Back to Journals » Clinical Ophthalmology » Volume 17
Defocus Curve and Satisfaction of Patients with Presbyopia After LASIK Using the Differential Modulation of Binocular Longitudinal Spherical Aberration
Authors Zhang J , Shao J, Cao X, Zhang Y, Zheng L
Received 27 August 2023
Accepted for publication 16 November 2023
Published 21 November 2023 Volume 2023:17 Pages 3531—3542
DOI https://doi.org/10.2147/OPTH.S437324
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Jun Zhang, Jie Shao, Xinfang Cao, Yonggang Zhang, Li Zheng
Department of Ophthalmology, Hangzhou MSK Eye Hospital, Hangzhou, People’s Republic of China
Correspondence: Jun Zhang, Hangzhou MSK Eye Hospital, No. 384, Fengqi Road, Gongshu District, Hangzhou, Zhejiang, People’s Republic of China, Tel +86 18667046602, Fax +86 85068587, Email [email protected]
Purpose: To investigate the visual acuity and satisfaction of patients after Zhang & Zheng’s corneal laser-enhanced accommodation refraction Q (ZZ-CLEAR-Q) surgery utilizing differential modulation of binocular longitudinal spherical aberration and determine its clinical significance.
Patients and Methods: This prospective observational study enrolled a consecutive cohort of patients with presbyopia who underwent ZZ-CLEAR-Q surgery between December 2020 and January 2023. The study assessed visual acuity, distance-corrected defocus curve, satisfaction, Q factor, manifest spherical equivalent, and primary spherical aberration, among others, at 3 months postoperatively. Additionally, the study conducted a binocular comparison to analyze the clinical significance of setting the different longitudinal spherical aberrations.
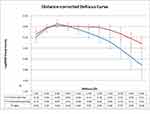
Results: A total of 232 eyes of 116 patients were included. The binocular uncorrected distance visual acuity was 20/20 for all patients. At 3 months postoperatively, the binocular uncorrected near visual acuity was Jaeger 1 for 96% of the patients and Jaeger 2 for 100% of the patients. Furthermore, 93.1% of the patients expressed satisfaction. The monocular distance-corrected defocus curve revealed that the dominant eyes had significantly better visual acuity at 0 D (P< 0.001), while the non-dominant eyes had significantly better visual acuity across various defocus levels except 0 and − 0.50 D (All P< 0.05). At 3 months, there were no significant differences between the expected and achieved manifest spherical equivalents, corneal Q factor values, and ocular primary spherical aberration values of both groups.
Conclusion: Patients with presbyopia who underwent ZZ-CLEAR-Q surgery were likely to achieve normal uncorrected visual acuity and be satisfied. The increased depth of field has clinical significance for assisting near vision.
Keywords: defocus curve, LASIK, presbyopia, Q factor, spherical aberration
Introduction
Age-related accommodative deficiency, also known as presbyopia, refers to the natural decline in the ability of the eye to focus on close objects because of aging. This condition leads to a progressive deterioration in the clarity of near vision.1 Presbyopia is a common age-related phenomenon and occurs due to the weakening of the ciliary muscle and/or increased stiffness of the lens, which hinders the adjustment of the focal point.1 Correcting presbyopia has been a longstanding challenge for ophthalmologists.
Due to the current limitations in fully restoring dynamic accommodative ability, the primary approach for addressing presbyopia continues to be the redistribution of focus. This can be achieved through different corrective methods such as monovision with binoculars.2–4 Multifocal with monoculars,5,6 or blend vision.7–9 Compared with intraocular lens replacement, which is commonly used in individuals older than 55 years of age or those with increased lens density,10 corneal-based procedures offer the advantage of refractive state reversibility.11,12 One factor that can impact satisfaction with vision is longitudinal spherical aberration (LSA), which is a high-order physiological aberration.13 LSA refers to the distance between the two intersections of the marginal and paraxial rays with the optical axis within a circular area.14 The coefficient of asphericity (Q) represents the rate of curvature variation in a lens as it moves away from the center.15
PresbyLASIK, which can delay the onset of age-related near vision symptoms by way of a multifocal effect,16,17 is a commonly used method for correcting age-related accommodative deficiency or presbyopia in patients who do not have cataracts.1 An appropriate presbyLASIK strategy can address ametropia correction and reduce dependence on reading spectacles, while providing a better visual experience. Compared with the traditional monovision procedure, the advanced monovision procedure combines the aspherical or multifocal shape design in either monocular or binocular settings, allowing for easier binocular fusion and more comfortable vision outcomes. In terms of corneal reshaping design, refractive multifocal approaches are theoretically more likely to result in visual disturbances known as “visual jumps” caused by changes in pupil diameter. They also require higher precision in the centricity of the ablation.18 Therefore, the corneal laser enhanced accommodation refraction Q (CLEAR Q) treatment, which utilizes an aspherical Q-factor guided laser-assisted corneal surgery technique, offers potential advantages related to visual quality. This is especially relevant when considering that achieving microscopic diffractive multifocal effects through corneal reshaping can be challenging.
CLEAR Q can effectively extend focus by adjusting the target Q factor to modulate spherical-like aberration and extend the deeps of focus.19 Optimal focus extensions should not significantly compromise visual acuity while improving near vision for eyes with consistent manifest refraction. However, there is currently no consensus on the ideal target Q factor.20 Inappropriate Q factor settings can result in a focus extension that is too narrow to have a noticeable impact on near vision or too wide, causing a decline in visual acuity. Furthermore, addressing the individual corneal morphology and accounting for the influence of crystalline lenses are two challenges that should be taken into consideration. Therefore, it is essential to individualize the target Q factor rather than rely on a fixed value, considering the unique characteristics of the eyes of each patient.
To address these challenges, a modified strategy called Zhang & Zheng CLEAR-Q (ZZ-CLEAR-Q) was proposed for CLEAR-Q treatment. ZZ-CLEAR-Q incorporates three additional constraints: (a) constraint of the focus extension of the operated eye; (b) constraint of the boundary of the LSA optical zone; and (b) constraint of anisometropia in refraction and visual acuity.
By implementing these additional constraints, the ZZ-CLEAR-Q strategy aims to improve the precision and effectiveness of the CLEAR-Q treatment for presbyopia correction.
Materials and Methods
Study Design and Participants
This prospective observational study enrolled a consecutive cohort of patients with presbyopia scheduled to undergo ZZ-CLEAR-Q surgery at Hangzhou MSK Eye Hospital between December 2020 and January 2023. The study obtained institutional review board approval from the medical research ethics committee of Hangzhou MSK Eye Hospital (#MSKLL201215), and all procedures were conducted in accordance with the principles outlined in the Declaration of Helsinki. Prior to participation, all participants were fully informed about the potential risks and benefits associated with the procedure, and they provided written informed consent to participate in the study.
The study had specific inclusion and exclusion criteria. The inclusion criteria were as follows: (a) age between 40 and 52 years; (b) myopia ranging from −0.50 to −6.00 DS; (c) refractive astigmatism ranging from 0.00 to −3.00 DC; and (d) corrected distance visual Snellen acuity of 20/20 or better. On the other hand, the exclusion criteria were as follows: (a) non-binocular refractive correction; (b) poor tolerance of monovision, defined by experiencing significant discomfort after wearing a contact lens with +1.00 DS added to the non-dominant eye for 3 hours; (c) history of corneal refractive surgery; (d) presence of nebula, macula, leukoma, or other corneal opacities; (e) target optical zone diameter less than 6.5 mm; (f) inability to achieve the target LSA due to limitations of the device used; or (g) presence of contraindications to corneal refractive surgery. Additionally, participants with a follow-up duration of less than 3 months were excluded from the final analysis.
Procedures
All patients underwent a complete ophthalmic examination that included assessment of manifest refraction, cycloplegic refraction, determination of dominant eye with the hole-in-The-card test and the lens fogging technique, a monovision tolerance test, anterior segment tomography (Sirius; CSO, Florence, Italy), ocular wavefront aberration (Analyzer; Alcon, Fort Worth, TX, USA), slit-lamp microscopy, axial length (AL) measurement, intraocular pressure (IOP) measurement, and funduscopy.
All procedures were performed with the patient in the supine position by the same experienced surgeon (JZ) who had 10 years of experience in corneal refractive surgery.21 ZZ-CLEAR-Q surgery was performed using the WaveLight Refractive Suite platform (FS200 & EX500; Alcon, Fort Worth, TX, USA).
During flap creation, settings were adjusted to achieve a thickness of 100 μm, side-cut angle of 120°, 8 × 8 μm point spacing of the flap, and 5 × 3 μm point spacing of the side cut. After a femtosecond laser scan, the corneal stroma was ablated with the following target refraction and Q-value.
Dominant Eye Group
In the study, the dominant eye was treated to correct distance vision with a target of 0.00 D of ocular LSA within a 5.0 mm optical zone. The refractive target for the dominant eye was −0.25 DS, ensuring that the distance visual acuity remained no worse than 20/20.
Non-Dominant Eye Group
On the other hand, the non-dominant eye was treated to correct near vision with a target of −1.00 D for ocular LSA within a 5.0 mm optical zone. The refractive target for the non-dominant eye was −1.00 DS while ensuring that the distance visual acuity remained no worse than 20/30.
These treatment strategies aimed to achieve optimal vision for both distance and near vision, with the dominant eye optimized for distance vision and the non-dominant eye optimized for near vision.
The Target Q-Value
The target setting of the Q factor was determined using Zhang & Zheng’s LSA formula (referred to as ZZ LSA). The details of this formula can be found in the patent application number 2019111386516 on the Chinese invention patent website (www.cpquery.sipo.gov.cn). Additionally, ZZ LSA is open access, and it is available at https://www.zzcal.com/calc/en/lsa_qd (Figure 1).
 |
Figure 1 Screenshot demonstrating the application of the Zhang & Zheng longitudinal spherical aberration (ZZ LSA) formula. |
Outcomes
The study measured various outcomes, including visual acuity, manifest spherical equivalent (SE), distance-corrected defocus curve, patient satisfaction, corneal Q factor, and ocular primary spherical aberration (PSA). The visual acuity measurements included monocular and binocular uncorrected and corrected distance visual acuities (UCDVA and CDVA, respectively) and uncorrected and distance-corrected near visual acuities at a distance of 40 cm (UCNVA and DCNVA, respectively).
UCDVA, CDVA, UCNVA, and DCNVA were measured and recorded before the surgery as well as at 1 day, 2 weeks, 1 month, and 3 months postoperatively. The anterior corneal Q factor in a 5.0 mm zone was determined using the Sirius tomography instrument before and after the surgery. The ocular PSA in a 5.0 mm zone was determined using the aberration analyzer before and after the operation. Only values that met the criteria of high quality, repeatability, and centrality were included in the statistical analysis.21 The evaluators were blinded to whether the evaluated eyes were dominant or non-dominant. At 3-month follow-up, a monocular distance-corrected defocus curve was obtained, and the patients completed the visual-related quality questionnaire (VFQ25).22 Any complications that affected daily life, such as glares, halos, or eye dryness, were monitored during the 3-month follow-up.
The baseline demographic data, including age and sex, and clinical data, including the dominant eye, spherical manifest refraction, cylindrical refraction, anterior corneal Q factor in a 5.0 mm zone, ocular PSA in a 5.0 mm zone, central corneal thickness, Kf, intraocular pressure, and axial length, were collected.
Statistical Analysis
All statistical analyses were conducted using Microsoft Excel 2010 (Microsoft Corporation, Redmond, WA) and SPSS 19.0 (IBM, Armonk, NY, USA). The normality of continuous variables was assessed using the Kolmogorov–Smirnov test, and homoscedasticity was assessed using Levene’s test. Continuous variables that followed a normal distribution were presented as means ± standard deviation (SD) and compared using paired t-tests. Continuous variables that had a skewed distribution were presented as medians (range) and compared using the Wilcoxon signed-rank test. Categorical variables were presented as counts and percentages (n [%]). Corneal aspherical and aberration parameters at different examination points were analyzed using one-way repeated-measures analysis of variance (ANOVA). Two-sided p-values less than 0.05 denoted statistical significance.
Results
A total of 232 eyes of 116 patients (mean age, 45.57±3.14 years; 51 males) were included in the final analysis (Table 1). The baseline data of the groups were comparable (Table 2). At 3 months postoperatively, the binocular uncorrected distance visual acuity was 20/20 for 100% of the patients, and the binocular uncorrected near visual acuity was Jaeger 1 for 96% of the patients and Jaeger 2 for 100% of the patients. (Figure 2). The monocular distance-corrected defocus curve revealed that the dominant eyes had significantly better visual acuity at 0 D (P < 0.001), while the non-dominant eyes had significantly better visual acuity across various defocus levels except 0 D and −0.50 D (All P < 0.05) (Figure 3).
 |
Table 1 Preoperative Clinical Characteristics of the Study Participants |
 |
Table 2 Preoperative Clinical Characteristics of the Dominant and Non-Dominant Groups |
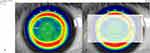
The corneal Q factor and ocular PSA of the dominant and non-dominant eyes remained stable throughout the first postoperative month, with no significant changes observed between 1 and 3 months postoperatively. In the dominant eyes, there were no significant changes in the corneal Q factor (p=0.070) and ocular PSA (p=0.159) between 1 and 3 months postoperatively. Similarly, in the non-dominant eyes, no significant changes were found in the corneal Q factor (p=0.338) and ocular PSA (p=0.079) during the same period. At 3 months postoperatively, the anterior corneal Q factor values were −0.11±0.19 and −0.51±0.15 (p<0.001) and the ocular PSA values were −0.01±0.06 and −0.12±0.04 (p<0.001) for the dominant and non-dominant eyes, respectively (Figure 4). Furthermore, there were no significant differences between the expected and achieved manifest refraction SEs, corneal Q factor values, and ocular PSA values of the dominant eyes, as well as the SEs and corneal Q factor values of the non-dominant eyes at the 3-month follow-up (Table 3).
 |
Table 3 Corneal Characteristics of 5 Mm at 3 Months Postoperatively |
 |
Figure 4 The corneal Q factor (A) and ocular primary spherical aberration (PSA) (B) of the dominant and non-dominant eyes measured in a 5.0-mm zone. |
At the 3-month follow-up, no eye had experienced a loss of two or more lines of CDVA. Only one eye (3.3%) experienced a loss of one line of CDVA, while two eyes (6.67%) gained one line of CDVA. None of the patients required any additional refractive retreatment procedures. These results indicate overall positive outcomes in terms of visual acuity stability and the absence of significant vision loss.
At the 3-month follow-up, a high level of satisfaction was reported by most patients. Out of the 116 patients, 108 (93.1%) expressed satisfaction with their visual comfort for everyday activities and indicated that they would recommend surgery to others. Only 8 patients (6.9%) still required spectacles for near vision. None of the patients reported experiencing glares, halos, or significant eye dryness that impacted their daily lives during the follow-up.
Discussion
This study demonstrated excellent outcomes related to binocular UCDVA, as all patients achieved 20/20 vision. Binocular UCNVA was also highly favorable, with 93% and 100% of patients achieving Jaeger 1 and Jaeger 2, respectively. Furthermore, a high percentage (96%) of patients reported satisfaction with the surgery and expressed their willingness to recommend it to others. These findings suggest that the ZZ-CLEAR Q surgery is a valuable approach for addressing presbyopia in patients. The study provides valuable insights and serves as a reference for the treatment of presbyopia.
Age-related accommodative deficiency, often observed during the early stages of presbyopia, refers to a situation where patients have not completely lost their accommodative ability but have a reduced amount of accommodation.23 In conventional laser vision correction approaches, patients may still require reading glasses immediately after the procedure, which can be inconvenient in their daily activities. However, the ZZ-CLEAR Q strategy for presbyopic LASIK aims to address this issue by combining the advantages of monovision and aspherical ablation. By utilizing this approach, ZZ-CLEAR Q intends to compensate for the accommodative deficits and provide patients with improved near vision without the immediate need for reading glasses. This strategy offers potential benefits in overcoming the challenges associated with age-related accommodation deficiency and improving the overall visual experience for patients with presbyopia.
Aspherical ablation can modify the refractive power in the peripheral regions of the cornea, while the central or paraxial refractive power remains relatively unchanged. This selective modulation of peripheral refractive power allows for an extension of the depth of focus, enabling improved near vision without significantly compromising distance vision. However, there is no consensus on the optimal direction and extent of peripheral refractive power modulation. Both increasing and decreasing peripheral refractive power have been proposed to extend the depth of focus. Similar to previous studies,5,24,25 the peripheral refractive power was reduced in this study. This decision was based on the understanding that reading activities typically occur in brighter environments, which lead to pupillary constriction. By reducing peripheral refractive power, the study aimed to optimize the visual experience during near-vision tasks. The magnitude of peripheral refractive power modulation presents three challenges that require consideration. Firstly, determining the appropriate diameter of the analysis optical zone is crucial. This is because the Q factor or spherical aberration within a specific zone is determined by the curvature of the corneal apex and the circle within which the optical zone is located while disregarding the middle area. In corneas corrected for myopia, the Q factor remains relatively stable within the fully corrected optical zone, which can be approximated through ray tracing methods.26 However, the PSA or LSA tends to change systematically with an increase beyond the size of the fully corrected optical zone. For instance, in the case of a patient with myopia who undergoes correction with a target optical zone diameter of 6.5 mm and a target ocular PSA of 0 D, the effective or functional optical zone diameter can easily surpass 6.0 mm. However, the fully corrected optical zone diameter often ends up around 5.0 mm (see Figure 5), and it tends to reduce as the refractive power of the myopia correction increases. This phenomenon could be attributed to the cosine theorem, which reduces the peripheral ablation effect. Consequently, the ocular PSA can be close to 0 μm within 5.0 mm of the optical zone diameter but rapidly reach 0.1 μm when it exceeds 5.0 mm (see Figure 6). Therefore, it is more meaningful and reasonable to extend the depth of focus within the fully corrected optical zone. Contrary to the observed optical zone diameter of 6.0 or 6.5 mm utilized in most previous studies,27–30 the present study opted for 5.0 mm. This variability in conclusions regarding the significant increase in spherical aberration or Q value resulting from laser vision correction may be attributed to the reason discussed earlier. The systematic changes in PSA or LSA beyond the size of the fully corrected optical zone can lead to differing outcomes in different studies. The selection of the optical zone size and the effects on PSA and LSA can vary, thereby influencing the conclusions drawn regarding the impact of laser vision correction on spherical aberration or Q value.30,31 Second, it is important to strike a balance between improving near vision and maintaining distance vision. Since there was no tolerance test for stretching focus available, the present study aimed for a relatively moderate magnitude for the non-dominant eye. In contrast to previous studies, the use of LSA in diopters rather than PSA in micrometers was introduced. This not only allows for a more relatable connection between near visual improvement and familiar reading spectacles measured in diopters but also establishes a link between distance visual impairment and familiar ametropia measured in diopters. Thirdly, achieving the desired visual magnitude should be accomplished through corneal morphological reshaping. In contrast to previous strategies, this study focused on targeting aspheric factors based on individual ocular spherical aberration to achieve the desired ocular LSA. The goal was to minimize significant deviations of ocular LSA from the expected value, as such deviations could lead to inadequate accommodation or excessive reduction in visual acuity due to individual variations in corneal or crystalline lens spherical aberration. Furthermore, by modulating the ocular LSA differently between the two eyes and comparing the binocular distance-corrected defocus curves, the clinical significance of LSA in assisting near vision could be demonstrated.
 |
Figure 6 Schematic diagram illustrating the positive spherical aberration mutation in the peripheral zone. |
To achieve the desired ocular LSA, this study introduced the ZZ LSA formula, which is a proprietary calculation process not yet published, to assist in the CLEAR Q treatment and determine the target Q factor. CLEAR Q refers to a specific technique of aspherical Q-factor-guided laser-assisted corneal surgery, primarily aimed at patients with ametropia and age-related accommodation deficiency. The target Q factor consists of two components: an initial ineffective modulation of −0.30 ΔQ and a subsequent target Q +0.30 after stabilization. The amount of ineffective modulation was determined based on a preliminary study, which took into account factors such as corneal morphological rebalancing and epithelial remodeling. This finding aligns with a previous study conducted by Llorente et al.32 By considering the individual differences in ocular LSA and the relationship between LSA and spherical refractive power,33 the ZZ LSA formula can be used to determine the optimal spherical power compensation after Q factor modulation for each patient. This personalized approach is expected to improve the accuracy of the refractive outcome and reduce the risk of overcorrection or undercorrection.34 However, it should be noted that the ZZ LSA formula has not been independently validated, and further studies are needed to confirm its effectiveness and safety.
The refractive outcomes, such as manifest SE and corneal Q factor, in the dominant eyes were related to the target values. While direct measurement of ocular LSA was not possible with the devices used in this study, the achieved ocular PSA served as an indirect reference. Based on the experience of the authors, the LSA value was estimated to be approximately 8 times that of PSA in normal eyes, and the achieved ocular LSA was associated with the targeted value. Furthermore, in the monocular distance-corrected defocus curve, which eliminates the effect of ametropia, the non-dominant eye demonstrated superior intermediate and near vision over the dominant eye. Specifically, the near-vision part of the curve showed an improvement of more than two Snellen lines, indicating that modulation of spherical aberration may contribute to enhanced near vision. These findings suggest that the ZZ-CLEAR Q approach, with its targeted aspheric ablation and consideration of ocular LSA, could effectively improve near-vision outcomes in patients with presbyopia.
However, the treatment effect, especially on the UCNVA, gradually decreases, with presbyopia increasing year by year for the relatively young patient cohort. Therefore, patients need to have a reasonable understanding of the duration before treatment. Besides, the differential modulation of binocular LSA may provide insights into the selection of spherical aberration of intraocular lenses for future cataract surgery.
This study acknowledges several limitations. First, the small sample size suggests that larger studies are necessary to validate and generalize the findings. Second, there is a need for further discussion and optimization of the target values for binocular refractive power and LSA. Third, a single surgeon performed all the procedures, and this introduces potential bias. Fourth, the discrepancy between the optical zones of the corneal Q factor and ocular PSA, as detected by the devices used in this study, should be considered. The center of the optical zone used to derive the ocular PSA, which is located at the pupil center, may deviate from the visual axis, potentially affecting visual acuity. Fifth, follow-up duration of 3 months was limited, and this prevented the evaluation of long-term outcomes. Future investigations should focus on assessing long-term changes in ocular LSA and its implications. Lastly, the approach used in this study was not compared with other approaches, such as traditional LASIK or monovision contact lenses, and related studies will be conducted in the future.
Conclusion
In summary, this study suggests that ZZ-CLEAR Q surgery could be a viable option for addressing age-related accommodative deficiency in patients. The results indicate that patients who underwent this treatment had the potential to achieve normal uncorrected visual acuity and reported satisfaction with the procedure. Furthermore, the modulation of spherical aberration appears to have a positive impact on near vision. Therefore, ZZ-CLEAR Q can be considered an optional LASIK strategy for optimizing visual outcomes in patients with age-related accommodative deficiency. These findings have potential implications for clinical practice in this patient population.
Data Sharing Statement
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study received ethical approval from the Medical Research Ethics Committee of Hangzhou MSK Eye Hospital (#MSKLL201215) and was conducted in accordance with the principles outlined in the Declaration of Helsinki. Prior to participating in the study, all participants were provided with detailed information regarding the potential risks and benefits of the procedure. Written informed consent was obtained from each participant, indicating their voluntary agreement to participate in the study. Adherence to ethical guidelines ensured the protection of participants’ rights and welfare throughout the research process.
Funding
This study received support from the Zhejiang Medical and Health Science and Technology Project, specifically grant numbers 2018267858 and 2020167858. It is important to note that the funders had no involvement in the design of the study, collection and analysis of data, decision to publish, or preparation of the manuscript. The funding was provided solely to support the research and its findings.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Katz JA, Karpecki PM, Dorca A., et al. Presbyopia - A review of current treatment options and emerging therapies. Clin Ophthalmol. 2021;15:2167–2178. doi:10.2147/OPTH.S259011
2. Goldberg DB. Laser in situ keratomileusis monovision. J Cataract Refract Surg. 2001;27(9):1449–1455. doi:10.1016/S0886-3350(01)01001-X
3. Wright KW, Guemes A, Kapadia MS, Wilson SE. Binocular function and patient satisfaction after monovision induced by myopic photorefractive keratectomy. J Cataract Refract Surg. 1999;25(2):177–182. doi:10.1016/S0886-3350(99)80123-0
4. Evans BJ. Monovision: a review. Ophthalmic Physiol Opt. 2007;27(5):417–439. doi:10.1111/j.1475-1313.2007.00488.x
5. Wang Yin GH, Mcalinden C, Pieri E, et al. Surgical treatment of presbyopia with central presbyopic keratomileusis: one-year results. J Cataract Refract Surg. 2016;42(10):1415–1423. doi:10.1016/j.jcrs.2016.07.031
6. Rouimi F, Ouanezar S, Goemaere I, et al. Presbyopia management with Q-factor modulation without additive monovision: one-year visual and refractive results. J Cataract Refract Surg. 2019;45(8):1074–1083. doi:10.1016/j.jcrs.2019.02.039
7. Mcneely RN, Moutari S, Palme C, Moore JE. Visual outcomes and subjective experience after combined implantation of extended depth of focus and trifocal IOLs. J Refract Surg. 2020;36(5):326–333. doi:10.3928/1081597X-20200318-01
8. Song JE, Han SY, Khoramnia R, et al. Clinical outcomes of combined implantation of an extended depth of focus IOL and a trifocal IOL in a Korean population. J Ophthalmol. 2021;2021:9034258. doi:10.1155/2021/9034258
9. Ruiz-Alcocer J, Lorente-Velazquez A, Hernandez-Verdejo JL, De Gracia P, Madrid-Costa D. Optical performance of a trifocal IOL and a novel extended depth of focus IOL combined with different corneal profiles. J Refract Surg. 2020;36(7):435–441. doi:10.3928/1081597X-20200519-02
10. Refractive Surgery Group Of Chinese Ophthalmologist A. 中国医师协会眼科医师分会屈光手术学组. 中国伴年龄相关性调节不足屈光不正患者激光角膜屈光手术专家共识(2021年) [Chinese expert consensus on laser corneal refractive surgery for correction of refractive errors with age-related accommodation deficiency (2021)]. Zhonghua Yan Ke Za Zhi. 2021;57:651–657. Chinese
11. Ang RE, Reyes RM, Solis ML. Reversal of a presbyopic LASIK treatment. Clin Ophthalmol. 2015;9:115–119. doi:10.2147/OPTH.S72676
12. Luger MH, Ewering T, Arba-Mosquera S. Nonwavefront-guided Presby reversal treatment targeting a monofocal cornea after bi-aspheric ablation profile in a patient intolerant to multifocality. J Refract Surg. 2014;30(3):214–216. doi:10.3928/1081597X-20131223-01
13. Glasser A, Campbell MC. Presbyopia and the optical changes in the human crystalline lens with age. Vision Res. 1998;38(2):209–229. doi:10.1016/S0042-6989(97)00102-8
14. El-Nashar NF. Longitudinal spherical aberration and mass of bi-aspheric aphakic rigid contact lenses. Ophthalmic Physiol Opt. 1999;19(5):441–445. doi:10.1046/j.1475-1313.1999.00467.x
15. Da Rocha Lucena A, Da Rocha Lucena D, Da Rocha Lucena D, et al. Study of asphericity coefficient and longitudinal spherical aberration surface corneal. Rev Bras Oftalmol. 2017;76:61–64.
16. Artola A, Patel S, Schimchak P, Ayala MJ, Ruiz-Moreno JM, Alió JL. Evidence for delayed presbyopia after photorefractive keratectomy for myopia. Ophthalmology. 2006;113(5):735–741. doi:10.1016/j.ophtha.2006.01.054
17. Alió JL, Chaubard JJ, Caliz A, Sala E, Patel S. Correction of presbyopia by technovision central multifocal LASIK (presbyLASIK). J Refract Surg. 2006;22(5):453–460. doi:10.3928/1081-597X-20060501-06
18. Sieburth R, Chen M. Intraocular lens correction of presbyopia. Taiwan J Ophthalmol. 2019;9(1):4–17. doi:10.4103/tjo.tjo_136_18
19. Stival LR, Figueiredo MN, Santhiago MR. Presbyopic Excimer Laser Ablation: a Review. J Refract Surg. 2018;34(10):698–710. doi:10.3928/1081597X-20180726-02
20. Villegas EA, Alcon E, Mirabet S, et al. Extended depth of focus with induced spherical aberration in light-adjustable intraocular lenses. Am J Ophthalmol. 2014;157(1):142–149. doi:10.1016/j.ajo.2013.08.009
21. Zhang J, Zheng L, Zhao X, et al. Corneal aberrations after small-incision lenticule extraction versus Q value-guided laser-assisted in situ keratomileusis. Medicine. 2019;98(5):e14210. doi:10.1097/MD.0000000000014210
22. Mangione CM, Lee PP, Gutierrez PR, et al. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119(7):1050–1058. doi:10.1001/archopht.119.7.1050
23. Hussaindeen JR, Murali A. Accommodative Insufficiency: prevalence, Impact and Treatment Options. Clin Optom. 2020;12:135–149. doi:10.2147/OPTO.S224216
24. Avila MY, Vivas PR. Visual outcomes in hyperopic myopic and emmetropic patients with customized aspheric ablation (Q factor) and micro-monovision. Int Ophthalmol. 2021;41(6):2179–2185. doi:10.1007/s10792-021-01775-4
25. Courtin R, Saad A, Grise-Dulac A, Guilbert E, Gatinel D. Changes to corneal aberrations and vision after monovision in patients with hyperopia after using a customized aspheric ablation profile to increase corneal asphericity (Q-factor). J Refract Surg. 2016;32(11):734–741. doi:10.3928/1081597X-20160810-01
26. Tabernero J, Klyce SD, Sarver EJ, Artal P. Functional optical zone of the cornea. Invest Ophthalmol Vis Sci. 2007;48(3):1053–1060. doi:10.1167/iovs.06-0867
27. Hou J, Wang Y, Lei Y, Zheng X. Comparison of effective optical zone after small-incision lenticule extraction and femtosecond laser-assisted laser in situ keratomileusis for myopia. J Cataract Refract Surg. 2018;44(10):1179–1185. doi:10.1016/j.jcrs.2018.06.046
28. Zhang JH, Wang SR, He YX, Yao BY, Zhang Y. The best optical zone for small-incision lenticule extraction in high myopic patients. J Cataract Refract Surg. 2020;46(9):1302–1307. doi:10.1097/j.jcrs.0000000000000282
29. Ozulken K, Kaderli A. The effect of different optical zone diameters on the results of high-order aberrations in femto-laser-assisted in situ keratomileusis. Eur J Ophthalmol. 2020;30(6):1272–1277. doi:10.1177/1120672119865688
30. Piao J, Li YJ, Whang WJ, et al. Comparative evaluation of visual outcomes and corneal asphericity after laser-assisted in situ keratomileusis with the six-dimension Amaris excimer laser system. PLoS One. 2017;12(2):e0171851. doi:10.1371/journal.pone.0171851
31. Goyal JL, Garg A, Arora R, Jain P, Goel Y. Comparative evaluation of higher-order aberrations and corneal asphericity between wavefront-guided and aspheric LASIK for myopia. J Refract Surg. 2014;30(11):777–784. doi:10.3928/1081597X-20141021-10
32. Llorente L, Barbero S, Merayo J, Marcos S. Total and corneal optical aberrations induced by laser in situ keratomileusis for hyperopia. J Refract Surg. 2004;20(3):203–216. doi:10.3928/1081-597X-20040501-03
33. Zhang J, Zheng L, Zhang Y, Wang K. Analysis of asphericity and corneal longitudinal spherical aberration of 915 Chinese myopic adult eyes. Clin Ophthalmol. 2023;17:591–600. doi:10.2147/OPTH.S404437
34. Zhang J, Zheng L, Zheng C, Sun P. A comparison of three cylindrical treatment strategies for topography-guided LASIK: manifest, topographic, and ZZ VR cylinders. Clin Ophthalmol. 2023;17:1335–1345. doi:10.2147/OPTH.S408101
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.