Back to Journals » Clinical Interventions in Aging » Volume 18
Delirium After Surgery for Proximal Femoral Fractures in the Frail Elderly Patient: Risk Factors and Clinical Outcomes
Authors de Haan E , van Rijckevorsel VA , Bod P, Roukema GR, de Jong L
Received 18 October 2022
Accepted for publication 24 January 2023
Published 13 February 2023 Volume 2023:18 Pages 193—203
DOI https://doi.org/10.2147/CIA.S390906
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Eveline de Haan,1,2 Veronique AJIM van Rijckevorsel,1 Pepijn Bod,1 Gert R Roukema,1 Louis de Jong1 On behalf of Dutch Hip Fracture Registry Collaboration (DHFR)
1Surgery Department, Maasstad Hospital, Rotterdam, the Netherlands; 2Surgery Department, Franciscus Hospital, Rotterdam, the Netherlands
Correspondence: Eveline de Haan, Tel +31654922535, Email [email protected]
Purpose: The primary aim of this study was to identify risk factors for delirium after hip fracture surgery. The secondary purpose of this study was to verify peri-operative clinical outcomes, adverse events and mortality rates in delirium patients after hip fracture surgery.
Patients and Methods: A prospective hip fracture database was used to obtain data. In total, 2051 patients older than 70 years undergoing a hip fracture surgery between 01– 01-2018 and 01– 01-2021 were included. A delirium was diagnosed by a geriatrician based on the DSM-V criteria.
Results: The results showed that 16% developed a delirium during hospital admission. Multivariable analysis showed that male gender (OR: 1.99, p< 0.001), age (OR: 1.06, p< 0.001), dementia (OR: 1.66, p=0.001), Parkinson’s disease (OR: 2.32, p=0.001), Δhaemoglobin loss (OR: 1.19, p=0.022), pneumonia (OR: 3.86, p< 0.001), urinary tract infection (UTI) (OR: 1.97, p=0.001) and wound infection (OR: 3.02, p=0.007) were significant independent prognostic risk factors for the development of a delirium after hip surgery. The median length in-hospital stay was longer in patients with a delirium (9 days) vs patients without a delirium (6 days) (p< 0.001). The 30-day mortality was 7% (with delirium 16% vs with no delirium 6% (p< 0.001)).
Conclusion: Significant independent prognostic factors associated with delirium after hip surgery were male gender, age, dementia, Parkinson’s disease, Δhaemoglobin loss, pneumonia, UTI and wound infection.
Keywords: geriatric patients, hip fractures, delirium, risk factors, clinical outcomes
Introduction
In 2050, the population aged over 70 is expected to be doubled due to an increasing life expectancy.1 In geriatric patients, falling incidents are frequently causing hip fractures.2 During admission for a hip fracture, delirium is the most frequent complication with incidence rates between 19% and 39%3–13 Delirium during admission is associated with an increased level of impaired cognitive and less functional recovery, with an extended admission duration, higher treatment costs and increased mortality rates.4,5,12,14–16 To enable preventive measures against delirium, determination of risk factors for delirium during hip fracture treatment is needed. Previous literature report risk factors such as age, body mass index (BMI), American Society of Anesthesiologists (ASA) classification, cognitive impairment, Parkinson’s disease, polypharmacy, living in an institution and acute admission.3,6,7,9,11,17–20 Previous research has been based on relatively small populations. Furthermore, a limited number of baseline and perioperative factors were analyzed in preceding articles.
The primary aim of this study was to identify new risk factors and validate earlier reported risk factors for delirium after hip fracture surgery. Furthermore, this study aimed to verify peri-operative clinical outcomes, adverse events and mortality rates in delirium patients after hip fracture surgery.
Patients and Methods
The STROBE guidelines were used to ensure the reporting of this study.
Study Design and Patient Selection
Baseline characteristics and clinical outcomes were retrospectively acquired from a prospective registry database from two level II trauma teaching hospitals in the Netherlands. The database is a hospital initiative in which all hip fractures from the two hospitals were added to collect data to improve hip fracture care. Patients who underwent surgical treatment for proximal femoral fractures (ie, femoral neck fracture, trochanteric fracture or sub-trochanteric fracture) between 01–01-2018 and 01–01-2021 were screened for eligibility. Patients older than 70 years receiving hip hemiarthroplasty, total hip arthroplasty, cannulated screw fixation, dynamic hip screw, femoral neck system and gamma-nail were included in the study (n=2051) (Figure 1). Follow-up duration was at least 3 months, in which patients were approached by phone or were seen at the outpatient clinic. All operations were performed in a laminar flow theater. Usual antibiotic prophylaxis, 1–3g cefazolin (Kefzol), was given prior to surgery.
 |
Figure 1 Flow chart of included patients. |
Risk Factors for Delirium
Baseline characteristics of all included patients were collected to evaluate the risk factors for delirium after hip fracture surgery. Information about the living situation prior to hospital admission was obtained. The nutritional status was expressed in BMI and Short Nutritional Assessment Questionnaire for Residential Care (SNAQ) score. The Katz Index of Independence in activities of daily living (KATZ-ALD) was used as measurement to define the functional status of a patient. The Nottingham hip fracture score (NHFS) and the Charlson Comorbidity Index (CCI) were used as frailty prediction scores, in which patient’s comorbidities and general status are combined.21–23
Perioperative Risk Factors
We selected perioperative variables described in previous literature as risk factors for the development of delirium after hip fracture surgery.3,6,7,9,11,17–20 Risk factors were time to surgery, moment of the week (week or weekend), moment of the day (day or nighttime), duration of the surgery, estimated blood loss, complications and reoperations. The type of anesthesia (general or local) and the ASA score were also collected.
Delirium
Patients were admitted to the geriatric trauma unit (GTU) or the orthopedic trauma ward. Prior to surgery, the geriatrician was consulted as usual care for all patients with a hip fracture. Patients with dementia and patients with a high suspicion of development of a delirium by the geriatrician were admitted at the GTU. In general, frail elderly patients will be admitted to the GTU because of a higher a priori chance on delirium, compared to cognitive and functional “healthy” patients who were admitted to the orthopedic trauma ward.
The Delirium Observation Screening Scale (DOSS) was used to screen patients for delirium, which was scored by trained nurses. Three or more points on the DOSS were considered as highly indicative of delirium. The geriatrician confirmed the diagnosis delirium based on the DSM-V.
Clinical Outcomes, Adverse Events and Mortality
The secondary aim of this study was to verify the effect of delirium on several peri-operative clinical outcomes, complications, the length of in-hospital stay, and mortality rates (30 days, 1 year).
Statistical Analysis
Categorical variables are presented as frequencies and percentages. Continuous variables are presented as mean (±SD) in case of a normal distribution or as median (IQR) in case of non-normal distribution. Associations between potential risk factors and the primary outcome delirium were analyzed by univariable logistic regression. To analyze the association with delirium, significant associations observed in univariable analysis and significant variables reported in previous literature were included in the multivariable model. Fixed variables in the multivariable model were CCI and type of admission ward (GTU or orthopedic trauma ward). Subsequently, backward elimination was performed until all remaining variables reached a P-value <0.10. Stata version 14.0 was used to perform statistical analyses (StataCorp, College Station, TX, USA). All statistical tests were two-sided with a significance level of P<0.05. Mortality rates were estimated and displayed using the Kaplan–Meier estimator.
Ethics
The local ethics committee approved the study protocol (L2017044, Toetsingscommissie Wetenschappelijk Onderzoek Rotterdam (TWOR), Rotterdam). The local ethics committee established that patients consent to review their medical records was not required because of no change in standard practice of care and the high percentage of cognitive dysfunction. Patient data were stored anonymously. All the protocols were performed in compliance with the Declaration of Helsinki. For this study, no external funding was used.
Results
Risk and Prognostic Baseline Risk Factors
In total, 2051 patients were analysed of which 326 patients (16%) developed a delirium during hospital admission. In Table 1, the results of the univariable analysis of the risk and prognostic baseline factors are presented. The risk at the development of a delirium is significantly increased by the gender male (OR: 1.66, 1.30–2.11, p<0.001), age (85 vs 79 years, OR: 1.07, 1.05–1.09, p<0.001), nursing home (27% vs 18%, OR: 1.68, 1.27–2.22, p<0.001), use of a walking aids (OR: 1.97, 1.55–2.51, p<0.001), SNAQ score ≥3 (20% vs 15%, OR: 1.48, 1.07–2.03, p=0.016), higher KATZ-ADL score (2 vs 0, OR: 1.21, 1.15–1.27, p<0.001), higher NHFS (5 vs 4, OR: 1.51, 1.39–1.65, p<0.001), higher CCI (5.4 vs 5.7, OR: 1.21, 1.13–1.28, p<0.001), ASA score 3 and 4 (OR: 2.21, 1.65–2.96, p<0.001), medical history of cardiovascular disease (69% vs 60%, OR: 1.47, 1.14–1.89, p=0.003), dementia (35% vs 18%, OR: 2.35, 1.81–3.04, p<0.001), myocardial infarction (12% vs 8%, OR: 1.52, 1.04–2.22, p=0.032), Parkinson’s disease (10% vs 4%, OR: 2.69, 1.74–4.18, p<0.001), transient ischemic attack (TIA) (12% vs 7%, OR: 1.84, 1.26–2.68, p=0.002), decreased glomerular filtration rate (GFR) (61 vs 71, OR: 0.99, 0.98–0.99, p<0.001), decreased haemoglobin (Hb) level (7,7 vs 7.9, OR: 0.87, 0.78–0.98, p=0.019) and polypharmacy (>4 medications) (65% vs 54%, OR: 1.56, 1.22–1.99, p<0.001).
 |
Table 1 Univariable Analyses of Risk and Prognostic Baseline Factors |
Risk and Prognostic Perioperative Risk Factors
Results of the univariable analysis of the risk and prognostic perioperative factors are presented in Table 2. The factors that significantly increase the risk of delirium are: time to surgery ≥48 hours (OR: 1.80, 1.12–2.90, p=0.016), receiving a prosthesis for a femoral neck fracture (OR: 1.38, 1.08–1.77, p=0.011), perioperative Hb loss (median 1.6mmol/L vs 1.2mmol/L, OR: 1.37, 1.20–1.56, p<0.001), and infection during admission: pneumonia (OR: 5.58, 4.03–7.73, p<0.001), urinary tract infection (UTI) (OR: 2.69, 1.89–3.85, p<0.001) and wound infection (OR: 4.03, 2.00–8.12, p<0.001). The results suggest a decreased risk of delirium is decreased when surgery time is ≤45 minutes (OR: 0.77, 0.60–0.98, p=0.034) and osteosynthesis of femoral neck fractures is performed (OR: 0.34, 0.19–0.61, p<0.001).
 |
Table 2 Univariable Analyses of Risk and Prognostic Perioperative Factors |
Clinical Outcomes
Clinical outcomes are presented in Table 3. The median length of delirium was 4 (3–5) days. The median length of primary in-hospital stay was significantly longer in patients with a delirium compared to those without a delirium: 9 days (6–14) vs 6 days (4–9) (p<0.001). The 30-day all-cause mortality was 7% (n=152) (with delirium 16% (n=53) vs with no delirium 6% (n=99) (p<0.001)). After 1 year of follow-up, the overall mortality was 19% (n=395). Thirty-three percent (n=109) of the patients with a delirium during submission, died within 1 year after surgery compared with 17% (n=286) in patients with no delirium (p<0.001). The all-cause survival rate is available in Figures 2 and 3 (Kaplan–Meier analysis).
 |
Table 3 Clinical Outcomes After Delirium |
 |
Figure 2 Kaplan–Meier curve of mortality rates in patients with and without delirium during 30-days follow-up. Note: Patients with no delirium = blue, patients with delirium = red. |
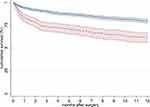 |
Figure 3 Kaplan–Meier curve of mortality rates in patients with and without delirium during 1-year follow-up. Note: Patients with no delirium = blue, patients with delirium = red. |
Multivariable Analysis
A multivariable analysis of factors associated with delirium after hip surgery was performed fixed for CCI and type of admission ward (Table 4). Significant independent prognostic risk factors for the development of a delirium after multivariable analysis, were that male gender (OR: 1.99, 1.51–2.63, p<0.001), age (OR: 1.06, 1.04–1.08, p<0.001), dementia (OR1.66, 1.24–2.23, p=0.001), Parkinson’s disease (OR: 2.32, 1.42–3.80, p=0.001), ΔHb loss (OR: 1.19, 1.03–1.38, p=0.022), pneumonia (OR: 3.86, 2.70–5.51, p<0.001), UTI (OR: 1.97, 1.33–2.90, p=0.001) and wound infection (OR: 3.02, 1.36–6.75, p=0.007).
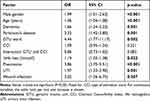 |
Table 4 Multivariable Analysis of Factors Associated with Delirium (n = 2.012) |
Discussion
In elderly patients, hip fracture surgery has a high impact on cognitive and functional outcomes. During admission for a hip fracture, early identification and treatment of (risk factors for) complications is useful to decrease the perioperative complication and mortality rate. The most frequent reported complication after hip surgery is delirium.3–13 In this study, the incidence rate of delirium was 16% (n=326). Results of the multivariable analysis found male gender, age, dementia, Parkinson’s disease, ΔHb loss, pneumonia, UTI and wound infection as significant independent prognostic risk factors for the development of a delirium after hip surgery.
Risk and Prognostic Perioperative Risk Factors
Univariable analysis showed that time to surgery ≥48 hours was associated with a higher incidence rate of delirium after hip fracture surgery. This may be correlated with higher frailty of patients who must be optimized for surgery. The multivariable analysis supports this hypothesis because after correcting for frailty (CCI), no significant difference between time to surgery and the occurrence of a delirium was emerged. Furthermore, no significant difference was found between surgery performed during the week or weekend, as well as surgery performed during daytime or nighttime.
This study found type of anesthesia did not significantly influence the development of postoperative delirium. This is comparable with the results of two recent randomized controlled trials (2021 and 2022) and a systematic review (2018) showing no difference in the incidence of postoperative delirium after hip fracture surgery between spinal and general anesthesia surgery.24–26
Ravi et al evinced prolonged surgical time was associated with a higher risk for delirium, with an OR of 1.06 per extra 30 minutes of surgery.27 This study did not prove an association between a longer time of hip surgery and delirium, which is in accordance with other previous studies.3,8 Patients receiving a prosthesis for a femoral neck fracture were more likely to develop a delirium after surgery, while patients receiving osteosynthesis for a femoral neck fracture had a significant lower risk on delirium. This difference was eliminated after multivariable analysis correcting for frailty. This can be explained by the fact that patients who received a prosthesis were more vulnerable compared to patients who received an osteosynthesis for femoral head preserving surgery. Surgery time ≤45 minutes was associated with significantly lower percentages of delirium. However, osteosynthesis surgery takes in general less time compared to a prosthesis. As mentioned earlier, it seems plausible that the osteosynthesis group is less frailty, what can explain the significant difference.
Clinical Outcomes
The most frequent reported complication after hip surgery is delirium with incidence rates between 19% and 39%.3–13 In this study, the incidence rate of delirium was 16% (n=326). Hypothetically, the lower delirium incidence rate is due to the admission of frail patients to the GTU since 2018 in the participating hospitals. Domesticity and rhythm were preserved on the GTU. We expect that by maintaining routine and domesticity, delirium will be less likely to develop.
The median length of delirium in this study was 4 days, which is similar compared to the median delirium duration of 4 and 5 days in previous studies of Bellelli et al and de Jong et al.3,28 The length of hospital stay was 3 days longer for delirium patients compared to non-delirium patients (9 days vs 6 days). Patients with dementia and a delirium stayed 7 days in hospital, while patients with dementia and no delirium stayed 4 days in hospital. The difference in admission duration between dementia and non-dementia patients may be the result of more dementia patients already live in nursing homes before admission and can be discharged sooner.
This study found a 30-day overall mortality of 7% (with delirium 16% vs with no delirium 6%). After 1 year of follow-up, the overall mortality was 19% in all patients (with delirium 33% vs with no delirium 17%). These results are in line with a previous study of de Jong et al and Ruggiero et al who described respectively a 1-year mortality rate of 39% and 23.3% in the delirium-positive group and 19% and 8.1% in the non-delirium group, considering that Ruggiero et al included a younger population.3,29
Multivariable Analysis
Previous literature reported higher age, male gender, BMI, higher ASA classification, living in a care institution pre-admission, dementia, Parkinson’s disease, polypharmacy, acute admission, and infection during admission as risk factors for delirium after hip surgery.3,11,17–19 The multivariable analysis of this study identified male gender, age, dementia, Parkinson’s disease, ΔHb loss, pneumonia, UTI and wound infection as significant independent prognostic risk factors for the development of a delirium after hip surgery.
This study shows the female gender is less likely to develop delirium after hip fracture surgery (OR: 0.60), comparable with results of a meta-analysis of Yang et al with an OR of 0.83.6 A higher age was found to be an independent prognostic baseline factor for the development of delirium. The median age of the delirium group was 85 years and 79 years in the non-delirium group. This is in accordance with previous literature showing higher age is an independent risk factor for delirium in elderly hip fracture patients.3,17,19
Cognitive impairment is reported to be associated with the occurrence of delirium after hip fracture surgery.30 This study demonstrated dementia as a strong independent predictor associated with the occurrence of delirium. Patients with Parkinson’s disease showed in this study a significant higher delirium incidence rate compared to patients with no Parkinson’s disease (10 vs 4%). Choi et al showed Parkinson’s disease to be an independent predictor of delirium after hip fracture surgery (OR: 5.75). Patients living in a nursing home pre-operatively sustained a delirium significantly more often (27%) compared to those who did not (18%). These outcomes are comparable to previous studies.3,6
Frail patients were admitted at the GTU ward to prevent a delirium. Nevertheless, admission on the GTU ward showed more delirium compared to admission at another ward. Our hypothesis is that admission at the GTU ward decreases the incidence of delirium in frail elderly patients but not to such an extent that it reaches the incidence level of delirium at a “normal” ward. We added the CCI GTU interaction at the multivariate analyses what confirmed our hypothesis. The GTU is not a significant factor associated with a delirium anymore after correction for CCI (frailty) after multivariable analyses (P=0.083, OR: 0.86).
After multivariable analysis, higher peri-operative hemoglobin loss was associated with higher rates of delirium after hip surgery (OR: 1.19). A meta-analysis (2021) evinced higher blood loss was associated with the occurrence of postoperative delirium after knee and hip replacement.20 Reducing blood loss perioperatively may reduce the incidence of delirium after hip fracture surgery.
The present study approved that infection during admission was independently associated with delirium, with the largest association of pneumonia, followed by wound infection and UTI. Our findings are also in line with a meta-analysis of Smith et al, who evinced that hip fracture patients who experienced post-operative pneumonia or a urinary tract infection were at nearly three-times and four-times greater chance of postoperative delirium, respectively.19 A previous study by de Jong et al found infection during admission, as an independent prognostic factor highly associated with the development of delirium during admission after hip hemiarthroplasty.3
Strengths
This study examines what clinical factors are associated with delirium after hip fracture surgery and the clinical outcomes including the rate of mortality after a delirium. The strength of this study is that we were able to examine a large and detailed prospective hip fracture database which prevents selection bias. We controlled for various confounders, including patient characteristics and hospital properties in the multivariate analysis.
Limitations
The study is observational, which means that causal relationships cannot be established, only risk factors that are strongly associated with delirium could be examined. In addition, due to its observational nature, it is not a standardized study. Despite the multivariate analysis, there may still be confounding. Secondly, this study is an observational cohort study based on patients’ medical charts, which can ensure that unreported data is not included in our analysis. Finally, there is always a similarity in symptoms between delirium and dementia, so that the distinction cannot always be made during hospitalization. In addition, the diagnosis of dementia cannot be made during a hospital stay if there is a suspicion. Both influence the reported incidence of delirium and dementia.
Conclusion
This study found male gender, higher age, dementia, Parkinson’s disease, hemoglobin loss, pneumonia, UTI and wound infection during admission as factors highly associated with delirium after hip fracture surgery. Delirium was associated with a two times as high 30-day and 1-year all-cause mortality.
Acknowledgments
This article is published on behalf of the author collaborator group Dutch Hip Fracture Registry Collaboration (DHFR): F. van Beek2, J.M. van Buijtenen2, B.I. Cleffken1, T. Klem2, T.M. Kuijper3, A.G.J. van Marle2, N.W.L. Schep1, G.B. Schmidt2, N.M.R. Soesman2, J. Vermeulen1, C.H. van der Vlies1, O. Wijers2.
1Surgery Department, Maasstad Hospital, 3079 DZ Rotterdam, the Netherlands;
2Surgery Department, Franciscus Hospital, 3045 PM Rotterdam, the Netherlands;
3Science Board, Maasstad Hospital, 3079 DZ Rotterdam, the Netherlands.
The authors thank Flip van Beek, Jesse M van Buijtenen, Berry I Cleffken, Taco MAL Klem, Martijn Kuijper, Alexander GJ van Marle, Niels WL Schep, G Ben Schmidt, Nicolaj MR Soesman, Jefrey Vermeulen, Cornelis H van der Vlies and Olivier Wijers of the Dutch Hip Fracture Registry.
Ethics Approval
The local medical ethics committee approved the study and the study was registered in the Dutch Trial Register (nr NL 8313).
Consent to Participate
Due to the high percentage of cognitive dysfunction in the study population and since there were no changes in usual practice of care, the committee determined that patients’ consent to review medical charts was not required.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Leon DA. Trends in European life expectancy: a salutary view. Int J Epidemiol. 2011;40(2):271–277. doi:10.1093/ije/dyr061
2. Kanis JA, Oden A, McCloskey EV, et al. A systematic review of Hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23(9):2239–2256. doi:10.1007/s00198-012-1964-3
3. de Jong L, van Rijckevorsel V, Raats JW, Klem T, Kuijper TM, Roukema GR. Delirium after hip hemiarthroplasty for proximal femoral fractures in elderly patients: risk factors and clinical outcomes. Clin Interv Aging. 2019;14:427–435. doi:10.2147/CIA.S189760
4. Gleason LJ, Schmitt EM, Kosar CM, et al. Effect of delirium and other major complications on outcomes after elective surgery in older adults. JAMA Surg. 2015;150(12):1134–1140. doi:10.1001/jamasurg.2015.2606
5. Krogseth M, Wyller TB, Engedal K, Juliebo V. Delirium is a risk factor for institutionalization and functional decline in older hip fracture patients. J Psychosom Res. 2014;76(1):68–74. doi:10.1016/j.jpsychores.2013.10.006
6. Yang Y, Zhao X, Dong T, Yang Z, Zhang Q, Zhang Y. Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res. 2017;29(2):115–126. doi:10.1007/s40520-016-0541-6
7. Wang CG, Qin YF, Wan X, Song LC, Li ZJ, Li H. Incidence and risk factors of postoperative delirium in the elderly patients with hip fracture. J Orthop Surg Res. 2018;13(1):186. doi:10.1186/s13018-018-0897-8
8. Mosk CA, Mus M, Vroemen JP, et al. Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging. 2017;12:421–430. doi:10.2147/CIA.S115945
9. Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–522. doi:10.1046/j.1532-5415.2001.49108.x
10. Juliebø V, Bjøro K, Krogseth M, Skovlund E, Ranhoff AH, Wyller TB. Risk factors for preoperative and postoperative delirium in elderly patients with hip fracture. J Am Geriatr Soc. 2009;57(8):1354–1361. doi:10.1111/j.1532-5415.2009.02377.x
11. Choi YH, Kim DH, Kim TY, Lim TW, Kim SW, Yoo JH. Early postoperative delirium after hemiarthroplasty in elderly patients aged over 70 years with displaced femoral neck fracture. Clin Interv Aging. 2017;12:1835–1842. doi:10.2147/CIA.S147585
12. Bellelli G, Mazzola P, Morandi A, et al. Duration of postoperative delirium is an independent predictor of 6-month mortality in older adults after hip fracture. J Am Geriatr Soc. 2014;62(7):1335–1340. doi:10.1111/jgs.12885
13. Bai J, Liang Y, Zhang P, et al. Association between postoperative delirium and mortality in elderly patients undergoing hip fractures surgery: a meta-analysis. Osteoporos Int. 2020;31(2):317–326. doi:10.1007/s00198-019-05172-7
14. Krogseth M, Watne LO, Juliebo V, et al. Delirium is a risk factor for further cognitive decline in cognitively impaired hip fracture patients. Arch Gerontol Geriatr. 2016;64:38–44. doi:10.1016/j.archger.2015.12.004
15. Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA. 2010;304(4):443–451. doi:10.1001/jama.2010.1013
16. Dolan MM, Hawkes WG, Zimmerman SI, et al. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol Biol Sci Med Sci. 2000;55(9):M527–534. doi:10.1093/gerona/55.9.M527
17. Kalisvaart KJ, Vreeswijk R, de Jonghe JF, van der Ploeg T, van Gool WA, Eikelenboom P. Risk factors and prediction of postoperative delirium in elderly hip-surgery patients: implementation and validation of a medical risk factor model. J Am Geriatr Soc. 2006;54(5):817–822. doi:10.1111/j.1532-5415.2006.00704.x
18. Oh ES, Li M, Fafowora TM, et al. Preoperative risk factors for postoperative delirium following hip fracture repair: a systematic review. Int J Geriatr Psychiatry. 2015;30(9):900–910. doi:10.1002/gps.4233
19. Smith TO, Cooper A, Peryer G, Griffiths R, Fox C, Cross J. Factors predicting incidence of post-operative delirium in older people following hip fracture surgery: a systematic review and meta-analysis. Int J Geriatr Psychiatry. 2017;32(4):386–396. doi:10.1002/gps.4655
20. Rong X, Ding ZC, Yu HD, Yao SY, Zhou ZK. Risk factors of postoperative delirium in the knee and hip replacement patients: a systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):76. doi:10.1186/s13018-020-02127-1
21. Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101(4):511–517. doi:10.1093/bja/aen236
22. Moppett IK, Parker M, Griffiths R, Bowers T, White SM, Moran CG. Nottingham Hip Fracture Score: longitudinal and multi-assessment. Br J Anaesth. 2012;109(4):546–550. doi:10.1093/bja/aes187
23. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
24. Neuman MD, Feng R, Carson JL, et al. Spinal anesthesia or general anesthesia for hip surgery in older adults. N Engl J Med. 2021;385(22):2025–2035. doi:10.1056/NEJMoa2113514
25. Li T, Li J, Yuan L, et al. Effect of regional vs general anesthesia on incidence of postoperative delirium in older patients undergoing hip fracture surgery: the RAGA randomized trial. JAMA. 2022;327(1):50–58. doi:10.1001/jama.2021.22647
26. Patel V, Champaneria R, Dretzke J, Yeung J. Effect of regional versus general anaesthesia on postoperative delirium in elderly patients undergoing surgery for hip fracture: a systematic review. BMJ Open. 2018;8(12):e020757. doi:10.1136/bmjopen-2017-020757
27. Ravi B, Pincus D, Choi S, Jenkinson R, Wasserstein DN, Redelmeier DA. Association of duration of surgery with postoperative delirium among patients receiving hip fracture repair. JAMA Netw Open. 2019;2(2):e190111. doi:10.1001/jamanetworkopen.2019.0111
28. Bellelli G, Carnevali L, Corsi M, et al. The impact of psychomotor subtypes and duration of delirium on 6-month mortality in hip-fractured elderly patients. Int J Geriatr Psychiatry. 2018;33:1229–1235. doi:10.1002/gps.4914
29. Ruggiero C, Bonamassa L, Pelini L, et al. Early post-surgical cognitive dysfunction is a risk factor for mortality among hip fracture hospitalized older persons. Osteoporos Int. 2017;28(2):667–675. doi:10.1007/s00198-016-3784-3
30. Hou M, Zhang Y, Chen AC, et al. The effects of dementia on the prognosis and mortality of hip fracture surgery: a systematic review and meta-analysis. Aging Clin Exp Res. 2021;33(12):3161–3172. doi:10.1007/s40520-021-01864-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
