Back to Journals » Patient Preference and Adherence » Volume 17
Development of a Specific Variant of Patient Benefit Index (PBI) Assessing Patient Needs, Goals and Benefits in Rosacea Treatment
Authors Augustin M , Sommer R, Blome C, Kirsten N , Langenbruch A
Received 14 February 2023
Accepted for publication 9 May 2023
Published 1 June 2023 Volume 2023:17 Pages 1335—1345
DOI https://doi.org/10.2147/PPA.S378724
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Matthias Augustin, Rachel Sommer, Christine Blome, Natalia Kirsten, Anna Langenbruch
German Center for Health Services Research in Dermatology (CVderm), Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Hamburg, Germany
Correspondence: Matthias Augustin, German Center for Health Services Research in Dermatology (CVderm), Institute for Health Services Research in Dermatology and Nursing (IVDP), University Medical Center Hamburg-Eppendorf (UKE), Martinistraße 52, Hamburg, 20246, Germany, Tel +49 40 7410 55428, Fax +49 40 7410 55348, Email [email protected]
Introduction: Evaluation of patient-reported outcomes including health-related quality of life (HRQoL) and perceived benefits from treatment has become a fundamental component of medical decision-making. Standardized evaluation of treatment benefits in rosacea based on patient preferences is still lacking.
Objective: Development and validation of an instrument for recording patient-defined benefits in rosacea therapy based on the Patient Benefit Index (PBI) methodology.
Patients and Methods: In an open survey of n = 50 patients, potential benefits of therapy from the patient’s perspective were examined. The generated item pool was combined with pre-existing PBI items for other skin conditions and reviewed by an expert panel of dermatologists, psychologists and patients. Items were condensed to n = 25 and converted into a Likert-scaled questionnaire. The validity and feasibility of the resulting Patient Benefit Index for rosacea (PBI-RO) were tested on individuals with rosacea recruited from a German rosacea patient organization.
Results: N = 446 patients with rosacea completed the PBI-RO. The internal consistencies measured by Cronbach’s alpha were high (Patient Needs Questionnaire [PNQ] 0.94). Mean PBI-RO was 1.9 ± 1.2 (scale from 0 = no benefit to 4 = maximum benefit), 23.5% of the patients experienced a PBI-RO < 1 (no clinically relevant benefit). The PBI-RO correlated with HRQoL, health state, current extent of rosacea lesions and treatment satisfaction. The highest correlation was found between PBI-RO and satisfaction with previous treatment (r = − 0.59, p < 0.001); correlation with the extent of rosacea lesions was low (r = 0.16, p < 0.001).
Conclusion: The PBI-RO shows satisfying internal consistency and construct validity. It offers the option of a patient-weighted evaluation of the therapeutic benefit of rosacea therapy and may add to more stringent goal orientation in therapy.
Keywords: patient needs, treatment goals, disease burden, health-related quality of life, Patient Benefit Index, rosacea
Introduction
Rosacea is a chronic inflammatory dermatosis characterized by persistent erythema and telangiectasia, papules and pustules affecting mostly the face.1,2 Rare locations are the periorbital areas, neck, décolleté and scalp. Different clinical variants and degrees of severity can occur. As a late consequence of rosacea, particularly men can develop rhinophyma.3 Ocular complications such as blepharitis, conjunctivitis and even keratitis have been described.4
Throughout Germany, rosacea occurs in adult persons with a frequency of 2.3% on average, ranging from 0.2% in adults <25 years to >6% in those >65 years.5 Men are mildly more frequently affected than women (2.43% vs 2.11%). Global prevalence may be higher but in most studies subject to uncertainty.6
The etiology of this dermatosis is still unclear. It is believed that rosacea is a multifactorial disease in which genetics, vascular disorders, sebaceous gland hypoplasia as well as inflammatory influences, emotional stress and environmental factors can contribute to genesis.7–9 In about 30–40% of all affected people, family history is positive. Environmental influences such as UV radiation, strong temperature fluctuations, heat and cold are regarded as triggers of rosacea.10 Treatment remains challenging and there is no cure or sustained response without active treatment.11 According to the currently valid German guideline of 2022, topical metronidazole, azelaic acid and ivermectin are indicated as the first choice. In persistent centrofacial erythema, brimonidine or oxymetazoline may also be considered.
In severe or refractory cases of rosacea, systemic therapy is recommended. Low-dose doxycycline is the first option, in further cases isotretinoin. In cases of ocular involvement of rosacea, lid margin hygiene is important and topical preparations containing ciclosporin, azithromycin, ivermectin or metronidazole are used. General measures include identification and avoidance of trigger factors.12 Recently, also laser treatments have been shown to be effective.13
Though not burdensome as psoriasis or eczema in most cases, rosacea can cause psychological restrictions14 related to the visibility of lesions perceived as stigmatizing and to physical discomfort.15 Patients of different ages have to deal with conspicuous red spots in the prominent parts of the face, which can be very stressful psychologically for the reasons mentioned. Weak self-esteem, auto-aggression, anxiety, social withdrawal and isolation have been observed in various studies.10,15 Coping with disease may thus be negatively affected.16 An intensive education of the patients about the possible course of the disease, as well as the combination of clinical and psychological care can contribute to a better coping with disease.
Recent data have demonstrated a moderate impairment of health-related quality of life (HRQoL) and a moderate willingness to pay as a marker for disease burden.17 Nevertheless, some patients do suffer from more severe burden.18 In spite of that, the average quality of healthcare for rosacea in Germany was rated only moderate.19 In particular, many patients did not consider their treatment effective. In this nationwide study, some even experienced marked burden and side effects from treatment. Thus, there is a need for improving quality of healthcare and patient benefits in rosacea on a large scale. This could be facilitated with a goal-oriented treatment approach as has been established in other fields like psoriasis.20,21 In the latter, a consensus on treatment goals was established22,23 and tools for better identification of needs, goals and benefits were consented.19,24,25 The principle of goal attainment scaling as used in the Patient Benefit Index (PBI) is to define patients’ treatment goals before therapy and evaluate achievement in the course of therapy. Previous versions have shown the validity26 and stability of the overall score as well as of the subscales27 of this technology.
The aim of this study was to develop and validate a patient-reported outcomes tool measuring patient needs (reflecting treatment goals) and resulting benefits from rosacea therapy in order to enable patients and clinicians to be better informed about the therapeutic needs and to use treatment goals more efficiently.
Patients and Methods
Study Design
The study was performed in two steps: first a development study on the rosacea-specific PBI questionnaire including item selection with patient involvement, second a validation study on patients with rosacea.
Patient and Outcomes Parameters
Socio-Demographic Data
Socio-demographic data including gender, age, marital status, income (own and household), household size, schooling, occupation, type of everyday activity, place of residence, height and weight were obtained.
Health-Related Quality of Life and Quality of Healthcare
The measurement of dermatology-specific quality of life was carried out with the Dermatology Life Quality Index (DLQI) consisting of ten items. The generic health condition was measured with the visual analogue scale (VAS) of the EuroQol five dimensions questionnaire (EQ-5D),28,29 whereby the patient assessed his current state of health on a scale ranging from 0 (“worst imaginable health state”) to 100 (“best imaginable health state”).
Quality of healthcare as rated by the patients was also obtained with two single items, one asking for the overall healthcare, the other for satisfaction with rosacea treatment.
Extent of Rosacea Lesions
For the assessment of the extent of rosacea lesions, a grid scheme of the head containing small squares and 612 interception points was completed by the patients. They were asked to mark all areas which they considered affected by rosacea. For analysis, not the squares themselves but the interception points of two lines located within the patient’s drawing were counted.
Development of PBI-RO for Rosacea
Creation of an Item Pool on the Basis of Open Patient and Physician Surveys
In accordance with internationally accepted standards of psychometric test development,30,31 an open patient survey (n = 50) initially generated a pool of items by asking open questions on personally relevant therapeutic benefits.
Development of a Questionnaire for Benefit Assessment by a Panel of Experts with Patient Participation
An expert panel (two dermatologists, two psychologists and two patients) reduced the item pool obtained to particularly relevant patient-related benefits of rosacea treatment. The selected items were transferred to a questionnaire. A 5-point Likert scale (0 = “not at all”, 1 = “somewhat”, 2 = “moderately”, 3 = “quite”, 4 = “very”), supplemented by the option “does not apply to me” was chosen as a response scale like in most other variants of PBI.32,33
Characteristics of the Benefit Index PBI
The PBI methodology involves the identification of patient needs from treatment based on the single items of the Patient Needs Questionnaires (PNQ), a standardized list to be answered by the patient before treatment. The needs constitute weighted treatment goals from the patient perspective. The achievement of these individually rated goals is considered a patient benefit and is measured during the course of therapy or at the end of therapy using the Patient Benefit Questionnaire (PBQ) which used the same items as the PNQ. Scaling leads from 0 = “Treatment did not help at all” to 4 = “Treatment helped very much”. Patients can also rate “Did not apply to me”.
Finally, the preferences before therapy (PNQ) and the benefits achieved from therapy (PBQ) are converted into a weighted index value, the Patient Benefit Index (PBI). The global score PBI is computed for each patient according to the following algorithm. The importance of each treatment goal is divided by the sum of all importance values of the respective patient and is multiplied with the goal attainment value. The resulting products are added up. This can take values between 0 (“no benefit”) and 4 (“maximum benefit”).
The procedure used ensures that patients for whom only a few goals were particularly important at the beginning of treatment can achieve the same high overall value as patients for whom more goals were important.
Based on previous studies for several indications, patients with PBI ≥ 1 are considered having at least minimum patient-relevant treatment benefit. The target criterion for the “response” of a treatment is therefore the percentage of patients for whom a PBI > 1 was achieved.
Validation Markers of the Patient Benefit Index for Rosacea (PBI-RO)
The cross-sectional validation was conducted in collaboration with the German rosacea association using standardized questionnaires. Inclusion criteria were the presence of a clinically confirmed rosacea and age ≥18 years. Participants returned the completed questionnaires by post mail.
It was planned to recruit a sample of at least n = 400 patients with rosacea being in contact with a German rosacea patient organization. No remuneration was given.
Validation Procedures
Validation procedures followed the standards of international test psychology.34 Briefly, they contained feasibility, reliability and construct validity (Table 1). The latter indicates that a test developed to evaluate a specific construct (ie, anxiety) is in fact measuring this construct and includes convergent and discriminant validity. Convergent validity relates two measures supposed to measure the same construct and demonstrates their correlation. By contrast, discriminant validity demonstrates that two instruments not supposed to measure the same construct are in fact unrelated.
 |
Table 1 Validation Procedures for the Patient Benefit Index for Rosacea (PBI-RO) |
Feasibility of the questionnaire was assessed in an independent sample of n = 50 patients with rosacea from routine care at the dept of dermatology, University Medical Center Hamburg-Eppendorf (UKE). A 5-point Likert questionnaire from 0 = “not feasible” to 4 = “very feasible” was used.
Data Management and Statistical Analysis
All data were analyzed descriptively using standard statistical measures (frequencies for categorical data, mean value, standard deviation for continuous data).
A Pearson product moment correlation coefficient was calculated examining the statistical relationship between EQ VAS, DLQI, current rosacea severity assessed by the patient, satisfaction with previous treatment and the PBI-RO. Differences between correlation coefficients were tested35 for significance.
Means were compared between subgroups (patient needs of male vs female participants and PBI-RO of patients aged ≤50 vs >50 years) by unpaired t-tests. For the adjustment of alpha errors, a Bonferroni correction was conducted.
Missing values were not replaced. The α level was set at 5%. All analyses were performed with IBM SPSS Statistics for Microsoft Windows, version 23.0 (IBM Corp, Armonk, NY).
Results
Socio-Demographic Data
Data from n = 475 patients were obtained in 2008/2009. Related to population, all federal regions of Germany were represented. The majority of participants were female (79.9%), mean age was 56.3 ± 12.5 years, the youngest participant was 26 years old, the oldest 90 years. The majority were married (59.8%). The working status was reported by 226 patients (48.5%). The highest school degree was held by 31.8%, 40.3% had a medium secondary school degree, 19.6% had a lower secondary school degree. In the last 12 months, 15 people (7.5% of 199 workers) had been unable to work for at least one day due to rosacea. Average time off work lasted 9.1 ± 11.0 days.
History and Clinics of Rosacea
The initial diagnosis of rosacea was 8.8 ± 8.2 years ago on average. Patients having first-degree relatives who also suffered from rosacea were 106 (22.6%).
The extent of rosacea lesions was drawn by the patients in the front head/face area of the figure According to this figure, 7.4% ± 6.8% of the facial area was affected on average.
On a scale of 0–4 (0 = “not affected” to 4 = “extremely affected”), the patients indicated which regions of the head and neck area were affected and to what intensity, respectively. The nose and cheek area were described as most severely affected.
Almost all patients (96.4%) had received topical therapy in the last five years. Ointments containing cortisone were used by 24%. Systemic therapies were received by 41% of patients.
63.6% of patients who received treatment felt little or no treatment induced stress.
Satisfaction with Care and Treatment
Respondents rated the quality of rosacea care over the last few years on a scale of 1–5 (1 = “very good” to 5 = “insufficient”). The majority (41%) rated the care as mediocre and 27.5% rated the care as poor/unsatisfactory. The majority (49.6%) were moderately satisfied with the previous treatment. About one-third (33.8%) were rather or very dissatisfied with it.
Health-Related Quality of Life
The mean total value in the questionnaire on dermatology-specific quality of life (DLQI, scale from 0 = “no loss” to 30 = “maximum loss”) was 4.3 ± 4.6 (for comparison: atopic eczema 8.5 ± 6.0,36 psoriasis: 6.7 ± 6.237). Significant loss of quality of life (DLQI > 10) was found in 11%. Stating a value over 50 on the VAS of the EQ-5D and rating their state of health as rather good (0 = “worst imaginable”, 100 = “best imaginable health”) was done by 73.3%.
Patient Needs and Benefits (PBI)
Development of the Questionnaire
Conjointly with patients, the medical and psychological expert group identified eight de novo items (eg, “tolerate heat and cold better”) and 17 items from previously existing PBI standard version (PBI-S) (eg, “… feel less depressed”) as most relevant for the PBI-RO version. These were included in a questionnaire with 25 items as described previously (Table 2).
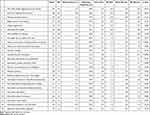 |
Table 2 Patient Needs from Treatment (n = 475) |
Patient Therapeutic Needs (Patient Needs Questionnaire)
The importance of therapy goals shows a broad spectrum of patient-defined benefit preferences. The needs and thus potential therapy goals were evaluated on average between 2.3 and 3.9 on a scale of 0 = “not important at all” to 4 = “very important” (Table 2).
The goals “not suffer further aggravation of the rosacea”, “not have reddened skin anymore”, “not have pustules anymore” and “regain control of the disease” were the most important therapeutic goals as measured by the mean values; these were also among the goals which were most frequently answered as being “quite important” or “very important”. The importance was lowest for the goals “have fewer burdens at the work place” and “need less time for daily treatment”.
Significant gender differences were found for the needs “have no more pain or burning sensation on the skin” (women: 3.5 ± 0.9 vs men 2.7 ± 1.4; p < 0.002) and “tolerate heat and cold better” (women: 3.3 ± 0.9 vs men 2.8 ± 1.0; p < 0.002) (Table 2).
Patient Treatment Benefit (Patient Benefit Questionnaire)
The following goals were best achieved by the current treatment in mean values, according to mean benefit ratings: “not to suffer a worsening of rosacea”, “to have no more pain” and “no itching anymore” (Table 3 and Figure 1).
 |
Table 3 Treatment Benefits in Patients with Rosacea Related to Last Active Therapy, Item Wise (n = 475) |
 |
Figure 1 Evaluation of treatment benefit per item in the Patient Benefit Questionnaire (PBQ) for rosacea: distribution of response levels (n = 475). |
The proportion of responses “quite/very much benefit” was highest for the goals “not suffer further aggravation of the rosacea” and “be free of itching”. The achievement of objectives was evaluated on average with values between 1.3 and 2.4.
The following goals showed the lowest mean achievements: “to have fewer out-of-pocket treatment expenses”, “to have fewer dietary restrictions”, “to be able to spend more time in the sunlight”, “need less time for daily treatment”.
Patient Benefit Index for Rosacea
Mean PBI-RO was 1.9 ± 1.2, indicating an overall low level of patient-relevant benefit from rosacea treatment (Table 4). There were no significant differences in the PBI-RO between men and women. Age groups (≤50 vs >50 years) did not differ either.
 |
Table 4 Distribution of Patient Benefit Index (PBI) results Reflecting Patient Benefits from Rosacea Treatment (n = 446; Mean PBI = 1.9 ± 1.2) |
Validation Markers
Internal Consistency
The internal consistency of the PNQ measured by Cronbach’s alpha was 0.94 in PNQ (n = 86).
Correlations with Other Patient Reported Outcomes
The PBI-RO correlated poorly with the current extent of rosacea lesions (r = 0.16, n = 446, p < 0.01) and weakly with the EQ VAS (r = 0.30, n = 434, p < 0.001) and with the DLQI (r = −0.26, n = 437, p < 0.001). The highest correlation was found between PBI-RO and satisfaction with previous treatment (r = −0.59, n = 444 p < 0.001). It was significantly higher than the correlation between PBI-RO and extent of rosacea lesions and between PBI-RO and quality of life, as hypothesized.
Feasibility of the PBI-RO
In an independent sample of n = 50 patients, more than 95% of the patients responded that the questionnaire was easy to fill in and that the content of the questionnaire would fit the benefit concerns of patients with rosacea. The rate of missing values was between 0.8% and 8.0% for single items and 6.1% for the PBI-RO index.
Discussion
The aim of the present study was to develop and validate a rosacea-specific version of the Patient Benefit Index (PBI) for the evaluation of specific patient-relevant needs and benefits from treatment. The procedures and methods followed previous developments of PBI versions for other dermatological indications. The study “RosaReal” was carried out with persons from the address database of the “Deutsche Rosacea Hilfe e. V.”, a German patient organization. Contrarily to surveys in the healthcare environment, such a study situated at home is supposed to create a greater sense of anonymity when answering the questions and to avoid a possible distortion of the data due to the answering of social desirability.
The validation data provide first evidence for a good level of discriminant and construct validity. The feasibility was also very good, reflected by a high level of acceptance and understandability.
The PNQ indicated a broad spectrum of needs from treatment. The distribution underlines that patients with rosacea report individual treatment goals with varying relevance, which should be considered in treatment decision.
Remarkably, in direct questioning, about one-third of patients are more or very dissatisfied with their treatment. In addition, PBI is lower in rosacea patients (1.9 ± 1.2) compared to psoriasis and atopic eczema, suggesting that the treatment benefit of rosacea patients is unsatisfactory. Accordingly, the proportion of patients who did not benefit from therapy (PBI < 1) tends to be larger in the “RosaReal” study with 23.6% than in the “PsoReal” and “AtopicReal” studies. This highlights the need for improved therapies, especially in rosacea patients. In concordance with this, satisfaction with care can be described as mediocre.
These data indicate a large space for improving management of rosacea. Rigorous goal attainment scaling in routine practice could facilitate the identification of patient needs and a more stringent treatment in practice. Given the large number of effective, guideline-compliant therapies, the PBI could optimize the individual choice with highest potential.
A potential limitation of the current study is the conduction in patients recruited from patient advocacy groups. Thus, no direct medical data are available. Nevertheless, the medical background and the outcomes are plausible. Furthermore, patient-reported data were more essential for the purpose of validating such a tool.
In summary, the PBI-RO is a useful instrument with which the patient benefit of rosacea treatment can be assessed reliably and easily. It can be recommended for use in routine care as well as in clinical trials and healthcare research. While it is advantageous for a differentiated care to identify a broad set of patient-relevant benefits as PNQ and PBQ do, a single benefit parameter is needed for outcomes research and quality assurance. This is possible with the PBI as index. The distribution characteristics of the PBI of different samples are directly comparable and can be used in outcome analyses. It makes sense to combine several outcomes methods with a) clinical score, b) quality of life questionnaire and c) patient-defined benefit assessment (PBI). Electronic support for the calculation of indices is recommended.
Conclusion
There is great importance for the assessment of patient needs and for the evaluation of patient-relevant treatment outcomes in rosacea. The new developed rosacea-specific patient benefit questionnaire PBI-RO is a valid and feasible tool to address such patient needs and benefits in rosacea routine management. It may add to more stringent goal orientation in rosacea therapy.
Data Sharing Statement
Data are available upon reasonable request from the corresponding author.
Ethics Approval Statement
This study has been conducted in accordance with the Helsinki Declaration of 1975 by the World Medical Association, as revised by the 59th WMA general assembly 2008 in Seoul. Consultation of the local ethics committee of the Hamburg chamber of physicians confirmed that no formal ethics approval was required in such kind of non-interventional study. This is in line with the German national regulation as released by the German agency for drugs and devices (BfArM) which also exempts non-interventional studies which are not related to drugs or medical devices from the need of positive ethics votes. Informed consent was obtained from all participants.
Acknowledgments
We thank the Scientific Communication Team of the IVDP, in particular Mathilda Meyer and Mario Gehoff, for copy editing.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Plewig G, Klingman AM. Akne und Rosazea. Berlin/Heidelberg: Springer-Verlag; 1994.
2. Ahn CS, Huang WW. Rosacea pathogenesis. Dermatol Clin. 2018;36(2):81–86. doi:10.1016/j.det.2017.11.001
3. Weinkle AP, Doktor V, Emer J. Update on the management of rosacea. Clin Cosmet Investig Dermatol. 2015;8:159–177. doi:10.2147/CCID.S58940
4. Wladis EJ, Adam AP. Treatment of ocular rosacea. Surv Ophthalmol. 2017;63(3):340–346. doi:10.1016/j.survophthal.2017.07.005
5. Augustin M, Herberger K, Hintzen S, Heigel H, Franzke N, Schaefer I. Prevalence of skin lesions and need for treatment in a cohort of 90 880 workers. Br J Dermatol. 2011;165(4):865–873. doi:10.1111/j.1365-2133.2011.10436.x
6. Gether L, Overgaard LK, Egeberg A, Thyssen JP. Incidence and prevalence of rosacea: a systematic review and meta-analysis. Br J Dermatol. 2018;179(2):282–289. doi:10.1111/bjd.16481
7. Jørgensen AR, Egeberg A, Gideonsson R, Weinstock LB, Thyssen EP, Thyssen JP. Rosacea is associated with Helicobacter pylori: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2017;31(12):2010–2015. doi:10.1111/jdv.14352
8. Lacey N, Russell-Hallinan A, Zouboulis CC, Powell FC. Demodex mites modulate sebocyte immune reaction: possible role in the pathogenesis of rosacea. Br J Dermatol. 2018;179(2):420–430. doi:10.1111/bjd.16540
9. Reinholz M, Ruzicka T, Steinhoff M, et al. Pathogenesis and clinical presentation of rosacea as a key for a symptom-oriented therapy. J Dtsch Dermatol Ges. 2016;14(Suppl 6):4–15.
10. Alinia H, Tuchayi SM, Patel NU, et al. Rosacea triggers: alcohol and smoking. Dermatol Clin. 2018;36(2):123–126. doi:10.1016/j.det.2017.11.007
11. McGregor SP, Alinia H, Snyder A, Tuchayi SM, Fleischer A, Feldman SR. A review of the current modalities for the treatment of papulopustular rosacea. Dermatol Clin. 2018;36(2):135–150. doi:10.1016/j.det.2017.11.009
12. Clanner-Engelshofen BM, Bernhard D, Dargatz S, et al. S2k guideline: rosacea. J Dtsch Dermatol Ges. 2022;20(8):1147–1165. doi:10.1111/ddg.14849
13. Bennardo L, Patruno C, Zappia E, et al. Combination of specific vascular lasers and vascular intense pulsed light improves facial telangiectasias and redness. Medicina. 2022;58(5):651. doi:10.3390/medicina58050651
14. Oussedik E, Bourcier M, Tan J. Psychosocial burden and other impacts of rosacea on patients’ quality of life. Dermatol Clin. 2018;36(2):103–113. doi:10.1016/j.det.2017.11.005
15. Hart W, Gieler U. Psychosomatische Dermatologie. Berlin/Heidelberg: Springer-Verlag; 2006.
16. Cardwell LA, Nyckowski T, Uwakwe LN, Feldman SR. Coping mechanisms and resources for patients suffering from rosacea. Dermatol Clin. 2018;36(2):171–174. doi:10.1016/j.det.2017.11.013
17. Beikert FC, Langenbruch AK, Radtke MA, Augustin M. Willingness to pay and quality of life in patients with rosacea. J Eur Acad Dermatol Venereol. 2013;27(6):734–738. doi:10.1111/j.1468-3083.2012.04549.x
18. Heisig M, Reich A. Psychosocial aspects of rosacea with a focus on anxiety and depression. Clin Cosmet Investig Dermatol. 2018;11:103–107. doi:10.2147/CCID.S126850
19. Langenbruch AK, Beket E, Augustin M. Quality of health care of rosacea in Germany from the patient’s perspective. results of the national health care study RosaReal 2009. Dermatology. 2011;223(2):124–130. doi:10.1159/000330555
20. Blome C, Costanzo A, Dauden E, et al. Patient-relevant needs and treatment goals in nail psoriasis. Qual Life Res. 2016;25(5):1179–1188. doi:10.1007/s11136-015-1136-y
21. Radtke MA, Reich K, Spehr C, Augustin M. Treatment goals in psoriasis routine care. Arch Dermatol Res. 2014;307(5):445–449. doi:10.1007/s00403-014-1534-y
22. Mrowietz U, Kragballe K, Reich K, et al. Definition of treatment goals for moderate to severe psoriasis: a European consensus. Arch Dermatol Res. 2011;303(1):1–10. doi:10.1007/s00403-010-1080-1
23. Mrowietz U, Kragballe K, Nast A, Reich K. Strategies for improving the quality of care in psoriasis with the use of treatment goals – a report on an implementation meeting. J Eur Acad Dermatol Venereol. 2011;25(Suppl 3):1–13. doi:10.1111/j.1468-3083.2011.04033.x
24. Blome C, Gosau R, Radtke MA, et al. Patient-relevant treatment goals in psoriasis. Arch Dermatol Res. 2016;308(2):69–78. doi:10.1007/s00403-015-1613-8
25. Radtke MA, Spehr C, Reich K, Rustenbach SJ, Feuerhahn J, Augustin M. Treatment satisfaction in psoriasis: development and use of the PsoSat patient questionnaire in a cross-sectional study. Dermatology. 2016;232(3):334–343. doi:10.1159/000444635
26. Augustin M, Radtke MA, Zschocke I, et al. The patient benefit index: a novel approach in patient-defined outcomes measurement for skin diseases. Arch Dermatol Res. 2009;301(8):561–571. doi:10.1007/s00403-009-0928-8
27. Blome C, Augustin M, Behechtnejad J, Rustenbach SJ. Dimensions of patient needs in dermatology: subscales of the patient benefit index. Arch Dermatol Res. 2011;303(1):11–17. doi:10.1007/s00403-010-1073-0
28. Greiner W, Nieuwenhuizen M, Oppe S, et al. A single European currency for EQ 5–D health states. results from a six-country study. Eur J Health Econ. 2003;4(3):222–231. doi:10.1007/s10198-003-0182-5
29. Hurst NP, Kind P, Ruta D, Hunter M, Stubbings A. Measuring health-related quality of life in rheumatoid arthritis: validity, responsiveness and reliability of EuroQol (EQ-5D). Br J Rheumatol. 1997;36(5):551–559. doi:10.1093/rheumatology/36.5.551
30. Patrick DL, Burke LB, Gwaltney CJ, et al. Content validity establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO good research practices task force report: part 2-assessing respondent understanding. Value Health. 2011;14(8):978–988. doi:10.1016/j.jval.2011.06.013
31. Reeve BB, Wyrwich KW, Wu AW, et al. ISOQOL recommends minimum standards for patient-reported outcome measures used in patient-centered outcomes and comparative effectiveness research. Qual Life Res. 2013;22(8):1889–1905. doi:10.1007/s11136-012-0344-y
32. Augustin M, Blome C, Zschocke I, et al. Benefit evaluation in the therapy of chronic wounds from the patients’ perspective-development and validation of a new method. Wound Repair Regen. 2012;20(1):8–14. doi:10.1111/j.1524-475X.2011.00751.x
33. Augustin M, Schaefer I, Rabini S, Lee-Seifert C, Radtke M, Rustenbach SJ. Assessing the value of supportive skin care. Development and validation of an instrument for evaluating patient-relevant benefit. Dermatology. 2009;218(3):255–259. doi:10.1159/000195174
34. Lienert G, Raatz U. Testaufbau und Testanalyse.
35. Steiger JH. Tests for comparing elements of a correlation matrix. Psychol Bull. 1980;87(2):245–251. doi:10.1037/0033-2909.87.2.245
36. Beikert FC, Langenbruch AK, Radtke MA, Kornek T, Purwins S, Augustin M. Willingness to pay and quality of life in patients with atopic dermatitis. Arch Dermatol Res. 2014;306(3):279–286. doi:10.1007/s00403-013-1402-1
37. Langenbruch AK, Radtke MA, Augustin M. Quality of psoriasis care from the patients’ perspective - results of the national health care study psoReal. Eur J Dermatol. 2012;22(4):518–524. doi:10.1684/ejd.2012.1740
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
