Back to Journals » Journal of Pain Research » Volume 10
Depression, social factors, and pain perception before and after surgery for lumbar and cervical degenerative vertebral disc disease
Authors Jabłońska R , Ślusarz R, Królikowska A, Haor B , Antczak A , Szewczyk M
Received 2 September 2016
Accepted for publication 10 November 2016
Published 4 January 2017 Volume 2017:10 Pages 89—99
DOI https://doi.org/10.2147/JPR.S121328
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Renata Jabłońska,1 Robert Ślusarz,1 Agnieszka Królikowska,1 Beata Haor,1 Anna Antczak,1 Maria Szewczyk2
1Neurological and Neurosurgical Nursing Department; 2Department of Surgery Nursing, Faculty of Health Science, The Ludwik Rydygier Collegium Medicum in Bydgoszcz, The Nicolaus Copernicus University,Toruń, Bydgoszcz, Poland
Objectives: The purpose of this study was to evaluate the effects of psychosocial factors on pain levels and depression, before and after surgical treatment, in patients with degenerative lumbar and cervical vertebral disc disease.
Patients and methods: The study included 188 patients (98 women, 90 men) who were confirmed to have cervical or lumbar degenerative disc disease on magnetic resonance imaging, and who underwent a single microdiscectomy procedure, with no postoperative surgical complications. All patients completed two questionnaires before and after surgery – the Beck Depression Inventory scale (I–IV) and the Visual Analog Scale for pain (0–10). On hospital admission, all patients completed a social and demographic questionnaire. The first pain and depression questionnaire evaluations were performed on the day of hospital admission (n=188); the second on the day of hospital discharge, 7 days after surgery (n=188); and the third was 6 months after surgery (n=140).
Results: Patient ages ranged from 22 to 72 years, and 140 patients had lumbar disc disease (mean age, 42.7±10.99 years) and 44 had cervical disc disease (mean age, 48.9±7.85 years). Before surgery, symptoms of depression were present in 47.3% of the patients (11.7% cervical; 35.6% lumbar), at first postoperative evaluation in 25.1% of patients (7% cervical; 18.1% lumbar), and 6 months following surgery in 31.1% of patients (7.5% cervical; 23.6% lumbar). Patients with cervical disc disease who were unemployed had the highest incidence of depression before and after surgery (p=0.037). Patients with lumbar disc disease who had a primary level of education or work involving standing had the highest incidence of depression before and after surgery (p=0.368).
Conclusion: This study highlighted the association between social and demographic factors, pain perception, and depression that may persist despite surgical treatment for degenerative vertebral disc disease.
Keywords: degenerative disc disease; depression, intervertebral disc, surgery
Introduction
Chronic back pain and chronic neck pain due to degenerative vertebral disc disease are common, with an estimated 90% of the population expected to experience these conditions within their lifetime.1 In approximately 30% of cases, sciatica or brachialgia may be additional symptoms.1 The most common cause of these symptoms is a slipped disc, which results in nerve root compression.1 However, back pain is also reported to be associated with psychogenic disorders, including depressive illness.2
Treatments for cervical and lumbar degenerative disc disease include physiotherapy, pharmacotherapy, and surgical treatment. The approach to surgical intervention is individualized following the patient response to conservative treatment, the extent of any sensory or motor disorders, and patient preferences.3 There may be a relapse of the symptoms of cervical or lumbar pain following conservative and surgical treatment approaches, although these are reported to be less common following surgery.4 Between 3% and 34% of patients who have surgery for degenerative disc disease complain of recurring pain postoperatively.5–7 The reoccurrence of pain following disc surgery may be due to several demographic, social, and psychological factors, including depressive disorders.6,7
There are now several studies that support the role of social and psychological variables, including depression, anxiety, mental state, or patient personality, in affecting the results of spinal surgery,8–10 with depression having a recognized negative association.10,11 For more than a decade, since the publication of the standard text by Block et al,12 it has been known that, in the context of spinal surgery, reactive depression can be both a response to chronic pain and to the subsequent limitations that result from pain and limitation of movement and function, such as loss of employment, social life, and friends. Furthermore, depression is known to precede the onset of back pain, and when this occurs, the results of spinal surgery tend to be less satisfactory.12 In 2004, Curie and Wang13 showed that the severity of depression increased linearly with the severity of back pain experienced by patients with degenerative lumbar disc disease. While it is now accepted that psychological factors need to be evaluated in patients with lumbar degenerative disc disease to minimize unfavorable postoperative results and to improve the recovery prognosis, there are few studies on psychosocial factors and the outcome of surgery for cervical degenerative disc disease.
The purpose of this study was to evaluate the effects of social and demographic factors on pain levels and depression, before and after surgical treatment, in patients with degenerative lumbar and cervical vertebral disc disease.
Methods
Ethical considerations
The research protocol was approved by the bioethics committee of the Collegium Medicum, Nicolaus Copernicus University, Toruń, Poland. All patients included in the study agreed to participate and provided informed consents.
Patients studied and inclusion criteria
The study was conducted at the Department of Neurosurgery at Collegium Medicum University Hospital in Bydgoszcz, Nicolaus Copernicus University (UMK) in Toruń. The study included 188 patients who were diagnosed with cervical or lumbar vertebral degenerative disc disease, confirmed by magnetic resonance imaging, and who qualified for postoperative treatment.
Patients were selected for the study with the following inclusion criteria: 1) diagnosis of cervical or lumbar degenerative vertebral disc disease, made by two independent doctors (a radiologist and a neurosurgeon) based on a clinical examination and spinal magnetic resonance imaging; 2) medical history of a single microdiscectomy procedure, performed after being recruited for the study; and 3) lack of any complications in the postoperative period (eg, disc space infection).
The following criteria excluded patients from the study: 1) diagnosis of a spinal condition other than cervical and lumbar degenerative disc disease; 2) past medical history of more than one microdiscectomy procedure; and 3) postoperative disc space infection.
Assessment questionnaires
Sociodemographic patient admission questionnaire
A questionnaire was developed locally to include the following social and demographic details:
sociodemographic details (age, gender, address, education),
occupation (professional status, working conditions),
disease associations (duration of pain, body mass index [BMI]).
Beck Depression Inventory scale (I–IV)
The Beck Depression Inventory (BDI) scale,14 Polish version,15 was a self-assessment questionnaire used to record the degree of depressive symptoms. The questionnaire included 21 statements concerning the most frequently occurring symptoms of depression, evaluated on a scale of I-IV. Based on the sum of the points from each question, patients were divided into four groups: group I – no depression; group II – mild depression; group III – moderate depression; group IV – severe depression.15
Visual Analog Scale for pain (0–10)
The Visual Analog Scale (VAS)16 was a questionnaire where current pain experienced by the patient was compared with the most severe pain the person could imagine. The outcome was plotted on an 11-grade diagram, in which grade 0 denoted lack of pain, grade 1 indicated the mildest pain, and grade 10 the most severe pain. Patients were divided into four groups based on the intensity of experienced pain: group I, 0 points, no pain; group II, 1–3 points, mild pain; group III, 4–7 points, average pain; group IV, 8–10 points, severe pain.
Timing of assessments
First assessment, preoperative
The first assessment was conducted on the day of hospital admission and included 188 patients. The Sociodemographic Patient Admission Questionnaire, the BDI scale, and the VAS were administered.
Second assessment, day of discharge, 7 days postoperative
The second assessment included 188 patients and was conducted on the day of discharge from hospital, usually 7 days after surgery. The second assessment included the BDI scale and the VAS.
Third assessment, 6 months postoperative
The third assessment included 140 patients at 6 months from surgery. The third assessment included the BDI scale and the VAS.
Statistical analysis
The numerical data from the analysis of the patient questionnaires were collated using charts that allowed the calculation of percentages, mean, and standard deviations. Statistical correlations between two variables were calculated using Spearman’s correlation coefficient. Differences between groups were calculated using the Friedman test, the Kruskal–Wallis test, and the nonparametric Mann–Whitney U test to compare one property across two groups. A null hypothesis (H0) was applied, assuming that there was no difference between the studied groups, and p≤0.05 represented statistical significance. The t-value represented the difference between the sample statistic and the hypothesized sample parameter. All calculations were performed using Microsoft Excel (Microsoft Corporation, Redmond, WA, USA) and software STATISTICA 10 (StatSoft, Tulsa, OK, USA).
Results
Patient characteristics
The study included 188 patients, 98 women and 90 men. Patient ages ranged from 22 to 72 years, and 140 patients had lumbar disc disease (mean age, 42.7±10.99 years) and 48 patients had cervical disc disease (mean age, 48.9±7.85 years). The patients had either dynamic, standing occupation (46/188) or sedentary, static occupations (32/188). The period of time between the first episode of pain and the surgery exceeded 5 years in 82/188 patients. The comparison of results related to sociodemographic factors of patients with cervical vertebral disc disease and lumbar vertebral disc disease are shown in Table 1.
  | Table 1 Demographic data regarding the study participants, N (%) Notes: aMann–Whitney U test. Significant p-values are in bold. Abbreviations: BMI, body mass index; SD, standard deviation. |
Prevalence and severity of depressive disorders
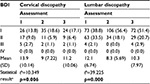
Prior to surgery (first assessment), symptoms of depression were present in 47.3% of patients (11.7% with cervical disc disease and 35.6% with lumbar disc disease).
In the second assessment, at 7 days following surgery, symptoms of depression were present in 25.1% of patients (7% with cervical disc disease and 18.1% with lumbar disc disease).
In the third assessment, at 6 months following surgery, symptoms of depression were present in 31.1% (7.5% with cervical disc disease and 23.6% with lumbar disc disease) (Table 2).
The results from the BDI showed that most patients had symptoms of mild (group II) or moderate (group III) depression (Table 2). For patients with cervical disc disease, the average BDI scale in the first assessment, before surgery was 13.9 points; the average BDI scale in the second assessment, 7 days after surgery was 7 points; and the average BDI scale in the third assessment, 6 months after surgery was 11.2 points.
For patients with lumbar disc disease, the average BDI scale in the first assessment, before surgery was 12.1 points; the average BDI scale in the second assessment, 7 days after surgery was 8.3 points; and the average BDI scale in the third assessment, 6 months after surgery was 10.3 points. The comparative data between the two groups is shown in Table 2.
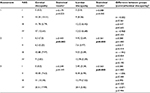
The average number of points using the BDI scale was greater in the preoperative assessments for both groups of patients with cervical and lumbar disc disease. For patients with cervical degenerative disc disease, the highest BDI scale result was found for the patients with a history of unemployment (BDI score: 21.1). For patients with lumbar degenerative disc disease, the highest BDI scale result was found for the patients with a primary-level education (BDI score: 15.3) (Table 3).
Assessments of depressive disorders (multivariate analysis)
For patients with cervical degenerative disc disease, the average values of depressive disorders in the three assessment measurements differed significantly for women (p=0.042), city dwellers (p=0.017), people with vocational training (p=0.031), and the unemployed (p=0.037), when the time period between the first onset of pain and surgery exceeded 5 years (p=0.040), where the last record of pain occurred after more than 5 months from the surgery (p=0.020), and for patients who were overweight, with a BMI >25 kg/m2 (p=0.014) (Table 3).
For patients with lumbar degenerative disc disease, there was a significant correlation between the variables in the three successive assessments (p≤0.05). The factors that varied between the three assessments included age >60 years (p=0.317), primary education (p=0.368), performing sedentary work (p=0.311), or performing standing, static work (p=0.368) (Table 3).
Differences between the analyzed variables in subsequent measurements
Analysis of the results in individual subgroups in relation to one another was performed. In the second assessment (7 days postoperative), with regard to cervical degenerative disc disease, differences between men and women in relation to the variable of performed work (t=2.203; p=0.028) were observed.
For patients with lumbar degenerative disc disease, individual variables were more varied. Statistically significant differences were found within the following variables: gender (t=2.194; p=0.028) (first assessment), age (t=0.199; p=0.018) (second assessment), education (t=0.307; p=0.001) (second assessment), and type of work performed (t=2.396; p=0.017) (third assessment).
The time interval from the last occurrence of pain up to the time of surgery affected the results for each measurement following surgery, 7 days (t=7.443; p=0.024) and 6 months after the surgery (t=6.849; p=0.033) (Table 4).
Association of pain and depressive disorders
Table 5 summarizes the findings from the analysis of the relationship between pain and depressive disorders. For patients with cervical degenerative disc disease, a statistically significant correlation (p=0.002) was found between pain and depression at 1 week following surgery (second assessment). At the second assessment, the greatest score for depression was observed for persons with average pain, or group III on the VAS (0–10), where the mean sum of the points on the BDI scale was 13.88. The lowest mean sum of the points on the BDI scale was 6.5 points and was found for patients with mild pain.
For patients with lumbar degenerative disc disease, a statistically significant correlation (t=0.361; p=0.000) was found between pain and depression at 1 week following surgery (second assessment) and at 6 months following surgery (t=0.563; p=0.000) (third assessment). One week following surgery (second assessment), the most severe depression was observed for patients in group IV of the VAS (12.78 points) and the least severe was observed in patients in group I of the VAS (4.42 points). Six months after surgery (third assessment), the most severe depression was observed for patients in group IV of the VAS (20.4 points) and the least severe was observed in patients in group I of the VAS (3.45 points).
No statistically significant differences were found between the BDI and VAS results of the individual assessments of the pain subgroups in the patients with cervical and lumbar degenerative disc disease (Table 5). No statistically significant differences were found between BDI and VAS results from the subsequent stages of the study (Table 6).
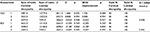  | Table 6 Differences in the assessments of pain (VAS) and depressive disorders (BDI) in the context of clinical diagnosis Abbreviations: VAS, Visual Analog Scale; BDI, Beck Depression Inventory. |
Discussion
This study was done to evaluate the effects of psychosocial factors on pain levels and depression, before and after surgical treatment, in patients with degenerative lumbar and cervical vertebral disc disease. Patients with cervical disc disease who were unemployed had the highest incidence of depression before and after surgery, and patients with lumbar disc disease who had a primary level of education or work involving standing had the highest incidence of depression before and after surgery. The findings of this study support the importance of the psychological and social evaluation of patients who are being considered for surgery for degenerative vertebral disc disease.
Mental health disorders, including depression, are a global health problem and are known to impact on the effects of chronic physical diseases.17–19 The significance of the psychological state of the patient and its contribution to the outcome of chronic physical disease have been supported by the present study and is supported by the findings of Kim et al20 who showed that depression is five times more common in patients diagnosed with degenerative lumbar vertebral disc disease when compared with the normal population. Previous studies have shown that both depression and anxiety prior to surgery for degenerative lumbar disc disease range from 21.5%21 to 48%,22 and after the surgery from 4.1%22 to 79.6%.23 The results of these previous studies are supported by the findings of the present study for patients with lumbar vertebral disc disease. However, in the present study, depression was also evaluated prior to surgery for degenerative cervical disc disease and was found to be present in 11.7% of patients. When viewed together, the findings of this study and previously published studies reflect the severity of the problem of depression for patients with degenerative disc disease, particularly for patients suffering from lumbar disc disease who may have symptoms of depression and pain years after surgery.24
Previous studies have shown that pain is the most significant predictor of depressive illness in patients suffering from degenerative disc disease,25 although patients may rarely discuss their mental health when seeing a neurologist.26 Previous studies have suggested that there may be an association between preoperative depression and both preoperative and postoperative pain severity.27,28 However, Blozik et al,29 who studied the effects of anxiety and depression in patients suffering from cervical pain, reported a significant correlation between the intensity of neck pain and depression. However, a recent study by Falaviga et al30 has shown that patients suffering from chronic depression, even without pain, have a worse response to surgery compared with patients without depression or pain.
In this study, the results of the BDI questionnaire in patients diagnosed with cervical discopathy were statistically significant only between pain groups in the second assessment, which was done postoperatively. However, for patients suffering from lumbar disc disease, the results of the BDI questionnaire in patients diagnosed with lumbar discopathy were statistically significant between pain groups in all postoperative assessments. These findings may be attributed to the fact that a patient who undergoes a surgical procedure tends to expect an immediate improvement in terms of pain symptoms, and where pain persists, feelings of depression may still be relatively great. Also, patients with chronic pain and depression are less willing to undergo physiotherapy, which may delay their recovery.6 Depressive disorders may affect the subjective perception of pain symptoms in chronic bone and joint disease, or even contribute to the chronic nature of the condition.31
In the present study, there were significant gender differences in the severity of depression only in the preoperative assessment of patients diagnosed with lumbar degenerative disc disease. This finding is supported by a recently published community-based study that estimated the 12-month prevalence rates of depression ranged from 2.9% to 3.6% for men and 5.0% to 6.9% for women in the general population.32 The recent study conducted by Löbner et al6 showed that women undergoing disc surgery showed significantly more symptoms of depression in the preoperative period, but no significant differences were found between women and men in the postoperative period. A recent study by Misiak and Snarska33 has shown that men rarely suffer from depression prior to surgery for degenerative lumbar vertebral disc disease. The effect of age on the development of depression for patients undergoing disc surgery remains unclear and requires further study.6,18
This study has shown that city dwellers with lower education were at greater risk of depression in degenerative disc disease, for both cervical and lumbar disease. The study by Misiak and Snarska33 also found that for patients with lumbar disease, depression affected 21.6% of patients who had only primary education and 29.7% with a vocational education and that it also affected 48.6% patients residing in cities with a population greater than 100,000.
This study showed that degenerative vertebral disc disease affected professional individuals with physically active jobs, with 72.9% of patients affected with lumbar disc disease and 58.3% of patients with cervical disc disease. This trend has been previously reported.34 It is possible that in this professional group, the development of depression is due to the deterioration of economic status following sick leave or other effects on their work due to back pain, or due to anxiety regarding returning to work following surgery.29,33 The study by Misiak and Snarska33 showed that depressive disorders affected 16.2% of professionally active people. In the present study, the highest score in the BDI was that for unemployed patients prior to surgery for cervical degenerative disc disease.
This study also showed that depression was more common in overweight patients suffering from degenerative disc disease. This finding has been confirmed by previous studies.24,33 In the study by Misiak and Snarska,33 patients suffering from mild or moderate depression had a higher BMI than those who did not. These findings highlight the importance of educating patients on weight control to reduce the incidence of degenerative disc disease, and also as a preparation for surgery and recovery.35
Limitations
This was a preliminary study that had several limitations. The study was performed at a single center with the data collected and analyzed by the authors, which may have introduced some degree of study bias. Future larger studies are recommended to include larger patient numbers and multiple centers and perform independent data analysis. Although the current study did not examine cases of repeat surgery, previous studies have shown an association between depression and increased incidence of repeat spinal surgery.22,29,36,37 These findings, combined with the findings of the current study, highlight that for both clinical and economic reasons, and to improve preoperative informed consent procedures, patients, and health care systems, would benefit from implementing preoperative psychosocial assessment of patients with degenerative vertebral disc disease.38,39
Conclusion
In conclusion, this study has highlighted the association between social and demographic factors, pain perception, and depression that may persist despite surgical treatment for degenerative vertebral disc disease. The findings of this study also highlight the importance of the psychological and social evaluation of patients who are being considered for vertebral disc surgery.
Acknowledgments
The authors thank staff and colleagues at the The Ludwik Rydygier Collegium Medicum in Bydgoszcz, The Nicolaus Copernicus University in Toruń, Bydgoszcz, Poland, and all the patients who participated in this study.
Disclosure
The authors report no conflicts of interests in this work.
References
Graczyk D, Jankowski R, Misterska E, Głowacki M, Żukiel R, Kowalska A. Patient satisfaction with nursing after surgery due to cervical or lumbar discopathy. Med Sci Monit. 2013;28(19):892–902. | ||
Bener A, Verjee M, Dafeeah E, et al. Psychological factors: anxiety, depression, and somatization symptoms in low back pain patients. J Pain Res. 2013;6:95–101. | ||
Kleinig TJ, Brophy BP, Maher CG. Practical neurology – 3: back pain and leg weakness. Med J Aust. 2011;195(8):454–457. | ||
Taher F, Essig D, Lebl DR, et al. Lumbar degenerative disc disease: current and future concepts of diagnosis and management. Adv Orthop. 2012;2012:970752. | ||
Parker SL, Mendenhall SK, Godil SS, et al. Incidence of low back pain after lumbar discectomy for herniated disc and its effect on patient-reported outcomes. Clin Orthop Relat Res. 2015;473(6):1988–1999. | ||
Löbner M, Luppa M, Matschinger H, et al. The course of depression and anxiety in patients undergoing disc surgery: a longitudinal observational study. J Psychosom Res. 2012;72:185–194. | ||
Pollock R, Lakkol S, Budithi C, Bhatia C, Krishna M. Effect of psychological status on outcome of posterior lumbar interbody fusion surgery. Asian Spine J. 2012;6(3):178–182. | ||
Alodaibi FA, Minick KI, Fritz JM. Do preoperative fear avoidance model factors predict outcomes after lumbar disc herniation surgery? A systematic review. Chiropr Man Therap. 2013;21(1):40. | ||
Young AK, Young BK, Riley LH, Skolasky RL. Assessment of presurgical psychological screening in patients undergoing spine surgery: use and clinical impact. J Spinal Disord Tech. 2014;27(2):76–79. | ||
Misterska E, Jankowski R, Głowacki M. Chronic pain coping styles in patients with herniated lumbar discs and coexisting spondylotic changes treated surgically: considering clinical pain characteristics, degenerative changes, disability, mood disturbances, and beliefs about pain control. Med Sci Monit. 2013;27(19):1211–1220. | ||
Hong JH, Lee MJ, Jung SW, Lee SY. Does spinal stenosis correlate with MRI findings and pain, psychologic factor and quality of life? Korean J Anesthesiol. 2015;68(5):481–487. | ||
Block AR, Gatchel RJ, Deardorff W, Guyer RD. The Psychology of Spine Surgery. Washington, DC: American Psychological Association; 2003. | ||
Currie SR, Wang J. Chronic back pain and major depression in the general Canadian population. Pain. 2004;107(1–2):54–60. | ||
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psych. 1961;4:53–63. | ||
Parnowski T, Jernajczyk W. Beck’s depression inventory in the rating of mood in normal subjects and in patients with affective disturbances. Psychiatr Pol. 1977;11(4):417–421. | ||
Manniche C, Asmussen K, Lauritens B, Vinterberg H, Kreiner S, Jordan A. Low back pain rating scale: validation of a tool for assessment of low back pain. Pain. 1994;57(3):317–326. | ||
Levinson D, Lakoma MD, Petukhova M, et al. Associations of serious mental illness with earnings: results from the WHO World Mental Health surveys. Br J Psychiatry. 2010;197(2):114–121. | ||
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. | ||
Kessler RC, Bromet EJ. The epidemiology of depression across cultures. Annu Rev Public Health. 2013;34:119–138. | ||
Kim TS, Pae CU, Hong CK, et al. Interrelationships among pain, disability, and psychological factors in young Korean conscripts with lumbar disc herniation. Mil Med. 2006;171(11):1113–1116. | ||
Guilfoyle MR, Granesan D, Seeley H, Laing RJ. Prospective study of outcome in lumbar discectomy. Br J Neurosurg. 2007;21(4):389–395. | ||
Sinikallio S, Lehto SM, Aalto T, Airaksinen O, Kröger H, Viinamäki H. Depressive symptoms during rehabilitation period predict poor outcome of lumbar spinal stenosis surgery: a two-year perspective. BMC Musculoskelet Disord. 2010;6(11):152. | ||
Mayer TG, Anagnostis C, Gatchel RJ, Evans T. Impact of functional restoration after anterior cervical fusion on chronic disability in work-related neck pain. Spine J. 2002;2(4):267–273. | ||
Wang H, Zhang D, Ma L, Shen Y, Ding W. Factors predicting patient dissatisfaction 2 years after discectomy for lumbar disc herniation in a Chinese older cohort: a prospective study of 843 cases at a single institution. Medicine (Baltimore). 2015;94(40):e1584. | ||
Lebow R, Parker SL, Adogwa O, et al. Microdiscectomy improves pain-associated depression, somatic anxiety, and mental wellbeing in patients with herniated lumbar disc. Neurosurgery. 2012;70(2):306–311. | ||
Wrodycka B, Chmielewski H, Gruszczyński W, Zytkowski A, Chudzik W. Masked (atypical) depression in patients with back pain syndrome in outpatient neurological care. Pol Merkur Lekarski. 2006;21(121):38–40. | ||
Li S, Qi M, Yuan W, Chen H. The impact of the depression and anxiety on prognosis of cervical total disc replacement. Spine. 2015;40(5):E266–E271. | ||
Zieger M, Schwarz R, König HH, Härter M, Riedel-Heller SG. Depression and anxiety in patients undergoing herniated disc surgery: relevant but under researched – a systematic review. Cen Eur Neurosurg. 2010;71(1):26–34. | ||
Blozik E, Lapinskaya D, Herrmann-Lingen C, et al. Depression and anxiety as major determinants of neck pain: a cross-sectional study in general practice. BMC Musculoskelet Disord. 2009;26(10):13. | ||
Falavigna A, Righesso O, Teles AR, et al. Responsiveness of depression and its influence on surgical outcomes of lumbar degenerative diseases. Eur J Orthop Surg Traumatol. 2015;25(Suppl 1):S35–S41. | ||
von der Hoeh NH, Voelker A, Gulow J, Uhle U, Przkora R, Heyde CE. Impact of a multidisciplinary pain program for the management of chronic low back pain in patients undergoing spine surgery and primary total hip replacement: a retrospective cohort study. Patient Saf Surg. 2014;8(8):34. | ||
Gagne S, Vasiliadis HM, Preville M. Gender differences in general and specialty outpatient mental health service use for depression. BMC Psychiatry. 2014;9(14):135. | ||
Misiak B, Snarska K. Quality of life of patients with back pain. J Neurolog Neurosurg Nurs. 2014;3(3):107–115. | ||
Saleem S, Aslam HM, Rehmani MAK, Raees A, Alvi AA, Ashraf J. Lumbar disc degenerative disease: disc degeneration symptoms and magnetic resonance imaging findings. Asian Spine J. 2013;7(4):322–334. | ||
Samartzis D, Karppinen J, Chan D, Luk KD, Cheung KM. The association of lumbar intervertebral disc degeneration on magnetic resonance imaging with body mass index in overweight and obese adults: a population-based study. Arthritis Rheum. 2012;64(5):1488–1496. | ||
Adogwa O, Parker SL, Shau DN, et al. Preoperative Zung Depression Scale predicts outcome after revision lumbar surgery for adjacent segment disease, recurrent stenosis, and pseudarthrosis. Spine J. 2012;12(3):179–185. | ||
Pakarinen M, Vanhanen S, Sinikallio S, et al. Depressive burden is associated with a poorer surgical outcome among lumbar spinal stenosis patients: a 5-year follow-up study. Spine J. 2014;14(10):2392–2396. | ||
Prina A, Cosco TD, Dening T, Beekman A, Brayne C, Huisman M. The association between depressive symptoms in the community, non-psychiatric hospital admission and hospital outcomes: a systematic review. J Psychosom Res. 2015;78(1):25–33. | ||
Ghoneim MM, O’Hara MW. Depression and postoperative complications: an overview. BMC Surg. 2016;16:5. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.