Back to Journals » Clinical Interventions in Aging » Volume 15
Declined Functional Status Prolonged Hospital Stay for Community-Acquired Pneumonia in Seniors
Authors Chen H, Hara Y, Horita N, Saigusa Y, Hirai Y, Kaneko T
Received 12 June 2020
Accepted for publication 12 August 2020
Published 27 August 2020 Volume 2020:15 Pages 1513—1519
DOI https://doi.org/10.2147/CIA.S267349
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Walker
Hao Chen,1 Yu Hara,1 Nobuyuki Horita,1 Yusuke Saigusa,2 Yoshihiro Hirai,3 Takeshi Kaneko1
1Department of Respiratory Medicine, Yokohama City University Hospital, Kanazawa, Yokohama 236-0004, Japan; 2Department of Biostatistics, Yokohama City University Hospital, Kanazawa, Yokohama 236-0004, Japan; 3Department of Respiratory Medicine, Kanto Rosai Hospital, Kawasaki 211-8510, Japan
Correspondence: Hao Chen
Department of Respiratory Medicine, Yokohama City University Hospital, 3-9 Fukuura, Kanazawa, Yokohama 236-0004, Japan
Tel +81 45-352-7962
Fax +81 45-352-7963
Email [email protected]
Purpose: Among senior community-acquired pneumonia (CAP) survivors, functional status after hospitalization is often decreased. This study investigated the change of functional status affecting delayed discharge.
Patients and Methods: This retrospective observational study was conducted in two medical facilities from January 2016 to December 2018. Hospitalized CAP patients > 64 years old were divided into two groups: an early group discharged ≤ 1 week after ending antibiotic treatment and a delayed group discharged > 1 week after ending antibiotic treatment. The primary outcome was decline in functional status.
Results: The early group comprised 170 patients and the delayed group comprised 155 patients (median age: 78 vs 82 years; p = 0.007). Distribution of the causative microorganisms and initial prescription of antibiotics showed no significant differences in the two groups (p=0.38; p=0.83, respectively) More patients showed decline in functional status in the delayed group than the early group (16 (9.4%) vs 49 (31.6%), p< 0.001), even if rehabilitation was more frequently conducted (77 (45.3%) vs 118 (76.1%); p< 0.001). Higher medical expenses were observed in the delayed group ($8631 vs $3817, respectively; p< 0.001). Multivariable regression analysis of factors contributing delayed discharge revealed that decreased functional status, pneumonia severity index (PSI) categories, rehabilitation enrolled, aspiration and age were independently associated with delayed discharge (odds ratio 4.31, 95% confidence interval (CI) 2.32– 7.98; 2.34, 95% CI 1.43– 3.82; 15.96, 95% CI 4.56– 55.82 (PSI V vs II); 2.48, 95% CI 1.11– 5.98; and 1.03, 95% CI 1.01– 1.06; respectively).
Conclusion: Functional status decline was independently associated with extended hospitalization.
Keywords: community-acquired pneumonia, functional status, patient discharge, rehabilitation, senior
Introduction
The aging of populations around the world has been associated with increases in morbidity and mortality attributable to lung diseases. Advancing age increases the susceptibility to severe bacterial pneumonia. The annual incidence of community-acquired pneumonia (CAP) in the United States has recently been estimated as 248 cases per 10,000 adults, and the incidence of hospitalization for pneumonia was approximately 25 times higher among adults ≥80 years old than among adults 18–49 years old.1 CAP hospitalizations cost $13 billion USD annually, and this figure is expected to grow with the aging population.2 Japan has been the most rapidly aging society in the world, with a life expectancy of 80.1 years for men and 86.4 years for women.3 Pneumonia is the third highest cause of death, with most of these deaths occurring among seniors.4
Besides the high mortality, senior CAP patients also experience deteriorations of functional status (FS) during and after treatment, as an important component of quality of life for older adults and their caregivers.5 The prevalence of functional declines has been reported at 8.6% among CAP patients.6 Functional declines during or after hospitalization are associated with adverse health outcomes, prolonged hospital stays, more frequent episodes of early hospital readmission and even higher long-term mortality rates.7–10 Only a few studies have focused on changes in FS for seniors after hospitalization. The present study focused on changes of FS delaying discharge for CAP in seniors.
Methods
This study was a retrospective cohort study of inpatients admitted to a community-based hospital and a teaching hospital in Japan from January 2017 to December 2018. This study was approved by the institutional review boards of Yokohama City University Hospital and Kanto Rosai Hospital (reference numbers: B190600008 and KR2018-29, respectively) and conforms to the provisions of the Declaration of Helsinki (as revised in Brazil 2013). Written informed consent was obtained from participants before starting the study.
Patients
Senior patients hospitalized with CAP were divided into two groups: early discharge group, discharged ≤1 week after the end of antibiotic treatment; and a delayed discharge group, discharged >1 week after the end of antibiotic treatment. All enrolled cases had been diagnosed with CAP according to definitions in the American Thoracic Society/Infectious Diseases Society of America guideline.11 Patients who fulfilled all the following inclusion criteria were enrolled in the study: 1) age >64 years; 2) symptoms compatible with pneumonia (eg, fever, cough, sputum, pleuritic chest pain, or dyspnea); and 3) appearance of new pulmonary infiltrates consistent with pneumonia on chest X-ray or computed tomography. To ensure that all eligible cases were enrolled, study investigators screened the hospital database for International Classification of Diseases, 10th revision (ICD-10) codes and reviewed hospital medical records. Duration of antibiotic treatment was determined including both injections and oral anti-bacterial medicines. FS was assessed on admission and at discharge. Requirements for rehabilitation were determined on the day of admission.
Exclusion Criteria
Cases of healthcare-associated pneumonia (HCAP) and hospital-acquired pneumonia (HAP) were excluded.12 Repeated episodes of pneumonia in the same patient within a 2-week period were regarded as a single episode. Cases with complications that occurred during admission (myocardial infarction, femoral fracture, cerebral infarction, etc.) and that would have affected discharge from hospital were also excluded.
Outcomes
The primary outcome was change in FS, as evaluated using activities of daily living (ADL) by the Barthel Index13 (BI) (range, 0–100, in 5-point increments). ADL was graded into three categories according to BI: independent, BI 80–100; semi-dependent, BI 30–75; and dependent, BI 0–25. A decline in FS was defined as a decrease in ADL by ≥1 category. We also collected demographic information, duration of antibacterial treatment, comorbidities, laboratory values on admission, in-hospital mortality and site of acquisition. Comorbidities were identified according to the Charlson Comorbidity Index (CCI).14 Pneumonia severity index (PSI) score was calculated based on data obtained at the time of admission.15
Statistical Analyses
Results are presented as numbers and percentages or medians and interquartile ranges unless otherwise indicated. Groups were compared using Wilcoxon rank-sum tests. Candidate risk factors for delayed discharge and in-hospital mortality were selected as those showing values of p<0.2 between groups. Variables for inclusion in multivariable regression analysis were determined by stepwise regression analysis using modeling with the minimum corrected Akaike’s information criterion (AICc) in the forward direction. In all instances, two-tailed values of p<0.05 were considered indicative of statistical significance. Data analysis was performed using JMP software (version 12.0; SAS Institute, Cary, NC).
Results
We identified 1368 patients diagnosed with pneumonia. After excluding 1043 cases with reasons, the remaining 325 cases were included in the study, comprising 170 patients in the early group and 155 patients in the delayed group (Figure 1). Background characteristics of these patients are summarized in Table 1. Participants comprised 212 men (65.2%) and 113 women (34.8%), with a median age of 80 years. Patients in the delayed group were older and showed higher ratios of dementia, aspiration and higher PSI category. First-choice antibiotics showed no significant difference between groups (p=0.83).
 |
Table 1 Population Demographics and Characteristics of Patients with Early and Delayed Discharge |
 |
Figure 1 Flowchart for the study. |
The distribution of causative microorganisms is shown in Table 2. Of the 309 cases (95.1%) for which sputum culture was performed, causative microorganisms were revealed for 166 (53.7%). The top three causative microorganisms were Streptococcus pneumoniae (n=24, 14.1%), Klebsiella pneumoniae (n=11, 6.5%), and Pseudomonas aerogenes (n=8, 4.7%) in the early discharge group, and Staphylococcus aureus (n=15, 9.7%), K. pneumoniae (n=14, 9.0%) and S. pneumoniae (n=12, 7.7%) in the delayed discharge group. No significant differences in top 3 and overall frequencies of causative microorganisms were seen between groups (p=0.12; p=0.38; respectively). Blood cultures were obtained for 238 patients (73.2%), coincidentally comprising 119 patients from each group. Seven patients in each group showed positive blood cultures, with S. pneumoniae from 3 patients in each group. Results for the 4 remaining patients in each group were different.
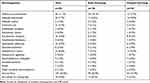 |
Table 2 Distribution of Causative Microorganisms in Sputum Cultures from Patients with Early and Delayed Discharge* |
Outcomes of patients are shown in Table 3. The delayed group showed a higher frequency of rehabilitation during hospitalization (n=118, 76.1%) than the early group (n=77, 45.3%; p<0.001), but still displayed a higher frequency of declines in FS (49, 31.6%) than the early group (n=16, 9.4%; p<0.001). Only a few patients (n=3, 1.9%) were discharged within 2 weeks and not quite half of patients could be discharged within 4 weeks in the delayed group. Accordingly, hospitalization expenses were significantly higher in the delayed group ($8631) than in the early group ($3817; p<0.001).
 |
Table 3 Outcomes and Costs of Patients with Early and Delayed Discharge |
Multivariable analyses of factors contributing to delayed discharge and in-hospital mortality are shown in Table 4. Decreased PS, enrolment for rehabilitation, PSI category, aspiration and age were independently associated with delayed discharge (odds ratio (OR) 4.31, 95% confidence interval (CI) 2.32–7.98; 2.34, 95% CI 1.43–3.82; 3.63, 95% CI 1.37–9.69 (PSI III vs II); 5.08, 95% CI 1.81–14.3 (PSI IV vs II), 15.96, 95% CI 4.56–55.8 (PSI V vs II); 2.48, 95% CI 1.11–5.98; and 1.03, 95% CI 1.01–1.06; respectively). Decreased PS, PSI V, aspiration and age were independently associated with in-hospital mortality (OR 21.6, 95% CI 5.1–119.1; 18.3, 95% CI 3.8–93.2; 4.61, 95% CI 1.35–16.22 and 1.04, 95% CI 1.01–1.09; respectively).
 |
Table 4 Multivariate Analysis of Factors Contributing to Delayed Discharge and In-Hospital Mortality |
Discussion
In this retrospective cohort study, decreased FS was observed more frequently in the delayed discharge group than in the early discharge group. After multivariable regression analysis, decreased FS was identified as an independent factor contributing to delayed discharge. Only a few patients in the delayed group could be discharged within 2 weeks, and more than half could not be discharged within 4 weeks. Decreased FS was considered to affect length of stay in both the short and long term after admission. In the delayed group, despite a higher frequency of enrolment to receive rehabilitation, declines in FS were also more frequent. Exercise or sports in midlife reduces the risk of functional limitations and disability,16,17 but effective methods of rehabilitation to prevent declines in FS remain unclear for seniors. A need for rehabilitation itself was found to prolong the length of stay.
Various severity scores have been used in assessing mortality for CAP, with PSI considered the best predictor. A higher PSI score has been associated with higher mortality.15,18 Length of stay is also influenced by comorbid conditions, as determined by PSI on presentation.19 Most patients who die from pneumonia are elderly, with multiple comorbidities and significant limitations in care put in place on or during admission. Surviving patients faced the additional problem of deteriorated general condition after severe pneumonia, requiring more time to recover, and thus prolonging the duration of hospitalization.
Aspiration pneumonia is a subclass of CAP that is expected to contribute increasingly to mortality and morbidity, particularly among elderly populations over the coming decades.20 Diagnosing aspiration pneumonia has been notoriously problematic, because standardized criteria for its diagnosis have yet to be established. Aspiration pneumonia is often diagnosed clinically, relying on the history and physical examination. Aspiration pneumonia accounts for 5–15% of CAP cases.21 Malnutrition, which has often been associated with aspiration pneumonia, was considered a factor inhibiting the recovery of patients.
People worldwide are living longer, and the proportion of the global population over 60 years old is predicted to nearly double by 2050. Aging is a major risk factor for the development of virtually every lung disease, with increased morbidity and mortality, while morbidities and mortalities from other prevalent diseases have declined or remained stable. Age-associated alterations not only decrease innate and adaptive immune responses, but also involve structural and functional deteriorations of most physiological systems, which may negatively impact the ability of the individual to carry out ADL.22
Previous studies have shown declines in FS after hospitalization are associated with adverse health outcomes, prolonged hospital stays and more frequent episodes of early hospital readmission.9,10 The combination of functional status and PSI has provided more accurate prognostic information for mortality than the use of each index separately.23 Our research revealed similar conclusions, identifying PSI and FS as independent factors of in-hospital mortality of pneumonia.
Limitations
Some limitations to this study need to be considered when interpreting the present results. First, this study was limited to two medical facilities. Second, we only included CAP patients, and divided patients into two groups determined by the interval between end of antibiotic treatment and discharge. Viral pneumonia might not have been included in this study. FS in HCAP or HAP is also important for seniors, but remained unclear. Third, we divided FS into three categories, whereas continuous variables might be more informative. Fourth, due to the size of experimental samples, although no differences were seen in causative microorganisms or initial prescription of antibiotics overall between the two groups, the potential influences of microbiology and antibiotics on delayed discharge remain unclear.
Conclusions
Declined FS was independently associated with prolonged hospital stays among senior CAP survivors. Enrolment for rehabilitation, PSI, aspiration and age also played important roles in delayed discharge.
Abbreviations
CAP, community-acquired pneumonia; FS, functional status; ICD-10, International Classification of Diseases, 10th revision; HCAP, healthcare-associated pneumonia; HAP, hospital-acquired pneumonia; ADL, activities of daily living; BI, Barthel Index; CCI, Charlson Comorbidity Index; PSI, pneumonia severity index; AICc, corrected Akaike’s information criterion; OR, odds ratio; CI, confidence interval.
Funding
This study received no funding.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Jain S, Self WH, Wunderink RG, et al. Community-acquired pneumonia requiring hospitalization among U.S. adults. N Engl J Med. 2015;373(5):415–427. doi:10.1056/NEJMoa1500245
2. Brown JD, Harnett J, Chambers R, et al. The relative burden of community-acquired pneumonia hospitalizations in older adults: a retrospective observational study in the United States. BMC Geriatr. 2018;18(1):92. doi:10.1186/s12877-018-0787-2
3. Tokudome S, Hashimoto S, Igata A. Life expectancy and healthy life expectancy of Japan: the fastest graying society in the world. BMC Res Notes. 2016;9(1):482. doi:10.1186/s13104-016-2281-2
4. Ishiguro T, Kagiyama N, Uozumi R, et al. Risk factors for the severity and mortality of pneumococcal pneumonia: importance of premorbid patients’ performance status. J Infect Chemother. 2016;22(10):685–691. doi:10.1016/j.jiac.2016.07.008
5. Simone PM, Haas AL. Frailty, leisure activity and functional status in older adults: relationship sith subjective well being. Clin Gerontol. 2013;36(4):275–293. doi:10.1080/07317115.2013.788114
6. Kosai K, Izumikawa K, Imamura Y, et al. Importance of functional assessment in the management of community-acquired and healthcare-associated pneumonia. Intern Med. 2014;53(15):1613–1620. doi:10.2169/internalmedicine.53.2499
7. Kim SJ, Lee JH, Han B, et al. Effects of hospital-based physical therapy on hospital discharge outcomes among hospitalized older adults with community-acquired pneumonia and declining physical function. Aging Dis. 2015;6(3):174. doi:10.14336/AD.2014.0801
8. Jeon K, Yoo H, Jeong BH, et al. Functional status and mortality prediction in community-acquired pneumonia: functional status and mortality in CAP. Respirology. 2017;22(7):1400–1406. doi:10.1111/resp.13072
9. Murcia J, Llorens P, Sánchez-Payá J, et al. Functional status determined by Barthel Index predicts community acquired pneumonia mortality in general population. J Infect. 2010;61(6):458–464. doi:10.1016/j.jinf.2010.08.006
10. Tonkikh O, Shadmi E, Flaks-Manov N, et al. Functional status before and during acute hospitalization and readmission risk identification: functional status and readmission. J Hosp Med. 2016;11(9):636–641. doi:10.1002/jhm.2595
11. Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society Consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;4:S27–S72. doi:10.1086/511159
12. Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–e111. doi:10.1093/cid/ciw353
13. Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14(2):61–65.
14. Charlson M, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
15. Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336(4):243–250. doi:10.1056/NEJM199701233360402
16. Pettee Gabriel K, Sternfeld B, Colvin A, et al. Physical activity trajectories during midlife and subsequent risk of physical functioning decline in late mid-life: the Study of Women’s Health Across the Nation (SWAN). Prev Med. 2017;105:287–294. doi:10.1093/ageing/afi063
17. Monma T, Takeda F, Noguchi H, et al. Exercise or sports in midlife and healthy life expectancy: an ecological study in all prefectures in Japan. BMC Public Health. 2019;19(1):1238. doi:10.1186/s12889-019-7570-y
18. Ranzani OT, Prina E, Menéndez R, et al. New sepsis definition (sepsis-3) and community-acquired pneumonia mortality. A validation and clinical decision-making study. Am J Respir Crit Care Med. 2017;196(10):1287–1297. doi:10.1164/rccm.201611-2262OC
19. Cabre M, Bolivar I, Pera G, et al. Factors influencing length of hospital stay in community-acquired pneumonia: a study in 27 community hospitals. Epidemiol Infect. 2004;132(5):821–829. doi:10.1017/S0950268804002651
20. Rodriguez AE, Restrepo MI. New perspectives in aspiration community acquired pneumonia. Expert Rev Clin Pharmacol. 2019;12(10):991–1002. doi:10.1080/17512433.2019.1663730
21. Mandell LA, Niederman MS. Aspiration pneumonia. N Engl J Med. 2019;380(7):651–663. doi:10.1086/511159
22. Roberts CE, Phillips LH, Cooper CL, et al. Effect of different types of physical activity on activities of daily living in older adults: systematic review and meta-analysis. J Aging Phys Act. 2017;25(4):653–670. doi:10.1123/japa.2016-0201
23. Sanz F, Morales-Suárez-Varela M, Fernández E, et al. A composite of functional status and pneumonia severity index improves the prediction of pneumonia mortality in older patients. J Gen Intern Med. 2018;33(4):437–444. doi:10.1007/s11606-017-4267-8
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
