular and nasal symptoms, and TSS were assessed at every visit. Additionally at Day 30, the satisfaction section of the EAPIQ was administered using a 6-point Likert scale (very satisfied to very dissatisfied), as was treatment preference using a 5-point Likert scale (no preference, moderately or much preferred either treatment; “moderately” and “much” preferred were collapsed to “preferred” for analysis). Rescue therapy with topical steroids was available for uncontrolled symptoms.
The primary outcome was patient-reported treatment preference for self-administered versus physician-administered therapy at Day 30. Secondary outcomes included mean ocular hyperemia and itching scores, proportion of eyes with eyelid swelling and tearing/watering, rate of rescue therapy, mean change in TSS and IOP, and the incidence and severity of adverse events. Various types of data were collected in this study, for each data type the most appropriate analysis methods were used. Treatment preference was analyzed using binomial tests. Ocular hyperemia and itching scores were analyzed using the Wilcoxon Signed Rank test. Eyelid swelling and tearing/watering was analyzed using McNemar Chi-Squared. TSS and IOP were analyzed using repeated measures analysis of variance. There were no observations of incidences of rescue therapy or adverse events; no analysis was performed. No formal power analysis was undertaken; instead, a sample size adequate to estimate the primary outcome was selected based on recent similar studies.11–13
Results
Thirty subjects participated in this study; all subjects completed the study. All received DEX in the self-reported most symptomatic eye, and 15 received LOT and the other 15 received OLO in the fellow eye. Baseline demographic data for the study sample are given in Table 1; no clinically significant differences were noted between the 2 comparator groups at baseline.
 |
Table 1 Demographic Data for the Study Sample by Comparator Group |
Preference and Satisfaction Results
Overall, patients expressed a significant preference for the DEX insert over topical therapy, with 18/30 (60%) preferring DEX, 10/30 (33.3%) preferring topical therapy, and 2/30 (6.7%) having no preference (p = 0.0029; Figure 1). Within specific topical comparators, patients significantly preferred DEX over LOT: 10/15 (66.6%) preferred DEX, 4/15 (26.7%) preferred LOT, and 1/15 (6.7%) had no preference (p = 0.0103; Figure 1). In contrast, there was no clear preference between DEX and OLO: 8/15 (53.3%) preferred DEX, 6/15 (40%) preferred OLO, and 1/15 (6.7%) had no preference (p = 0.1044; Figure 1). Satisfaction with therapy was closely related to treatment preference (Table 2). Patients reported higher satisfaction scores related to allergy symptoms with DEX over LOT (p = 0.0241) but not DEX over OLO (p = 0.2931); similarly, satisfaction with the rate of symptom relief favored DEX over LOT (p = 0.0185) but not OLO (p = 0.6606).
 |
Table 2 Patient Satisfaction with Allergy Symptoms and the Rate of Symptom Improvement by Study Cohort, n (%) |
 |
Figure 1 Patient treatment preferences for DEX versus topical therapies LOT and OLO assessed at Day 30. |
Clinical Outcomes
The course of ocular itching (graded on a 0–4 scale) is shown in Figure 2. In the LOT cohort (Figure 2A), DEX-treated eyes improved continuously from a median baseline itching score of 2.5 to a median score of 0 at Days 15 and 30, while LOT-treated eyes plateaued on Day 3 with a median ocular itching score of 1.0 that persisted through the end of the study (p = 0.009 favoring DEX over LOT). In the OLO cohort (Figure 2B), itching scores improved from a median of 2.5 in both the DEX and OLO groups to 0 in both groups by Day 30 (p = 0.074).
 |
Figure 2 Median ocular itching score over time by study cohort and treatment groups. (A) LOT cohort; (B) OLO cohort. Error bars represent interquartile range. |
The course of ocular hyperemia (also graded on a 0–4 scale) is shown in Figure 3. In the LOT cohort (Figure 3A), DEX-treated eyes improved from a median baseline hyperemia score of 2.0 to a median score of 1 at Day 30, while LOT-treated eyes showed no improvement from baseline at any on-treatment time point (p = 0.0004 favoring DEX). In the OLO cohort (Figure 3B), hyperemia scores in the DEX group improved from a median of 2.0 at baseline to 1.0 at every follow-up visit, while scores in the OLO group improved from 2.0 at baseline to a range from 1.0–2.0 throughout follow-up (p < 0.0001 favoring DEX).
 |
Figure 3 Median ocular hyperemia score over time by study cohort and treatment groups. (A) LOT cohort; (B) OLO cohort. Error bars represent interquartile range. |
No between-group differences were seen in eyelid swelling or tearing/watering in either cohort (data not shown). The patient-level mean (SD) total symptom score improved significantly from 200 (84) at baseline to 90 (79) at every on-treatment visit (p ≤0.001) including at Day 30 (p < 0.0001).
No adverse events related to treatment were observed. No eyes required rescue therapy with topical steroids. Mean IOP (Table 3) was comparable between treatment groups in the LOT cohort (p = 0.4921) and slightly higher in the DEX group than the topical group in the OLO cohort (p = 0.0403).
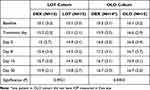 |
Table 3 Mean (SD) Intraocular Pressure at Each Time Point by Cohort and Treatment Group |
Discussion
To our knowledge, this is the first real-world study of the dexamethasone intracanalicular insert for allergic conjunctivitis. Patients experienced greater improvements in signs and symptoms with the dexamethasone intracanalicular insert than with the topical steroid loteprednol and preferred the insert to topical therapy by more than a 2-to-1 margin. Conversely, outcomes were similar and no clear preference was demonstrated between the insert and the use of the topical antihistamine/mast cell stabilizer olopatadine.
Statistical differences in signs and symptoms of allergic conjunctivitis favoring the dexamethasone insert over topical loteprednol therapy may be explained in several ways. First is the two drugs’ relative potency: dexamethasone is considered a highly potent corticosteroid while loteprednol is considered a weak corticosteroid.14 Second is differences in formulation. Solutions typically clear from the ocular surface within 15 minutes and suspensions within 2 hours.15 In contrast, the intracanalicular insert provides constant tapered delivery of dexamethasone over its ~30-day dosing period.6 Consequently, the bioavailability of drug at the ocular surface is likely greater with the dexamethasone insert compared to the loteprednol solution. Regarding the strong preference expressed by patients for the dexamethasone insert over topical loteprednol, part may be explained by the superior efficacy of the insert over topical drops in relieving the signs and symptoms of ocular allergy, while part may be related to the freedom from self-administration of topical drops 2 times daily for 30 days (60 instillations).
In contrast, there was no significant difference in improvement of most signs and symptoms of allergic conjunctivitis, nor a strong preference by patients, between the dexamethasone insert and the topical antihistamine/mast cell stabilizer olopatadine (OLO). Changes in ocular itching, eyelid swelling, and tearing/watering were similar between treatment groups, while there was a significant difference favoring the dexamethasone insert in ocular hyperemia. This may be explained in part by differences in mechanism of action of these two drugs. Antihistamines and mast cell stabilizers directly target the specific form of inflammation underlying allergic conjunctivitis, while corticosteroids have a broader and nonspecific action on histamine-mediated inflammation. In addition, OLO is used once daily with a reduced drop burden. Given the different mechanism of action, a further study to evaluate the use of both medications together may be useful.
All treatments evaluated in this study were safe and well tolerated. No treatment-related adverse events were observed. Mean IOP rose more in DEX eyes than in OLO eyes, and while the difference was statistically significant (p = 0.0403), the magnitude of the difference—less than 1 mmHg at any time point—was clinically insignificant. There was no difference in mean IOP between the DEX and LOT groups and the maximum IOP rise from baseline was less than 1 mmHg in both treatment groups.
In addition to the benefits evaluated in this study, there are other potential benefits of sustained drug delivery for allergic conjunctivitis and other ocular conditions. For example, sustained drug delivery in glaucoma might overcome the well-described high rate of therapeutic nonadherence16–20 that leads to higher progression rates.16,17,21,22 Specific to steroid therapy, long-acting (up to 3 years) intraocular implants incorporating fluocinolone acetonide have significantly reduced the treatment burden associated with repeated intraocular injections of short-acting steroids for various posterior segment disorders.23,24 Also, a sustained release delivery system for steroids at the ocular surface is a critical step toward a drop-free postoperative experience for cataract patients which has been advocated in recent years as a means of improving surgical outcomes.25–28
This study had several strengths related to its design. It was a prospective analysis. It was a real-world study seeking to characterize outcomes in a less rigidly defined study sample than is typical of large clinical trials. Also, it was a comparative study providing relative efficacy and safety data for therapies in common usage for the treatment of allergic conjunctivitis. Limitations include its small sample size and the inability for investigator masking given the need to confirm the placement of the dexamethasone insert at each visit. Also, patients were unmasked as they used topical medications in the non-insert eye. There is no reasonable basis for patient-related bias beyond being biased in favor of whichever drug made them feel better, which is the point of the study and the primary outcome. Lack of investigator masking could have introduced bias in the assessment of secondary outcomes. Selection of the worse eye for DEX therapy could have introduced a bias in that there was greater room for improvement in the worse eye, which would be in DEX’s favor. However, it could also be argued that the worse eye was less likely to achieve complete resolution of symptoms, which would be in the comparator’s favor.
Conclusion
Overall, this real-world study demonstrated that the dexamethasone intracanalicular insert was preferred over topical therapy and was as effective as a topical antihistamine/mast cell stabilizer and more effective than topical steroids in relieving the signs and symptoms of allergic conjunctivitis. This insert should be considered as an alternative to topical therapy for the treatment of allergic conjunctivitis. Larger head-to-head trials of therapies for allergic conjunctivitis can further clarify the roles of these agents in disease management.
Acknowledgments
Renate Gorham provided assistance with the statistical analysis of the data for this manuscript. Tony Realini, MD, MPH, provided editorial assistance with a preliminary draft of this manuscript.
Disclosure
Shani Reich MD reports funding to conduct this study and for editorial assistance provided by Ocular Therapeutix. The authors report no other conflicts of interest in this work.
References
1. Rosario N, Bielory L. Epidemiology of allergic conjunctivitis. Curr Opin Allergy Clin Immunol. 2011;11(5):471–476. doi:10.1097/ACI.0b013e32834a9676
2. Virchow JC, Kay S, Demoly P, Mullol J, Canonica W, Higgins V. Impact of ocular symptoms on quality of life (QoL), work productivity and resource utilization in allergic rhinitis patients--an observational, cross sectional study in four countries in Europe. J Med Econ. 2011;14(3):305–314. doi:10.3111/13696998.2011.576039
3. Labib BA, Chigbu DI, Pan G. Therapeutic targets in allergic conjunctivitis. Pharmaceuticals. 2022;16(1):15. doi:10.3390/ph16010015
4. Drugs@FDA: dextenza. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/208742s007lbl.pdf.
5. Blizzard C, Desai A, Driscoll A. Pharmacokinetic studies of sustained-release depot of dexamethasone in beagle dogs. J Ocul Pharmacol Ther. 2016;32(9):595–600. doi:10.1089/jop.2016.0025
6. Driscoll A, Blizzard C. Toxicity and pharmacokinetics of sustained-release dexamethasone in beagle dogs. Adv Ther. 2016;33(1):58–67. doi:10.1007/s12325-015-0280-7
7. Torkildsen G, Abelson MB, Gomes PJ, McLaurin E, Potts SL, Mah FS. Vehicle-controlled, phase 2 clinical trial of a sustained-release dexamethasone intracanalicular insert in a chronic allergen challenge model. J Ocul Pharmacol Ther. 2017;33(2):79–90. doi:10.1089/jop.2016.0154
8. McLaurin EB, Evans D, Repke CS, et al. Phase 3 randomized study of efficacy and safety of a dexamethasone intracanalicular insert in patients with allergic conjunctivitis. Am J Ophthalmol. 2021;229:288–300. doi:10.1016/j.ajo.2021.03.017
9. Alexander M, Berger W, Buchholz P, et al. The reliability, validity, and preliminary responsiveness of the Eye Allergy Patient Impact Questionnaire (EAPIQ). Health Qual Life Outcomes. 2005;3(1):67. doi:10.1186/1477-7525-3-67
10. Mikhail E, Azizoglu S, Gokhale M, Suphioglu C. Questionnaires assessing the quality of life of ocular allergy patients. J Allergy Clin Immunol Pract. 2020;8(9):2945–2952. doi:10.1016/j.jaip.2020.04.023
11. Greenwood MD, Gorham RA, Boever KR. A randomized fellow-eye clinical trial to evaluate patient preference for dexamethasone intracanalicular insert or topical prednisolone acetate for control of postoperative symptoms following bilateral femtosecond Laser in Site Keratomileusis (LASIK). Clin Ophthalmol. 2020;14:2223–2228. doi:10.2147/OPTH.S265311
12. Larsen J, Whitt T, Parker B, Swan R. A randomized controlled, prospective study of the effectiveness and safety of an intracanalicular dexamethasone ophthalmic insert (0.4 mg) for the treatment of post-operative inflammation in patients undergoing Refractive Lens Exchange (RLE). Clin Ophthalmol. 2021;15:2211–2217. doi:10.2147/OPTH.S311070
13. Suner IJ, Peden MC. Dexamethasone sustained-release intracanalicular insert for control of postoperative inflammation after pars plana vitrectomy. Clin Ophthalmol. 2021;15:3859–3864. doi:10.2147/OPTH.S330255
14. Sen P, Jain S, Mohan A, Shah C, Sen A, Jain E. Pattern of steroid misuse in vernal keratoconjunctivitis resulting in steroid induced glaucoma and visual disability in Indian rural population: an important public health problem in the pediatric age group. Indian J Ophthalmol. 2019;67(10):1650–1655. doi:10.4103/ijo.IJO_2143_18
15. Balla A, Ruponen M, Valtari A, et al. Understanding dexamethasone kinetics in the rabbit tear fluid: drug release and clearance from solution, suspension and hydrogel formulations. Eur J Pharm Biopharm. 2022;172:53–60. doi:10.1016/j.ejpb.2022.01.005
16. Rossi GC, Pasinetti GM, Scudeller L, Radaelli R, Bianchi PE. Do adherence rates and glaucomatous visual field progression correlate? Eur J Ophthalmol. 2011;21(4):410–414. doi:10.5301/EJO.2010.6112
17. Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011;118(12):2398–2402. doi:10.1016/j.ophtha.2011.05.013
18. Olthoff CM, Schouten JS, van de Borne BW, Webers CA. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112(6):953–961. doi:10.1016/j.ophtha.2004.12.035
19. Stewart WC, Chorak RP, Hunt HH, Sethuraman G. Factors associated with visual loss in patients with advanced glaucomatous changes in the optic nerve head. Am J Ophthalmol. 1993;116(2):176–181. doi:10.1016/S0002-9394(14)71282-6
20. Kass MA, Gordon M, Morley RE, Meltzer DW, Goldberg JJ. Compliance with topical timolol treatment. Am J Ophthalmol. 1987;103(2):188–193. doi:10.1016/S0002-9394(14)74225-4
21. Newman-Casey PA, Niziol LM, Gillespie BW, Janz NK, Lichter PR, Musch DC. The association between medication adherence and visual field progression in the collaborative initial glaucoma treatment study. Ophthalmology. 2020;127(4):477–483. doi:10.1016/j.ophtha.2019.10.022
22. Rajurkar K, Dubey S, Gupta PP, John D, Chauhan L. Compliance to topical anti-glaucoma medications among patients at a tertiary hospital in North India. J Curr Ophthalmol. 2018;30(2):125–129. doi:10.1016/j.joco.2017.09.002
23. Adan A, Cabrera F, Figueroa MS, et al. Clinical-decision criteria to identify recurrent diabetic macular edema patients suitable for fluocinolone acetonide implant therapy (ILUVIEN((R))) and follow-up considerations/recommendations. Clin Ophthalmol. 2020;14:2091–2107. doi:10.2147/OPTH.S252359
24. Zarranz-Ventura J, Mali JO. Effectiveness of 190 microg fluocinolone acetonide and 700 microg dexamethasone intravitreal implants in diabetic macular edema using the area-under-the-curve method: the CONSTANT analysis. Clin Ophthalmol. 2020;14:1697–1704. doi:10.2147/OPTH.S253370
25. Shorstein NH, Myers WG. Drop-free approaches for cataract surgery. Curr Opin Ophthalmol. 2020;31(1):67–73. doi:10.1097/ICU.0000000000000625
26. Lindstrom RL, Galloway MS, Grzybowski A, Liegner JT. Dropless cataract surgery: an overview. Curr Pharm Des. 2017;23(4):558–564. doi:10.2174/1381612822666161129150628
27. Assil KK, Greenwood MD, Gibson A, Vantipalli S, Metzinger JL, Goldstein MH. Dropless cataract surgery: modernizing perioperative medical therapy to improve outcomes and patient satisfaction. Curr Opin Ophthalmol. 2020;3:6.
28. Bardoloi N, Sarkar S, Pilania A, Das H. Efficacy and safety of dropless cataract surgery. Indian J Ophthalmol. 2020;68(6):1081–1085. doi:10.4103/ijo.IJO_1186_19
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
