Back to Journals » Clinical Ophthalmology » Volume 14
Cylinder Axis Agreement: Unexpected Scenarios
Authors Nabil KM
Received 7 November 2019
Accepted for publication 4 March 2020
Published 31 March 2020 Volume 2020:14 Pages 977—984
DOI https://doi.org/10.2147/OPTH.S237757
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Karim Mahmoud Nabil
Department of Ophthalmology, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Correspondence: Karim Mahmoud Nabil
Department of Ophthalmology, Faculty of Medicine, University of Alexandria, Alexandria, Egypt
Email [email protected]
Background: The purpose of this retrospective study was to evaluate cylinder axis agreement between manifest refraction (MR), cycloplegic refraction (CR), Allegro Oculyzer ІІ and Allegro Topolyzer-Vario.
Methods: We included 82 patients (32 males and 50 females, 28.1 ± 8.7 years old), with 156 eyes scheduled for wavefront optimized laser refractive surgery, photorefractive keratectomy (PRK) in 50 eyes and laser-assisted in situ keratomileusis (LASIK) in 106 eyes, for correction of simple, myopic, hyperopic or mixed astigmatism. Cylinder axis was determined under manifest and cycloplegic refractions and using Allegro Occulyzer ІІ and Allegro Topolyzer-Vario platforms. Cylinder axis agreement was assessed by intraclass correlation coefficient, Pearson correlation coefficient and by the method described by Bland and Altman.
Results: Intraclass correlation coefficient and Pearson correlation coefficient showed statistically significant cylinder axis agreement between manifest refraction, cycloplegic refraction, Allegro Oculyzer ІІ and Allegro Topolyzer-Vario (p < 0.001). Despite statistically significant cylinder axis agreement between the four measuring tools, 4 of 156 eyes (2.5%) showed unexpected discrepancy between Allegro Oculyzer ІІ and Allegro Topolyzer-Vario cylinder axis.
Conclusion: Although cylinder axis shows statistically significant agreement between manifest refraction, cycloplegic refraction, Allegro Oculyzer ІІ and Allegro Topolyzer-Vario, unexpected discrepancies occur.
Keywords: manifest refraction, cycloplegic refraction, Allegro Oculyzer ІІ, Allegro Topolyzer-Vario, PRK, LASIK
Introduction
Laser refractive surgery, including photorefractive keratectomy (PRK) and laser-assisted in situ keratomileusis (LASIK), gained global establishment as a reliable and safe procedure for correction of refractive errors.1,2
Laser refractive surgery is undergoing great evolutions, including excimer laser current flying spot technology, enhanced intraoperative pupillary tracking mechanism and cyclorotation adjustment.3–5 The WaveLight EX500 (Alcon Laboratories; Ft Worth, TX, USA), the recent excimer laser evolution, applies a 1050 Hertz (Hz) multidimensional active tracking system with estimated 2 milliseconds (ms) latency and pupillary size tracking ability ranging from 1.5 mm to 8 mm.6
The term “wavefront optimized” was introduced to describe aspherical ablation profiles attempting to eliminate or reduce spherical aberration associated with myopic laser refractive correction.7
The majority of refractive surgeons rely on clinical refraction, manifest or cycloplegic; however, this refractive data occasionally shows difference from topography, regarding cylinder axis. Some surgeons advocated clinical refractive data adjustment with topography, introducing the new term “topography-modified refraction”.8
Cylinder axis significance is not solely related to laser refractive surgery; it represents a cornerstone in lenticular refractive surgery, phakic intraocular lens (IOL) implantation or refractive lens exchange, particularly toric IOL. Similarly, cylinder axis determination is a crucial step in contact lens fitting.
Multiple factors might influence the accurate measurements of corneal astigmatism such as tear film stability, xerophthalmia, ocular surface status and corneal epitheliopathy. In addition, soft or hard contact lens wear may alter the accuracy of corneal astigmatism measurements.
Currently, it is not clearly documented which instrument measures corneal astigmatism with the greatest reproducibility and repeatability, and whether available measuring modalities could be applied interchangeably. Therefore, multiple
Comparison studies were undertaken to determine reproducible and accurate methods for corneal astigmatism measurement.9
The aim of this study was to evaluate cylinder axis agreement between manifest refraction (MR), cycloplegic refraction (CR), Allegro Oculyzer ІІ and Allegro Topolyzer-Vario.
Methods
All patients were recruited from the Department of Ophthalmology, Faculty of Medicine, Alexandria University (Alexandria, Egypt). Informed consent was obtained from all patients. This study was approved by the Ethics of Research Committee, Faculty of Medicine, University of Alexandria, Egypt.
Recruited patients were scheduled for wavefront optimized laser refractive surgery, PRK or LASIK, for correction of simple, myopic, hyperopic or mixed astigmatism. Exclusion criteria were coexisting ocular pathologies, uncontrolled diabetes mellitus, collagen vascular diseases, pregnancy or breastfeeding, severe xerophthalmia, corneal dystrophies, forme fruste keratoconus, and keratoconus.
Preoperative Examination
All patients underwent manifest and cycloplegic refractions by a TOPCON RM-8900 Auto Refractometer (Topcon Medical Systems, Tokyo, Japan), measurements of the uncorrected visual acuity (UCVA) and best spectacle-corrected visual acuity (BSCVA).
All eyes were subjected to corneal topography assessment by Allegro Topolyzer-Vario (WaveLight, Erlangen, Germany) and Scheimpflug tomography examination by Allegro Oculyzer ІІ (WaveLight, Erlangen, Germany). The Oculyzer presents a Scheimpflug rotating camera, with a 360 degrees rotating light beam, scanning the cornea with a high density of points from the corneal centre. In contrast, the Topolyzer is a placido-disk-based system with a camera imaging reflections from the surface of the cornea. Since the Topolyzer camera is located at the centre of the topographer, a central scotoma is produced corresponding to the camera location, and hence a small area of central corneal data are extrapolated.10
Patients enrolled in the study had pre-operative pachymetry ≥460 microns (μm) for PRK and ≥500 μm for LASIK. PRK subjects were required to retain an average post-operative residual corneal bed ≥380 μm. LASIK subjects were required to retain an average post-operative residual corneal bed ≥300 μm.
Operative and Postoperative Data
All patients underwent wavefront optimized laser refractive surgery, PRK in 50 eyes and LASIK in 106 eyes, for correction of simple, myopic, hyperopic or mixed astigmatism, applying WaveLight EX500 (Alcon Laboratories; Ft Worth, TX, USA). All surgeries were performed by a single surgeon, the author. A superior hinge was applied in LASIK cases using Moria Evolution 3 Microkeratome (Moria, Antony, France) with a programmed planned flap thickness of 110 μm and a diameter of 8 mm. In PRK, the corneal epithelium was removed in a diameter of 8 mm in a centripetal fashion using a blunt hockey blade. UCVA and manifest refraction were evaluated at 1 month post-operatively. Postoperative refraction was assessed by a TOPCON RM-8900 Auto Refractometer (Topcon Medical Systems, Tokyo, Japan).
Statistical Analysis of the Data
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). Intraclass correlation coefficient (ICC) and Pearson correlation coefficient were used to assess agreement. A p value less than 0.05 was considered statistically significant. Cylinder axis agreement was also studied using the method described by Bland and Altman. This method also computed 95% limits of agreement (LoA=mean difference ± 1.96SD).
Results
The present study was conducted on 82 patients 32 (39%) males and 50 (61%) females and involved 156 eyes scheduled for wavefront optimized laser refractive surgery, PRK in 50 eyes and LASIK in 106 eyes, for correction of simple, myopic, hyperopic or mixed astigmatism. The age of the studied patients ranged from 18 to 49 years (28.1 ± 8.7 years). (Table 1)
 |
Table 1 Distribution of the Studied Cases According to Different Parameters (n = 156) |
Intraclass correlation coefficient and Pearson correlation coefficient showed statistically significant cylinder axis agreement between manifest refraction (MR), cycloplegic refraction (CR), Allegro Oculyzer ІІ and Allegro Topolyzer-Vario (p <0.001*). (Tables 2 and 3) (Figure 1).
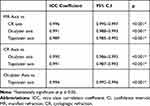 |
Table 2 Intra Class Correlation Coefficient for Cylinder Axis Agreement |
 |
Table 3 Pearson Correlation Coefficient for Cylinder Axis Agreement |
Despite statistically significant cylinder axis agreement between the four measuring tools, 4 of 156 eyes (2.5%) (3 patients) showed unexpected discrepancy between Allegro Oculyzer ІІ and Allegro Topolyzer-Vario cylinder axis (Figure 2). In these cases, the cylinder axis applied for laser treatment was the mean of the four measurements. One month postoperatively, these cases showed 0 cylinder with UCVA 1. In the first case, MR cylinder axis was 104, CR cylinder axis was 94, Allegro Oculyzer ІІ cylinder axis was 136 and Allegro Topolyzer-Vario cylinder axis was 88. The cylinder axis applied for laser treatment was the mean of the four values 105. In the second case, MR cylinder axis was 52, CR cylinder axis was 15, Allegro Oculyzer ІІ cylinder axis was 38 and Allegro Topolyzer-Vario cylinder axis was 5. The cylinder axis applied for laser treatment was the mean of the four values 28. In the third case, MR cylinder axis was 100, CR cylinder axis was 100, Allegro Oculyzer ІІ cylinder axis was 49 and Allegro Topolyzer-Vario cylinder axis was 152. The cylinder axis applied for laser treatment was the mean of the four values 100. In the last case, MR cylinder axis was 97, CR cylinder axis was 95, Allegro Oculyzer ІІ cylinder axis was 155 and Allegro Topolyzer-Vario cylinder axis was 134. The cylinder axis applied for laser treatment was the mean of the four values 120.
 |
Figure 2 Allegro Oculyzer ІІ and Allegro Topolyzer-Vario cylinder axis disagreement in four studied cases. |
Discussion
The Alcon/WaveLight refractive surgery laser platform comprises the EX500 excimer laser, and a series of diagnostic networked devices that constitute the Refractive Suite® (including Allegro Placido Topolyzer-Vario and Allegro Scheimpflug Oculyzer ІІ).11
This Refractive Suite applies ethernet networking, allowing diagnostic data import from networked screening devices into the laser planning software, including topography data from Allegro Placido Topolyzer-Vario and topometric data from Allegro Scheimpflug Oculyzer ІІ.12 Multiple studies reported the application of topography-guided treatment with such platforms, whether in normal or irregular corneas.13–20
The Oculyzer presents a Scheimpflug rotating camera, with a 360 degrees rotating light beam, scanning the cornea with a high density of points from the corneal centre. Therefore, it should be the first choice when planning laser treatment in corneas with central irregularities or aberrations. However, it can be affected by ocular movement or corneal haze or cloudiness.10
In contrast, the Topolyzer is a placido-disk-based system with a camera imaging reflections from the surface of the cornea. Since the Topolyzer camera is located at the centre of the topographer, a central scotoma is produced corresponding to the camera location, and hence a small area of central corneal data are extrapolated.
Therefore, it should be the first choice when planning laser treatment in corneas with more peripheral irregularities or aberrations. However, it lacks the provision of full surface information, with lower accuracy in cases of central corneal aberrations.10
A recent study by Cummings et al showed that both the Oculyzer and Topolyzer provide reliable and comparable results in pre-operative myopes and in subjects with mixed astigmatism.10 This coincides with the present study, where statistically significant agreement between Allegro Oculyzer ІІ and Allegro Topolyzer-Vario was detected.
In a recent study by Kanellopoulos, clinical refractive data were modified with topographic data, considering cylinder axis and amount, introducing the new term “topography-modified refraction”. This provided superior visual function regarding UCVA, residual refractive error, total high-order aberrations, coma aberration, and contrast sensitivity. He hypothesized that “topography-modified refraction” allows to bypass the bias induced by lenticular astigmatism, particularly active in young myopic patients. Such hypothesized lenticular astigmatism seems to be responsible for the distortion of the objective cylinder axis and amount.8
Numerous comparative studies were undertaken to correlate between corneal measurements using variable techniques. Lee et al21 reported that corneal astigmatism measurements obtained via partial coherence interferometry, automated keratometry, Orb scan slit topography, iTrace ray tracing, and Pentacam Scheimpflug imaging were comparable to manual keratometric measurements, concluding possible interchangeable application of these instruments for assessment of corneal astigmatism. Another study addressed the accuracy of preoperative astigmatism measurements in cases of toric IOL and concluded non-significant difference between manual keratometry, automated keratometry, Pentacam Scheimpflug imaging or partial coherence interferometry.22 Similarly, Shirayama et al23 reported comparable corneal astigmatism measurements obtained using manual keratometry, partial coherence interferometry, Atlas placido-based topographer, and Galilei Dual Scheimpflug analyzer. On the other hand, Visser et al24 reported poor agreement considering the vector of corneal astigmatism between Pentacam Scheimpflug imaging, manual keratometer, partial coherence interferometer, placido-based corneal topographer, or optical low coherence reflectometer. Similarly, Crawford et al25 reported limited agreement between Orb scan slit topographer and Pentacam Scheimpflug imaging or Galilei Dual Scheimpflug analyzer in both steep and flat keratometric measurements.
Taking these comparative studies into consideration demonstrates considerable variability in corneal measurements obtained using various instruments. Behshad et al recommended the comparison of data from more than one measuring modality, looking for agreement, in order to confirm the magnitude and axis of corneal astigmatism in order to minimize errors, in cases of toric IOL implantation.26
Similarly, Browne et al27 assessed absolute sphere, astigmatism amount, and steepest cylindrical axis in 87 eyes (54 patients) undergoing toric IOL implantation, using manual keratometry and four automated keratometers. The mean of the five measurements for sphere, astigmatism amount, and steepest cylindrical axis were labeled meld sphere, meld astigmatism, and meld axis, respectively. Although Bland–Altman plots for statistical analysis yielded an insignificant difference from meld measurement for each parameter, the authors documented a disturbing number of outliers that might be overlooked if a single measurement modality was applied. Authors concluded that measurement errors can be dramatically reduced by averaging measurements from manual keratometry with any automated technology to make toric IOL selection more accurate.
This goes in agreement with the present study, where 4 of 156 eyes (2.5%) (3 patients) showed unexpected discrepancy between Allegro Oculyzer ІІ and Allegro Topolyzer-Vario cylinder axis. In these cases, the cylinder axis applied for laser treatment was the mean of the four measurements. 1 month postoperatively, these cases showed 0 cylinder with UCVA 1. In the first case, MR cylinder axis was 104, CR cylinder axis was 94, Allegro Oculyzer ІІ cylinder axis was 136 and Allegro Topolyzer-Vario cylinder axis was 88. The cylinder axis applied for laser treatment was the mean of the four values 105. In the second case, MR cylinder axis was 52, CR cylinder axis was 15, Allegro Oculyzer ІІ cylinder axis was 38 and Allegro Topolyzer-Vario cylinder axis was 5. The cylinder axis applied for laser treatment was the mean of the four values 28. In the third case, MR cylinder axis was 100, CR cylinder axis was 100, Allegro Oculyzer ІІ cylinder axis was 49 and Allegro Topolyzer-Vario cylinder axis was 152. The cylinder axis applied for laser treatment was the mean of the four values 100. In the last case, MR cylinder axis was 97, CR cylinder axis was 95, Allegro Oculyzer ІІ cylinder axis was 155 and Allegro Topolyzer-Vario cylinder axis was 134. The cylinder axis applied for laser treatment was the mean of the four values 120.
“These findings may change the current clinical paradigm of the optimal subjective refraction utilized in laser vision correction.”8
Conclusions
Although cylinder axis shows statistically significant agreement between manifest refraction, cycloplegic refraction, Allegro Oculyzer ІІ and Allegro Topolyzer-Vario, unexpected discrepancies occur.
Abbreviations
MR, manifest refraction; CR, cycloplegic refraction; PRK, photorefractive keratectomy; LASIK, laser-assisted in situ keratomileusis; Hz, Hertz; Ms, milliseconds; UCVA, uncorrected visual acuity; BSCVA, best spectacle-corrected visual acuity; μm, microns; ICC, intra class correlation coefficient; LoA, limits of agreement.
Data Sharing Statement
Datasets are available in additional supporting files by reasonable request to the author.
Ethics and Consent Statement
This study was approved by the Ethics of Research Committee (IRB 00007555, FWA 00015712), Faculty of Medicine, University of Alexandria, Egypt. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Written informed consent to participate in the study was obtained from all individual participants included in the study.
Consent
Written informed consent to publish the results of the study and identifying images or other personal or clinical details of participants that compromise anonymity was obtained from all individual participants included in the study.
Funding
No funding was obtained for this study and there were no sources of public or private financial support.
Disclosure
The author reports no financial or proprietary interest in a product, method, or material and declares no conflicts of interest in this work.
References
1. Kugler LJ, Wang MX. Lasers in refractive surgery: history, present, and future. Appl Opt. 2010;49(25):F1–F9. doi:10.1364/AO.49.0000F1
2. Lukenda A, Martinović ZK, Kalauz M. Excimer laser correction of hyperopia, hyperopic and mixed astigmatism: past, present, and future. Acta Clin Croat. 2012;51(2):299–304.
3. Vega-Estrada A, Alió JL, Arba Mosquera S, Moreno LJ. Corneal higher order aberrations after LASIK for high myopia with a fast repetition rate excimer laser, optimized ablation profile, and femtosecond laser-assisted flap. J Refract Surg. 2012;28(10):689–696. doi:10.3928/1081597X-20120921-03
4. Winkler von Mohrenfels C, Khoramnia R, Lohmann CP. Comparison of different excimer laser ablation frequencies (50, 200, and 500 Hz). Graefes Arch Clin Exp Ophthalmol. 2009;247(11):1539–1545. doi:10.1007/s00417-009-1102-x
5. Iseli HP, Mrochen M, Hafezi F, Seller T. Clinical photoablation with a 500-Hz scanning spot excimer laser. J Refract Surg. 2004;20(6):831–834. doi:10.3928/1081-597X-20041101-12
6. Matsuura T, Ikeda H, Idota N, Motokawa R, Hara Y, Annaka M. Anisotropic swelling behavior of the cornea. J Phys Chem B. 2009;113(51):16314–16322. doi:10.1021/jp907232h
7. de Ortueta D, Magnago T, Triefenbach N, Arba Mosquera S, Sauer U, Brunsmann U. In vivo measurements of thermal load during ablation in high-speed laser corneal refractive surgery. J Refract Surg. 2012;28(1):53–58. doi:10.3928/1081597X-20110906-01
8. Kanellopoulos AJ. Topography-modified refraction (TMR): adjustment of treated cylinder amount and axis to the topography versus standard clinical refraction in myopic topography-guided LASIK. Clin Ophthalmol. 2016;10:2213–2221. doi:10.2147/OPTH.S122345
9. Lee H, Kim T, Kim EK. Corneal astigmatism analysis for toric intraocular lens implantation: precise measurements for perfect correction. Curr Opin Ophthalmol. 2015;26:34–38. doi:10.1097/ICU.0000000000000119
10. Cummings AB, Mascharka N. Clinical outcomes after topography-based corneal laser surgery with the wavelight oculyzer and topolyzer platforms. J Refract Surg. 2010;26(7):478–485. doi:10.3928/1081597X-20090814-05
11. Kanellopoulos AJ, Asimellis G. Correlation between central corneal thickness, anterior chamber depth, and corneal keratometry as measured by oculyzer II and WaveLight OB820 in preoperative cataract surgery patients. J Refract Surg. 2012;22:1–6.
12. Kanellopoulos AJ. Topography-guided hyperopic and hyperopic astigmatism femtosecond laser-assisted LASIK: long-term experience with the 400 Hz eye-Q excimer platform. Clin Ophthalmol. 2012;6:895–901. doi:10.2147/OPTH.S23573
13. Han DC, Chen J, Htoon HM, Tan DT, Mehta JS. Comparison of outcomes of conventional WaveLight(®) Allegretto Wave(®) and Technolas(®) excimer lasers in myopic laser in situ keratomileusis. Clin Ophthalmol. 2012;6:1159–1168. doi:10.2147/OPTH.S29660
14. Celik HU, Alagöz N, Yildirim Y, et al. Accelerated corneal crosslinking concurrent with laser in situ keratomileusis. J Cataract Refract Surg. 2012;38(8):1424–1431. doi:10.1016/j.jcrs.2012.03.034
15. Kanellopoulos AJ. Long-term safety and efficacy follow-up of prophylactic higher fluence collagen cross-linking in high myopic laser-assisted in situ keratomileusis. Clin Ophthalmol. 2012;6:1125–1130. doi:10.2147/OPTH
16. Kanellopoulos AJ, Asimellis G. Refractive and keratometric stability in high myopia LASIK with high-frequency femtosecond and excimer lasers. J Refract Surg. 2013;29(12):832–837. doi:10.3928/1081597X-20130924-02
17. Kanellopoulos AJ, Asimellis G. Keratoconus management: long-term stability of topography-guided normalization combined with high-fluence CXL stabilization (the Athens Protocol). J Refract Surg. 2014;30(2):88–92. doi:10.3928/1081597X-20140120-03
18. Kanellopoulos AJ, Asimellis G. Corneal refractive power and symmetry changes following normalization of ectasias treated with partial topography-guided PTK combined with higher-fluence CXL (the Athens Protocol). J Refract Surg. 2014;30(5):342–346. doi:10.3928/1081597X-20140416-03
19. Kanellopoulos AJ, Asimellis G. LASIK ablation centration: an objective digitized assessment and comparison between two generations of an excimer laser. J Refract Surg. 2015;31(3):164–169. doi:10.3928/1081597X-20150225-01
20. Kanellopoulos AJ, Asimellis G. Novel placido-derived topography-guided excimer corneal normalization with cyclorotation adjustment: enhanced athens protocol for keratoconus. J Refract Surg. 2015;31(11):768–773. doi:10.3928/1081597X-20151021-06
21. Lee H, Chung JL, Kim EK, et al. Univariate and bivariate polar value analysis of corneal astigmatism measurements obtained with 6 instruments. J Cataract Refract Surg. 2012;38(9):1608–1615. doi:10.1016/j.jcrs.2012.04.035
22. Chang M, Kang SY, Kim HM. Which keratometer is most reliable for correcting astigmatism with toric intraocular lenses. Korean J Ophthalmol. 2012;26:10–14. doi:10.3341/kjo.2012.26.1.10
23. Shirayama M, Wang L, Weikert MP, Koch DD. Comparison of corneal powers obtained from 4 different devices. Am J Ophthalmol. 2009;148:
24. Visser N, Berendschot TT, Verbakel F, et al. Comparability and repeatability of corneal astigmatism measurements using different measurement technologies. J Cataract Refract Surg. 2012;38:1764–1770. doi:10.1016/j.jcrs.2012.05.036
25. Crawford AZ, Patel DV, McGhee CN. Comparison and repeatability of keratometric and corneal power measurements obtained by Orbscan II, Pentacam, and Galilei corneal tomography systems. Am J Ophthalmol. 2013;156:53–60. doi:10.1016/j.ajo.2013.01.029
26. Behshad S, Tucker J, Garg S. Toric intraocular lens alignment: manual versus automated alignment techniques for toric IOLs. Int Ophthalmol Clin. 2016;56:71–84. doi:10.1097/IIO.0000000000000115
27. Browne AW, Osher RH. Optimizing precision in toric lens selection by combining keratometry techniques. J Refract Surg. 2014;30(1):67–72. doi:10.3928/1081597X-20131217-07
 © 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2020 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

