Back to Journals » Clinical Ophthalmology » Volume 18
Determination of Refractive Error Using Direct Ophthalmoscopy in Children
Authors Vijendran S, Kamath YS , Alok Y, Kuzhuppilly NIR
Received 10 December 2023
Accepted for publication 11 March 2024
Published 2 April 2024 Volume 2024:18 Pages 989—996
DOI https://doi.org/10.2147/OPTH.S453207
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Sruthi Vijendran,1,* Yogish S Kamath,1,* Yash Alok,2 Neetha IR Kuzhuppilly1
1Department of Ophthalmology, Kasturba Medical College Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India; 2Department of Community Medicine, Kasturba Medical College Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, India
*These authors contributed equally to this work
Correspondence: Neetha IR Kuzhuppilly, Department of Ophthalmology, Kasturba Medical College Manipal, Manipal Academy of Higher Education, Manipal, Karnataka, 576104, India, Tel +91 98861 61979, Fax +91-820-2571934, Email [email protected]
Purpose: Refractive error is a major cause of visual impairment in children and its early detection can prevent ocular morbidity such as amblyopia and strabismus. Brückner test is a comprehensive test which can be easily administered in children using a direct ophthalmoscope. We aimed to determine refractive error in children by analysis of the red reflex using modified Brückner test.
Patients and Methods: This prospective observational study was conducted on 683 undilated eyes of 683 children aged four to 10 years. They were evaluated with a direct ophthalmoscope from one meter in a dimly lit room. The characteristics of the red reflex and crescent obtained were compared with photoscreener refraction value and analyzed.
Results: The presence of superior crescent was associated with hypermetropia (Chi square 37.11, p < 0.001, kappa = 0.15) and inferior crescent with myopia (Chi square 157.29, p < 0.001, kappa = 0.477). Superior crescent was 98.4% sensitive in detecting hypermetropia. Hypermetropia greater than +1.5D, was associated with larger superior crescent crossing horizontal midline of pupil (Chi square = 5.29, p = 0.021).
Conclusion: The modified Brückner test is useful in detection and quantification of refractive error in children. It is easy, simple, quick and can be employed in the community as a screening test to detect potentially amblyogenic refractive errors.
Keywords: visual impairment, pediatric refraction, hypermetropia, myopia, Brückner test, refractive error
Introduction
Visual impairment and blindness are debilitating conditions which affect the formative development of children, the majority of which are preventable if detected early. In Indian children, refractive errors like hypermetropia, myopia or astigmatism form some of the major components of visual impairment, the current prevalence of which is estimated to be eight among every 100 children.1–5 Refractive errors associated with anisometropia or isoametropia are known causes for amblyopia. Hypermetropic anisometropia of even one diopter (D) can be amblyogenic in children aged 3.5 years and above,6 as can higher isoametropia, especially hypermetropic isoametropia.7
Screening for refractive errors in children is essential if we aim to reduce it as a cause of visual impairment. Automated refractometers and photoscreeners are instruments available for screening but are not easily accessible or affordable to all.8,9 Retinoscopy which is another means of objective assessment of refractive error also takes time, cooperation, and training of personnel.5 Brückner transillumination test, in its original methodology or with modifications, is a simple test for strabismus and amblyopia assessment.10–14 It is available for screening refractive errors in children, but it is seen that many studies on Brückner test have knowledge gaps regarding its quantification.14–17
An easy and quick screening for refractive errors in young children is the need of the hour. Modifying the Brückner test, using a direct ophthalmoscope to elicit a red reflex in the eyes of children and then by evaluating the reflex, we attempted to aid the screening efforts.
The objective of our study was to determine the refractive error in children [from four to ten years] by analysis of the red reflex using distant direct ophthalmoscopy. We hypothesize that the modified Brückner test can help us screen for the type of refractive error as well as quantify it.
Materials and Methods
This prospective observational study was conducted from June 2021 to September 2022. It was conducted at the outpatient clinic as well as outreach camps held by the department of ophthalmology at a tertiary care hospital in South India. Children aged between four and ten years of both genders were recruited. Children were excluded from the study if consent for the test could not be obtained. Data from eyes with astigmatism greater than three diopters were excluded.
Informed consent was obtained from the parent or legal guardian. The tenets of declaration of Helsinki were adhered to. Ethics Committee approval was taken prior to commencement to study from Institutional ethics committee (IEC 650–2020, dated 12/02/2021). Clinical Trials Registry- India CTRI registration was done, with registration number: CTRI/2021/05/033615, registered on 13/05/2021. Confidentiality of all participants was ensured by usage of indirect identifiers.
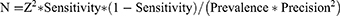
A sample size of 683 eyes was determined taking into consideration 9% prevalence, sensitivity 80%, 95% confidence interval and precision of 10%. The sample size formula is as follows:
Sampling was done using stratified random sampling. 683 children were evaluated and either right or left eye per child was selected randomly using randomization tool of Excel.
Data Collection Tool and Technique
The children were evaluated in a dimly lit room with no bright sunlight or other light sources by a trained ophthalmology resident. The undilated eyes were examined with the help of a direct ophthalmoscope (Welch-Allyn 3.57 Model) from a distance of one meter, with the examiner at the eye level of the children. Children were instructed to fixate a distant target. Using the direct ophthalmoscope, the red reflex from the children’s eyes were examined, the lens dial of the ophthalmoscope was turned till the light reflex in the pupillary area was focused well.
The intensity and brightness of the red reflex was noted and classified as normal or abnormal, the abnormal glow was further classified as dull or bright. If a bright yellowish orange glow was seen only partly covering the pupil, it was referred to as a crescent.16 Details of the crescent were noted as either, “No crescent”, “Superior crescent”, or “Inferior crescent”. Quantification of crescent was done by assessing whether the crescent crossed the horizontal midline from the upper or lower half of the pupil.
The child was then evaluated with an autorefractor/photoscreener- Plusoptix A09 Binocular autorefractor (Plusoptix GmbH, Nuremberg, Germany) to determine the refractive error objectively,18 by an independent optometrist masked to the findings of red glow or crescent. Spherical equivalent of refractive error between +0.5D and −0.5D was considered as emmetropia, greater than +0.5D as hypermetropia and greater than −0.5D as myopia. Vision testing using Snellen’s chart and Lea symbol chart (for children four years of age) was done.
Observations attained through the modification of Brückner test with location of crescent and whether it crossed the midline were compared with photoscreener spherical equivalent.
Statistical Analysis
Statistical analysis was done using SPSS 26.0 (IBM Corporation, Chicago, Illinois, USA). Descriptive statistics were calculated first. Categorical data was represented as frequencies and percentages and continuous data was represented using median and interquartile range for non-parametric and mean and standard deviation for parametric data. For association between categorical variables, Chi square test was used. Agreement statistics were calculated using kappa statistic. Sensitivity, specificity, positive and negative predictive values of the crescent to detect refractive error was calculated. A p value of <0.05 was taken as significant.
Results
Six hundred and eighty-three children participated in this study out of which 364 were girls and 319 were boys; 683 eyes of 683 children were selected for analysis. Mean age of the participants was 7.91 ±1.8 years. Table 1 gives the uncorrected visual acuities in the eyes examined.
 |
Table 1 Ocular Characteristics of the Participants |
During modified Brückner testing, three eyes had an abnormal dull glow and rest had normal glow. The majority had a superior crescent, and three eyes did not show a crescent formation within the pupil. Table 2 shows the spherical equivalent of refractive error detected in the eyes and their relation to the position of crescent. Five hundred and seven (74%) of the eyes had hypermetropia (greater than +0.5D), 33 eyes (4.8%) had myopia (greater than −0.5 D) and 143 (20.9%) were emmetropic.
 |
Table 2 Relationship of Spherical Equivalent of Refractive Error with the Position of Crescent in Modified Brückner Test |
It was observed that presence of superior crescent was significantly associated with presence of a hypermetropic spherical equivalent more than +0.5 D (Odds ratio: 8.911[Confidence interval: 3.889–20.417], Chi square 37.11, df = 1, p < 0.001, kappa = 0.15, Cronbach’s alpha: 0.304), and inferior crescent was significantly associated with presence of spherical equivalent greater than - 0.5 D ie myopia (Odds ratio: 44.306[Confidence interval: 18.158–108.105], Chi square 157.29, df = 1, p < 0.001, kappa = 0.477, Cronbach’s alpha: 0.647). Additionally, hypermetropia greater than +1.5D, was associated with larger superior crescent which crossed the horizontal midline of the pupil (Odds ratio: 1.686[Confidence interval: 1.074–2.648], Chi square= 5.234, df=1, p=0.021) (Table 3).
 |
Table 3 Relationship of the Refractive Error with the Crescent Crossing the Midline of the Pupil |
There were three eyes with dull glow and all of them had myopia greater than −0.5D. It was observed that the presence of dull glow was significantly associated with myopia greater than −0.5 D (Odds ratio: 22.667[Confidence interval: 15.975–32.161], Chi square 59.35, df = 1, p < 0.001).
The presence of a superior crescent is 98.4% sensitive in detecting hypermetropia but has low specificity of 12.5%. The reliability parameters of inferior crescent and absence of crescent are given in Table 4.
 |
Table 4 Reliability Parameters of Location of Crescent for Detecting Respective Refractive Errors |
Discussion
In this study, we assessed the utility of a modification of the Brückner test using a direct ophthalmoscope in detecting the presence and type of refractive error. We were able to determine that the presence and location of the crescent within the red glow inside the pupil can be a good indicator in such cases. Additionally, it may help in quantifying the hyperopic error.
In our study, direct ophthalmoscope was used for conducting the modified Brückner test similar to some studies in the past,10,19 whereas others have used retinoscopes or indirect ophthalmoscopes.14,20 Any coaxial light source which is easily portable would be suitable for this purpose.21 Direct ophthalmoscopes are easily available, lesser expensive and do not require specialized training in its use. It is also quick to use as demonstrated by Kothari who could complete the examination in ten seconds.16
We used an autorefractometer to objectively assess the refractive errors in the children even though most studies have compared the modified Brückner test with results of cycloplegic refraction.14–17,21 Due to low hospital accrual, lack of time, and non-consenting parents, cycloplegic refraction was not performed in our study. Further, we wished to analyse the eye under physiological conditions. Previous studies have shown good correlation between Plusoptix refraction and cycloplegic refraction.18
It was observed that 74% of the eyes had hypermetropia, 4.8% had myopia and 20.9% were emmetropic. Our study detected more hypermetropia (507 eyes) than myopia (33 eyes). This is in accordance with the fact that children undergo emmetropisation from a hypermetropic refractive state which is attained by adolescence due to the growth of the eye.6,22 Most studies have portrayed their results as ametropia versus emmetropia. This study detected ametropia in 88.7% which was similar to studies by Amitava (63.5%) and Rajalakshmi (66.66%).14,15 This could possibly be because these studies have a similar age group as in our study.
The existence of a superior crescent was significantly associated with hypermetropia and inferior crescent with myopia in our study. This was similar to the findings of Kotwal et al, and Kumar et al.23,24 In the study by Kotwal, in children aged two to 15 years, on classifying an eye as hypermetropic with a superior crescent and as myopic with an inferior crescent, high sensitivity and specificity were noted of the test in detecting refractive errors.23 Kumar et al reported high reliability measures of superior crescent detecting hypermetropia and inferior crescent detecting myopia in participants aged 10 to 40 years.24 A modified Brückner test using streak retinoscope was found to be very accurate in detecting anisometropia and strabismus in a study by Amitava.14 In the present study, with high sensitivity of 98.4% for superior crescent to detect hypermetropia, the chances of the test missing out on any eye with hypermetropia is less. But low specificity implies that it overestimates the condition.
In our study, we used a simple approach to quantify the refractive error, namely, crossing the horizontal midline by the crescent. This is simpler than previously reported methods in determining the magnitude of refractive errors using modified Brückner test. Kothari measured the dimensions of the crescent and determined that if the inferior crescent was greater than 1mm it was suggestive of myopia. If the crescent size was more than 2mm and superior, it was indicative of hyperopia, and if the crescent was decentered by one clock hour it was indicative of astigmatism.16 In the study by Kotwal et al, crescent size was determined based on whether it occupied <1/3, 1/3 to 2/3 or >2/3 area of the pupil and its correlation to refractive error was evaluated.23 Significant association was seen between crescent size and degree of hypermetropia as well as myopia. The approach in the present study is easier to understand for laypersons like teachers or rural health workers who can quickly screen for refractive error in children. With this method, we were able to establish that there was a significant association between larger superior crescent crossing the midline and higher hypermetropia > +1.5D, with Chi square value of 5.29, p=0.021. A similar association between myopia could not be evaluated due to smaller numbers of myopic eyes in our study.
We observed that superior crescent tended to appear in hypermetropia, and inferior crescent in myopia. When an indirect ophthalmoscope is used, the opposite effect may be seen with the crescent being inferior in hypermetropes, as demonstrated by Bhayana et al.20 This is due to the relative positions of the illumination and viewing systems of the instrument being used. In a classical direct ophthalmoscope, the illumination line is located below the viewing axis whereas it is vice versa in the indirect ophthalmoscope. Therefore, it is important that we consider the instrument being used while interpreting the results of modified Brückner screening tests.
In tackling visual impairment, it is essential to detect refractive errors early in children. It is recommended to prescribe glasses in children aged four and above with hyperopia more than +2.5D and more than +1.5D even when asymptomatic, in school going children.6 In those with myopia, distance visual acuity is compromised, but the children can see near objects with ease. However, hypermetropia is more difficult to detect and is more amblyogenic. If there is anisometropia, it becomes even more critical to detect it early. In children aged 3.5 years and above, hyperopic anisometropia as low as 1D can be amblyogenic. Many such cases can go undiagnosed as most children do not get routine formal vision screening tests especially in developing nations. With this study we have shown that using a direct ophthalmoscope alone to roughly quantify higher refractive errors has a potential role in preventing amblyopia.
In the future, modified Brückner screening need not be limited to an ophthalmoscope alone. Using digital cameras to screen for refractive errors has been studied.25 This can make tele-ophthalmological consultations easy and the counselling of the diagnosis to parents more approachable and feasible, it can be documented at each follow-up for the improvement or deterioration of the condition. Now, with the ubiquitous nature of mobile phones with camera, possibilities abound in this field. It is essential that we first establish the relationship between refractive errors and crescents in children as we venture into this newer field. This is one of the few studies that aimed at quantification of the refractive error in children using a simple and quick assessment of the crescent seen on modified Brückner test.
A limitation of the study was that due to the prevalent COVID-19 pandemic situation during the study period, more subjects from outreach camps were recruited and cycloplegic refraction was not performed. We have not evaluated the ability of modified Bruckner test to detect or quantify astigmatism in this study. Future studies can be planned, including this. The photoscreener used to measure refractive error may tend to underestimate hypermetropia and overestimate myopia.26,27 Participants were asked to fixate at a distant target, however pseudomyopia is possible if the participant failed to understand and looked at the direct ophthalmoscope.
Conclusion
In conclusion, this test is a useful screening tool in the detection of refractive error in children. It is a feasible, quick, simple and non-contact method for roughly quantifying refractive errors and has a potential to reduce visual impairment due to amblyopia.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical Statement
This research was reviewed and approved by the institutional review board of Kasturba Medical College Manipal, Manipal Academy of Higher Education (registration number ECR/146/Inst/KA/2013/RR-19). Informed consent was obtained from the parents or legal guardians of all the participants. The trial was registered prospectively with Clinical Trials Registry- India (registration number: CTRI/2021/05/033615, registered on 13/05/2021).
Acknowledgments
We would like to thank the Department of Optometry, Manipal College of Health Professions, Manipal Academy of higher Education, Manipal for allowing the usage of Plusoptix autorefractor during the conduct of this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No funding was received for this work.
Disclosure
Yogish S Kamath and Neetha Kuzhuppilly report grants from Indian Council of Medical Research (ICMR). The authors report no other conflicts of interest in this work.
References
1. Kalikivayi V, Naduvilath TJ, Bansal AK, Dandona L. Visual impairment in school children in southern India. Indian J Ophthalmol. 1997;45(2):129–134.
2. Ghosh S, Mukhopadhyay U, Maji D, Bhaduri G. Visual impairment in urban school children of low-income families in Kolkata, India. Indian J Public Health. 2012;56(2):163. doi:10.4103/0019-557X.99919
3. Prakash W, Marmamula S, Mettla A, Keeffe J, Khanna R. Visual impairment and refractive errors in school children in Andhra Pradesh, India. Indian J Ophthalmol. 2022;70(6):2131–2139. doi:10.4103/ijo.IJO_2949_21
4. Sheeladevi S, Seelam B, Nukella PB, Modi A, Ali R, Keay L. Prevalence of refractive errors in children in India: a systematic review. Clin Exp Optom. 2018;101(4):495–503. doi:10.1111/cxo.12689
5. Saxena R, Sharma P, Gopal S, et al. National consensus statement regarding pediatric eye examination, refraction, and amblyopia management. Indian J Ophthalmol. 2020;68(2):325–332. doi:10.4103/ijo.IJO_471_19
6. Leat SJ. To prescribe or not to prescribe? Guidelines for spectacle prescribing in infants and children. Clin Exp Optom. 2011;94(6):514–527. doi:10.1111/j.1444-0938.2011.00600.x
7. Klimek DL, Cruz OA, Scott WE, Davitt BV. Isoametropic amblyopia due to high hyperopia in children. J AAPOS. 2004;8(4):310–313. doi:10.1016/j.jaapos.2004.05.007
8. Murali K, Vidhya C, Murthy SR, Mallapa S. Cost-Effectiveness of photoscreeners in screening at-risk amblyopia in Indian children. Indian J Public Health. 2022;66(2):171–175. doi:10.4103/ijph.ijph_1848_21
9. Kinori M, Molina I, Hernandez EO, et al. The plusoptix photoscreener and the retinomax autorefractor as community-based screening devices for preschool children. Curr Eye Res. 2018;43(5):654–658. doi:10.1080/02713683.2018.1437453
10. Tongue AC, Cibis GW. Brückner test. Ophthalmology. 1981;88(10):1041–1044. doi:10.1016/S0161-6420(81)80034-6
11. Roe LD, Guyton DL. The red reflex from retinoscopy’s point of view. Reflections on a small area. Surv Ophthalmol. 1984;28(4):345–348. doi:10.1016/0039-6257(84)90099-7
12. Carrera A, Saornil MA, Zamora MI, Maderuelo A, Cañamares S, Pastor JC. Detecting amblyogenic diseases with the photographic Bruckner test. Strabismus. 1993;1(1):3–9. doi:10.3109/09273979309033847
13. Gole GA, Douglas LM. Validity of the Brückner reflex in the detection of amblyopia. Aust N Z J Ophthalmol. 1995;23(4):281–285. doi:10.1111/j.1442-9071.1995.tb00177.x
14. Amitava A, Kewlani D, Khan Z, Razzak A. Assessment of a modification of Brückner′s test as a screening modality for anisometropia and strabismus. Oman J Ophthalmol. 2010;3(3):131. doi:10.4103/0974-620X.71890
15. Rajalakshmi A, Rajeshwari M. Efficacy of Brückner’s test for screening of refractive errors by non-ophthalmologist versus ophthalmologist: a comparative study. Middle East Afr J Ophthalmol. 2019;26(4):185. doi:10.4103/meajo.MEAJO_121_19
16. Kothari M. Can the Brückner test be used as a rapid screening test to detect significant refractive errors in children? Indian J Ophthalmol. 2007;55(3):213. doi:10.4103/0301-4738.31943
17. LaMattina KC, Vagge A, Nelson LB. Can the red reflex test detect unequal refractive error? J Pediatr. 2019;214:175–177. doi:10.1016/j.jpeds.2019.06.051
18. Thomas J, Rajashekar B, Kamath A, Gogate P. Comparison between Plusoptix A09 and gold standard cycloplegic refraction in preschool children and agreement to detect refractive amblyogenic risk factors. Oman J Ophthalmol. 2021;14(1):14. doi:10.4103/ojo.OJO_284_2019
19. Iyer V, Saeed P, Saeed P. The Brückner Test Variant (BTV): a promising instrument in detecting vision disorders. Am Orthopt J. 2013;63(1):97–102. doi:10.3368/aoj.63.1.97
20. Bhayana AA, Prasad P, Azad SV. Refractive errors and the red reflex- Brückner test revisited. Indian J Ophthalmol. 2019;67(8):1381–1382. doi:10.4103/ijo.IJO_2107_18
21. Tuteja SY, Blaikie A, Kekunnaya R. Identification of amblyogenic risk factors with the Brückner reflex test using the low-cost Arclight direct ophthalmoscope. Eye. 2021;35(11):3007–3011. doi:10.1038/s41433-020-01341-9
22. Flitcroft DI. Emmetropisation and the aetiology of refractive errors. Eye. 2014;28(2):169–179. doi:10.1038/eye.2013.276
23. Kotwal NN, Kulkarni V, Khandgave T. Predictive value of brückner test in detecting refractive errors among children. J Clin Diagn Res. 2022;16:4.
24. Kumar PS, Kamath YS. The utility of a direct ophthalmoscope in estimating the magnitude of refractive error using a modification of the Brückner test. Expert Rev Ophthalmol. 2021;16(5):411–415. doi:10.1080/17469899.2021.1945924
25. Bani SAO, Amitava AK, Sharma R, Danish A. Beyond photography: evaluation of the consumer digital camera to identify strabismus and anisometropia by analyzing the Brückner’s reflex. Indian J Ophthalmol. 2013;61(10):608–611. doi:10.4103/0301-4738.121092
26. Payerols A, Eliaou C, Trezeguet V, Villain M, Daien V. Accuracy of PlusOptix A09 distance refraction in pediatric myopia and hyperopia. BMC Ophthalmol. 2016;16(1):72. doi:10.1186/s12886-016-0247-8
27. Yan XR, Jiao WZ, Li ZW, Xu WW, Li FJ, Wang LH. Performance of the plusoptix A09 photoscreener in detecting amblyopia risk factors in Chinese children attending an eye clinic. PLoS One. 2015;10(6):e0126052. doi:10.1371/journal.pone.0126052
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.