Back to Journals » Drug Design, Development and Therapy » Volume 16
Determination of the Cut-off Value for Imatinib Plasma Levels Linked to Occurrence of Bone Pain in CML Patients
Authors Hamza MS , Shouman SA , Abdelfattah R, Moussa HS, Omran MM
Received 14 March 2022
Accepted for publication 26 May 2022
Published 30 May 2022 Volume 2022:16 Pages 1595—1604
DOI https://doi.org/10.2147/DDDT.S365646
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Tuo Deng
Marwa S Hamza,1 Samia A Shouman,2 Raafat Abdelfattah,3 Heba S Moussa,4 Mervat M Omran2
1Clinical Pharmacy Practice Department, Faculty of Pharmacy, The British University in Egypt, El-Sherouk City, Cairo, Egypt; 2Pharmacology Unit, Cancer Biology Department, National Cancer Institute, Cairo University, Cairo, Egypt; 3Medical Oncology Department, National Cancer Institute, Cairo University, Cairo, Egypt; 4Clinical Pathology Department, National Cancer Institute, Cairo University, Cairo, Egypt
Correspondence: Marwa S Hamza, Clinical Pharmacy Practice Department, Faculty of Pharmacy, The British University in Egypt, El-Sherouk City, Cairo, Egypt, Email [email protected]
Background: Imatinib is used to treat chronic myelogenous leukemia (CML). Variations in imatinib pharmacokinetics have been linked to genetic variations. That has an impact on imatinib response and adverse effects. Therefore, the aim of the study was to study bone pain as an adverse effect that occurs with imatinib and to investigate the risk factors for bone pain.
Methods: The relationship between the peak and trough plasma concentrations of imatinib with bone pain as one of the most frequently occurring adverse effects was examined. Multiple linear regression analysis and binary logistic regression analysis were used to measure the impact of various patients’ characteristics on both peak and trough imatinib concentrations and the risk of the occurrence of imatinib-induced bone pain.
Results: As a side effect of imatinib, approximately 15% of patients with CML who were taking it experienced bone pain. This side effect was linked to the imatinib peak and trough plasma levels. Imatinib trough concentration was also linked to gender and the gene SLCO1B3-334T > G (TT). There were significant associations between peak concentrations and gender as well as patient weight.
Conclusion: Higher peak and trough plasma concentrations of imatinib are linked with the risk of the occurrence of bone pain as a side effect of imatinib. Monitoring plasma concentrations of imatinib is useful to predict the bone pain of imatinib and to support quality of life in patients with CML.
Keywords: imatinib, tyrosine kinase inhibitor, chronic myelogenous leukemia, trough plasma concentration, bone pain
Introduction
Nearly 1–2 of every 100,000 persons in the world are diagnosed with chronic myelogenous leukemia (CML).1–3 Tyrosine-kinase inhibitors (TKIs) are typically used as first-line therapy for CML patients.4 Imatinib mesylate is the gold standard for first-line therapy.3,5–7 The standard dose of imatinib is 400 mg/day for patients with chronic phase CML.8,9 This dose is well tolerated by most patients.10 Prioritizing criteria including toxicity, age, risk score, and patients’ ability to tolerate TKI therapy should be utilized while selecting treatment.11 Despite the fact that TKIs for CML are far superior to traditional chemotherapy, a case report study stated that they have a variety of side effects, such as bone pain and growth attenuation.12 Also, imatinib is linked to toxicity; most of them occur within the first two years after commencing treatment, and some reverse with continuous use of the drug at the same dose. In the vast majority of cases, toxicity is minimal or non-existent, and it is easy to control and even reverse. Fluid retention as a side effect of imatinib can cause weight gain in some people, notably in those with infraorbital edema, but it can also be more widespread. As previously stated, imatinib can cause bone pain, which can be quite severe.13
According to prior research, pain in patients treated with imatinib can occur everywhere in the body, including the shoulders, hips, hands, and feet. At other times, it can also be described as muscle soreness or seem like polymyalgia rheumatica.14 It is possible that imatinib is the cause of the pain syndrome because of the quick disappearance of symptoms after discontinuing imatinib and the rapid return of symptoms after restarting the medication.15 While severe leg and arm pain has been linked to imatinib-induced bone edema in the past, these studies focus on situations where the edema is predominantly in the long shaft bones.15 Other examples of imatinib-induced bone toxicity, such as osteonecrosis in the diaphysis of the tibia, the femoral head, and the jaw, have been documented in the literature.16–18
Single nucleotide polymorphisms (SNPs) in genes are linked to imatinib absorption, distribution, metabolism, and excretion. SNPs are likely to have a role in the reported variations in imatinib pharmacokinetics. The human organic anionic transporter OATP1B3 is involved in imatinib absorption.19 Transporter polymorphisms may alter how much of a medication is able to reach the target cells, which can have an impact on imatinib response and adverse effects. Until now, SNP variations in closely related transporters have not been studied in relation to imatinib-induced bone pain as a side effect. Therefore, this study investigated whether bone pain is an adverse effect that occurs with imatinib in patients with CML. Also, find out what causes bone pain so that best practices can be developed.
Methods
Design
This study was based on data from 102 patients, obtained from our previously published dataset.20 This study was conducted at the Hematological Outpatient Clinic of the National Cancer Institute at Cairo University. Patients were diagnosed with CML, at least 18 years old, and were receiving imatinib therapy for at least 30 days (to reach a steady state). Patients with documented imatinib sensitivities and those with serious medical conditions were excluded from the study.
Drug Administration, Blood Sampling and Assay
As mentioned in our previous work,20 whole blood samples were drawn and placed in tubes that contained EDTA just prior to administering the medication (trough samples) and 2 hours after imatinib administration (peak sample). Injecting 10 µL of plasma into the LC/MS/MS system after it was analyzed using HPLC autosampler bottles.21 Pharmacogenetic analysis requires preparation of DNA for polymorphism determination using the Gentra Puregene Blood Kit (Qiagen Inc., Minneapolis, MN, USA) following the manufacturer’s instructions. The whole-cell pellet was used for the extraction of genomic DNA. Until the analysis, the DNA was kept at a temperature of −80℃. For the genotyping of ABCG2 SNPs 34 G > A and 421C > A and the solute carriers SLCO1B3 SNPs 334T > G, the polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) method was used.22,23
Evaluation of Bone Pain as an Adverse Effect of Imatinib
Bone pain was reported during imatinib therapy. According to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE) version 5.0, bone pain is defined as a disorder characterized by a sensation of marked discomfort in the bones.24 The patients were considered to be suffering from bone pain, either in grade 1, 2 or 3 according to the CTCAE.
Data Collection
All patients’ data was collected, such as age, gender, other diseases other than CML, body weight, height, concomitant medications, serum albumin, total bilirubin, aspartate aminotransferase, alanine aminotransferase, hemoglobin, urea, and serum creatinine. As well as the previous genetic polymorphism data for those patients that was extracted from our previous study.20
Statistical Analysis
The baseline features and events throughout imatinib therapy were described using descriptive statistics. Statistical information was summarized using percentages and numbers to represent the qualitative data. Proportion independence was evaluated using a chi-squared test or a Fisher exact test. A Student’s t-test and an ANOVA test were done between both trough as well as peak imatinib plasma concentration and different categorical variables. A Spearman’s rank correlation test was used to confirm that they were employed to compare the average results of two different groups. A Spearman’s rank correlation test was carried out for the confirmation of the association between peak and trough plasma concentration, patient characteristics, genetic polymorphism, and laboratory data. Multiple linear regression analysis was used to determine the role of various genetic polymorphisms and other factors in the fluctuation of imatinib plasma concentrations.
Binary logistic regression analysis was used to characterize the effects of variables on bone pain in order to compare the incidence of bone pain as a side effect of imatinib. Varieties of genotypes had different chances of adverse responses, as shown by the odds ratio (OR) and its 95% confidence interval (95% CI). In addition, ROC curves were used to find the imatinib trough and peak plasma concentration cut-off values for the incidence of bone pain in patients. The cut-off value was considered to be the maximum of the sum of sensitivity and specificity. The Statistical Package for Social Science (SPSS) (version 23.0; SPSS, Chicago, USA) was used to conduct the statistical analysis. p values less than 0.05 were considered statistically significant differences.
Results
Demographic and Clinical Characteristics
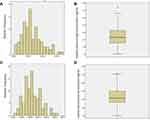
There were 102 CML patients in the present study. Forty-seven of them were men, and 55 of them were women, with a mean age of 40.6±11 years and normal liver and kidney laboratory results. The imatinib dose was 400 mg/day. It was found that plasma imatinib levels peaked at 2884 ± 1063 ng/mL while the trough plasma level was 1416 ± 701 ng/mL (Figure 1). Fifteen patients (14.7%) were suffering from bone pain. This cohort’s demographical, clinical, and pharmacokinetic features are shown in Table 1 and Figure 1.
 |
Table 1 Demographic and Clinical Characteristics of CML Patients After Treatment with Imatinib According to Bone Pain |
Association Between Imatinib Peak and Trough Plasma Concentration and Certain Patients’ Features
A Student’s t-test test was done to examine the relationship between both trough and peak imatinib plasma concentration and gender. Interestingly, it was found that males had lower imatinib plasma levels where the mean values of the trough and peak levels were 1168±613, 2529± 959 ng/mL for males vs 1628±707, 3187±1062 ng/mL for females, respectively (P< 0.001).
Then an ANOVA test was done, and it was found that there was no significant association between both trough and peak imatinib plasma concentration and different gene categories. The Spearman’s rank correlation test was used to confirm whether patient characteristics or laboratory data were correlating with imatinib trough and peak plasma concentration. Hemoglobin level (r = −0.28, r= −0.29, P<0.05) and the alpha-1-acid glycoprotein (r = −0.23, r = 0.2, P<0.05) were the only factors found to be significantly but weekly correlated with the trough and peak imatinib plasma concentrations, respectively. Imatinib trough plasma concentration was not correlated with several laboratory data, such as height, body weight, total protein, total bilirubin, aspartate aminotransferase, alanine aminotransferase and serum creatinine.
Multiple linear regression analysis was done where the imatinib trough concentration was used as the dependent variable and age, sex, laboratory data, as well as gene polymorphism as prognostic variables (Table 2). There were significant associations between trough concentrations with the gender, and SLCO1B3-334T>G (TT). For females, the trough concentration increased by 445ng/mL (95% confidence interval [CI], 185 to 705). The trough plasma concentration of imatinib decreased by 520 ng/mL in patients with SLCO1B3-334T>G homozygous wild type TT allele rather than in patients with the variant type GG (95% confidence interval [CI]: −985.8 to −56.2) (Table 2).
 |
Table 2 Associations Between Imatinib Trough Plasma Level and Patients’ Characteristic |
Another multiple linear regression analysis was done where the imatinib peak concentration was used as the dependent variable while age, sex, laboratory data, and gene polymorphism were used as prognostic variables (Table 3). There were significant associations between peak concentrations and the gender, as well as patients’ weight. For females, the peak concentration increased by 826 ng/mL (95% confidence interval [CI], 420 to 1232). The peak plasma concentration of imatinib increased by 11.8 ng/mL for every 1 kg increase in the patients’ weight (95% confidence interval [CI], 0.126 to 23.4) (Table 3).
 |
Table 3 Associations Between Imatinib Peak Plasma Level and Patients’ Characteristic |
Association Between Bone Pain and Trough and Peak Plasma Concentration of Imatinib, Patient Characteristics, Laboratory Data
The mean of the peak and trough plasma concentrations of imatinib in patients who did not suffer from bone pain were 2620839 and 1239571 respectively. Whereas the mean of peak and trough plasma concentrations of imatinib in patients who suffered from bone pain were 4414±942, 2440±479, respectively. (Figure 2A and B).
The Spearman’s rank correlation test was used to confirm the patient characteristics, laboratory and genetic polymorphism, as well as the peak and trough plasma concentrations of imatinib data that may be correlated with the occurrences of bone pain. Only the trough plasma concentration of imatinib (r = 0.547, p 0.001), the peak plasma concentration of imatinib (r = 0.517, p 0.001), the weight (r = 0.226, p 0.05), and the plasma alpha-1-acid glycoprotein (r = 0.242, p 0.05) were found to be significantly and positively correlated with the occurrences of bone pain. Other laboratory data, such as height, body weight, total protein, total bilirubin, aspartate aminotransferase, alanine aminotransferase, and serum creatinine, did not show a connection between the presence of bone pain and these other lab results, which did not show any connection.
Binary logistic regression analysis was done where the occurrences of bone pain were used as the dependent variable and age, sex, laboratory data, and gene polymorphism as well as the imatinib peak and trough concentration as prognostic variables. There was a significant association between the occurrence of bone pain and the imatinib trough and peak plasma levels. The risk of developing bone pain increases by ~ 1 time for every 1 ng/mL increase in imatinib trough concentration (95% CI, 1.001 to 1.004). Also, the risk of bone pain occurrence increases by ~ 1 time for every 1 ng/mL increase in the imatinib peak concentration (95% confidence interval [CI], 1.001 to 1.003) (Table 4).
 |
Table 4 Logistic Regression Analysis to Identify Risk Factors for Bone Pain in CML Patients Treated with Imatinib |
Receiver Operating Characteristic (ROC) Curves
The cut-off values for imatinib peak and trough plasma concentrations were 3720 and 1775 ng/mL. The area under the ROC curve (AUC) was 0.92 and 0.94 for the peak and trough curves, respectively. Table 3 summarizes the sensitivity and specificity of this cut-off at 0.93 and 0.15, respectively, for the trough concentration and 0.87 and 0.11 for the peak concentration (Table 5). The ROC curve is shown in Figure 2C and D.
 |
Table 5 The Parameters of the Receiver Operating Characteristic (ROC) Curve for the Cut-off for Trough Plasma Imatinib Concentration in Bone Pain |
Discussion
Imatinib has been linked to toxicity, but the majority of side effects are seen during the first two years of commencing medication, and some go away with continuous use of the same dose.13 Some individuals may suffer from skin reactions,25 interstitial lung disease26 and edema.27 Bone discomfort is another devastating side effect.28 The connection between plasma levels and adverse drug reactions (ADRs) in patients with CML using imatinib has only been studied in small samples till now. According to our research, which included 102 patients with advanced CML, bone pain was the most prevalent side effect after receiving imatinib therapy. Most experts agree that detecting imatinib plasma concentration is critical for drug guidance and dose modification,29 as imatinib plasma concentration plays a role in the occurrence of imatinib side effects. Therefore, we hypothesized that bone pain is significantly associated with imatinib plasma concentrations.
In this study, the mean imatinib trough plasma levels were 1199± 506 ng/mL. This value falls within the imatinib trough plasma concentration range of 181 to 2947 ng/mL, with a mean of 1058 ng/mL for the 400 mg/day dosage.30 Also, it lies within the range of 363–2900 ng/mL with a mean of 1325.61 in different studies.31 All these concentrations are greater than 1002 ng/mL, which means there is a higher chance of a major molecular response (MMR).32
Multiple linear regression analyses were carried out to verify the link between imatinib trough and peak plasma levels with several patient-specific variables. Gender and weight had strong relationships with imatinib plasma concentrations. Females had imatinib peak and trough plasma levels higher than males. Previous research showed that females had greater imatinib trough plasma levels, which supports this assertion.33–35 This may be explained by the fact that females have a higher percentage of body fat than males36 and low-density lipoproteins are inhibited by imatinib, which inhibits glycosaminoglycan production on vascular proteoglycans and reduces their binding to the platelet-derived growth factor receptor both in vitro and in vivo.37 Besides the fact that fat metabolism is related to the level of low-density lipoproteins.38 Another study reported that the effective imatinib dose is associated with age as well as body surface area, and a reduced dose of 300 mg/day of imatinib may be sufficient for the treatment of CML patients with smaller body sizes, particularly when intolerability arises.39 Therefore, in order to avoid inadequate effectiveness at decreased dosages in men, the effective dose of imatinib must be raised.39 Also, in order to minimize side effects at high dosages of imatinib, the effective dose for females must be reduced.
In addition, interindividual variability in imatinib pharmacokinetics is still debated due to genetic variations and race differences. Our earlier research showed that a high imatinib trough is linked with a strong response to the drug, and that the genotypes ABCG2.34 G > A and SLCO1B3.334 T > G were associated with a good imatinib response in Egyptian CML patients.20 In this study, for individuals who had the wild homogenous allele TT SLCO1B3.334 T > G, we discovered that the imatinib trough concentration was 520 ng/mL higher in them than in those with the heterozygous GA allele and the variant type. This supports our previous finding that patients with the wild variant of SLCO1B3.334 T > G have favorable response to imatinib.20 According to earlier research on the immunosuppressant medication Mycophenolic acid, SLCO1B3 334T > G was shown to be strongly linked to adverse outcomes, although heterozygous carriers of SLCO1B3 334T > G had a lower chance of experiencing gastrointestinal side effects than wild-type people.40
As a result, patients’ dosages should be tailored to their imatinib trough concentration. However, the present study did not examine the relationship between an effective dose of imatinib and other drug-metabolizing enzymes and drug transporter genotypes. In previous studies, Imatinib pharmacokinetics have been shown to be linked to ABC transporters, the human organic cation transporter, and cytochrome P450 isoenzymes.19,41–43 There is still a lot of debate about how important genetic variation and body surface area variability are when it comes to the effective dose and pharmacokinetics of imatinib. More research is needed to figure out how important they are.39
In the last decade, researchers have argued that an appropriate plasma concentration of imatinib can be linked to a satisfactory clinical response. Following these results, the determination of the trough plasma imatinib concentration is useful for patients with a suboptimal response, treatment failure,44 unpredicted severe adverse reactions, supratherapeutic levels45 and drug-drug interactions with imatinib.46 Despite the fact that plasma concentration measurements may be helpful in these difficult situations, decisions about whether to interrupt treatment, reduce the dose, or change the therapy should always be made based on the overall clinical situation until more data is available.46
The relationship between imatinib plasma concentration and therapeutic effects has been extensively studied in clinical trials. However, the relationship between imatinib plasma concentration and toxicity in CML has received far less attention. In this study, it was shown that imatinib trough and peak concentration, as well as certain patient characteristics, were associated with an increased chance of developing bone pain as a side effect. As we mentioned before, the correlation between the occurrence of bone pain and the level of alpha-1 glycoprotein was significantly positive but week (r = 0.242, p< 0.05). Since imatinib is predominantly bound to plasma alpha-1-acid glycoprotein, this might dramatically affect the distribution and elimination of imatinib47 leading to bone pain.
A binary logistic regression analysis was conducted to examine the role of different patients’ characteristics that may play a role in the development of bone pain. Imatinib trough and peak plasma levels were shown to be significantly associated with the occurrence of bone pain. For every 1 ng/mL rise in the imatinib either trough or peak plasma level of imatinib, the risk of bone pain rose by 1 time.
Although in this study there was no association between SLCO1B3.334 T > G and the occurrence of bone pain, we confirmed in our previous work that patients with the heterogeneous allele of SLCO1B3.334 T > G (TG) were more likely to respond favorably in earlier studies.20 Therefore, SLCO1B3 may serve as a diagnostic, therapeutic, and prognostic biomarker.48
After carrying out the ROC curve analysis, we found that the cut-off points for the imatinib trough and peak plasma levels are 1775 and 3720 ng/mL, respectively. Above that, the risk of bone pain as a side effect of imatinib increases. According to prior research, patients with CML who receive imatinib at a trough concentration of more than 1002 ng/mL should have their blood tested often.30 Another study reported that the trough concentration of imatinib that can contribute to the incidence of CML-wide adverse effects is 926 ng/mL.49 This information lets us formulate the drug regimen in a way that ensures a good response in terms of avoiding or relieving bone pain, as well as continuing therapy as needed.
Conclusion
Imatinib trough concentration is linked to gender and the intake transporter SLCO1B3.334 T > G. Imatinib peak concentration is linked to the patient’s gender and weight. Also, patients with CML using imatinib may experience bone pain as a side effect, which is linked to the imatinib trough and peak plasma levels. Imatinib plasma concentration monitoring may be useful in predicting the likelihood of bone discomfort.
Ethical Approval
The Institutional Review Board (IRB) of the National Cancer Institute of Cairo University, Egypt, reviewed and approved the study with acceptance number IRB00004025. The study was carried out in accordance with the ethical principles outlined in the Helsinki Declaration of the World Medical Congress and its amendments.
Informed Consent
All participants included in this study signed informed consent.
Disclosure
All of the authors declare no conflicts of interest in relation to this work and that there is no conflict of interest associated with this manuscript.
References
1. Wan Z, Chen X, Gao X, et al. Chronic myeloid leukemia-derived exosomes attenuate adipogenesis of adipose derived mesenchymal stem cells via transporting miR-92a-3p. J Cell Physiol. 2019;234(11):21274–21283. doi:10.1002/jcp.28732
2. McMullan RR, McConville C, McMullin MF. Response to therapy, treatment intolerance and Tyrosine Kinase inhibitor cessation eligibility in a real-world cohort of chronic myeloid leukaemia patients. Ulster Med J. 2019;88(2):105–110.
3. Meenakshi Sundaram DN, Jiang X, Brandwein JM, Valencia-Serna J, Remant KC, Uludağ H. Current outlook on drug resistance in chronic myeloid leukemia (CML) and potential therapeutic options. Drug Discov Today. 2019;24(7):1355–1369. doi:10.1016/j.drudis.2019.05.007
4. Efficace F, Stagno F, Iurlo A, Breccia M, Cottone F, Bonifacio M. Health-related quality of life of newly diagnosed chronic myeloid leukemia patients treated with first-line dasatinib versus imatinib therapy. Leukemia. 2020;34(2):488–498. doi:10.1038/s41375-019-0563-0
5. Jabbour EJ, Mendiola MF, Lingohr-Smith M, Lin J, Makenbaeva D. Economic modeling to evaluate the impact of chronic myeloid leukemia therapy management on the oncology care model in the US. J Med Econ. 2019;22(11):1113–1118. doi:10.1080/13696998.2019.1618316
6. Soysal T, Eskazan AE, Serin I, et al. The outcomes of chronic myeloid leukemia patients with molecular warning responses during imatinib treatment according to the European LeukemiaNet 2013 recommendations. Clin Lymphoma Myeloma Leuk. 2019;19(7):e377–e384. doi:10.1016/j.clml.2019.03.028
7. Molica M, Colafigli G, Scalzulli E, et al. Ten-year outcome of chronic-phase chronic myeloid leukemia patients treated with imatinib in real life. Ann Hematol. 2019;98(8):1891–1904. doi:10.1007/s00277-019-03706-x
8. O’Brien SG, Guilhot F, Larson RA, et al. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348(11):994–1004. doi:10.1056/NEJMoa022457
9. Druker BJ, Guilhot F, O’Brien SG, et al. Five-year follow-up of patients receiving imatinib for chronic myeloid leukemia. N Engl J Med. 2006;355(23):2408–2417. doi:10.1056/NEJMoa062867
10. Peng B, Hayes M, Resta D, et al. Pharmacokinetics and pharmacodynamics of imatinib in a Phase I trial with chronic myeloid leukemia patients. J Clin Oncol. 2004;22(5):935–942. doi:10.1200/jco.2004.03.050
11. Radich JP, Deininger M, Abboud CN, et al. chronic myeloid leukemia, version 1.2019, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. 2018;16(9):1108–1135. doi:10.6004/jnccn.2018.0071
12. Lavoie DCT, Robinson M-E, Johnston D, et al. The bone phenotype and pain response to pamidronate in Tyrosine Kinase inhibitor-treated chronic myelogenous leukemia. J Endocr Soc. 2019;3(5):857–864. doi:10.1210/js.2018-00268
13. Mughal TI, Schrieber A. Principal long-term adverse effects of imatinib in patients with chronic myeloid leukemia in chronic phase. Biologics. 2010;4:315–323. doi:10.2147/BTT.S5775
14. Richter J, Söderlund S, Lübking A, et al. Musculoskeletal pain in patients with chronic myeloid leukemia after discontinuation of imatinib: a Tyrosine Kinase inhibitor withdrawal syndrome? J Clin Oncol. 2014;32(25):2821–2823. doi:10.1200/jco.2014.55.6910
15. Dubost -J-J, Ledoux-Eberst J, Vaure-Chiffre J, Pezet D, Soubrier M. Imatinib-induced bone oedema mimicking type 1 complex regional pain syndrome. Rheumatology. 2020;59(6):1444–1446. doi:10.1093/rheumatology/kez503
16. Yeh CN, Fu CJ, Yen TC, Chiang KC, Jan YY, Chen MF. Osteonecrosis of the tibia associated with imatinib in metastatic GI stromal tumor. J Clin Oncol. 2013;31(16):e248–50. doi:10.1200/jco.2012.45.1294
17. Nataraj V, Kandasamy D, Bakhshi S. Imatinib-induced avascular necrosis of femur in childhood chronic myeloid leukemia. Pediatr Hematol Oncol. 2014;31(3):268–270. doi:10.3109/08880018.2013.862588
18. Viviano M, Rossi M, Cocca S. A rare case of osteonecrosis of the jaw related to imatinib. Journal of the Korean Association of Oral and Maxillofacial Surgeons. 2017;43(2):120–124. doi:10.5125/jkaoms.2017.43.2.120
19. Hu S, Franke RM, Filipski KK, et al. Interaction of imatinib with human organic ion carriers. Clin Cancer Res. 2008;14(10):3141–3148. doi:10.1158/1078-0432.ccr-07-4913
20. Omran MM, Abdelfattah R, Moussa HS, Alieldin N, Shouman SA. Association of the trough, peak/trough ratio of imatinib, Pyridine-N-Oxide imatinib and ABCG2 SNPs 34 G>A and SLCO1B3 334 T>G with imatinib response in Egyptian chronic myeloid leukemia patients. Front Oncol. 2020;10:1348. doi:10.3389/fonc.2020.01348
21. Titier K, Picard S, Ducint D, et al. Quantification of imatinib in human plasma by high-performance liquid chromatography-tandem mass spectrometry. Ther Drug Monit. 2005;27(5):634–640. doi:10.1097/01.ftd.0000175973.71140.91
22. Anthony A, Ankathil R, Ai-Sim G, Fadilah SAW, Baba AA. Influence of ABCB1 C3435T and ABCG2 C421A gene polymorphisms in response to imatinib mesylate in chronic myeloid leukemia patients. Int J Environ Sci Dev. 2012;274–278. doi:10.7763/IJESD.2012.V3.230
23. Bedewy AM, El-Maghraby SM. Do SLCO1B3 (T334G) and CYP3A5*3 polymorphisms affect response in Egyptian chronic myeloid leukemia patients receiving imatinib therapy? Hematology. 2013;18(4):211–216. doi:10.1179/1607845412y.0000000067
24. US Department of Health and HumanServices. Common Terminology Criteria for Adverse Events (CTCAE) version5. National Institutes of Health, National Cancer Institute; 2017.
25. Rule SA, O’Brien SG, Crossman LC. Managing cutaneous reactions to imatinib therapy. Blood. 2002;100(9):3434–3435. doi:10.1182/blood-2002-08-2431
26. Ohnishi K, Sakai F, Kudoh S, Ohno R. Twenty-seven cases of drug-induced interstitial lung disease associated with imatinib mesylate. Leukemia. 2006;20(6):1162–1164. doi:10.1038/sj.leu.2404207
27. Ebnöether M, Stentoft J, Ford J, Buhl L, Gratwohl A. Cerebral oedema as a possible complication of treatment with imatinib. Lancet. 2002;359(9319):1751–1752. doi:10.1016/s0140-6736(02
28. Berman E, Nicolaides M, Maki RG, et al. Altered bone and mineral metabolism in patients receiving imatinib mesylate. N Engl J Med. 2006;354(19):2006–2013. doi:10.1056/NEJMoa051140
29. Diekstra MH, Liu X, Swen JJ, et al. Association of single nucleotide polymorphisms in IL8 and IL13 with sunitinib-induced toxicity in patients with metastatic renal cell carcinoma. Eur J Clin Pharmacol. 2015;71(12):1477–1484. doi:10.1007/s00228-015-1935-7
30. Picard S, Titier K, Etienne G, et al. Trough imatinib plasma levels are associated with both cytogenetic and molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood. 2007;109(8):3496–3499. doi:10.1182/blood-2006-07-036012
31. Li Q-B, Chen C, Chen Z-C, et al. Imatinib plasma trough concentration and its correlation with characteristics and response in Chinese CML patients. Acta Pharmacol Sin. 2010;31(8):999–1004. doi:10.1038/aps.2010.79
32. Martins DH, Wagner SC, Dos Santos TV, et al. Monitoring imatinib plasma concentrations in chronic myeloid leukemia. Rev Bras Hematol Hemoter. 2011;33(4):302–306. doi:10.5581/1516-8484.20110081
33. Koo DH, Ryu MH, Ryoo BY, et al. Association of ABCG2 polymorphism with clinical efficacy of imatinib in patients with gastrointestinal stromal tumor. Cancer Chemother Pharmacol. 2015;75(1):173–182. doi:10.1007/s00280-014-2630-6
34. Belsey SL, Ireland R, Lang K, et al. Women administered standard dose imatinib for chronic myeloid leukemia have higher dose-adjusted plasma imatinib and norimatinib concentrations than men. Ther Drug Monit. 2017;39(5):499–504. doi:10.1097/ftd.0000000000000440
35. Wu X, Li J, Zhou Y, et al. Relative factors analysis of imatinib trough concentration in Chinese patients with gastrointestinal stromal tumor. Chemotherapy. 2018;63(6):301–307. doi:10.1159/000493195
36. Chen Y, Dong X, Wang Q, et al. Factors influencing the steady-state plasma concentration of imatinib mesylate in patients with gastrointestinal stromal tumors and chronic myeloid leukemia. Front Pharmacol. 2020;11:569843. doi:10.3389/fphar.2020.569843
37. Ballinger ML, Osman N, Hashimura K, et al. Imatinib inhibits vascular smooth muscle proteoglycan synthesis and reduces LDL binding in vitro and aortic lipid deposition in vivo. J Cell Mol Med. 2010;14(6b):1408–1418. doi:10.1111/j.1582-4934.2009.00902.x
38. Dikariyanto V, Smith L, Francis L, et al. Snacking on whole almonds for 6 weeks improves endothelial function and lowers LDL cholesterol but does not affect liver fat and other cardiometabolic risk factors in healthy adults: the ATTIS study, a randomized controlled trial. Am J Clin Nutr. 2020;111(6):1178–1189. doi:10.1093/ajcn/nqaa100
39. Kawaguchi T, Hamada A, Hirayama C, et al. Relationship between an effective dose of imatinib, body surface area, and trough drug levels in patients with chronic myeloid leukemia. Int J Hematol. 2009;89(5):642–648. doi:10.1007/s12185-009-0315-4
40. Na Takuathung M, Sakuludomkan W, Koonrungsesomboon N. The impact of genetic polymorphisms on the pharmacokinetics and pharmacodynamics of mycophenolic acid: systematic review and meta-analysis. Clinical Pharmacokinetics. 2021;60:1291–1302. doi:10.1007/s40262-021-01037-7
41. Dulucq S, Bouchet S, Turcq B, et al. Multidrug resistance gene (MDR1) polymorphisms are associated with major molecular responses to standard-dose imatinib in chronic myeloid leukemia. Blood. 2008;112(5):2024–2027. doi:10.1182/blood-2008-03-147744
42. Gurney H, Wong M, Balleine RL, et al. Imatinib disposition and ABCB1 (MDR1, P-Glycoprotein) Genotype. Clin Pharmacol Ther. 2007;82(1):33–40. doi:10.1038/sj.clpt.6100201
43. Gardner ER, Burger H, van Schaik RH, et al. Association of enzyme and transporter genotypes with the pharmacokinetics of imatinib. Clin Pharmacol Ther. 2006;80(2):192–201. doi:10.1016/j.clpt.2006.05.003
44. Kantarjian HM, Larson RA, Guilhot F, et al. Efficacy of imatinib dose escalation in patients with chronic myeloid leukemia in chronic phase. Cancer. 2009;115(3):551–560. doi:10.1002/cncr.24066
45. Blasdel C, Egorin MJ, Lagattuta TF, Druker BJ, Deininger MW. Therapeutic drug monitoring in CML patients on imatinib. Blood. 2007;110(5):1699–1701. doi:10.1182/blood-2007-03-079871
46. Arora B, Gota V, Menon H, et al. Therapeutic drug monitoring for imatinib: current status and Indian experience. Indian J Med Paediatr Oncol. 2013;34(3):224–228. doi:10.4103/0971-5851.123752
47. Gambacorti-Passerini C, Zucchetti M, Russo D, et al. Alpha1 acid glycoprotein binds to imatinib (STI571) and substantially alters its pharmacokinetics in chronic myeloid leukemia patients. Clin Cancer Res. 2003;9(2):625–632.
48. Tang T, Wang G, Liu S, et al. Highly expressed SLCO1B3 inhibits the occurrence and development of breast cancer and can be used as a clinical indicator of prognosis. Sci Rep. 2021;11(1):631. doi:10.1038/s41598-020-80152-0
49. Gotta V, Bouchet S, Widmer N, et al. Large-scale imatinib dose-concentration-effect study in CML patients under routine care conditions. Leuk Res. 2014;38(7):764–772. doi:10.1016/j.leukres.2014.03.023
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.