Back to Journals » Journal of Pain Research » Volume 13
Decreased Initial Peak Pain Sensation with Aging: A Psychophysical Study
Authors Daguet I, Bergeron-Vezina K, Harvey MP, Martel M, Coulombe-Leveque A , Leonard G
Received 11 April 2020
Accepted for publication 17 June 2020
Published 22 September 2020 Volume 2020:13 Pages 2333—2341
DOI https://doi.org/10.2147/JPR.S257791
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Michael Schatman
Ines Daguet,1,2 Kayla Bergeron-Vezina,1,2 Marie-Philippe Harvey,1,2 Marylie Martel,1,2 Alexia Coulombe-Leveque,1– 3 Guillaume Leonard1– 3
1Faculty of Medicine and Health Sciences, Université de Sherbrooke, Sherbrooke, QC, Canada; 2Research Centre on Aging, CIUSSS de l’Estrie - CHUS, Sherbrooke, QC, Canada; 3School of Rehabilitation, Faculty of Medicine and Health Sciences, Université de Sherbrooke, Sherbrooke, QC, Canada
Correspondence: Guillaume Leonard
Research Centre on Aging, CIUSSS de l’Estrie – CHUS, 1036, rue Belvédère Sud, Sherbrooke, Québec J1H 4C4, Canada
Tel +1 819-780-2220 Ext 45246
Fax +1 819-820-6864
Email [email protected]
Background and Purpose: Aging is associated with an impairment of diverse physiological functions, including nociception. For example, older adults in comparison to young adults, show an overall increase in pain thresholds, reflecting a decline in pain sensitivity and changes in the nociceptive pathways. These results are, however, debated as they were not always replicated depending on the stimulus modality, duration, and location. The aim of the current study was to determine how the temporal evolution of pain intensity during a continuous tonic heat pain test is influenced by aging. More specifically, we wanted to 1) assess the effect of age on initial peak and late-phase pain and 2) determine whether potential age effects depend on the stimulation site.
Participants and Methods: 13 young adults (average of 27.9 years old) and 13 older adults (average of 67.5 years old) participated in this study. Experimental heat pain was evoked on an appendicular (forearm) and axial (lower-back) body region, using a thermode (2-minute stimulation at a constant, individually-adjusted temperature). During the nociceptive stimulation, participants used a computerized visual analogue scale to continuously rate their pain.
Results: We show that initial peak (0– 30 seconds) pain sensation was significantly lower in older adults compared to young adults, while late-phase (30– 120 seconds) pain sensation was similar across the two age groups. These results hold true for both stimulation sites, suggesting the existence of an age effect on both appendicular and axial body regions.
Conclusion: The lower magnitude of initial peak pain observed in older adults, which affects both appendicular and axial body regions, could reflect generalized peripheral or central alterations of the nociceptive system in older adults. These alterations in older adults could have significant clinical impacts, such as an increased vulnerability to injury or an underestimation of the severity of their pain condition.
Keywords: pain, experimental pain, age, aging, elderly, psychophysics
Introduction
Aging is associated with a wide range of functional and anatomical changes, ranging from cognitive impairment to neurochemical alterations and brain volume reductions.1 These functional and anatomical age-related changes can also affect pain perception. Indeed, aging appears to be associated with increased pain thresholds,2,3 reflecting decreased pain sensitivity. The prevalence of chronic pain, however, increases in older adults.4 This apparent contradiction highlights the complex and multidimensional character of pain, and suggests that aging does not have a general effect on the nociceptive system, but rather affects differently various aspects of the painful experience.
A recent meta-analysis conducted by Lautenbacher et al (2017) summarizes the numerous studies conducted on the effect of age on pain perception and tolerance thresholds and revealed that while aging appears to be related to increased pain perception thresholds (a more intense stimulus is required for the pain to be felt), aging has no effect on pain tolerance thresholds (the stimulus intensity that can be tolerated is unaffected).2 However, a different review by El Tumi et al (2017) suggests that the effect of age on pain perception may not be so straightforward, as it also depends on the type, duration, and location of the painful stimulus.5 In agreement with this view, Helme et al (2004) have identified that although older adults reported lower pain scores than young adults, this age-difference is of large amplitude for short 1 second stimulations and is less visible for longer stimulations, signifying that the duration of the stimulation plays a crucial role.6 Although their study did not assess the evolution of the pain intensity across time during a prolonged stimulation, their results suggest that aging affects the rapid initial pain response, but not the prolonged pain response. Furthermore, the effect of age on supra-threshold pain ratings remains unclear, as studies have reported either no effect of age,7 or a decreased pain intensity in older adults.8 Assessing the influence of aging on prolonged supra-threshold pain is essential, as these tonic pain tests better mimic a continuous pain sensation, which is present in real-life clinical conditions.9
The aforementioned studies2,3,5,7 have predominantly been conducted on appendicular/distal body regions (such as the arm or the leg); however the stimulation site has been suggested as having an important impact on findings.3 It therefore remains unclear whether the results summarized above can be generalized to axial body areas. The aim of the current study was to determine how the temporal evolution of pain intensity during a continuous tonic heat pain test is influenced by aging. More specifically we wanted to 1) assess the effect of age on initial peak and late-phase pain and 2) determine whether potential age effects depend on the stimulation site. We hypothesized that for both areas, initial but not late-phase pain sensations would be reduced in older adults compared to younger adults.
Methods
Participants
Thirteen young adults (21 to 39 years old; average of 27.9 ± 5.8 years old; 6 men) and 13 older adults (59 to 74 years old; average of 67.5 ± 4.1 years old; 6 men) took part in this study. To be included, participants had to be healthy with no cognitive impairments (able to understand verbal explanations), nor sensory impairments (normal sensitivity values according to the Von Frey monofilament sensory test). People suffering from a pain condition or having an existing neurological disorder were excluded. Participants were asked to refrain from consuming short-term analgesics 6 hours before testing, and caffeine or tobacco products 2 hours before testing. The experiment took place at the Research Centre on Aging (Sherbrooke, Quebec, Canada). Participants were all French-speaking, community-dwelling adults. All experimental procedures were carried out in accordance to the principles of the Declaration of Helsinki. The study was approved by the CIUSSS de l’Estrie-CHUS Research Ethics Committee (Approval #21-01-2016), and each participant provided written informed consent before taking part in the study.
Experimental Design
Participants took part in 2 experimental sessions (minimum 1-week interval between the sessions), during which a Peltier-type thermode (30×30 mm, TSA-II, Medoc Advanced Medical Systems) was used to induce prolonged experimental heat pain. The thermode was placed on the lower-back during the first session, and on the non-dominant forearm (in order to account for hand dominance effects) during the second session.10,11 The regions of the forearm (commonly used in previous studies2) and of the lower-back (well distanced from the forearm) were chosen to assess appendicular and axial pain sensitivity, respectively. Participants used a computerized visual analogue scale (CoVAS; Medoc Advanced Medical Systems, Minneapolis) ranging from 0 (no pain) to 100 (intolerable pain) to rate their pain using their dominant hand.12–14
Heat Pain Pre-Test
At the beginning of each experimental session, a pre-test was conducted to familiarize participants with the CoVAS and the Peltier-type thermode (Medoc Advanced Medical Systems, Minneapolis; for similar procedures15–18) and to determine the stimulation temperature to be used for the tonic heat pain test. During the pre-test, the thermode temperature was gradually increased from 32 °C to 51 °C (rising rate = 0.3 °C/sec) while participants used the CoVAS to continuously rate their pain. Instructions were to start moving the CoVAS cursor at the first feeling of pain (pain perception threshold) and to have the cursor reach the right end of the scale when the pain became unbearable (100/100; pain tolerance threshold). This procedure was repeated (3 times on average) until pain reports were consistent between trials (≤ 1 °C difference for pain perception and pain tolerance thresholds). The thermode temperature used during the subsequent experimental heat pain test was determined by selecting the temperature for which the participant had rated the pain intensity at 50/100 with the CoVAS (for similar procedures15–18). To avoid pain sensitization, the thermode was applied on adjacent regions of the lower-back or the forearm (never on the exact same site).
Tonic Heat Pain Test
For the tonic heat pain test, the thermode was applied for two minutes on the lower-back region (first session) and on the non-dominant forearm (second session). Sessions were not randomized as this study was part of a larger scale project. Participants used the CoVAS to continuously rate their pain during each test (CoVAS sampling rate = 10 Hz). The temperature was individually adjusted, according to pre-test results, to induce a pain intensity of approximately 50/100 (± 15/100) for each participant and body region. The thermode temperature increased from 32 °C to the individually adjusted temperature at a rate of 5 °C/sec (heat-pain coupling). Once the targeted temperature was reached, the thermode temperature remained constant throughout the whole 2-minute test. Participants, however, were told that the thermode temperature could rise, remain stable, or decrease during the test, in order to ensure that their perception was not biased by expectations. The reliability of such a tonic heat pain protocol is well established19,20 and continuous noxious stimulations (such as tonic heat pain tests) are believed to better mimic clinical pain9 in comparison to phasic stimulations or pain threshold measures.
Sample Size and Statistical Analysis
The tonic heat pain test used in this study allows the assessment of pain dynamics by separating the 2-minute pain test into two time epochs defined as initial peak and late-phase pain.7,16,18,21 In order to conduct statistical analyses, we decided on a cut-off between the two phases at 30 seconds (initial peak pain: 0–30 seconds; late-phase pain: 30–120 seconds). This decision was based on visual inspection of the data and on previous works.16,22 To confirm the validity of this analysis, we also divided the late-phase segment into three sub-epochs (30s - 60s; 60s - 90s and 90s - 120s), and analysed these sub-epochs separately. The pain intensity ratings obtained during the initial peak pain and late-phase pain of the 2-minute tonic heat-pain test were averaged for each participant, and the mean was used in subsequent analyses. The heat-pain coupling phase, corresponding to the increase in thermode temperature before the targeted temperature was reached, was not included in the analysis.
The study was designed to detect a between-group difference of 20 points on the CoVAS (minimal clinically important change).23 To detect this difference, with a statistical power of 80% and a significance level of 5%, we determined that 13 young and 13 older adults should be enrolled in the study (estimated standard deviation of 18, based on preliminary results). Given the small number of participants and because visual inspection of the histograms did not allow us to assume that the data were normally distributed, nonparametric tests (Mann–Whitney; bilateral significance) were used to compare pain intensity between the young and older groups. Statistical differences were considered significant if p < 0.05 was obtained. Effect size values were reported for each statistical test; a large effect was defined as | r | > 0.5, a medium effect as | r | > 0.3, and a small effect as | r | > 0.1.24 Unless otherwise indicated, all results are reported as average ± SD. All tests were performed using SPSS (version 19.0 for Windows, Chicago, IL, USA).
Results
Thirteen young participants (27.9 ± 5.8 years old), and 13 older adults (67.5 ± 4.1 years old) completed the study (Table 1). The mean age difference between the young and the older group was 40 years (p < 0.0001), confirming a distinct age difference between the two groups. Stimulation temperatures were comparable between young and older participants, both for the back and the forearm (all ps > 0.65). The mean pain intensity (averaged over the whole 2-minute pain test) did not differ between young and older participants, regardless of the stimulus location (all ps > 0.45). This absence of difference in pain intensity was expected, as the study was designed to induce moderate pain in both age groups (individually-adjusted thermode temperature, see Methods).
 |
Table 1 Characteristics of the Participants in the Young and the Older Group |
Pain responses obtained from forearm stimulations are presented in Figure 1. The temporal evolution of pain intensity throughout the 2-minute forearm stimulation is depicted in Figure 1A, and appears higher in young participants compared to older participants during the early part of the stimulation, but similar in the two groups in the later part of the stimulation. The average intensity from the first 30 seconds (Figure 1B) and the remaining 90 seconds (Figure 1C) was compared between the two groups; results confirmed that pain intensity was higher in the young group compared to the older group for the first 30 seconds (Figure 1B; p = 0.003; r = - 0.59) but not for the remaining 90 seconds (Figure 1C; p = 0.37; r = - 0.18). Within this 90s segment, the mean pain intensity of each of the three sub-epochs (30s - 60s; 60s - 90s and 90s - 120s) was comparable between young and older adults (all ps > 0.28; - 0.22 < all rs < 0).
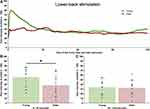
Pain responses obtained from back stimulations are presented in Figure 2, and show a similar temporal pattern to pain responses obtained from forearm stimulation (Figure 2A), wherein pain intensity was higher in the young group compared to the older group for the first 30 seconds (Figure 2B; p = 0.03; r = - 0.42) but not for the remaining 90 seconds (Figure 2C; p = 0.82; r = - 0.05). For both groups, pain intensity was similar across all three sub-epochs (30s - 60s; 60s - 90s and 90s - 120s; all ps > 0.73; - 0.08 < all rs < 0).
Discussion
The aim of this study was to assess the effect of age on heat pain dynamics (initial peak and late-phase pain sensations) on two different body areas: forearm and lower-back. In agreement with our hypothesis, our results show that initial peak pain but not late-phase pain is decreased in older adults on both the forearm and lower-back. These results are consistent with previous studies reporting that aging is associated with a reduced sensation of “sharpness”25 and a diminished initial component of pain.7 Our findings not only replicate those of Tousignant Laflamme and colleagues (2012) in their study on forearm heat pain stimulation in women,7 but also extend them to both men and women, and to different body regions (forearm and lower-back). The repeatability of this result on two body sites confirms the existence of an age effect on both appendicular and axial body regions. Consequently, these results suggest an alteration of the initial sensory-discriminative pain response (as opposed to the late sensory-discriminative component) that is independent of body region.
At first sight, the absence of difference between the two groups in terms of targeted stimulation temperature (≃ 46.5 °C) and average pain intensity (≃ 40/100) appears to indicate that there is no effect of age on pain sensitivity. However, a closer analysis reveals decreased initial peak pain sensations in older adults, but no difference in late-phase pain sensations between the two groups. These results highlight the importance of looking at the temporal dynamics of pain sensitivity, rather than just at the average sensation. Moreover, the differential effect of age on initial and late-phase pain we observed suggests that the tonic heat pain test activates at least two distinct nociceptive “circuitries”, which are differently altered with aging. Indeed, prolonged or repeated heat pain stimulations provoke nociceptive responses which evolve across time. In terms of response dynamics, previous studies suggested that different phases can be identified (including peak pain, adaptation, habituation and temporal summation).7,16,26,27 We showed that initial pain (peak pain and the subsequent adaptation) was significantly lower in older adults compared to young adults. A decrease of this initial “rise and fall” pattern in older adults, which is typically observed at the start of a tonic heat pain test,7,16,18 suggests that the pain circuitry responsible for this initial pain sensation is modified in older adults. In contrast, we observed that late-phase pain (habituation and temporal summation) was similar across the two groups, which suggests that the circuitry responsible for this late-phase sensation remains relatively intact with aging. If the exact same circuitry was responsible for both sensations (initial peak and late-phase pain), we would expect that the difference between the two groups would be similar for the two sensations. That a between-group difference was observed for only one of the two sensations, and not both, leads us to believe that the mechanisms underlying initial and late-phase sensations are different, and that only the former is affected by aging.
Aging has been associated with morphological1 and functional25,28 alterations of the central nervous system, both at the spinal and at the supra-spinal level. At the supra-spinal level, functional brain imaging studies suggest that aging is associated with reduced activity in two regions of the pain matrix, the primary somatosensory cortex (S1) and the insular cortex,25 during a painful heat stimulation. It is possible that this alteration of the nociceptive circuitry is involved in the changes in pain perception observed with aging.1,25,28 Increases in brain activity observed in the prefrontal areas of older adults during experimental heat pain may also play a role in this altered pain perception, via a possible relationship between pain and higher-order functions such as attention and cognition.28 These supra-spinal mechanisms are only two of the multiple processes that may explain the alteration of pain processing with aging. At the spinal level, age-related modifications impacting pain plasticity have also been noted.29 Previous studies have reported an increase in temporal summation with aging,27 as well as a preserved facilitation of pain and spinal nociceptive responses30 in older adults. In the current study, the absence of difference in the late-phase pain sensation between the two age groups suggests no modifications in terms of temporal summation with aging, which is coherent with previous tonic heat pain data7 and may be due to the duration of the stimulation. A longer tonic heat pain test (7 minutes9 for example) may have revealed differences in terms of habituation or temporal summation. An increase in temporal summation with aging may be one explanation for the higher prevalence of chronic pain in older adults.4
Age-related changes in pain perception may also originate at the peripheral level, from an alteration of nociceptive A-delta and C fibers. These nerve fibers are responsible for the transmission of the pain signal from the periphery to the central nervous system, generating the first sharp pricking pain sensation and the prolonged painful sensation that generally outlasts the stimulus.31 While aging seems to alter both myelinated A-delta and unmyelinated C fibers,2,32,33 experimental studies have highlighted a particularly detrimental effect of age on A-delta fibers.34,35 Kemp and collaborators (2014) reported longer somatosensory evoked potentials (SEP) latencies for myelinated A-delta fiber stimulation, but not for unmyelinated C fiber stimulation, in older adults when compared to young adults.35 This result is coherent with Sato et al’s (2012) observation that the conduction velocity of C fibers in rats does not vary with age.36 Together, these studies suggest that aging has a more pronounced effect on A-delta fibers than on C fibers. Some texts suggest that A-delta fibers are particularly involved in the first sharp sensation of pain evoked by a nociceptive stimulation37–39 (although other findings suggest that the two types of fibers share some overlap in function40,41). As such, though only hypothetical, it is possible that the decrease in A-delta fiber function observed in older adults plays a role in their decreased sensation of initial pain.7
This study has some limitations. First, only two body regions were tested, which does not allow us to conclude that initial peak pain sensations are altered homogeneously across the whole body. Second, even though the two age groups in our study were clearly differentiated (40 years of difference) and consistent with other studies on aging,15,17,42 the participants in the young group may have already been affected by aging,43 and the participants in the older group were relatively young (< 75 years old). It is therefore possible that even stronger age-effects may have been obtained with younger and older populations. Third, the two experimental conditions were not randomized, as they were part of a larger-scale study. However, as the two sessions were weeks apart and our main results concern between-group differences (and not between-session differences), we believe that this lack of randomization does not significantly jeopardize the validity of our results. Fourth, the choice of the temporal cut-off between the two phases (initial peak pain and late-phase pain), although based on previous works,16,22 was arbitrary and therefore can be discussed. Fifth, the two main interconnected pain components were not assessed independently, preventing us from determining if the age effect on pain sensitivity arose from the sensory-discriminative component or the emotional/affective component. However, contact heat induces significantly less unpleasantness than other modalities,44 lessening the possible implication of the emotional component.
The current results show that the effect of age on pain perception was not only statistically significant, but also clinically significant for the forearm and on the edge of clinical significance for the lower-back,23 suggesting that there are “real-life” implications to the age-related difference observed in this study. For example, this decreased pain sensation may make it more difficult for older adults to detect potentially harmful stimuli, rendering them more vulnerable to injury in everyday life. It may also result in decreased pain complaints in elderly patients, such that caretakers, researchers, and medical and rehabilitation professionals may underestimate the severity of their condition.45 On the other hand, it may be that young adults tend to overestimate peak pain intensity (due to the surprise), and that older adults, through their experience, have learnt to better estimate this initial pain.
Overall, our results show that following a continuous heat pain stimulation, initial peak but not late-phase pain sensation is less prominent in older adults compared to young adults. The lack of age-dependent differences between appendicular and axial body areas may be related to either central alterations of the nociceptive system in older adults, or generalized peripheral alterations (affecting both appendicular and axial body regions). These changes in acute pain sensitivity with aging need to be taken into account by healthcare professionals working in geriatrics, as they may have significant clinical impacts.
Acknowledgments
The authors would like to thank Marie-Claude Girard, Antoine Guillerand and Mathieu Hamel for their help with data collection.
Author Contributions
KB-V, MM, ID and GL contributed to the conception and design of the study. KB-V, M-PH and ID recruited the participants and collected the data. ID performed the statistical analysis. ID, ACL and GL interpreted the results. All authors took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version published; agreed on the journal to which the article was submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Farrell MJ. Age-related changes in the structure and function of brain regions involved in pain processing. Pain Med. 2012;13(suppl 2):S37–S43. doi:10.1111/j.1526-4637.2011.01287.x
2. Lautenbacher S, Peters JH, Heesen M, Scheel J, Kunz M. Age changes in pain perception: A systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev. 2017;75:104–113. doi:10.1016/j.neubiorev.2017.01.039
3. Gibson SJ, Farrell M. A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. Clin J Pain. 2004;20(4):227–239. doi:10.1097/00002508-200407000-00004
4. Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17(3):417–431. doi:10.1016/S0749-0690(05)70078-1
5. El Tumi H, Johnson MI, Dantas PBF, Maynard MJ, Tashani OA. Age-related changes in pain sensitivity in healthy humans: a systematic review with meta-analysis. Eur J Pain. 2017;21(6):955–964. doi:10.1002/ejp.1011
6. Helme RD, Meliala A, Gibson SJ. Methodologic factors which contribute to variations in experimental pain threshold reported for older people. Neurosci Lett. 2004;361(1–3):144–146. doi:10.1016/j.neulet.2003.12.014
7. Tousignant-Laflamme Y, Marchand S. Aging independently of the hormonal status changes pain responses in young postmenopausal women. Pain Res Treat. 2012;2012:1–7. doi:10.1155/2012/693912
8. Petrini L, Matthiesen ST, Arendt-Nielsen L. The effect of age and gender on pressure pain thresholds and suprathreshold stimuli. Perception. 2015;44(5):587–596. doi:10.1068/p7847
9. Naert ALG, Kehlet H, Kupers R. Characterization of a novel model of tonic heat pain stimulation in healthy volunteers. Pain. 2008;138(1):163–171. doi:10.1016/j.pain.2007.11.018
10. Neri M, Agazzani E. Aging and right-left asymmetry in experimental pain measurement. Pain. 1984;19(1):43–48. doi:10.1016/0304-3959(84)90063-0
11. Pud D, Golan Y, Pesta R. Hand dominancy—A feature affecting sensitivity to pain. Neurosci Lett. 2009;467(3):237–240. doi:10.1016/j.neulet.2009.10.048
12. Bird M-L, Callisaya ML, Cannell J, Gibbons T, Smith ST, Ahuja KD. Accuracy, validity, and reliability of an electronic visual analog scale for pain on a touch screen tablet in healthy older adults: a clinical trial. Interact J Med Res. 2016;5(1):e3. doi:10.2196/ijmr.4910
13. Moloney NA, Hall TM, O’Sullivan TC, Doody CM. Reliability of thermal quantitative sensory testing of the hand in a cohort of young, healthy adults. Muscle Nerve. 2011;44(4):547–552. doi:10.1002/mus.22121
14. Moloney NA, Hall TM, Doody CM. Reliability of thermal quantitative sensory testing: a systematic review. J Rehabil Res Dev. 2012;49(2):191–207. doi:10.1682/JRRD.2011.03.0044
15. Daguet I, Bergeron-Vézina K, Harvey M-P, Martel M, Léonard G. Transcutaneous electrical nerve stimulation and placebo analgesia: is the effect the same for young and older individuals? Clin Interv Aging. 2018;13:335–342. doi:10.2147/CIA.S152906
16. Tousignant-Laflamme Y, Pagé S, Goffaux P, Marchand S. An experimental model to measure excitatory and inhibitory pain mechanisms in humans. Brain Res. 2008;1230:73–79. doi:10.1016/j.brainres.2008.06.120
17. Bergeron-Vézina K, Corriveau H, Martel M, Harvey M-P, Léonard G. High- and low-frequency transcutaneous electrical nerve stimulation does not reduce experimental pain in elderly individuals. PAIN. 2015;156(10):2093–2099. doi:10.1097/j.pain.0000000000000276
18. Potvin S, Stip E, Tempier A, et al. Pain perception in schizophrenia: no changes in diffuse noxious inhibitory controls (DNIC) but a lack of pain sensitization. J Psychiatr Res. 2008;42(12):1010–1016. doi:10.1016/j.jpsychires.2007.11.001
19. Granot M, Granovsky Y, Sprecher E, Nir -R-R, Yarnitsky D. Contact heat-evoked temporal summation: tonic versus repetitive-phasic stimulation. Pain. 2006;122(3):295–305. doi:10.1016/j.pain.2006.02.003
20. Kong J-T, Johnson KA, Balise RR, Mackey S. Test-retest reliability of thermal temporal summation using an individualized protocol. J Pain. 2013;14(1):79–88. doi:10.1016/j.jpain.2012.10.010
21. Jensen MT, Petersen KL. Gender differences in pain and secondary hyperalgesia after heat/capsaicin sensitization in healthy volunteers. J Pain. 2006;7(3):211–217. doi:10.1016/j.jpain.2005.10.013
22. John Redmond W, Goffaux P, Potvin S, Marchand S. Analgesic and antihyperalgesic effects of nabilone on experimental heat pain. Curr Med Res Opin. 2008;24(4):1017–1024. doi:10.1185/030079908X280635
23. Farrar JT, Portenoy RK, Berlin JA, Kinman JL, Strom BL. Defining the clinically important difference in pain outcome measures. Pain. 2000;88(3):287–294. doi:10.1016/s0304-3959(00)00339-0
24. Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen. 2012;141(1):2–18. doi:10.1037/a0024338
25. Tseng M-T, Chiang M-C, Yazhuo K, Chao -C-C, Tseng W-YI, Hsieh S-T. Effect of aging on the cerebral processing of thermal pain in the human brain. Pain. 2013;154(10):2120–2129. doi:10.1016/j.pain.2013.06.041
26. Hashmi JA, Davis KD. Effects of temperature on heat pain adaptation and habituation in men and women. Pain. 2010;151(3):737–743. doi:10.1016/j.pain.2010.08.046
27. Edwards RR, Fillingim RB. Effects of age on temporal summation and habituation of thermal pain: clinical relevance in healthy older and younger adults. J Pain. 2001;2(6):307–317. doi:10.1054/jpai.2001.25525
28. Beach PA, Cowan RL, Dietrich MS, Bruehl SP, Atalla SW, Monroe TB. Thermal psychophysics and associated brain activation patterns along a continuum of healthy aging. Pain Med Malden Mass. 2019;pnz281. doi:10.1093/pm/pnz281
29. Farrell M, Gibson S. Age interacts with stimulus frequency in the temporal summation of pain. Pain Med. 2007;8(6):514–520. doi:10.1111/j.1526-4637.2007.00282.x
30. Marouf R, Piché M, Rainville P. Is temporal summation of pain and spinal nociception altered during normal aging? PAIN. 2015;156(10):1945–1953. doi:10.1097/j.pain.0000000000000254
31. Schmelz M. Neuronal sensitivity of the skin. Eur J Dermatol. 2011;21(S1):43–47. doi:10.1684/ejd.2011.1265
32. Namer B. Age related changes in human C-fiber function. Neurosci Lett. 2010;470(3):185–187. doi:10.1016/j.neulet.2009.07.023
33. Drac H, Babiuch M, Wiśniewska W. Morphological and biochemical changes in peripheral nerves with aging. Neuropatol Pol. 1991;29(1–2):49–67.
34. Chakour MC, Gibson SJ, Bradbeer M, Helme RD. The effect of age on A delta- and C-fibre thermal pain perception. Pain. 1996;64(1):143–152. doi:10.1016/0304-3959(95)00102-6
35. Kemp J, Després O, Pebayle T, Dufour A. Differences in age-related effects on myelinated and unmyelinated peripheral fibres: a sensitivity and evoked potentials study: different age-effect on sensory fibres. Eur J Pain. 2014;18(4):482–488. doi:10.1002/j.1532-2149.2013.00388.x
36. Sato A, Sato Y, Suzuki H. Aging effects on conduction velocities of myelinated and unmyelinated fibers of peripheral nerves. Neurosci Lett. 1985;53(1):15–20. doi:10.1016/0304-3940(85)90090-4
37. Marchand S. The Phenomenon of Pain. IASP Press; 2012.
38. Marchand S. Applied pain neurophysiology. In: Beaulieu P, Lussier D, Porreca F, Dickenson AH, editors. Pharmacology of Pain. IASP Press; 2010:3–26.
39. Price DD, Dubner R. Mechanisms of first and second pain in the peripheral and central nervous systems. J Invest Dermatol. 1977;69(1):167–171. doi:10.1111/1523-1747.ep12497942
40. Yeomans DC, Proudfit HK. Nociceptive responses to high and low rates of noxious cutaneous heating are mediated by different nociceptors in the rat: electrophysiological evidence. Pain. 1996;68(1):141–150. doi:10.1016/S0304-3959(96)03177-6
41. Treede RD, Meyer RA, Raja SN, Campbell JN. Evidence for two different heat transduction mechanisms in nociceptive primary afferents innervating monkey skin. J Physiol. 1995;483(3):747–758. doi:10.1113/jphysiol.1995.sp020619
42. Larivière M, Goffaux P, Marchand S, Julien N. Changes in pain perception and descending inhibitory controls start at middle age in healthy adults. Clin J Pain. 2007;23(6):506–510. doi:10.1097/AJP.0b013e31806a23e8
43. Bourisly AK, El-Beltagi A, Cherian J, Gejo G, Al-Jazzaf A, Ismail M. A voxel-based morphometric magnetic resonance imaging study of the brain detects age-related gray matter volume changes in healthy subjects of 21–45 years old. Neuroradiol J. 2015;28(5):450–459. doi:10.1177/1971400915598078
44. Rainville P, Feine JS, Bushnell MC, Duncan GH. A psychophysical comparison of sensory and affective responses to four modalities of experimental pain. Somatosens Mot Res. 1992;9(4):265–277. doi:10.3109/08990229209144776
45. Schofield P. Pain in older adults: epidemiology, impact and barriers to management. Rev Pain. 2007;1(1):12–14. doi:10.1177/204946370700100104
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.