Back to Journals » Clinical, Cosmetic and Investigational Dermatology » Volume 12
Dairy consumption and acne: a case control study in Kabul, Afghanistan
Authors Aalemi AK , Anwar I, Chen H
Received 14 April 2019
Accepted for publication 27 May 2019
Published 1 July 2019 Volume 2019:12 Pages 481—487
DOI https://doi.org/10.2147/CCID.S195191
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jeffrey Weinberg
Ahmad Khalid Aalemi,1,2 Idris Anwar,3 Hongxiang Chen1
1Department of Dermatology, Union Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan 430022, China; 2Department of Epidemiology, Kabul University of Medical Sciences, Kabul 1001, Afghanistan; 3Department of Environmental Health, Kabul University of Medical Sciences, Kabul 1001, Afghanistan
Background: Previous observational studies suggest that the development of acne may be triggered by dairy intake.
Objective: This study aimed to investigate the association of dairy intake and acne in Kabul citizens.
Methods: From February to September 2018, 279 acne patients and 279 controls aged 10–24 years were enrolled in a case control study at the dermatologic outpatient department of Maiwand Teaching Hospital in Kabul City, Afghanistan. The acne severity was determined by a dermatologist using the Global Acne Severity Scale.
Results: The consumption of whole milk 3 days or more per week was associated with moderate to severe acne (OR =2.36, 95% CI, 1.39–4.01). The association for low fat milk was less marked than for whole milk (OR 1.95 CI, 1.10–3.45). The risk was increased in those with a family history of acne in siblings (OR =4.13, 95% CI, 2.55–6.69). The risk was reduced in subjects doing physical exercise. No association with smoking emerged. A protective effect was associated with chicken consumption (OR =0.27, 95% CI, 0.15–0.49). Consumption of chocolate and chips was positively associated with acne.
Conclusion: This study showed an association between high intakes of dairy products and acne in adolescence suggesting that dairy intake may be a factor contributing to acne.
Keywords: acne, milk, dairy, dietary, case-control study, Kabul
Introduction
Acne is one of the most common skin diseases in the world.1,2 A degree of acne affects nearly all people during adolescence, prevalence data ranges from 50% to 95%.3 Numerous factors are involved in the pathogenesis of acne such as genetics, sex hormones, psychological factors, and the environment.1,3,4 The influence of environmental factors, such as diet, in the pathogenesis of acne is still being clarified. Dietary factors, particularly sweets, chocolate, milk, and fat, are frequently regarded by patients and clinicians as a cause or aggravator of acne.5 However, there is still a paucity of scientific evidence to prove a causal relationship between diet and acne. Several studies identified a positive association between acne and consumption of total milk and skimmed milk,5–7 and suggested that hormones and bioactive molecules present in milk might be linked to this association.5 In 2012 Di Landro et al8 found that increased consumption of milk increased the risk of acne and the odds ratio was 1.78. In 2016 LaRosa et al9 found that consumption of low-fat/skimmed milk was significantly higher in acne patients than those with no acne. In 2017 Ulvestad et al10 found that full fat dairy products were associated with moderate and severe acne, the odds ratio was 4.81 for boys and 1.8 for girls. A recent meta-analysis of 14 studies found that whole milk, low fat milk, and any milk were positively associated with acne.11 Whereas the same author could not find any association between milk and acne in a Mendelian randomization study in adults.12 Despite the many studies that have been done, few of them were conducted in developing countries. Furthermore some of the previous studies have some methodological shortcoming such as low sample size. Therefore this study was aimed to investigate if there is any association between dairy products consumption and acne in Kabul citizens. To the best of our knowledge, our study is the first study about acne in Afghanistan.
Methods
This study used a case control study design to examine the association between dairy products consumption and acne in people aged 10–24 years attending the dermatologic outpatient department of Maiwand Teaching Hospital in Kabul City, Afghanistan. Maiwand Teaching Hospital is one of the oldest hospitals in Afghanistan and is affiliated to Kabul University of Medical sciences and located in the first district of Kabul city. Ethical approval was obtained from the institutional review board of Kabul University of Medical Science. All research was performed in accordance with relevant guidelines/regulations and written informed consent of the participants or their parents was taken. Based on the Epi Info software, sample size was calculated as 558 subjects by considering CI =95%, Power =80%, Odds ratio =1.64,8 percent of control exposed =50%. The acne group comprised of 279 patients having a diagnosis of moderate to severe acne. A dermatologist evaluated the severity of acne using the Global Acne Severity Scale.13 The control group was comprised of 279 subjects who attended the dermatology outpatient department for an ailment not related to acne such as nevus, warts, eczema, atopic dermatitis etc. Subjects previously diagnosed with eating disorder, diabetes mellitus and coronary artery diseases were excluded from the study. A pre-structured questionnaire was administered by a dermatologist during the visit to collect epidemiological data (age, sex, education, occupation, etc.), family history of acne, menstrual pattern, and personal habits (smoking, cannabis consumption, drug abuse, etc.). The food consumption habits were recorded using a food frequency questionnaire. Investigated food included whole milk (milk whose fat content is unaltered), low fat milk (milk whose fat content is reduced), cream of milk, ice-cream, cheese, chocolate, cake, potatoes, fresh fruit, fresh vegetable, meat, chicken, and egg. Weight and height were measured with light clothes and without shoes, using a standardized method. Body mass index was computed as weight (Kg)/height (m2). Physical exercise was defined as regular when the individual exercised at least 3 days in a week each lasting about 30 mins and resulting in sweating. Physical exercise on less than 3 days a week was categorized as occasional physical exercise. Being on a diet was defined as yes when the individual had been on a diet in the last year to lose weight.
Statistical analysis
Statistical analysis was done using Statistical package for Social Science (SPSS) version 21.0 (IBM Corporation, Armonk, NY, USA). The socio-demographic characteristics and general information were presented by percentage, mean and standard deviation. Univariate analysis between the cases and controls were done by using the chi-square test or Fisher’s exact test for categorical variables and the independent t-test for continuous variables. Logistic Regression Analysis was used to assess the strength of association between dependent and independent variables which were found to be associated with the dependent variable during the univariate analysis. At univariate analysis, all independent variables with p-value less than 0.20 were included in the model except sleep duration. Odds ratio (OR) and 95% confidence interval (CI) were calculated (backward method). A p-value <0.05 was considered as statistically significant.
Results
Table 1 shows the socio-demographic characteristics of the subjects in the case and control groups. The percentage of males in the acne group was 54.1% and that of the control group was 53.4%. The average age was 18.7 (SD 3.2) and 18.2 (SD 4.1) years for the case and control groups respectively. The mean BMI was 24.5±2.8 for case and 24.0±2.7 for control. A total of 13.3% and 16.5% were ex or current smokers in the acne and control groups respectively. Among the acne group 7.9% were occasional or regular cannabis users, while in the control group 6.8% were occasional or regular cannabis users, with no statistically significant differences between case and control. Almost one third of the subjects in the acne group (32.3%) and 30.1% of the control group were students (p=0.003). Physical exercise was more prevalent among the control group (8.6%) relative to the acne group (5.7%), with a significant difference (p<0.001). The proportion of subjects on a diet in the last year was higher among the control group (14.0%) relative to the acne group (5.0%), with a significant difference (p<0.001). A family history of acne in siblings was present in 48.3% and 20.0% of subjects in the acne and control group respectively (p<0.001). The average duration of sleep was 7.6±1.3 and 8.4±1.3 hours for the acne and control groups, respectively (p<0.001). Age at menarche were 12.8±0.7 and 12.7±0.8 years among the acne and control groups, respectively with no significant difference (p=0.35). Nearly all the cases had facial lesions (98.9%); 30.4% had lesions on the back, 17.9% on their chest, and 4.6% on their arms. Most of the cases had moderate acne (83.8%), only 16.1% had severe acne, and there was no mild acne among the cases. The average age of acne onset was 17.4±2.9 years, and the average duration of current acne was 14.6±12.9 months.
 |
Table 1 Socio-demographic characteristics of the participants according to their case-control status |
Table 2 shows the food frequency intake among subjects. One third of the subjects (32.4%) consumed whole milk (≥3 times per week), with higher consumption noted in the case group (p<0.001). Of note, the consumption of low fat milk in the case group was higher than in the control group but the difference was not statistically significant in the univariate analysis. One fifth of the subjects (19.8%) in the acne group consumed cream of milk (≥3 times per week), while this value for the control group was 10.8% (p=0.003). The consumption of ice-cream was higher among the subjects in the acne group relative to the control group (p<0.001). Overall, 47.4% of the subjects consumed egg (≥3 times per week), 63.4% chocolate, 37.3% cake, 44.3% potato chips, 31.4% pizza/bolani, 15.8% dry fruit, and 14.0% red meat, with significant differences observed between case and control groups (p<0.05). Consumption of chicken and fresh vegetables was higher among controls than cases (p<0.001 and p=0.001 respectively). There was no significant difference in consumption of yogurt among case and control groups.
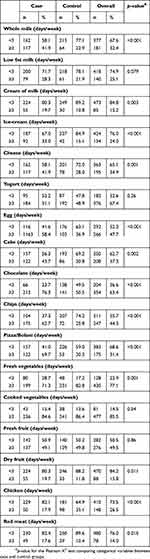 |
Table 2 Distribution of food intake frequency of participants according to their case and control status |
The results of multivariate analyses of variables associated with acne in the univariate analysis are shown in Table 3. The subjects in the acne group relative to the control group had 4.1 times higher odds of family history of acne (OR =4.13 [95% CI, 2.55–6.69]). The consumption of whole milk, 3 days or more in a week was 1360% higher among the acne group compared to control group (OR =2.36 [95% CI, 1.39–4.01]), similarly consumption of low fat milk was 95% higher among the acne group compared to the control group (OR =1.95 [95% CI, 1.10–3.45]). The following variables were also associated with acne: consumption of chocolate ≥3 days per week (OR =2.19 [95%CI, 1.36–3.53]), potato chips (OR =3.57 [95% CI, 2.20–5.80]), and egg (OR =1.95 [95% CI, 1.20–3.17]). The following variables were negatively associated with acne: being on a diet (OR =0.31 [95% CI, 0.13–0.74]), doing physical exercise regularly (OR =0.49 [95% CI, 0.29–0.84]) compared to occasionally or not doing any physical exercise, and consumption of chicken ≥3 days per week (OR =0.27 [95% CI, 0.15–0.49]). We did not find any other significant associations.
 |
Table 3 Results of the multivariate analysis of the variables associated with acne |
Discussion
Numerous studies in different countries have assessed the association of dairy products consumption and acne. Our study has found that consumption of certain products (whole and low fat milk, chocolate, potato chips, and egg), a family history of acne in first degree relatives (siblings), consumption of chicken, physical exercise, dieting, and sleep duration were associated with acne. The most affected body area by acne was the face, which is in line with the finding of Di Landro et al.8 Chest and back involvement was present in 30.4% and 17.9% of the cases respectively. Similar to other studies,5,14,15 we documented an association between whole and low fat milk consumption and acne. However, some studies found an association with low fat milk only.8,9 The association might be explained by the presence of milk derived amino acids which promote insulin secretion and induce hepatic insulin like growth factor-1 (IGF-1) synthesis.11,16 IGF-1 is known to stimulate the key factors involved in acne pathogenesis, including keratinocyte proliferation, sebocyte proliferation, and sebum production.17 It is also confirmed that IGF-1 plasma level is associated with acne severity.18
The association of chocolate consumption and acne, which was observed in our study, has also been confirmed by previous studies.19,20 Our findings showed an association between chips intake and acne. We could not find studies that assessed the association between potato chips and acne but a study by Wei et al21found an association of fried food with acne, and another study by Jung et al22 found an association with junk food. Consumption of egg was associated with acne in our study; we were unable to find studies on this. it is thought that this association could be due to high levels of leucine (8.5%) in egg.23 Leucine is believed to control the synthesis of lipids and proteins, which increase the activity of sebaceous glands and plugging of their ducts, respectively.24
The association of acne with family history of acne in first degree relative (parents and siblings) was confirmed by previous studies.8,15,25 However most of the subjects in our study were unaware of parent history of acne. We were only able to determine an association between acne and a history of acne in siblings.
Consumption of chicken and physical exercise was inversely associated with acne in our study. To our knowledge, no one has assessed the association of chicken consumption and physical exercise with acne. Further studies could investigate this association in different populations. Being on a diet was also inversely associated with acne. A study by Smith et al26 indicated that being on a low glycemic diet reduced the number of acne lesions. Fresh vegetable consumption was higher among controls than cases, however multivariate analysis showed no association between fresh vegetable consumption and acne.
The average duration of sleep was shorter in the case than in the control group in our study; this finding was consistent with other studies where they found that acne patients sleep less than controls.27,28
The mean BMI was higher among the acne than the control group; but the difference was not statistically significant. Similar studies confirmed that there is no association between BMI and acne.15,25,29,30 Tobacco smoking is another questioned association. We did not find any association between tobacco smoking and acne, possibly due to the low rate of smoking habits in our study. Some previous studies also did not find any association.25,30
The strengths of this study are: a large sample size, acne assessed by a dermatologist, demographic characteristics of both groups were similar, and the data were collected through face -to-face interview. Our study had some limitations as well, including case control design in which the causation cannot be determined, and self-report of food consumption.
The development of acne was positively associated with whole and low fat milk, whereas other types of dairy products had no associations. Chocolate and chips were also associated with acne but consumption of chicken, dieting, and physical exercise had negative associations in our study. We suggest that future studies on the association between chicken consumption and acne be done. Intervention studies will further clarify the association of milk consumption and acne.
IRB approval status
Reviewed and approved by Kabul University of Medical Science IRB; approval # 353/14-01-2018.
Disclosure
The authors have no conflicts of interest to declare in this work.
References
1. Bhate K, Williams HC. Epidemiology of acne vulgaris. Br J Dermatol. 2013;168(3):474–485. doi:10.1111/bjd.12149
2. Lynn DD, Umari T, Dunnick CA, Dellavalle RP. The epidemiology of acne vulgaris in late adolescence. Adolesc Health Med Ther. 2016;7:13–25. doi:10.2147/AHMT.S55832
3. Degitz K, Ochsendorf F. Acne. JDDG. 2017;15(7):709–722.
4. Williams HC, Dellavalle RP, Garner S. Acne vulgaris. Lancet. 2012;379(9813):361–372. doi:10.1016/S0140-6736(11)60321-8
5. Adebamowo CA, Spiegelman D, Danby FW, Frazier AL, Willett WC, Holmes MD. High school dietary dairy intake and teenage acne. J Am Acad Dermatol. 2005;52(2):207–214. doi:10.1016/j.jaad.2004.08.007
6. Aghasi M, Golzarand M, Shab-Bidar S, Aminianfar A, Omidian M, Taheri F. Dairy intake and acne development: a meta-analysis of observational studies. Clin Nutr. 2018;38(3):1067–1075. doi:10.1016/j.clnu.2018.04.015
7. Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in teenaged boys. J Am Acad Dermatol. 2008;58(5):787–793. doi:10.1016/j.jaad.2007.08.049
8. Di Landro A, Cazzaniga S, Parazzini F, et al. Family history, body mass index, selected dietary factors, menstrual history, and risk of moderate to severe acne in adolescents and young adults. J Am Acad Dermatol. 2012;67(6):1129–1135. doi:10.1016/j.jaad.2012.02.018
9. LaRosa CL, Quach KA, Koons K, et al. Consumption of dairy in teenagers with and without acne. J Am Acad Dermatol. 2016;75(2):318–322. doi:10.1016/j.jaad.2016.04.030
10. Ulvestad M, Bjertness E, Dalgard F, Halvorsen JA. Acne and dairy products in adolescence: results from a Norwegian longitudinal study. J Eur Acad Dermatol Venereol. 2017;31(3):530–535. doi:10.1111/jdv.13835
11. Juhl CR, Bergholdt HKM, Miller IM, Jemec GBE, Kanters JK, Ellervik C. Dairy intake and acne vulgaris: a systematic review and meta-analysis of 78,529 children, adolescents, and young adults. Nutrients. 2018;10(8):1049. doi:10.3390/nu10081049
12. Juhl CR, Bergholdt HKM, Miller IM, Jemec GBE, Kanters JK, Ellervik C. Lactase persistence, milk intake, and adult acne: a mendelian randomization study of 20,416 Danish adults. Nutrients. 2018;10(8):1041. doi:10.3390/nu10081041
13. Dreno B, Poli F, Pawin H, et al. Development and evaluation of a Global Acne Severity Scale (GEA Scale) suitable for France and Europe. J Eur Acad Dermatol Venereol. 2011;25(1):43–48. doi:10.1111/j.1468-3083.2010.03685.x
14. Adebamowo CA, Spiegelman D, Berkey CS, et al. Milk consumption and acne in adolescent girls. Dermatol Online J. 2006;12(4):1.
15. Ismail NH, Manaf ZA, Azizan NZ. High glycemic load diet, milk and ice cream consumption are related to acne vulgaris in Malaysian young adults: a case control study. BMC Dermatol. 2012;12:13. doi:10.1186/1471-5945-12-13
16. Mirdamadi Y, Thielitz A, Wiede A, et al. Insulin and insulin-like growth factor-1 can modulate the phosphoinositide-3-kinase/Akt/FoxO1 pathway in SZ95 sebocytes in vitro. Mol Cell Endocrinol. 2015;415:32–44. doi:10.1016/j.mce.2015.08.001
17. Melnik BC, Schmitz G. Role of insulin, insulin-like growth factor-1, hyperglycaemic food and milk consumption in the pathogenesis of acne vulgaris. Exp Dermatol. 2009;18(10):833–841. doi:10.1111/j.1600-0625.2009.00924.x
18. Rahaman SMA, De D, Handa S, et al. Association of insulin-like growth factor (IGF)-1 gene polymorphisms with plasma levels of IGF-1 and acne severity. J Am Acad Dermatol. 2016;75(4):768–773. doi:10.1016/j.jaad.2016.05.019
19. Poli F, Auffret N, Beylot C, et al. Acne as seen by adolescents: results of questionnaire study in 852 French individuals. Acta Dermato Venereologica. 2011;91(5):531–536. doi:10.2340/00015555-1125
20. Block SG, Valins WE, Caperton CV, Viera MH, Amini S, Berman B. Exacerbation of facial acne vulgaris after consuming pure chocolate. J Am Acad Dermatol. 2011;65(4):e114–e115. doi:10.1016/j.jaad.2010.08.015
21. Wei B, Pang Y, Zhu H, et al. The epidemiology of adolescent acne in North East China. J Eur Acad Dermatol Venereol. 2010;24(8):953–957. doi:10.1111/j.1468-3083.2010.03590.x
22. Jung JY, Yoon MY, Min SU, Hong JS, Choi YS, Suh DH. The influence of dietary patterns on acne vulgaris in Koreans. EJD. 2010;20(6):768–772. doi:10.1684/ejd.2010.1053
23. Millward DJ, Layman DK, Tome D, Schaafsma G. Protein quality assessment: impact of expanding understanding of protein and amino acid needs for optimal health. Am J Clin Nutr. 2008;87(5):1576s–1581s. doi:10.1093/ajcn/87.5.1576S
24. Melnik B. Dietary intervention in acne: attenuation of increased mTORC1 signaling promoted by Western diet. Dermato-Endocrinology. 2012;4(1):20–32. doi:10.4161/derm.19828
25. Di Landro A, Cazzaniga S, Cusano F, et al. Adult female acne and associated risk factors: results of a multicenter case-control study in Italy. J Am Acad Dermatol. 2016;75(6):1134–1141.e1131. doi:10.1016/j.jaad.2016.06.060
26. Smith RN, Mann NJ, Braue A, Makelainen H, Varigos GA. A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. Am J Clin Nutr. 2007;86(1):107–115. doi:10.1093/ajcn/86.1.107
27. Suh DH, Kim BY, Min SU, et al. A multicenter epidemiological study of acne vulgaris in Korea. Int J Dermatol. 2011;50(6):673–681. doi:10.1111/j.1365-4632.2010.04726.x
28. Wu TQ, Mei SQ, Zhang JX, et al. Prevalence and risk factors of facial acne vulgaris among Chinese adolescents. Int J Adolesc Med Health. 2007;19(4):407–412.
29. Stewart TJ, Bazergy C. Hormonal and dietary factors in acne vulgaris versus controls. Dermato-Endocrinology. 2018;10(1):e1442160. doi:10.1080/19381980.2018.1442160
30. Burris J, Rietkerk W, Woolf K. Relationships of self-reported dietary factors and perceived acne severity in a cohort of New York young adults. J Acad Nutr Diet. 2014;114(3):384–392. doi:10.1016/j.jand.2013.11.010
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
