Back to Journals » Psychology Research and Behavior Management » Volume 16
Development of the Panic Response Scale and the Predicting Factors of Panic Response During the COVID-19 Pandemic
Authors Tan Y, Lin X, Chen H, Xu M, Tang Y, Gao P, Ren W, Zhang D
Received 14 April 2023
Accepted for publication 13 July 2023
Published 31 July 2023 Volume 2023:16 Pages 2883—2895
DOI https://doi.org/10.2147/PRBM.S415240
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Yuxin Tan,1 Xiuyun Lin,1,2 Hui Chen,1 Min Xu,1 Yingying Tang,1 Pengfei Gao,1 Wei Ren,1 Di Zhang1
1Faculty of Psychology, Beijing Normal University, Beijing, People’s Republic of China; 2Beijing Key Laboratory of Applied Experimental Psychology, Faculty of Psychology, Beijing Normal University, Beijing, People’s Republic of China
Correspondence: Xiuyun Lin, Faculty of Psychology, Beijing Normal University, Beijing, 100875, People’s Republic of China, Email [email protected]
Introduction: During emergencies, individuals and communities often react in a variety of ways, including panic response. However, the study of panic response is limited due to narrow assessment tools that measure only one or two dimensions of human response (eg, physiology, cognition, emotion, and behavior). To address this limitation and to explore the risk and protective factors of panic response during the global spread of the Coronavirus Disease 2019 (COVID-19), the current study developed and evaluated the Panic Response Scale (PRS).
Methods: Four samples were recruited for the following purposes: interview analysis (n = 26); item analysis and exploratory factor analysis (n = 604); confirmatory factor analysis and reliability analysis (n = 603); and retest reliability, validity analysis, and regression analysis (n = 349).
Results: The PRS consists of 21 items with four subscales: Physical Discomfort, Anxious Fluster, Sensitive Depression, and Excessive Prevention. Each of these subscales demonstrated good internal consistency (rs > 0.73), test-retest reliability (rs > 0.77), criterion validity (r = 0.69, p < 0.01), and convergent validity (rs = 0.31– 0.65, p < 0.01). Regression analysis revealed significant predicting effects of COVID-19 knowledge and neuroticism on panic response. Additionally, cognitive reappraisal moderated the association between neuroticism and panic response.
Discussion: Following a traumatic event, the PRS offers a potential tool for identifying individuals in need of mental health services. Moreover, during the COVID-19 pandemic, knowledge and neuroticism served as risk factors for heightened panic response, while cognitive reappraisal served as a protective factor for coping with panic response.
Keywords: COVID-19, panic response, knowledge, neuroticism, cognitive reappraisal
Introduction
Worldwide, the increasing number of confirmed cases and deaths related to COVID-19 has been associated with increased mental health challenges.1–3 Likewise, several studies have linked the ongoing pandemic with psychological problems among individuals in China.4–7 Looking back to a study conducted during an outbreak of Severe Acute Respiratory Syndrome (SARS), panic response was one of the most severe stress reactions in affected individuals.8 Tong’s findings are similar to data gathered from the Psychological Assistance Hotline of Beijing Normal University which indicated that approximately 44.0% of clients suffered from panic response and panic-related issues during the COVID-19 pandemic.9 Symptoms associated with severe panic response included irrational behavior, compromised immune system, and an increased likelihood of infection.10–12 Considering these vulnerabilities, researchers need to more fully investigate both risk and protective factors associated with severe panic response. As such, an assessment instrument is needed to identify, measure, and compare the type and severity of symptoms.
Past measurements of panic response have been incomplete and lack sufficient sensitivity. Previous studies have solely relied on clinical scales measuring anxiety and depression.8 One recent study only utilized one direct question to measure the severity and extent of panic.7 Additionally, other researchers have indirectly measured the severity of panic through risk cognition or the number of people who reported suffering panic during the SARS outbreak13 and COVID-19 pandemic.14 Because the existing measurement of panic response solely involves one or two aspects related to physiology (as gastrointestinal discomfort and diarrhea), cognition (as difficulty concentrating and forgetfulness), emotion (as anxiety and fear), or behavior (as obsession and avoidance),13,15,16 a systematic and sensitive panic response measurement is urgently needed.
After the development and measurement of the Panic Response Scale (PRS), the risk and protective factors of panic response were considered in our study. The diathesis-stress model indicates that individuals with higher vulnerability are more sensitive to the influence of stressors from an external negative environment, further exacerbating emotional and/or behavioral problems.17 Under this theoretical framework, several researchers have studied the influence of negative environments (eg, stressful life events) and individual temperament characteristics (eg, neuroticism) on emotional disorders, such as anxiety and depression.18–21 Accordingly, the combined descriptors of environmental external stimuli and an individual’s internal personality may contribute to predict the level of panic response.
As learned from prior epidemics, knowledge of external stimuli is important in controlling the public’s response to the pandemic.13,22–24 For example, Dorfan and Woody (2011) noted that safety knowledge may diminish public fear. Moreover, during an outbreak of Ebola, Yang and Chu (2018) found that perceived risk of contracting the virus was associated with higher levels of negative emotion (eg, fear, anxiety). However, a Harvard School of Public Health (HSPH) poll suggested that panic surrounding the epidemic was not associated with knowledge about the actual risk, but occurred because of a more direct and visceral reaction to the risk.25 In this study, based on the prior findings and considering the diathesis-stress model, the level of COVID-19 knowledge was expected to be a predictor of panic response.
For internal personality, neuroticism was previously associated with the immune system26 and was also a marker of vulnerability in contracting COVID-19.27 Neuroticism, known as one of the Big Five personality traits, represents the persistent tendency to experience negative emotions, including anxiety, anger, guilt, and depression. To date, there is a paucity of knowledge regarding the personality trait of neuroticism and its impact on psychological outcomes (eg, negative affect, subjective well-being) during the COVID-19 pandemic.28–31 For example, Kroencke et al found that individuals high in neuroticism experienced more negative affect and higher affective variability in their daily lives, paid more attention to COVID-19-related information and worried more about the consequences of the pandemic (crisis preoccupation). We propose that, to the best of our knowledge, no study has adequately explored the effect of neuroticism on all aspects of panic response (including physiological, cognitive, emotional, and behavioral aspects). Therefore, this study proposed neuroticism as a risk associated with developing panic response.
Remarkably, previous studies found that the emotional and behavioral problems were effectively reduced by using emotional regulation strategies.18,21,32,33 Cognitive reappraisal and expressive suppression are the most often used emotion regulation strategies.34 However, it is generally considered that cognitive reappraisal is superior to expressive suppression.35,36 Notably, cognitive reappraisal was identified as a moderator between individual factors (eg, cultural alienation, neuroticism, and emotional perceptions) and psychological outcomes such as well-being, sleep quality, and depression.37–39 For example, Gu and Hyun (2019) demonstrated that cognitive reappraisal had a moderating effect on the relationship between neuroticism and sleep quality. Furthermore, Gu and Hyun (2019) tentatively speculated that cognitive reappraisal moderated the association between COVID-19 knowledge and panic response, and the relation between neuroticism and panic response.
Overall, to understand individual panic response and the associated protective and risk predictors, this study highlighted the need for development of the PRS. The first purpose of the current study was to develop a scale with feasibility for measuring the panic response of individuals during the COVID-19 pandemic, involving physiological, emotional, cognitive, and behavioral perspectives. The second purpose, from the perspective of prevention and reduction of panic response, was to explore the effects of COVID-19 knowledge and neuroticism on panic response. And the third purpose of the current study was to examine the moderating role of cognitive reappraisal in the association between COVID-19 knowledge and panic response, and the relationship between neuroticism and panic response.
Method
Participants
Study Design and Population
This was an empirical study that combined the interview method and questionnaire survey method. The research protocol was approved by the Institutional Review Board of Beijing Normal University. Prior to taking part in this research study, participants gave their informed consent. Payment of 10 RMB ($1.43 USD) was given to each participant after completing the questionnaire at each stage.
Description of Sample for Individual Interviews
There were 26 interviewees recruited from 11 regions across China, including Jiangxi province, Shandong province, Hubei province (center of the pandemic), Zhejiang province, Guangdong province, Beijing and so on in considering the distance from COVID-19 epidemic center. Participants included eight general residents stayed at home, six first-line medical staffs, six community service staffs and six professionals with psychological assistance experience. The total sample included 12 males and 14 females. The average age of participants was 30.96 years (SD = 8.59), ranged from 21 to 57.
Description of Samples for Statistical Analysis: Sample 1 and Sample 2
A total of 1218 questionnaires were collected. Of these, 11 questionnaires were excluded because of missing information, leaving 1207 valid questionnaires. The questionnaires were randomly divided into two samples. A total of 604 questionnaires (sample 1) were used for item analysis and exploratory factor analysis (EFA). The remaining 603 questionnaires (sample 2) were used for confirmatory factor analysis (CFA) and internal consistency coefficient (ICC).
Description of Sample 1 for Item Analysis and EFA
In sample 1 (n = 604), participants included 24 minors under 18 years (4.0%); 468 in early adulthood, ages 18–35 (77.5%); and 112 in the mid-adulthood, ages 36–60 (18.5%). The average age of all participants in this sample was of 27.41 years old (SD = 9.47). This sample included 175 males (29.0%) and 429 females (71.0%). Participants lived in the following locations: 190 participants (31.5%) resided in Hubei province (center of the pandemic with above 80% confirmed cases and 90% deaths during COVID-19 pandemic in China), 112 participants (18.5%) were from surrounding areas of Hubei province (Henan province, Anhui province, Jiangxi province, Hunan province, Chongqing province, Shanxi province), and 302 participants (50.0%) resided in other locations (except for the provinces mentioned above) in China.
Description of Sample 2: CFA and ICC
In sample 2 (n = 603), 22 participants reported ages under 18 years (3.7%); 479 reported ages in early adulthood, ages 18–35 (79.4%); and 102 reported ages in mid-adulthood, ages 36–60 (16.9%). The average age of participants in this sample was 27.69 years (SD = 9.22). Of the total participants, this sample included 192 males (31.8%) and 411 females (68.2%). Participants resided in the following locations: 208 participants (34.5%) were from Hubei province, 115 participants (19.1%) were from surrounding areas of Hubei province, and 280 participants (46.4%) resided in other locations in China.
Description of Sample for Retest
Of the 349 individuals, enrolled in in previous stage, participated in the retest, five participants were under 18 years of age (1.4%); 300 in early adulthood, ages 18–35 (86.0%); and 44 in the mid-adulthood, ages 36–60 (12.6%). The average age of participants was 26.42 years (SD = 8.42). Of the total participants, the sample included 100 males (28.7%) and 249 females (71.3%). Of the 349 initial participants, 348 were included in the sample for the retest involved in the predicting factors regression analysis. One participant’s retest was excluded due to missing information about their location of residence. Of the 348 participants who reported the location of their residence, 97 participants (27.9%) were from Hubei province, 66 participants (19.0%) were from surrounding areas of Hubei province, and 185 participants (53.1%) reported residing in other locations in China.
Survey Procedure
First, we prepared the interview outline according to related research literature and considering specific circumstances of the epidemic. At the beginning of the interview, we assessed the degree of each participant’s self-reported panic during the COVID-19 outbreak (eg, “Do you feel panic? If so, please assess the level of panic: ‘10 = extreme panic,’ ‘5 = medium degree of panic,’ ‘0 = Not feeling panic at all’”).
Then, we asked the interviewee to describe the response or expression of their panic (psychological, physical. and behavioral). After reviewing the related research literature and considering information gathered from the interviews, 26 items for measuring panic response were summarized, covering four descriptive aspects: physiological, emotional, cognitive, and behavioral. Next, two professors and five postgraduates who majored in psychology were invited to evaluate and revise these items. The evaluation included whether the description of each item was accurate; whether the item was in line with the actual situation; whether the item was not included, but considered important by the evaluator; and whether the content of the item was repeated. After this evaluation, 24 initial items were identified and clarified. Finally, this survey was disseminated through the WeChat platform and surveys were conducted online via a Chinese survey website [www.wjx.cn]. The questionnaire was collected through two stages. For the first stage, questionnaires were used for item analysis, EFA and CFA. For the second stage, a retest of the questionnaire was conducted three weeks after the first test. The retest was used for reliability analysis and validity analysis.
Measures
Candidate Items
Based on the interviews and professionals’ assessment, 24 items were formed to measure panic response, involving physiological, emotional, cognitive, and behavioral aspects. All questionnaire items included the same response options, a 5-point Likert scale ranging from 1 (totally disagree/disconfirm) to 5 (totally agree/confirm).
Validation Scales
For validations scales, because panic response is closely related to mental health, this study used the General Health Scale (GHS-12) and four subscales from the Symptom Checklist 90 (SCL-90). More specifically, the four subscales included somatization, anxiety, depression, and obsessive-compulsive.
The GHS-12 has good reliability and validity and is considered one of the most popular measurements to identify and measure psychological problems.40,41 Higher scores indicate more severe psychological problems. In this study, Cronbach’s α was 0.89.
The SCL-90 is a commonly used self-rating scale of mental health symptoms.42 Higher scores indicate more severe psychological problems. The SCL-90 is mainly used to measure the conscious symptoms and severity of psychological problems.43 The instrument’s subscales of somatization, anxiety, depression, and obsessive-compulsive have good reliability and validity.44 In this study, Cronbach’s α of these four subscales was 0.91, 0.90, 0.89, 0.92, respectively.
COVID-19 Knowledge
Participants were asked to answer whether they knew the details surrounding COVID-19 (eg, the time of Wuhan blockade, ways of transmission, symptoms, diagnostic criteria, etc). Participants responded to five items, each with yes (1) or no (0). Scores were averaged across items. Higher scores indicated greater knowledge of COVID-19.
Neuroticism
The neuroticism subscale of Neuroticism Extraversion Openness Five-Factor Inventory (NEO-FFI) was used to measure individual personality characteristics.45 The NEO-FFI included 12 items. Items were scored on a 5-point Likert scale, ranging from 1 (totally disagree) to 5 (totally agree). Scores were averaged across items, with higher scores indicating greater instability of mood. In this study, Cronbach’s α for the NEO-FFI was 0.89.
Cognitive Reappraisal
Six items of the cognitive reappraisal subscale of the Emotion Regulation Questionnaire (ERQ) were used to measure participants’ emotional regulation strategy.46 Items were scored on the 7-point Likert scale that ranged from 1 (totally incompatible) to 7 (totally compatible). Scores were averaged across items, with higher scores indicating stronger ability for cognitive reappraisal. In this study, Cronbach’s α for this subscale of ERQ was 0.84.
Data Analyses Plan
For the development and preliminary evaluation, we employed SPSS 20.0 for item analysis, EFA, correlation analysis, reliability analysis, and validity analysis. We employed Mplus 7.4 for CFA. To further explore the predicting factors, we adopted SPSS 20.0 for the hierarchical multiple regression analysis.
Results
Correlations of Items
The results of item analysis showed that all correlation coefficients between each item and the total score were larger than 0.4, thus none of the items were deleted. As planned, the newly developed questionnaire included 24 items.
Extraction of Common Factors
Before conducting EFA, the suitability of this analysis was examined. The value of Bartlett’s Test of Sphericity was 6350.51, p < 0.01, which indicated the possibility of EFA. Meanwhile, the value of Kaiser-Meyer-Olkin (KMO), a measure of sampling adequacy, was 0.92, greater than the commonly accepted standard 0.50. This demonstrates the suitability of the data for conducting factor analysis. Additionally, among all the items, the minimum measure of sampling adequacy (MSA) was 0.84, more than 0.50, indicating no need to eliminate items prior to conducting factor analysis. EFA of the 24 items used principal component analysis. Three items with cross loading and factor loading less than 0.40 were deleted, leaving 21 remaining items. Results of this analysis are presented in Table 1. The cumulative interpretation rate of the four dimensions was 61.3%. According to the meaning of each item, the four dimensions were labeled: physical discomfort, anxious fluster, sensitive depression, and excessive prevention.
 |
Table 1 Factor Loading of Each Item |
Confirmatory Factor Analysis (CFA)
Excellent fit is indicated by standardized root mean squared error (SRMR) ≤ 0.08; root mean square error of approximation (RMSEA) ≤ 0.06; and comparative fit index (CFI) ≥ 0.95. Good fit is indicated by comparative fit index (CFI) ≥ 0.90.47 The results showed that the four dimensions had an excellent fit: χ2/df = 2.88, RMSEA = 0.06, CFI = 0.95, Tucker Lewis Index (TLI) =0.93, and SRMR =0.05.
Reliability Analysis
The internal consistency of physical discomfort, anxious fluster, sensitive depression, excessive prevention was 0.89, 0.84, 0.79, 0.73 and 0.91, respectively. The results of retest showed that the test-retest reliability of physical discomfort, anxious fluster, sensitive depression, excessive prevention was 0.88, 0.90, 0.86, 0.77 and 0.93, respectively.
Validity Analysis
The correlation coefficient was used as criterion validity and convergent validity. The results showed that the total scores of the PRS and the GHS-12 were significantly and positively correlated (r = 0.69, p < 0.01), indicating good criterion validity. The scores of physical discomfort, anxious fluster, sensitive depression and excessive prevention were significantly and positively associated with somatization, anxiety, depression and compulsive symptoms respectively (rs = 0.31–0.65, p < 0.01), indicating good convergent validity.
Sample Characteristics
One-way ANOVA was conducted to compare sample characteristics, in which gender, age and location were identified as independent variables. The four dimensions of panic response and the total panic response were identified as dependent variables (see Table 2). Results indicated that the scores of physical discomfort, anxious fluster, sensitive depression, and total panic response for females were significantly higher than that of males (ps < 0.01). According to Post Hoc Test results, the score of excessive prevention for individuals from others (places far from Hubei province) was significantly lower than that of Hubei province and its surrounding areas (ps < 0.05).
 |
Table 2 Characteristics of Neuroticism, Cognitive Reappraisal and Panic Response (N = 348) |
Post Hoc Tests also showed that the scores of physical discomfort and anxious fluster for participants in early adulthood were significantly higher than that of minors (ps < 0.05); the scores of anxious fluster, sensitive depression, and excessive prevention for participants in early adulthood were significantly higher than that of mid-adulthood participants (ps < 0.01); the score of total panic response in early adulthood was higher than that of minors (p < 0.05) and mid-adulthood participants (p < 0.01)..
Correlations of Variables
Correlations among the variables are presented in Table 3. COVID-19 knowledge was positively correlated with excessive prevention (r = 0.12, p < 0.05), and neuroticism was positively correlated with physical discomfort, anxious fluster, sensitive depression, excessive prevention, and total panic response (rs = 0.25–0.45, p < 0.01). For demographic variables, gender was positively associated with cognitive reappraisal, physical discomfort, anxious fluster, sensitive depression, and total panic response (rs = 0.15–0.30, p < 0.01), while gender was negatively associated with COVID-19 knowledge (r = −0.12, p < 0.05); location was negatively related to excessive prevention (r = −0.15, p < 0.01); age was solely negatively correlated with neuroticism (r = −0.14, p < 0.05). Thus, gender and location were examined as covariates in the subsequent analyses.
 |
Table 3 Correlations Among All Variables |
The Predicting Effects of COVID-19 Knowledge and Neuroticism
The results of hierarchical multiple regression analysis in Table 4 showed that the COVID-19 knowledge significantly predicted anxious fluster (B = 0.27, p < 0.05), excessive prevention (B = 0.28, p < 0.01), and total panic response (B = 0.17, p < 0.05). Additionally, neuroticism significantly predicted physical discomfort (B = 0.31, p < 0.001), anxious fluster (B = 0.41, p < 0.001), sensitive depression (B = 0.52, p < 0.001), excessive prevention (B = 0.35, p < 0.001), and total panic response (B = 0.39, p < 0.001).
 |
Table 4 Predict Factors of Panic Response |
The Moderating Roles of Cognitive Reappraisal
Although the current study failed to find the moderating role of cognitive reappraisal in the association between COVID-19 knowledge and panic response, the results of hierarchical multiple regression analysis showed the moderating role of cognitive reappraisal in the relationship between neuroticism and panic response. Table 5 displayed the significant interacting effects between neuroticism and cognitive reappraisal on anxious fluster and excessive prevention (ps < 0.01), suggesting that cognitive reappraisal moderated the effect of neuroticism on anxious fluster and excessive prevention. With gender in the model, age and location failed to show a significant predicting effect on anxious fluster. Results showed that gender (β = 0.20, p < 0.01), neuroticism (β = 0.33, p < 0.01), and the interaction between neuroticism and cognitive reappraisal (β = −0.14, p < 0.01) significantly predicted anxious fluster. With location of residence left in the model, gender and age failed to show a significant predicting effect on excessive prevention. However, results showed that location (β = −0.15, p < 0.01), neuroticism (β =0.27, p < 0.01), and the interaction between neuroticism and cognitive reappraisal (β = −0.11, p < 0.05) significantly predicted excessive prevention.
 |
Table 5 Moderating Effects of Cognitive Reappraisal |
Figures 1 and 2 illustrate the results of a simple slope test. This regression line indicates that neuroticism predicted anxious fluster and excessive prevention more robustly at the lower end of cognitive reappraisal scores.
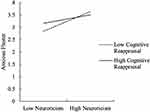 |
Figure 1 The Moderating effects of Cognitive Reappraisal on the Relationship between Neuroticism and Anxious Fluster. Note: “High” = M + 1SD, “Low” = M - 1SD. |
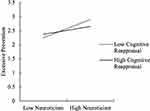 |
Figure 2 The Moderating effects of Cognitive Reappraisal on the Relationship between Neuroticism and Excessive Prevention. Note: “High” = M + 1SD, “Low” = M - 1SD. |
Discussion
On the basis of interview, item analysis, exploratory factor analysis (EFA), confirmatory factor analysis (CFA), reliability analysis, and validity analysis, the current study developed and analyzed the Panic Response Scale (PRS) in China during the COVID-19 pandemic. This scale is proposed to measure the panic response in China. With future evaluation outside of China, this scale might be possibly used in other countries. The PRS offered a more sensitive and complete tool to better understand the panic response associated with COVID-19. Additionally, the PRS further identified the risk and protective predictors associated with panic response. Briefly, this study highlighted the characteristics of individuals at-risk for panic response during the COVID-19 pandemic. Descriptors that were associated with higher panic response included being female, in early adulthood, in Hubei Province, with more COVID-19 knowledge, and for those with higher neuroticism. Fortunately, as a protective factor, cognitive reappraisal moderated the effects of neuroticism on panic response. Theoretically, these findings support the diathesis-stress model and offer insights to inform epidemic prevention policies and psychological intervention.
With rigorous procedures, the PRS was developed and initially validated with good reliability and validity. First, 26 initial items with comprehensive information of panic response were formulated and refined through interview, involving physiological, emotional, cognitive, and behavioral aspects. Upon further refinement and analysis, the number of items was reduced to 21. These items were categorized into four subscales that assessed the COVID-19 panic response: physical discomfort, anxious fluster, sensitive depression, and excessive prevention, which cumulatively explained most of the variance. The subscales performed well on various indices of reliability and validity, and were intercorrelated. Additionally, the CFA showed that all indicators were acceptable,48–51 suggesting an excellent fit of the four dimensions. The coefficients of internal consistency reliability coefficients of physical discomfort, anxious fluster, sensitive depression, and excessive prevention were above 0.73, meeting the recommended standard of psychometric.52 Finally, the retest reliability indicated good stability of the PRS.
The PRS directly measured the different dimensions of the panic response, which expanded the measurement’s sensitivity and utility. Among these dimensions, physical discomfort was associated with the physiological reaction produced during emergency situations, related to nerve conduction, nerve regulation, change in hormone production, activity in the cerebral cortex, and so on. Anxious fluster referred to heightened anxiety and flustered reactions. Sensitive depression referred to a somber mood and emotionally sensitive reactions. Excessive prevention referred to blind repetition and conformity of prevention behavior. However, existing measurements of panic response solely measure anxiety and depression or indirectly measure risk with low reliability.7,8,13,14 Comparatively, the PRS is a comprehensive and sensitive scale for panic response measurement with good reliability and validity, and is capable of being used in similar epidemic situations.
According to the diathesis-stress model, COVID-19 knowledge and neuroticism were found to be risk predictors of panic response. Cognitive reappraisal was identified as a protective factor diminishing the panic response. For COVID-19 knowledge, this study found it positively predicted anxious fluster and sensitive depression. Similar to previous studies, perceived risk of Ebola was associated with higher levels of fear and anxiety.23 A recent national survey also demonstrated that participants’ knowledge about COVID-19 was positively related to precautionary behavior.24 The current study discovered that neuroticism predicted the four dimensions of physical discomfort, anxious fluster, sensitive depression, and excessive prevention. Generally, people with high neuroticism fail to adequately address stressful situations, are more likely to interpret normal conditions as threats, and to perceive small setbacks as overwhelming challenges.27,53 Prior research supports these findings and notes the predicting effect of neuroticism on mental health disorder.18–21 The information processing model helps explain why neuroticism would be a risk predictor of panic response. Meanwhile, the plastic (flexible and open to change) information processing model hints that the risk predicting effect of neuroticism would be moderated by changing the interpretation of a stressful situation. The present study supports this and demonstrates that cognitive reappraisal moderated the relationship between neuroticism and panic response, specifically in the areas of anxious fluster and excessive prevention.
This study also revealed that certain characteristics place individuals at higher risk for panic response, specifically being a female, in early adulthood, and living in the Hubei province, the center of the COVID-19 pandemic. According to a previous study,13 the level of panic among females was higher than that of males because females tended to be more sensitive than males. A recent study found that age might be a potential risk factor for developing psychological problems, and younger participants (< 35 years) were more likely to develop anxiety and depressive symptoms during the COVID-19 outbreak.5 Similar to this research, a previous study in Taiwan during SARS54 also found that individuals in early adulthood were more likely to experience panic response. In the current study, those residing in the Hubei province, the center of the COVID-19 pandemic, faced the most extreme challenges related to COVID-19. Naturally, one would expect that these individuals would struggle with more excessive prevention than those living elsewhere.
Limitations
When reviewing and making sense of this study’s findings, it is important to understand the limitations of this study. First, the most prominent limitation is the uneven sampling. All provinces and cities in China were not represented. Future studies could include more provinces in China. Additionally, many more females than males were included in this study. Participants were not representative of the general public and occupations. Future studies could consider and balance the demographic information when screening subjects, such as gender and occupation. Furthermore, not all ages were adequately represented. Most of the participants were adults, while children under 12-years-old and elderly individuals were not included. Future studies may expand the sample size, especially to balance subjects to more adequately represent the population. Another limitation, participants were solely from China. Future studies should conduct cross-cultural research in order to understand the differences in panic response across populations. Finally, it is difficult to make causal inferences since the data and relevant analyses were derived from a cross-sectional design. Future research should consider conducting a longitudinal design in order to examine the temporal ordering and direction of effects.
Implications
Notwithstanding these limitations, the current study developed the PRS, which demonstrated good reliability and validity. Data analyses provided information about the risk and protective predictors of panic response. Our findings provided a more sensitive and complete tool for better understanding panic response associated with COVID-19. Additionally, this study highlighted the escalated risk factors facing women, people in early adulthood, people living in Hubei province, individuals with more COVID-19 knowledge, and those with higher neuroticism. It is noteworthy that cognitive reappraisal moderated the association between neuroticism and anxious fluster, and the relationship between neuroticism and excessive prevention. Therefore, interventions and policies might focus on individuals’ cognitive reappraisal and on the type of information disseminated about COVID-19 and the manner in which educational information is presented.
Conclusion
Our study indicates that the PRS is a comprehensive and sensitive scale that can be used in the Pandemic to measure panic response, and cognitive reappraisal moderate the association between neuroticism and anxious fluster, and the relationship between neuroticism and excessive prevention. These findings highlight the potential benefits of cognitive reappraisal in reducing the risk of high neuroticism on panic response. However, given the limitations of our small and uneven sample size, further research with larger and multicultural samples is necessary to provide more evidence on the effectiveness of the PRS and the potential benefits of cognitive reappraisal in reducing the risk of high neuroticism on panic response during the Pandemic. Healthcare providers should consider the benefit of cognitive reappraisal during the intervention and guidance, while policymakers should focus on and supervise the content and type of disseminated information to reduce the negative impact of the relevant information during the Pandemic.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical Approval
Prior to conducting the study, the Institutional Review Board of Beijing Normal University in China approved the research protocol, including the consent procedure. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
In the current study, participants aged from 12–60 years old. Before the study, participants signed informed consent forms.
Acknowledgments
The study described in this report was Funded by National Key R&D Program of China, the COVID-19 Prevention and Research Emergency Project of Beijing Normal University and the COVID-19 Mental Health Support Project of the Department of Psychology of Beijing Normal University. The content is solely the responsibility of the authors and does not necessarily represent the official views of Administration for Reacher and Development, Beijing Normal University. We are appreciative of the participants in our study and the many people who assisted in data collection.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Song FF, Wand X, Ju ZY, et al. Mental health status and related influencing factors during the epidemic of coronavirus disease 2019 (COVID–19). J Prev Med Public Health. 2020;31(2):23–27.
2. Yang Y, Wang H. Fear of COVID-19 and anxiety: serial mediation by trust in the government and hope. Psychol Res Behav Manag. 2023;16:963–970. doi:10.2147/PRBM.S399466
3. Yang Y, Wei W, Wang T. The relationship between perceived vulnerability to disease and anxiety during the COVID-19 pandemic: serial mediation by fear of COVID-19 and trust in the government. Psychol Res Behav Manag. 2023;16:989–996. doi:10.2147/PRBM.S398555
4. Cao WJ, Fang ZW, Hou GQ, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287:1–5. doi:10.1016/j.psychres.2020.112934
5. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288:1–6. doi:10.1016/j.psychres.2020.112954
6. Liu NQ, Zhang F, Wei C, et al. Prevalence and predictors of ptss during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287:1–7. doi:10.1016/j.psychres.2020.112921
7. Tian FY, Li HH, Tian SC, et al. Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 2020;288:1–9. doi:10.1016/j.psychres.2020.112992
8. Tong HJ. Model of sars stress and it’s character. Acta Psychol Sin. 2004;36(1):103–109.
9. Tan Y, Lin X, Wu D, et al. Different trajectories of panic and the associated factors among unmarried Chinese during the covid‐19 pandemic. Appl Psychol. 2020;12(4):967–982. doi:10.1111/aphw.12238
10. Arafat SM, Kar SK, Marthoenis M, et al. Psychological underpinning of panic buying during pandemic (COVID-19). Psychiatry Res. 2020;289:113061. doi:10.1016/j.psychres.2020.113061
11. Sim K, Chua HC, Vieta E, et al. The anatomy of panic buying related to the current COVID-19 pandemic. Psychiatry Res. 2020;2020:288.
12. Yu X. Strategies for overcoming panic during the COVID-19 epidemic. Chin Ment Health J. 2020;34(3):278–279.
13. Xie XF, Zheng R, Xie DM, et al. Analysis on psychological panic phenomenon of SARS. Acta Sci Naturalum Univ Pekinesis. 2005;41(4):628–639.
14. Nie XT, Feng K, Wang SN, et al. Factors influencing public panic during the COVID-19 pandemic. Front Psychol. 2021;12:1–10. doi:10.3389/fpsyg.2021.576301
15. Jiang HL. Research Group Panic Psychology and Behavior Features Based on Resource Constraint in Crises [Master’s Degree]. Shanghai Jiao Tong University; 2009.
16. Liu Y. Study on the Influence of Group Panic Psychology on the Unsafe Evacuation Behavior of Subway Passengers [Master’s Degree]. Xi’an University of Science and Technology; 2019.
17. Rosenthal D. Theoretical overview: a suggested conceptual framework. In: Rosenthal D, editor. The Genain Quadruplets: A Case Study and Theoretical Analysis of Heredity and Environment in Schizophrenia. Basic Books Inc; 1963:505–516.
18. Andrés ML, Richaud de Minzi MC, Castaneiras C, et al. Neuroticism and depression in children: the role of cognitive emotion regulation strategies. J Gen Psychol. 2016;177(2):55–71. doi:10.1080/00221325.2016.1148659
19. Bourgeois ML, Brown TA. Perceived emotion control moderates the relationship between neuroticism and generalized anxiety disorder. Cognit Ther Res. 2015;39(4):531–541. doi:10.1007/s10608-015-9677-5
20. Mohammadkhani P, Abasi I, Pourshahbaz A, et al. The role of neuroticism and experiential avoidance in predicting anxiety and depression symptoms: mediating effect of emotion regulation. Iran J Psychiatry Behav Sci. 2016;10(3):1–8.
21. Paulus DJ, Vanwoerden S, Norton PJ, et al. Emotion dysregulation, psychological inflexibility, and shame as explanatory factors between neuroticism and depression. J Affect Disord. 2015;190:376–385. doi:10.1016/j.jad.2015.10.014
22. Dorfan NM, Woody SR. Danger appraisals as prospective predictors of disgust and avoidance of contaminants. J Soc Clin Psychol. 2011;30:105–132. doi:10.1521/jscp.2011.30.2.105
23. Yang JZ, Chu HR. Who is afraid of the Ebola outbreak? The influence of discrete emotions on risk perception. J Risk Res. 2018;21(7):1–22. doi:10.1080/13669877.2016.1247378
24. Li JB, Yang A, Dou K, et al. Chinese public’s knowledge, perceived severity, and perceived controllability of the COVID-19 and their associations with emotional and behavioral reactions, social participation, and precautionary behavior: a national survey; 2020.
25. HSPH. Poll finds many in U.S. lack knowledge about Ebola and its transmission; 2014. Available from: http://www.hsph.harvard.edu/news/press-releases/poll-finds-manyin-us-lack-knowledge-about-ebola/.
26. Segerstrom SC. Personality and the immune system: models, methods, and mechanisms. Ann Behav Med. 2000;22(3):180–190. doi:10.1007/BF02895112
27. Khosravi M. Neuroticism as a marker of vulnerability to COVID-19 infection. Psychiatry Investig. 2020;17(7):710–711. doi:10.30773/pi.2020.0199
28. Damaris A, Strickhouser JE, Sesker A, et al. Psychological and behavioural responses to coronavirus disease 2019: the role of personality. Eur J Pers. 2020;2020:1.
29. Kroencke L, Geukes K, Utesch T, et al. Neuroticism and emotional risk during the COVID-19 pandemic. Ment Health Weekly Digest. 2020;2020:365–394.
30. Modersitzki N, Phan LV, Kuper N, et al. Who is impacted? Personality predicts individual differences in psychological consequences of the COVID-19 pandemic in Germany; 2020.
31. Szenczy AK, Nelson BD. Neuroticism and respiratory sinus arrhythmia predict increased internalizing symptoms during the covid-19 pandemic. Pers Individ Dif. 2021;182(2):111053. doi:10.1016/j.paid.2021.111053
32. Crow T, Cross D, Powers A, et al. Emotion dysregulation as a mediator between childhood emotional abuse and current depression in a low-income African-American sample. Child Abuse Negl. 2014;38(10):1590–1598. doi:10.1016/j.chiabu.2014.05.015
33. Duncombe ME, Havighurst SS, Holland KA, et al. The contribution of parenting practices and parent emotion factors in children at risk for disruptive behavior disorders. Child Psychiatry Hum Dev. 2012;43(5):715–733. doi:10.1007/s10578-012-0290-5
34. Gross JJ. The emerging field of emotion regulation: an integrative review. Rev Gen Psychol. 1998;2(3):271–299.
35. Wang DY, Zhou L. Between psychological well-being and negative academic emotions in left-behind middle school student in Anhui Province in 2016: the moderating role of cognitive reappraisal. J Hyg Res. 2017;46(6):935–941.
36. Yuan JJ, Long QS, Ding NX, et al. Suppression dampens unpleasant emotion faster than reappraisal: neural dynamics in a Chinese sample. Sci China Life Sci. 2014;44(6):602–613.
37. Cai YD, Ye BJ. The effect of cultural alienation on well-being of minority students in Han district colleges: the moderating effect of emotion regulation strategies. Chin J Clin Psychol. 2016;24(1):49–52.
38. Gu XY, Hyun MH. The moderating effect of emotion regulation on the relationship between neuroticism and sleep quality. Int J Content. 2019;15(1):25–31.
39. Kerswell NL, Strodl E. Emotion and its regulation predicts gluten-free diet adherence in adults with coeliac disease. Health Psychol Behav Med. 2015;3(1):52–68. doi:10.1080/21642850.2015.1010534
40. Li H, Boey KW. Assessing psychological well-being of college students: psychometric properties of GHQ-20. Psychol Dev Educ. 2002;18(1):75–79.
41. Li YM, Li YX. The factor structure of the 12- item general health questionnaire: the multi-group analyses. Psychol Explor. 2015;35(4):335–359.
42. Derogatis LR, Unger R. Symptom Checklist-90-Revised. John Wiley & Sons, Inc; 2010.
43. Liu YY, Wu SJ, Li YQ, et al. A survey of mental symptoms of Chinese population based on scl-90. Chin Ment Health J. 2018;32(5):437441.
44. Chen SL, Li LJ. Re-testing reliability, validity and norm applicatility of SCL-90. Chin J Nerv Ment Dis. 2003;29(5):323–327.
45. Costa PT, McCrae RR. Revised NEO Personality Inventory (NEO PI-R) and NEO Five-Factor Inventory (NEO-FFI) Professional Manual. PAR Psychological Assessment Resources Inc; 1992.
46. Gross JJ, John OP. Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J Pers Soc Psychol. 2003;85(2):348–362. doi:10.1037/0022-3514.85.2.348
47. Taylor S, Landry CA, Paluszek MM, et al. Development and initial validation of the covid stress scales. J Anxiety Disord. 2020;72:1–7. doi:10.1016/j.janxdis.2020.102232
48. Angel CM, Woldetsadik MA, Mcdaniel JT, et al. Confirmatory factor analysis of the enriched life scale among us military veterans. Front Psychol. 2019;10:2181. doi:10.3389/fpsyg.2019.02181
49. Chyung YS, Winiecki DJ, Hunt G, et al. Measuring learners’ attitudes toward team projects: scale development through exploratory and confirmatory factor analyses. Am J Eng Educ. 2017;8(2):61–82.
50. Flora DB, Flake JK. The purpose and practice of exploratory and confirmatory factor analysis in psychological research: decisions for scale development and validation. Can J Behav Sci. 2017;49(2):78–88. doi:10.1037/cbs0000069
51. Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6:1–55. doi:10.1080/10705519909540118
52. Wu XC, Liu C, Hu YR, et al. Development and validation of father involvement questionnaire. Chin J Clin Psychol. 2015;23(4):576–579.
53. Cohen S, Janicki-Deverts D, Crittenden CN, et al. Personality and human immunity. In: Segerstrom SC, editor. The Oxford Handbook of Psychoneuroimmunology. Oxford University Press; 2012:146–169.
54. Su TP, Lien TC, Yang CY, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. 2007;41(1–2):119–130. doi:10.1016/j.jpsychires.2005.12.006
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
