Back to Journals » Clinical, Cosmetic and Investigational Dentistry » Volume 6
Dental extraction in patients on warfarin treatment
Authors Abdullah W, Khalil H
Received 31 May 2014
Accepted for publication 25 June 2014
Published 19 August 2014 Volume 2014:6 Pages 65—69
DOI https://doi.org/10.2147/CCIDE.S68641
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Walid Ahmed Abdullah,1,2 Hesham Khalil1
1Department of Oral and Maxillofacial Surgery, College of Dentistry, King Saud University, Riyadh, Kingdom of Saudi Arabia; 2Department of Oral and Maxillofacial Surgery, College of Dentistry, Mansoura University, Mansoura, Egypt
Background: Warfarin is one of the most common oral anticoagulants used to prevent thromboembolic episodes. The benefits of discontinuation of this drug before simple surgical procedures are not clear and this approach could be associated with complications. The aim of this study was to evaluate the risk of bleeding in a series of 35 patients (in cases where the international normalized ratio [INR] is less than 4) following simple tooth extraction without modification of the warfarin dose given to patients.
Methods: Thirty-five patients taking warfarin who had been referred to the Oral and Maxillofacial Department, College of Dentistry, King Saud University, for dental extractions were included in the study. Exclusion criteria included patients with an INR of ≥4 or with a history of liver disease or coagulopathies. No alteration was made in warfarin dose, and the CoaguChek System was used to identify the INR on the same day of dental extraction. Bleeding from the extraction site was evaluated and recorded immediately after extraction until the second day.
Results: A total of 35 patients (16 women and 19 men) aged between 38 and 57 years (mean =48.7) were included in the present study. All patients underwent simple one-tooth extraction while undergoing warfarin treatment. Oozing, considered mild bleeding and which did not need intervention was seen in 88.6% of patients. Moderate bleeding occurred in 11.4% of all cases. The INR of the patients ranged from 2.00 to 3.50, with 77.2% of patients having INR between 2.0 and 2.5 on the day of extraction. No severe bleeding which needed hospital management was encountered after any of the extractions. The patients who suffered moderate bleeding were returned to the clinic where they received local treatment measures to control bleeding. Moderate bleeding occurred only in four patients, where three had INR between 3.1 and 3.5, and one with INR less than 3.
Conclusion: In the present study, we have shown that simple tooth extraction in patients on warfarin treatment can be performed safely without high risk of bleeding, providing that the INR is equal or less than 3.5 on the day of extraction. A close follow-up and monitoring of patients taking warfarin is mandatory after dental extraction.
Keywords: tooth extraction, bleeding, INR
Introduction
Warfarin, which acts by antagonizing the effect of vitamin K, is one of the most commonly used oral anticoagulants. The drug can be absorbed completely and reaches its peak in 1 hour after ingestion.1 Albumin is bound to circulating warfarin, and the half-life of warfarin is approximately 36 hours.2 The liver metabolizes warfarin into inactive compounds, which are then excreted, mainly into the urine. Warfarin has been used to decrease the thromboembolism in millions of patients worldwide. Its effect is measured by international normalized ratio (INR), which is a measure of patient’s prothrombin time divided by the laboratory control value of prothrombin time.3 The level of INR suitable for the patient depends on the condition of the patient. The recommended INR level according to the American College of Chest Physicians is between 2.0 and 3.0 for most conditions;4 however, patients using prosthetic heart valves may require higher level of INR.
Anticoagulant drugs may put the patient under a risk of bleeding following surgical procedures, and as a result, surgeons are always worried about bleeding in patients undergoing warfarin treatment. The reported percentage of major bleeding which can be life-threatening in patients taking warfarin ranges from 0.4 to 7.2%, while for minor bleeding, the percentage is approximately 15.4.5 It has been found that the annual rate of major bleeding in case of patients with atrial fibrillation who receive warfarin treatment is between 0.4 and 2.6. Such risk of bleeding has been found to be related to many factors, including the intensity of the anticoagulation and in some patients, related factors including age, hypertension, severe cardiac disease, and renal insufficiency. The percentage of intracranial hemorrhage in the first 3 months after treatment with warfarin was found to be 1.48% with annual percentage of 0.65%;6 this risk was, however, considered unlikely.7 The percentage of bleeding in sites outside the central nervous system was reported to be 7.3%.8 The risk of postsurgical bleeding in patients taking warfarin was reported to be very low in cases of dental extractions, providing that the INR was within an acceptable range; when major bleeding does however occur, it can be uncontrollable with local measures and need hospital management.9–11
A range of strategies has been used to manage patients undergoing warfarin treatment before surgical procedures. These include stopping warfarin 2–3 days before the procedure, reducing warfarin dose, continuing warfarin, and measuring the INR and replacing warfarin with low molecular weight heparin (anticoagulation bridge therapy) in an outpatient clinic or hospital setting.12,13 Heparin is used in anticoagulation bridge therapy, as it has a faster onset and offset action compared with warfarin.12 Many reports stated that patients requiring a minor dental procedure and having an INR of up to 4.0 are able to continue warfarin without any dose adjustment.3,14,15 It has, however, been debated whether stopping warfarin can increase the risk of cerebrovascular accidents (CVA). Suspension of warfarin treatment may be responsible for the development of CVA in patients undergoing dental extractions.16 Assessing both risks and benefits is very important in patients receiving warfarin, and a very close communication and consultation with the patient’s physician regarding the best management is critical.
In this study, we aimed to investigate the risk of bleeding after simple dental extraction in patients taking warfarin regularly and whose INR is below 4.0.
Patients and methods
All patients included in this study were undergoing warfarin treatment and were referred to the Department of Oral and Maxillofacial Surgery (OMF) for simple dental extraction. A full patient’s history was taken from all patients in accordance with the patient’s file at the OMF department, which includes a whole system review and detailed patient history and examination. Exclusion criteria included any patient with INR >4, any history of liver disease, or any other coagulopathies, and any patient who refused to sign the consent or otherwise refused to participate in the study after discussing possible complications related to the procedure was omitted from the study. All patients were purely on warfarin treatment, and no patients taking other anticoagulants of antiplatelet drugs such as aspirin were included in the study. The CoaguChek System (Roche Diagnostics, USA) was used to identify the INR on the same day of dental extraction. Each patient was subjected to a simple one-tooth extraction. No local or systemic hemostatic measures were used in these patients, except that a gauze pressure pack was applied on the extraction site for 30 minutes after extraction. Bleeding from the extraction site was evaluated and recorded immediately after extraction until the second day after extraction. Little oozing of blood from the extraction socket which is commonly seen after dental extraction was considered mild bleeding. When bleeding persisted on the second day and required the patient to come back and be managed by local measures, the outcome was considered to be moderate bleeding. In this case, a local hemostatic agent was employed, namely oxidized cellulose (Surgicel; Johnson and Johnson), with suturing using 3/0 Vicryl. Any bleeding that needed hospitalization was considered severe. Patients were strictly advised to contact the clinic at any time post-extraction in case of any complications related to the extraction.
Data were analyzed by descriptive analysis using SPSS program V.17. A Student’s t-test was used to compare the results, and P-value of less than 0.05 was considered significant.
Results
A total of 35 patients (16 women and 19 men) aged between 38 and 57 years (mean =48.7) were included in the present study. All patients underwent simple one-tooth extraction while they were undergoing warfarin treatment. The incidence of postoperative bleeding after dental extraction in patients recruited in this study is shown in Table 1. Oozing from the extraction socket which was considered mild bleeding and did not need intervention and management by gauze pressure at home was seen in 88.6% of patients. Moderate bleeding occurred in 11.4% of all cases. There was no significant difference in bleeding between males and females (P>0.05). The INR of the patients ranged from 2.00 to 3.50, with 77.2% of patients having INR between 2.0 and 2.5 on the day of extraction (Table 2). No severe bleeding which needed hospital management was encountered following any of the extractions. The patients showing moderate bleeding were returned to the clinic where they underwent local measures to control bleeding. Moderate bleeding occurred in only four patients, where three had an INR between 3.1 and 3.5, and one had an INR of less than 3 (Table 3).
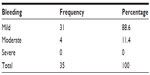  | Table 1 Bleeding after simple tooth extraction in patients on warfarin treatment |
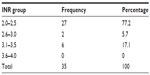  | Table 2 The INR range |
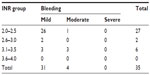  | Table 3 The INR range and post-extraction bleeding |
Discussion
Patients who receive warfarin management and undergo surgical procedure may be at risk of bleeding, and as a result, a range of guidelines exist relating to the management of such patients prior to surgical intervention. The American College of Chest Physicians suggests that patients should stop warfarin 5 days before any surgical intervention, and also that warfarin should be temporarily replaced with low molecular weight heparin as a bridge therapy.5,12 The American Heart Association, in contrast, suggests reducing the INR to a range between 2.0 and 2.5, with strict INR monitoring.17 Teeth extraction is a procedure where bleeding can be encountered. The difficulty of the extraction itself or complications related to the procedure may affect the risk of bleeding in at-risk patients. Simple tooth extraction involves gentle forceps manipulation of the tooth with minimal trauma to the tissue. A patient undergoing warfarin treatment should be carefully evaluated prior to such a dental procedure. There is always controversy related to the modification of warfarin treatment prior to dental procedure.18,19 The rebound hypercoagulability after suddenly stopping warfarin treatment has been reported in the literature.20
The results of the present study suggests that no significant bleeding occurs following simple tooth extraction in patients on warfarin treatment, and these patients can continue with their regular medication, providing that the INR is less than 3.50. A total of four (11.4%) patients experienced moderate bleeding after the tooth extraction. The bleeding was managed by local measures using local hemostatic agent; for simple tooth extraction, modification of warfarin treatment is therefore not necessary. Such recommendation is supporting the report of Aframian et al1 regarding single-tooth extraction and reduces the risk of developing CVA in case of stopping the drug a few days before the extraction. Bacci et al21 have shown that teeth extraction can be done safely in patients taking anticoagulants without any modification of the anticoagulation therapy, results which again agree with findings reported here. Although a number of similar recommendations can be found in the literature, many surgeons continue not to follow the current guidelines, essentially because they are concerned about the risk of bleeding.22 Although there are no well documented case reports of serious bleeding following dental surgery,21 invasive surgical procedures should be always discussed carefully with a patient’s physician. It has been shown that patients who have comorbidities such as diabetes, liver disease, and chronic renal failure need to bring their INR within a narrower safety range, with upper limit of between 2.5 and 2.8 to avoid serious bleeding complications during oral surgical procedures.23
The INR reading should be obtained at the same day of surgical procedure. This was obtained by the help of the CoaguChek system, which can give the value of INR within seconds. In the present study, all patients undergoing warfarin treatment having complicated medical history were automatically excluded. Since the presence of underlying disease such as liver or coagulopathies can increase the risk of bleeding in patients on warfarin treatment,23 it is advisable that any patient with complicated medical history and warfarin treatment should be treated under special conditions. The risk of bleeding in medically compromised patients who are taking warfarin could be due to changes in the physiologic process of hemostasis, epithelialization, and maturation of wounds following dental surgery.8,23
Various local measures to control bleeding in patients on warfarin treatment are available, including local hemostatic agents, suturing, and tranexamic acid.14,15 In the present study, no local measures were used immediately after tooth extraction, except that pressure was applied to the extraction socket using a piece of gauze. The use of such local measures may mask the immediate bleeding tendency in the study, and they were used only when moderate bleeding was encountered. We suggest the use of local hemostatic measures immediately after performing dental extraction, as it has been shown these minimize the risk of bleeding.15,24–26 Use of the INR therapeutic range is very important for preventing patient thromboembolic accidents; altering this range may clearly adversely affect the patient. The protocols described in the literature to manage patients on warfarin treatment prior to dental treatment vary widely. Many studies suggest that there is a very small risk of bleeding in only very few patients following dental procedures when the INR range is between 2 and 4.13,18,27 It has been also reported that there is no significant difference in bleeding tendency in patients whose warfarin treatment is discontinued prior to the treatment when compared with those patients who continue on warfarin.28 When bleeding occurred in these patients, it was easily managed by local hemostatic measures. The work reported in this study supports recommendations suggesting that warfarin discontinuation is not necessary for dental extraction when INR is monitored and when no extensive surgical procedure is required.
It has been shown elsewhere that the INR range is not correlated to the bleeding tendency.29 In our study, three of our patients had moderate bleeding when their INR was above 3. Only one patient with INR below 3 had moderate bleeding after simple extraction. This indicates that INR is not the only factor that estimates the risk of bleeding and that other factors related to the patient or the procedure may influence such risk. Therefore, in non-complicated medical history patients who are on warfarin treatment, simple tooth extraction can be done with low risk of post-extraction bleeding if the INR is below 3.5. Local hemostatic measures also help in reducing the risk of bleeding in these patients. We conclude by suggesting that further studies, employing larger sample size, are needed to consolidate such findings.
Conclusion
Since warfarin carries the risk of bleeding, it is very important to evaluate the need for dose modification during any surgical intervention when all patients should be assessed carefully. In the present study, we have shown that simple teeth extraction in patients on warfarin treatment can be performed safely without high risk of bleeding but providing that the INR is equal or less than 3.5 at the day of extraction. A close follow-up and monitoring of patients taking warfarin is mandatory after dental extraction.
Disclosure
The authors report no conflicts of interest in this work.
References
Aframian, DJ, Lalla RV, Peterson DE. Management of dental patients taking common hemostasis-altering medications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103 Suppl:S45–S11. | |
Karsli ED, Erdogan O, Esen E, Acarturk E. Comparison of the effects of warfarin and heparin on bleeding caused by dental extraction: a clinical study. J Oral Maxillofac Surg. 2011;69:2500–2507. | |
Salam S, Yusuf H, Milosevic A. Bleeding after dental extractions in patients taking warfarin. Br J Oral Maxillofac Surg. 2007;45:463–466. | |
Hirsh J, Fuster V, Ansell J, Halperin JL. American Heart Association/American College of Cardiology foundation guide to warfarin therapy. J Am Coll Cardiol. 2003;41:1633–1652. | |
Snipelisky D, Kusumoto F. Current strategies to minimize the bleeding risk of warfarin. J Blood Med. 2013;4:89–99. | |
Linkins LA, Choi PT, Douketis JD. Clinical impact of bleeding in patients taking oral anticoagulant therapy for venous thromboembolism: a meta-analysis. Ann Intern Med. 2003;139:893–900. | |
Go AS, Hylek EM, Chang Y, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trials translate into clinical practice? JAMA. 2003;290:2685–2692. | |
DiMarco JP, Flaker G, Waldo AL, et al. Factors affecting bleeding risk during anticoagulant therapy in patients with atrial fibrillation: observations from the atrial fibrillation follow-up investigation of rhythm management (AFFIRM) study. Am Heart J. 2005;149:650–656. | |
Devani P, Lavery KM, Howell CJ. Dental extractions in patients on warfarin: is alteration of anticoagulant regime necessary? Br J Oral Maxillofac Surg. 1998;36:107–111. | |
Dewan K, Bishop K, Muthukrishnan A. Management of patients on warfarin by general dental practitioners in South West Wales: continuing the audit cycle. Br Dent J. 2009;206:E8; discussion 214–215. | |
Wahl MJ. Dental surgery in anticoagulated patients. Arch Intern Med. 1998;158:1610–1616. | |
Jaffer AK, Brotman DJ, Chukwumerije N. When patients on warfarin need surgery. Cleve Clin J Med. 2003;70:973–984. | |
Hong C, Napenas JJ, Brennan M, Furney S, Lockhart P. Risk of postoperative bleeding after dental procedures in patients on warfarin: a retrospective study. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114:464–468. | |
Nematullah A, Alabousi A, Blanas N, Douketis JD, Sutherland SE. Dental surgery for patients on anticoagulant therapy with warfarin: a systematic review and meta-analysis. Tex Dent J. 2009;126:1183–1193. | |
Randall C. Surgical management of the primary care dental patient on warfarin. Dent Update. 2005;32:414–420, 423. | |
Stiefelhagen P. [Stroke after tooth extraction]. MMW Fortschr Med. 2009;151:17. German. | |
Brewer AK. Continuing warfarin therapy does not increased risk of bleeding for patients undergoing minor dental procedures. Evid Based Dent. 2009;10:52. | |
Lalla RV, Peterson DE, Aframian DJ. Should warfarin be discontinued before a dental extraction? Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:149–150. | |
Balevi B. Should warfarin be discontinued before a dental extraction? A decision-tree analysis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;110:691–697. | |
Genewein U, Haeberli A, Straub PW, Beer JH. Rebound after cessation of oral anticoagulant therapy: the biochemical evidence. Br J Haematol. 1996;92:479–485. | |
Bacci C, Maglione M, Favero L, et al. Management of dental extraction in patients undergoing anticoagulant treatment. Results from a large, multicentre, prospective, case-control study. Thromb Haemost. 2010;104:972–975. | |
Troulis MJ, Head TW, Leclerc JR. Dental extractions in patients on an oral anticoagulant: a survey of practices in North America. J Oral Maxillofac Surg. 1998;56:914–917. | |
Cocero N, Mozzati M, Ambrogio M, Bisi M, Morello M, Bergamasco L. Bleeding rate during oral surgery of oral anticoagulant therapy patients with associated systemic pathologic entities: a prospective study of more than 500 extractions. J Oral Maxillofac Surg. 2014;72:858–867. | |
Barrett D. Management of dental patients on warfarin therapy in a primary care setting. Dent Update. 2004;31:618. | |
Carter G, Goss A, Lloyd J, Tocchetti R. Tranexamic acid mouthwash versus autologous fibrin glue in patients taking warfarin undergoing dental extractions: a randomized prospective clinical study. J Oral Maxillofac Surg. 2003;61:1432–1435. | |
Carter G, Goss AN, Lloyd J, Tocchetti R. Current concepts of the management of dental extractions for patients taking warfarin. Aust Dent J. 2003;48:89–96. | |
Wahl MJ, Pinto A, Lalla RV. Interruption of warfarin anticoagulation for dental surgery. Chest. 2013;144:1424. | |
Miller CS. Evidence does not support the discontinuation of warfarin before a dental extraction. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;113:148–149. | |
Campbell JH, Alvarado F, Murray RA. Anticoagulation and minor oral surgery: should the anticoagulation regimen be altered? J Oral Maxillofac Surg. 2000;58:131–135. |
 © 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2014 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
