Back to Journals » Clinical Optometry » Volume 14
Design and Validation of a New Smartphone-Based Reading Speed App (GDRS-Test) for the Greek Speaking Population
Authors Almaliotis D, Athanasopoulos GP, Almpanidou S, Papadopoulou EP, Karampatakis V
Received 20 April 2022
Accepted for publication 17 July 2022
Published 2 August 2022 Volume 2022:14 Pages 111—124
DOI https://doi.org/10.2147/OPTO.S370215
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Diamantis Almaliotis, Georgios P Athanasopoulos, Stavroula Almpanidou, Eleni P Papadopoulou, Vasileios Karampatakis
Laboratory of Experimental Ophthalmology, School of Medicine, Aristotle University of Thessaloniki, Thessaloniki, Greece
Correspondence: Diamantis Almaliotis, Laboratory of Experimental Ophthalmology, University Campus, Aristotle University, Thessaloniki, Greece, Tel/Fax +306934035255, Email [email protected]
Purpose: To present a novel smartphone-based application (GDRS-test, Greek Digital Reading Speed - test) for the assessment of reading speed, to evaluate, whether this test could be easily and reliably used by patients with visual impairment and normal individuals serving as an adjunctive tool for their visual examination.
Patients and Methods: One hundred and five visually impaired and 32 normal eyes were examined. Depending on existing active ocular pathology, patients were divided into a non-macular and a macular group, We examined the reading performance for continuous text (MNREAD chart) and random unrelated words of the new smartphone-based reading speed app, monocularly. The patients’ best-corrected visual acuity ranged from 1.3 to 0.2 logMAR. Examinees were asked to read aloud (at a 40 cm distance) a series of 30 random two-syllable and then 30 three-syllable Greek words, without semantic connection. Reading speed was measured as correct words per minute for critical print size. The individuals were examined twice within 2 weeks for test-retest reliability. Correlations and comparisons concerning each group adjusted for age and visual acuity were performed.
Results: There was moderate correlation between MNREAD and 2SYL SPEED (Reading speed for 2-syllable) (Pearson’s rho = 0.589, p < 0.001) and 3SYL SPEED (Reading speed for 3-syllable) (Pearson’s rho = 0.617, p < 0.001) for healthy individuals. The mean 2SYL SPEED and 3SYL SPEED for Individuals of the maculopathies group or non-maculopathies group were significantly lower compared to normal individuals adjusted for age and visual acuity [B (95% CI): − 93.077 (− 104.165, − 81.98), p < 0.001] and [B (95% CI): − 92.254 (− 104.196, − 80.312), p < 0.001], respectively. The test-retest analysis showed a good agreement for patients and healthy individuals.
Conclusion: The novel-reading speed application for the Greek-speaking population was found to accurately detect differences between patients with visual impairment and healthy individuals. It was designed and constructed with the intention to ease and improve the ophthalmic examination allowing individuals to self-evaluate reading speed by transmitting the result to their physician.
Keywords: reading speed, visual impairment, print size, visual acuity, maculopathies
Introduction
In the shadow of other clinical examinations, such as visual acuity (VA), which has a dominant role in daily practice and trials, reading performance could be considered as an underestimated parameter of visual function assessment.1,2
Moreover, measured reading performance is closer to real-life daily tasks and scenarios than near visual acuity,3 and is among the best predictors of patients’ subjective visual ability and vision-related quality of life.4,5 For example, diabetic patients after macular laser photocoagulation are often unhappy due to poor reading performance, despite good distance and near visual acuity.6
It has also been used as the primary outcome measure for several clinical trials on the effectiveness of low vision rehabilitation7 and as a secondary outcome measure for clinical trials of pharmaceutical and surgical treatment of a wide range of eye diseases.
Various diseases affecting the macula, optic nerve, or peripheral retina may lead to deterioration of reading ability, in terms of reading speed, comprehension, or preferred print size, which could have a major negative impact on patients’ quality of life.8–10
Indicatively, the distribution of LV causes in the Greek population according to our previous estimation was as follows: Age-related macular degeneration (AMD) accounting for 50.0% of the cases (75 (64.1%) had the dry form and 42 (35.9%) had the wet form of the disease) diabetic retinopathy (DR) 19.9% and glaucoma 7.2%. Other causes of LV included retinitis pigmentosa in a percentage of 5.3% and other hereditary retinal diseases (3%), previous retinal detachment (2.5%), other maculopathies (2.1%) and various other ocular diseases (9.7%).11
Several tests have been developed to evaluate reading performance as accurately as possible. Jaeger, Parinaud, and Nieden were among the pioneers of this domain, although these primary efforts were not well standardized. The first efforts towards standardization, which is crucial for reliable assessment,12 were made by Birkhaeuser at the dawn of the 20th century.13 Bailey and Lovie’s reading chart contains 4-, 7- and 10-character random words in logarithmically progressing sizes.14 MNREAD chart consists of 60-character sentences in various print sizes, with logarithmic progression, too.15 There is also a Greek validated printed version of this chart,16 also available in digital form.17 In a similar style, we also mention the Colenbrander Continuous Text Near Vision Cards, consisting of shorter sentences (44 characters). Radner et al developed charts including standardized sentences concerning size and proportion of words and characters, under more strict rules.18,19 Pepper Visual Skills for Reading (VSR) test20 and SKread test21 use unregulated sequences of unrelated words and single characters, whereas other tests are based on the reading of small or larger paragraphs (eg, Sloan, Oculus Reading Probe II, Eschenbach and Zeiss test, Radner paragraph optotypes).
Among available near acuity charts, MNREAD seems to offer an essential advantage. The measurements are done on the logMAR scale, and the examiner can measure reading speed and critical print size. MNREAD is appropriate and reliable for both normally sighted as well as low vision subjects.15
Various digital tests have also been developed to evaluate reading performance. In general, grace to their compact size and long battery life, mobile devices might be readily utilized at the examination. The expanded processing power of smartphone devices, as well as their plenty of sensors, can empower reading metrics to be determined automatically. There are two digital methods for calculating the reading speed of each sentence: using a web stopwatch and utilizing a cursor of the recorded patient’s audio.22 A semi-automatic method to calculate reading duration (Salzburg Reading Desk) records the patient’s voice, whereas the administrator sets the starting and ending time of reading.23 A simple automatic timer was implemented as a feature of an iPad digital reading test.24 An automated method of measuring the speech duration by determining the onset and the end of vocalization has also been described.25
The aim of the present study is to develop and evaluate a new self-performed smartphone-based reading speed test allowing people with low vision to make a quick, and sensitive self-assessment. We confirmed the diagnostic performance of the novel reading speed app for identifying eyes as pathological or normal and also confirmed the test-retest reliability for the Greek-speaking population. The results of the test are stored in the mobile device and are transmitted to the authorized ophthalmologist, who has the follow-up of the patient and the ophthalmologist may advise the patient appropriately or ask for an immediate examination by physical presence in the doctor’s office.
Materials and Methods
This is a cross-sectional study. Approval for this study was granted by the bioethical committee (Ethical Approval code#1.60/21.11.2018) of the Aristotle University of Thessaloniki, School of Medicine, Medical Department, Aristotle University of Thessaloniki, and adhered to the principles embodied in the Declaration of Helsinki Code of Ethics of the World Medical Association. Consent forms for the research were acquired by all subjects before their participation. The General Data Protection Regulation GDPR in a research context, and the Greek Law of Data Protection were respected through the confidentiality and anonymity of the data.
All participants were recruited prospectively from our outpatient unit at Aristotle University of Thessaloniki, School of Medicine running the LIFE4LV project for patients with visual impairment, which it was official registered at ClinicalTrials.gov. The number of the study is NCT05184036.
Participants
Our study included 137 eyes of 105 patients and 32 age and gender matched healthy individuals. The examination took place in the Laboratory. The mean age of the total sample was 59.55 (sd:19.66), including only adults (>18 years of age) (Table 1).
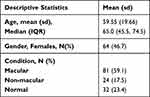 |
Table 1 Descriptive Statistics of the Total Sample |
All subjects underwent a comprehensive eye examination including demographic variables such as general health history, systemic conditions and medication along with the current spectacle correction. Measurement of BCVA determined with the Early Treatment Diabetic Retinopathy Study (ETDRS) chart (Precision Vision, USA, chart 1) under standard clinical conditions. The ophthalmological examination was performed from our outpatient unit at Aristotle University including among others: the slit-lamp examination providing details of the anterior part of the eye, the lens, and fundoscopy. BCVA was converted to logarithm of the minimal angle of resolution (logMAR) visual acuity.
The patients completed the whole examination in a single visit. Only the eye with the BCVA was included from each subject, and in the case of similar BCVAs, the right eye was chosen. Visually impaired patients were included if BCVA of the best eye was between 0.2 and 1.3 logMAR, (0.2–0.4 logMAR – mild impairment, 0.5–1 logMAR – moderate impairment and 1.1–1.3-severe impairment). Normal individuals had BCVA up to 0.1 logMAR. Depending on existing ocular pathology, patients were divided into a non-macular and a macular group. The non-macular group (24 eyes) included: glaucoma (7), optic neuropathy (7), retinitis pigmentosa (10). On the other hand, the macular group (81 eyes) included dry age-related macular degeneration (22), wet-age related macular degeneration (22) diabetic retinopathy with macula oedema (21), retinal detachment (4), myopic degeneration (2), macular hole (1), Stargardt’s disease (3), epiretinal membrane (4) Retinal vein occlusion (2).
Subjects with co-existence of macular and non-macular morbidity were excluded, as well as patients with significant cataracts (grade >1 LOCS II), corneal opacities, keratitis, acute uveitis, and acute glaucoma. Moreover, people with cognitive and/or mental impairment, illiterate and non-fluent Greek-reading individuals were also excluded.
Examination Protocol
The New Smartphone-Based Reading Speed App (GDRS-Test)
In the context of our smartphone application Life4lv®, the reading speed test was performed using a Samsung A30S smartphone (display: Super AMOLED, size 6.4 inches, resolution 720×1560 pixels, ratio 19.5:9, density ~268 ppi; GPU: Mali-G71 MP2) running Android OS 9.0.
The device was switched on approximately 5 min before each experimental session to allow its output to stabilize. The device was kept at a 40 cm distance from the eye, with examinees’ wearing their best-spectacle correction for reading. The eye with the BCVA was only examined. The contralateral eye was occluded with an eye patch.
The examinees hold the smartphone-based reading speed application in landscape mode and are instructed to read loudly (for easier scoring4), as fast as possible, a series of 30 random 2 or 3-syllable common Greek words, without semantic connection. The words were in rows through the whole screen. They are common and frequently used words, not resembling acoustically, containing Greek characters. Reading time was starting when the examinee pressed the Start button and stopped by pressing the Finish button on the screen (Figure 1). The chronometer was displayed on the right top of the screen. Reading errors were detected using an audio recorder (Google speech analyzer) through internet connection. Misread or omitted words were considered as wrong. At the end of the examination, the number of correct words and reading time were displayed. Reading speed was calculated as correct words per minute (wpm).
Characteristics of the New Digital Reading Speed App
All characters were black-on-white background. Spaces between consequent words were equivalent to one character’s size for the viewing distance of 40cm. Spaces between consequent characters were at the size of the characters’ lines. Every set of 30 words contains a series of 2-syllable or 3-syllable unrelated words in a sequence of decreasing sizes (at 0.1 logMAR steps) and in a proportionally-spaced font.
Summary of the Characteristics
- All characters were black-on-white background. Spaces between consequent words were equivalent to one character’s size.
- Every set of words contains a series of 30 2-syllable and 30 3-syllable unrelated words
- Size is defined by the height of a lowercase letter that has no ascenders or descenders.
- Sixteen different print sizes were successively demonstrated for reading, corresponding to VA from 1.4 to −0.1 logMAR when viewed at a reading distance of 40 cm.
- Crowding Effect: Vertical distance between rows of letters were equivalent to one character’s size.
- Words with high-frequency in Greek language were selected not resembling acoustically.
Procedure
- The normal subjects were asked to read aloud the MNREAD Acuity Chart. The examiner revealed the print size corresponding to VA and changing in steps of 0.1 logMAR and the normal participants were instructed to read the sentences aloud as quickly and accurately as possible. The researcher used a stopwatch to record the reading time (in seconds), and counted the number of errors (misread or missing words). For each sentence, the reading speed (measured in words per minute – wpm) is calculated by the following formula:
Reading speed:60*(10 − number of errors)/reading time
The same procedure was followed for the new smartphone-based reading speed app (GDRS-test). The normal participants were also examined with 30 2- and 3-syllable unrelated words in the print size corresponding to VA and changing in steps of 0.1 logMAR and the normal participants were instructed to read the words aloud as quickly and accurately as possible. The reading speed was measured in words per minute – (wpm)
- As regards the visually impaired individuals, 16 different print sizes were available to be demonstrated for reading, corresponding to VA from 1.4 to −0.1 logMAR. The minimum one corresponding to asymptotic levels of reading speed was chosen as “critical” print size (CPS) for our study, according to literature.26 Then, another series of 30 2-syllable and 3-syllable words were demonstrated for reading, following the same procedure.
- The retest was performed within two weeks.
Statistical Analysis
The Shapiro–Wilks test was used to assess normality of continuous variables. Continuous variables were described using mean (sd). Categorical variables were described using frequencies (percentages/relative frequencies). The relationship between two independent samples such as print size between individuals with maculopathies and healthy individuals was examined using Student’s independent samples t-test or the Mann–Whitney U-test. Chi-square test of independence was used to examine the association between categorical variables, such gender and disease status. Generalised linear models were used to examine the relationship of 2SYL SPEED, 3SYL SPEED, PRINT SIZE, INDEX 2SYL and INDEX 3SYL between macular, non-macular and healthy individuals adjusted for age. Fisher’s Least Significant Difference (LSD) was used to adjust for multiple testing. Pearson correlation coefficient was used to examine the association between Greek version of the MNREAD acuity chart and the new smartphone-based reading speed app. The intra-class correlation coefficient (ICC) was used as a measure of test-retest reliability of 2SYL SPEED, 3SYL SPEED, PRINT SIZE, INDEX 2SYL and INDEX 3SYL. P values less than 0.05 were considered statistically significant. SPSS 27.0 was used for the statistical analysis and R ver.4.0.0 (R Foundation of Statistical Computing, Vienna, Austria) was used for the calculation of ICC and Bland Altman analysis using the packages psych27 and blandr, 28 respectively.
Results
Concerning normal individuals, comparisons between MNREAD and new smartphone-based reading speed app (GDRS-test) (2SYL SPEED and 3SYL SPEED) were evaluated, while Bland Altman plots are presented in Figures 2 and 3. There is an association between MNREAD (range: 137.93–242.91), with mean reading speed: 181.69 (SD:29.53) and 2SYL SPEED and 3SYL SPEED. There was moderate correlation between MNREAD and 2SYL SPEED (Pearson's rho = 0.589, p < 0.001) and 3SYL SPEED (Pearson's rho = 0.617, p < 0.001).
 |
Figure 2 Association between MNread and 2SYL SPEED. |
 |
Figure 3 Association between MNread and 3SYL SPEED. |
According to Tables 2 and 3, age was significantly higher in macular cases compared to non-macular (p < 0.001) and normal individuals (p < 0.001), but it did not differ significantly between non-macular and normal individuals (p = 0.131). Furthermore, VA did not differ significantly between non-macular and macular individuals (p = 0.158). There is no association between disease status and gender (p = 0.814).
 |
Table 2 Descriptive Statistics of Age, VA, 2SYL SPEED, 3SYL SPEED, Print Size and Index for the Three Groups |
 |
Table 3 Relationship Between Disease Status and Gender |
The mean 2SYL SPEED and 3SYL SPEED for Individuals with maculopathies or non-maculopathies had significantly lower speed compared to normal individuals adjusted for age and VA [B (95% CI): −93.077 (−104.165, −81.98), p < 0.001]. [B (95% CI): −92.254 (−104.196, −80.312), p < 0.001], respectively.
Furthermore, the INDEX 2SYL and INDEX 3SYL regarding Individuals with maculopathies or non-maculopathies was significantly lower compared to normal individuals adjusted for age and VA [B (95% CI): −240.854 (−258.416, −223.292), p < 0.001] and B (95% CI): −224.301 (−246.586, −202.016), p < 0.001], respectively (Table 4).
 |
Table 4 Linear Regression Estimates for the Difference in 2SYL SPEED, 3SYL SPEED, PRINT SIZE and INDEX Between Diseased and Normal Individuals Adjusted for Age and VA |
Comparisons Between the Three Groups
No significant differences were detected in 2SYL SPEED (p = 0.744), 3SYL SPEED (0.869), INDEX 2SYL (p = 0.924) and INDEX 3SYL (p = 0.888) between individuals of macular and non-macular disease adjusted for age and VA (Tables 5 and 6).
 |
Table 6 LSD Adjusted Pairwise Comparisons Between the Three Groups |
On the other hand, mean speed for 2-syllable words was higher in normal individuals compared to macular (p < 0.001) and non-macular individuals adjusted for age and VA LOGMAR (p < 0.001). Moreover, the mean speed for 3-syllable words was higher in normal individuals compared to individuals with macular (p < 0.001) and non-macular morbidities adjusted for age and VA (p < 0.001) (Figures 4 and 5).
 |
Figure 4 Boxplot of 2-syllable words/min speed for the three subject groups. |
 |
Figure 5 Boxplot of 3-syllable words/min speed for the three subject groups. |
Test-Retest Reliability
The test-retest reliability analysis was performed on 55 eyes (24 impaired eyes, 31 normal). The patients were examined twice within a 2-week period and their scores in reading speed for 2-syl and 3-syl words were recorded. The enrolled patients were checked for changes in visual parameters in order to proceed for retest. Specifically, it was confirmed an agreement for test-retest for healthy, for patients as well as for the total number of the individuals. The summaries are presented in Table 7.
 |
Table 7 Results of Bland Altman Analysis of Agreement Test-Retest of 2SYL and 3SYL Speed |
Test-retest reliability analysis was applied by estimating the Intraclass Correlation Coefficients (ICCs) and the corresponding 95% confidence intervals. The ICCs in both 2-syllable and 3-syllable words for our total sample were found to be equal to 0.99 (95% CI: 0.98, 0.99) and 0.99 (95% CI: 0.98, 0.99), respectively, indicating excellent reliability, suggesting the high repeatability and consistency of the smartphone-based reading speed test.
Concerning our patients’ group, 2-syllable and 3-syllable words ICC was found equal to 0.85 (95% CI: 0.73, 0.92) and 0.86 (95% CI: 0.73, 0.92), respectively, indicating very good reliability.
For healthy controls, ICC was found equal to 0.98 (95% CI: 0.96, 0.99)
for 2-syllable and 0.95 (95% CI: 0.89, 0.97) for 3-syllable, respectively, indicating excellent reliability.
Moreover, the results of Bland Altman analysis regarding agreement in test-retest of Speed 2SYL and Speed 3SYL indicated excellent reliability for each group, Figures 6–9.
 |
Figure 6 Bland-Altmann plot. Test-retest of 2-syllable words/min speed for patients. |
 |
Figure 7 Bland-Altmann plot. Test-retest of 2-syllable words/min speed for healthy individuals. |
 |
Figure 8 Bland-Altmann plot. Test-retest of 3-syllable words/min speed for patients. |
 |
Figure 9 Bland-Altmann plot. Test-retest of 3-syllable words/min speed for healthy individuals. |
Discussion
The compared two tests in the Greek language (MNREAD and GDRS-test) differ from each other as regards measuring the reading speed with or without linguistic inference. If a sequence of words loses the syntactic and semantic coherence, reading becomes more difficult and slows down.14,15 Consequently, reading word-by-word is slower because it allows a limited degree of prediction of upcoming words. The MNREAD test uses simple sentences with intact grammar and meaning. It is a preferred instrument to determine reading speed and critical print size and is a well-used clinical tool to evaluate reading performance15
On the other hand, the new digital test uses random sequences of words, and there is no possibility for prediction of the next word based on the occurrence of the previous one. Thus, the new app minimizes the influence of linguistics, reading experience, and education level on test outcome.
Comparison of the MNREAD Acuity Chart and the new reading speed test was confirmed. There was moderate correlation between MNREAD and 2SYL SPEED (Pearson's rho = 0.589, p < 0.001) and 3SYL SPEED (Pearson's rho = 0.617, p < 0.001) in reading speed values. It has to be outpointed that the two tests have good agreement between them that were shown in the Bland-Altman plot and indicated that the new digital reading speed test was comparable with the standardized (MNREAD) reading chart.
The reading speed measurement using the new reading speed test in the current study was also similar to in reading speed values results reported by Legge et al.15 The new test can be installed in any androids and ios mobile device. Moreover, it is easily upgradable showing that it can be used in clinical and research settings.
With the printed chart, the experimenter must use a clear piece of paper to veil the following sentences. At that point, to start the trial, the experimenter must uncover the test sentence and start the chronometer. Additionally, start and stop counting the time of each sentence may have a little but significant delay given the short counted time of reading each sentence.
As a result, there might be an inaccuracy of the reading time, and consequently an inaccuracy of reading speed. In comparison, the app’s instant presentation of the test paired with an automatic start and an ending icon would lead to a more accurate estimate of reading time. There is a consideration that compared stopwatch versus computerized timing in a computer-based reading test22 These authors reported that stopwatch timing belittled reading time by approximately 0.3s. Such difference translates into a 5% difference in reading speed at 100 wpm, 7.5% at 150 wpm, 10% at 200 wpm, and 12.5% at 250 wpm.
Reading can be influenced by many factors including font typeface.6 The Times New Roman and Arial typefaces tuned specifically for the display on a computer screen29 In another study that was designed to compare the onscreen legibility between sans serif with serif typefaces. Participants read faster and their eye-movement behavior was better, when the fond type was set in san serif typeface30 (Arial, Verdana).
Hence, the presented digital test has several advantages. It is very likely to increase reliability, due to more consistent sentence display, and more accurate timing. Moreover, it allows for an instantaneous presentation of the results, by transmitting the result to their physician. Time sparing can be particularly important in clinics where many patients have to be seen. It is really important the potential for self-administration.
As a self performed test may help patient/physician for an early detection of changes that may need intervention in conjuction with other tests as well. A distant living patient or patients with certain difficulties for frequent visits (financial reason, mobility problems, need for accompanying person due to low vision etc) may use this application in cooperation with their physician.
Patients with ocular pathology demonstrate lower reading speed,31 compared to normal controls and the new test has ability to disseminate them. However, it seems that there is no significant impact of the macula status on the preferred word size. It would be reasonable for patients with maculopathy but a good peripheral vision to read bigger words (3-syllable) faster, as it would be easier to recognize the initial and final characters and then guess the inner ones and reconstruct the word. On the other hand, patients with good central, but impaired peripheral vision, should read shorter words (2-syllable) faster, supposing that missing initial and final characters should be more for larger words. However, it seems that word size’s effect on reading speed is not so easily predictable. People with maculopathy may have various types of scotoma or distortion, which may be central (typically), at the right, or at the left of fixation. Scotoma may even be like a ring, sparing the center of fixation in some cases. It has been demonstrated that patients using peripheral vision have worse reading performance26 because of lower information transfer rate, which is attributed to both smaller visual span in the periphery (which is the number of characters recognized at a glance while fixating at the center) and slower temporal processing.31 The crowding effect could also be influential, though this is not universally proven.32 Furthermore, scotomas at the right of fixation hide the terminal of words, which may be easier to predict, compared to left scotomas hiding the beginning, though it is shown that saccadic movements are more helpful in left scotomas.21,33 Scotomas below fixation or preferred retinal loci (PRL) are fairly disabled and lead to the omission of whole lines of text. We should take into account the development of PRL in many patients and their location concerning scotoma. Meanwhile, even patients with peripheral scotoma may also miss crucial characters at the beginning or the end of 2-syllable words, leading to misreading. Concerning glaucoma, it seems that reading performance is better for shorter and more frequent words, whereas difficulty increases for words at the end of the line.34
Based on previous work on test-retest reliability of vision tests using continuous text and random words,15 we had an expectation that the new digital reading speed test may also fare well in this regard. Specifically, an agreement was confirmed for test-retest for healthy, for patients as well as for the total number of the individuals. The results of Bland Altman analysis regarding agreement in test-retest of 2SYL Speed and 3SYL Speed indicated excellent reliability for each group, of the new digital reading speed test.
Limitations of our study include the inability to predict patients’ scotomata and distortion, as it is shown in patients with maculopathies and patients with diseases affecting peripheral vision. Other parameters which are considered to be related with reading performance, such as low-contrast vision, motor ability, and attentional field integrity34–36 have not been taken into account given the fact that they are always present as underlying factors in these patients.
To our knowledge, there is no other similar test consisting of various unrelated single words in Greek language. Lack of conceptual connection between consecutive words allows a more objective and valid assessment among different patients or at different examination times of a given patient, as it eliminates any possible advantage in reading time that could be attributed to a logical prediction of upcoming words,37 or a better mental, cognitive or lingual level of certain patients.
This application could serve as an easy-to-use and inexpensive means of self-assessment and remote monitoring of patients, to reduce burden in outpatient clinics and detect early signs of disease progression. As it is already shown, our test differentiates ophthalmology patients from healthy controls, and it demonstrates remarkable reproducibility and test-retest reliability.
Conclusion
It is the first study to investigate the parameters of reading speed using randomly arranged words not producing meaningful sentences, in the Greek population. Our intention is in a future work is to select words in other languages as well.
Significant difference in performance between patients with low vision and healthy controls, as well as elimination of semantic and linguistic connections due to randomized character of presented words, implement that our test could serve as a useful tool for the detection of visual disorders. Furthermore, very good ICC values achieved for all subjects’ categories suggest that this is a highly reliable and reproducible test, which could also be used for patients’ monitoring with the ability to indicate possible progress or deterioration in the course of their disease. In addition to that, the digital character of our test makes it more accessible to patients and easy for them to use, given they are familiar with smartphone technologies, therefore may play a valuable role in their follow-up. This novel digital test is a proper tool for consecutive home examinations with the co-operation of the attending physician.
Funding
This research has been co-financed by the European Union and Greek national funds through the Operational Program Competitiveness Entrepreneurship and innovation under the call Research-Create-Innovate (project CODE: T1EDK-03742).
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this paper. All authors report grants from Eidikos Logariasmos Kondylion Erevnas A.P.TH., during the conduct of the study.
References
1. Giacomelli G, Virgili G, Giansanti F, et al. Clinical and microperimetric predictors of reading speed in low vision patients: a structural equation modeling approach. Invest Ophthalmol Vis Sci. 2013;54(6):4403–4408. PMID: 23722392. doi:10.1167/iovs.12-10734
2. Patel PJ, Chen FK, Da Cruz L, et al. A. Test-retest variability of reading performance metrics using MNREAD in patients with age-related macular degeneration. Invest Ophthalmol Vis Sci. 2011;52(6):3854–3859. PMID: 21421873. doi:10.1167/iovs.10-6601
3. Chen AH, Khalid NM, Buari NH. Age factor affects reading acuity and reading speed in attaining text information. Int J Ophthalmol. 2019;12(7):1170–1176. PMID: 31341810; PMCID: PMC6629798. doi:10.18240/ijo.2019.07.19
4. Rubin GS. Measuring reading performance. Vision Res. 2013;90:43–51. PMID: 23506967. doi:10.1016/j.visres.2013.02.015
5. Kingsnorth A, Wolffsohn JS. Mobile app reading speed test. Br J Ophthalmol. 2015;99(4):536–539. PMID: 25355805. doi:10.1136/bjophthalmol-2014-305818
6. Pearce E, Sivaprasad S, Chong NV. Factors affecting reading speed in patients with diabetic macular edema treated with laser photocoagulation. PLoS One. 2014;9(9):e105696. PMID: 25265280; PMCID: PMC4179230. doi:10.1371/journal.pone.0105696
7. Nguyen NX, Weismann M, Trauzettel-Klosinski S. Improvement of reading speed after providing of low vision aids in patients with age-related macular degeneration. Acta Ophthalmol. 2009;87(8):849–853. PMID: 19141148. doi:10.1111/j.1755-3768.2008.01423.x
8. Kim JS, Kim JY, Kim KT, et al. Near reading speed changes after panretinal photocoagulation in diabetic retinopathy patients: a prospective study using an iPad application for the measurement of reading speed. Graefes Arch Clin Exp Ophthalmol. 2019;257(12):2631–2638. PMID: 31654187. doi: 10.1007/s00417-019-04494-w
9. Omari A, Niziol LM, Gardner TW. Reading deficits in diabetic patients treated with panretinal photocoagulation and good visual acuity. Acta Ophthalmol. 2019;97(7):e1013–e1018. PMID: 30968579. doi:10.1111/aos.14097
10. Varadaraj V, Lesche S, Ramulu PY, et al. Reading speed and reading comprehension in age-related macular degeneration. Am J Ophthalmol. 2018;186:138–143. PMID: 29246579. doi:10.1016/j.ajo.2017.11.026
11. Almpanidou S, Almaliotis D, Karamitopoulos L, Topouzis F, Labiris G, Karampatakis V. Causes of low vision in a Greek population. Acta Ophthalmol. 2021;99. doi:10.1111/j.1755-3768.2020.0254
12. Altpeter EK, Marx T, Nguyen NX, et al. Measurement of reading speed with standardized texts: a comparison of single sentences and paragraphs. Graefes Arch Clin Exp Ophthalmol. 2015;253(8):1369–1375. PMID: 26067392. doi: 10.1007/s00417-015-3065-4
13. Radner W. Reading charts in ophthalmology. Graefes Arch Clin Exp Ophthalmol. 2017;255(8):1465–1482. PMID: 28411305; PMCID: PMC5541099. doi:10.1007/s00417-017-3659-0
14. Bailey IL, Lovie JE. The design and use of a new near-vision chart. Am J Optom Physiol Opt. 1980;57(6):378–387. PMID: 7406006. doi:10.1097/00006324-198006000-00011
15. Legge GE, Ross JA, Luebker A, et al. Psychophysics of reading. VIII. The Minnesota low-vision reading test. Optom Vis Sci. 1989;66(12):843–853. PMID: 2626251. doi:10.1097/00006324-198912000-00008
16. Mataftsi A, Bourtoulamaiou A, Haidich AB, et al. Development and validation of the Greek version of the MNREAD acuity chart. Clin Exp Optom. 2013;96(1):25–31. doi:10.1111/j.1444-0938.2012.00799.x
17. Labiris G, Panagiotopoulou EK, Chatzimichael E, et al. Introduction of a digital near-vision reading test for normal and low vision adults: development and validation. Eye Vis. 2020;7:51. doi:10.1186/s40662-020-00216-0
18. Radner W, Willinger U, Obermayer W, et al. Eine neue Lesetafel zur gleichzeitigen Bestimmung von Lesevisus und Lesegeschwindigkeit [A new reading chart for simultaneous determination of reading vision and reading speed]. Klin Monbl Augenheilkd. 1998;213(3):174–181. German. PMID: 9793916. doi:10.1055/s-2008-1034969
19. Radner W, Obermayer W, Richter-Mueksch S, et al. The validity and reliability of short German sentences for measuring reading speed. Graefes Arch Clin Exp Ophthalmol. 2002;240(6):461–467. PMID: 12107513. doi: 10.1007/s00417-002-0443-5
20. Stelmack J, Stelmack TR, Fraim M, et al. Clinical use of the pepper visual skills for reading test in low vision rehabilitation. Am J Optom Physiol Opt. 1987;64(11):829–831. PMID: 3425678. doi:10.1097/00006324-198711000-00005
21. MacKeben M, Nair UK, Walker LL, et al. Random word recognition chart helps scotoma assessment in low vision. Optom Vis Sci. 2015;92(4):421–428. PMID: 25946100; PMCID: PMC4376273. doi:10.1097/OPX.0000000000000548
22. Xu R, Bradley A. IURead: a new computer-based reading test. Ophthalmic Physiol Opt. 2015;35(5):500–513. doi:10.1111/opo.12233
23. Dexl AK, Schlögel H, Wolfbauer M, et al. Device for improving quantification of reading acuity and reading speed. J Refract Surg. 2010;26(9):682–688. doi:10.3928/1081597X-20091119-01
24. Calabrèse A, To L, He Y, et al. Comparing performance on the MNREAD iPad application with the MNREAD acuity chart. J Vis. 2018;18(1):8. doi:10.1167/18.1.8
25. Radner W, Diendorfer G, Kainrath B, et al. The accuracy of reading speed measurement by stopwatch versus measurement with an automated computer program (rad-rd©). Acta Ophthalmol. 2017;95(2):211–216. doi:10.1111/aos.13201
26. Falkenberg HK, Rubin GS, Bex PJ. Acuity, crowding, reading and fixation stability. Vision Res. 2007;47(1):126–135. PMID: 17078991. doi:10.1016/j.visres.2006.09.014
27. Revelle W. psych: procedures for psychological, psychometric, and personality research. Northwestern University, Evanston, Illinois. R package version 2.1.9; 2021. Available from: https://CRAN.R-project.org/package=psych.
28. Datta D. blandr: a Bland-Altman method comparison package for R. Zenodo. Available from: https://github.com/deepankardatta/blandr.2017.
29. Kingery D, Furuta R. Skimming electronic newspaper headlines: a study of typeface, point size, screen resolution, and monitor size. Inf Process Manag. 1997;33:685–696. doi:10.1016/S0306-4573(97)00025-3
30. Bernard M, Chaparro B, Mills M, Hacomb C. Comparing the effects of text size and format on the readability of computer-displayed Times New Roman and Arial text. Int J Hum Comput Stud. 2003;59(6):823–835. doi:10.1016/S1071-5819(03)00121-6
31. Cheong AM, Legge GE, Lawrence MG, et al. Relationship between slow visual processing and reading speed in people with macular degeneration. Vision Res. 2007;47(23):2943–2955. PMID: 17881032; PMCID: PMC2094698. doi: 10.1016/j.visres.2007.07.010
32. Chung ST, Jarvis SH, Woo SY, et al. Reading speed does not benefit from increased line spacing in AMD patients. Optom Vis Sci. 2008;85(9):827–833. PMID: 18772718; PMCID: PMC2729069. doi:10.1097/OPX.0b013e31818527ea
33. Watson GR, Schuchard RA, De l’Aune WR, et al. Effects of preferred retinal locus placement on text navigation and development of advantageous trained retinal locus. J Rehabil Res Dev. 2006;43(6):761–770. PMID: 17310425. doi:10.1682/jrrd.2005.07.0120
34. Rolle T, Dallorto L, Cafasso R, et al. Reading ability in primary open-angle glaucoma: evaluation with Radner reading charts. Optom Vis Sci. 2019;96(1):55–61. PMID: 30570594. doi:10.1097/OPX.0000000000001319
35. Rossouw P, Guichard MM, Hatz K. Contrast sensitivity and binocular reading speed best correlating with near distance vision-related quality of life in bilateral nAMD. Ophthalmic Physiol Opt. 2020;40(6):760–769. PMID: 32959926; PMCID: PMC7702040. doi:10.1111/opo.12736
36. Sandberg MA, Gaudio AR. Reading speed of patients with advanced retinitis pigmentosa or choroideremia. Retina. 2006;26(1):80–88. PMID: 16395143. doi:10.1097/00006982-200601000-00013
37. Hohenstein S, Kliegl R. Semantic preview benefit during reading. J Exp Psychol Learn Mem Cogn. 2014;40(1):166–190. PMID: 23895448. doi:10.1037/a0033670
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.