Back to Journals » Open Access Emergency Medicine » Volume 15
Cutaneous Impact Location Predicts Intracranial Injury Among the Elderly Population with Traumatic Brain Injury
Authors Sedlák M , Wazir A, Dima A, Gazda J, Morochovič R
Received 24 May 2023
Accepted for publication 20 July 2023
Published 25 July 2023 Volume 2023:15 Pages 265—275
DOI https://doi.org/10.2147/OAEM.S422785
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Marián Sedlák,1,2 Adonis Wazir,3 Aikaterini Dima,4 Jakub Gazda,5 Radoslav Morochovič1
1Trauma Surgery Department, Pavol Jozef Safarik University in Kosice, Faculty of Medicine & Louis Pasteur University Hospital, Kosice, Slovakia; 2Zachranna Sluzba Kosice, Kosice, Slovakia; 3Swansea University Medical School, Swansea, UK; 4South London and Maudsley NHS Foundation Trust, London, UK; 5 2nd Department of Internal Medicine, Pavol Jozef Safarik University in Kosice, Faculty of Medicine & Louis Pasteur University Hospital, Kosice, Slovakia
Correspondence: Marián Sedlák, Pavol Jozef Safarik University in Kosice, Faculty of Medicine & Louis Pasteur University Hospital, Trauma Surgery Department, Kosice, Slovakia, Email [email protected]
Background: Traumatic brain injury (TBI) is one of the most common trauma-related diagnoses among the elderly population treated in emergency departments (ED). Identification of patients with increased or decreased risk of intracranial bleeding is of clinical importance. The objective of this study was to evaluate the implication of cutaneous impact location (CIL) on the prevalence of intracranial injury after suspected or confirmed TBI irrespective of its severity.
Methods: This was a retrospective, single-center, descriptive observational study of geriatric patients aged 65 years and older treated for suspected or confirmed TBI in a trauma surgery ED. The primary outcome of the study was the assessment of a CIL of the injury and its association with the prevalence of intracranial lesions found on a head computed tomography scan.
Results: Among 381 patients included in the analysis, the CIL of interest (temporo-parietal and occipital impacts) was present among 178 (46.7%) cases. Thirty-six (9.5%) patients were diagnosed with intracranial bleeding. The prevalence of intracranial bleeding was higher in the CIL of interest group compared with other locations outside (12.9% vs 6.4%; p = 0.030). CIL of interest was a predictor of intracranial bleeding (p = 0.033; OR: 2.17; 95% CI: 1.06 to 4.42).
Conclusion: The CIL of head injury is a predictor of intracranial lesions among geriatric patients with traumatic brain injury. Physicians should be aware of this association when assessing elderly patients with head injuries. More studies are needed to develop a clinical management tool incorporating CIL to guide the diagnosis of TBI in this population.
Keywords: cutaneous impact location, traumatic brain injury, TBI, geriatric TBI
Background
Traumatic brain injury (TBI) in the elderly population is one of the most common trauma-related diagnoses in the emergency department. With increasing numbers of patients seeking care and requiring hospitalization, effective and efficient diagnosis and management of traumatic brain injury becomes increasingly important.1 Geriatric patients with TBI require a specific approach due to unique physiological and clinical factors, including chronic medical conditions, polypharmacy, and frailty.2–4 Geriatric patients with traumatic brain injuries are at greater risk of death from injury.5 If they survive, compared to the rest of the population, their hospitalizations are longer, they recover more slowly, and they show worse functional outcomes than younger patients with similar injuries.5
Diagnostic algorithms for geriatric head injury include detailed personal history, thorough physical examination, and imaging modalities, mostly head computed tomography (CT) scan. Several clinical decision rules or aides help physicians choose the most suitable pathway and reduce unnecessary procedures, mostly imaging modalities among patients with minimal to mild TBI.6 However, the implementation of rules does not necessarily lead to a reduction in emergency department use of CT imaging.7
Dubucs et al suggested the cutaneous impact location (CIL) of injury as a possible predictor of intracranial lesions among the elderly with mild traumatic brain injury.8 The primary aim of this study was to assess the CIL of head injury and its association with intracranial lesions identified on head CT scans among a wider, general elderly population irrespective of TBI severity treated for suspected or confirmed traumatic brain injury at the emergency department.
Methods
Study Design
We conducted a retrospective, single-center, descriptive observational cohort study of geriatric patients aged 65 years and older treated for suspected or confirmed traumatic brain injury in the trauma surgery ED of the Louis Pasteur University Hospital in Košice. Patients were identified through the hospital emergency department’s electronic health records system. Patient assessment was conducted and documented by senior trauma surgery physicians. Additional data points were extracted from patients’ electronic health records. One-year mortality was assessed through the national mortality electronic records system.
Inclusion and Exclusion Criteria
All patients aged 65 years and older, who were treated in the emergency department for suspected or confirmed traumatic brain injury, and underwent initial CT scan imaging in the ED between January and June 2018 and January and June 2019 were included in the study. We selected the winter-spring periods to align with a selected pool of patients in the study by Dubucs et al.8 We excluded all patients with chronic lesions without new-onset intracranial bleedings (intracranial hematomas without active post-injury re-bleedings) and all patients with incomplete data (missing cutaneous impact location, missing blood thinners use) (Figure 1). The decision to perform a head CT scan was made by the treating physician according to the local standard procedure (all patients aged 65 years and older with suspected or confirmed TBI are indicated for a CT scan).
 |
Figure 1 Patient flowchart. |
Methodology
The study assessed the CIL of injury and its association with intracranial lesions found on a head CT scan among patients 65 years and older treated in the ED for suspected or confirmed TBI. All head CT scans were evaluated and interpreted at the time of the procedure by a senior radiologist through a written electronic report. Intracranial lesions were defined and described as acute epidural, subdural, or subarachnoid hemorrhages, and acute intra-parenchymal hematoma/cerebral contusion. In cases of more than one lesion, multiple lesions were reported. Additionally, besides intracranial injury, we reported skull fractures, fractures of facial bones, and other severe accidental findings (stroke, tumor). CIL of the injury (fronto-facial, temporoparietal, occipital, or no visible cutaneous impact) was recorded according to the electronic records, which were assessed and documented by a treating physician in the emergency department. The cutaneous location of the injury was described as follows: fronto-facial, temporoparietal, occipital, multiple impacts including occipital and/or temporoparietal zone or no visible cutaneous impact (Figure 2). The type of injury in regard to bleeding (open wound requiring suture or without needed suture) was recorded as described by the treating physician.
 |
Figure 2 Description of the cutaneous impact location of interest. |
The following demographic parameters were reported from patients’ electronic health records: Age (in years), sex, location of the incident (home, nursing home, healthcare facility, outside, other), type of injury (ground-level fall, fall from bed or a chair, fall from height or stairs, road traffic accident, found on the ground without further witnessed mechanism, other), mode of transportation to the hospital (EMS, alone, or sent from another department/healthcare facility to the ED). Additionally, the following parameters were included and analyzed: Glasgow score during initial presentation; the use of antiplatelet (aspirin, clopidogrel), anticoagulants (warfarin, direct oral anticoagulants – DOACs), subcutaneous anticoagulant (LWMH) or combinations; and death within 12 months of the injury. The transient symptoms after the injury were collected, if reported by the patient or noted by the physician or EMS crew (loss of consciousness, post-injury amnesia, ≥1 episode of vomiting). Alcohol intoxication was recorded as a qualitative parameter (based on laboratory values or self-reported use). Any unavailable variables were categorized as “undocumented”.
Ethics Approval
The study protocol was approved by the Ethics Committee of Louis Pasteur University Hospital in Kosice, Slovakia (code of approval: 2020/EK/12086).
Statistical Analysis
Statistical analysis was conducted using SPSS (version 28) for MacOs. Categorical variables are presented as absolute counts and percentages. Continuous variables are presented as means (standard deviations) or medians (IQR). The differences in the distribution of categorical variables were analyzed using Chi-square tests. Distributions of continuous variables were assessed for normality using the Shapiro–Wilk tests. The differences in the distribution of continuous variables were compared and analyzed using Mann–Whitney U testing. Additionally, a multivariable logistic regression model using a stepwise entry conditional model (p < 0.05 for entry and p > 0.15 for removal) was performed to investigate the factors predicting intracranial injury as the primary outcome, and effect sizes are reported as odds ratios. P-values of <0.05 were considered statistically significant.
Results
In two consecutive periods (January 2018 to June 2018 and January 2019 to June 2019), 532 patients were assessed for inclusion. Four patients were excluded per exclusion criteria (positive CT scans but not acute TBI – chronic subdural hematoma without active re-bleeding). We excluded 64 patients due to undocumented cutaneous impact location and 91 patients due to undocumented blood thinners use (unknown coagulation status). The remaining 381 patients were included in the final analysis (Figure 1). Overall, the mean age of the study population was 77.9 years (SD 8.3) and 168 (44.0%) were male. Shapiro–Wilk tests revealed non-normal distributions of continuous variables. The majority of patients was transported to the ED by emergency medical services (242 patients; 63.5%). Most of the accidents happened outside (129 patients; 33.9%) or at home (120 patients; 31.5%) and the most common mechanism of injury was ground-level fall from standing (258 patients; 67.7%). In total, 36 (9.5%) of the 381 patients included in the study were diagnosed with intracranial bleeding. Subarachnoid hemorrhage was the most prevalent finding (25 patients; 6.6%) followed by subdural hemorrhage (17 patients; 4.5%). Multiple types of intracranial bleeding occurred among 9 patients (2.4%). The usage of blood thinners was recorded among 227 patients (59.6%), of which 130 patients (34.1%) were on mono or dual antiplatelet therapy, 44 patients (11.5%) were on DOACs, 35 patients (9.2%) on warfarin, 12 patients (3.2%) on LMWH, and 6 patients (1.5%) on combined antiplatelet and anticoagulation therapy. A bleeding head wound was present in 143 cases (37.5%), bleeding wound in the location of interest was present in 60 cases (15.7%). Fifty-five patients (14.4%) were intoxicated by alcohol. CIL of interest was present among 178 (46.7%) patients. An impact outside of the location of interest was recorded among 203 (53.3%) patients. The most frequent location of impact was fronto-facial (193 patients; 50.7%), followed by occipital location (98 patients; 25.7%). Three patients required neurosurgical intervention. Two patients presented with GCS 15 and one with GCS 11, all of them had subdural bleeding, and one patient had a combination of subdural and subarachnoideal bleeding. Two had a frontal impact location, one had an occipital impact location. All of them were on blood thinners (one patient on NOAC, two on antiplatelet treatments), none of them had a bleeding wound and all made a full recovery. Further characteristics of the study population are presented in Table 1 and Table 2.
 |
Table 1 Summary of Patient Demographics and Characteristics (N = 381) |
 |
Table 2 Summary of Patient Clinical Findings and Outcomes (N = 381) |
The prevalence of intracranial bleeding was higher in the CIL of interest group compared with other locations outside (23 patients vs 13 patients; 12.9% vs 6.4%; p = 0.030). We observed a significantly higher number of subarachnoid hemorrhages in the CIL of interest group compared with CIL outside of the location of interest (18 cases vs 7 cases). A multivariable logistic regression model using a stepwise entry conditional model (p < 0.05 for entry and p > 0.15 for removal) was performed to investigate the factors (CIL, age, GCS, usage of blood thinners, intoxication) predicting intracranial injury as the primary outcome. CIL of interest was a predictor of intracranial bleeding (p = 0.033; OR: 2.17; 95% CI: 1.06–4.42; area under the ROC curve (AUC): 0.59). The usage of blood thinners was not associated with intracranial bleeding irrespective of CIL (Figure 3). The results of additional analyses are presented in Table 3 and Table 4.
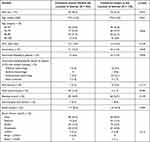 |
Table 3 Factors Associated with the CIL of Interest (N = 381) |
 |
Table 4 Binary Logistic Regression for the Outcome of Intracranial Bleeding |
 |
Figure 3 Association between blood thinners usage and intracranial bleeding in regard to the cutaneous impact location. |
Discussion
The overall prevalence of intracranial bleeding in our cohort of elderly patients with head trauma was 9.5%, which is consistent with several studies performed among this population.8–12 The most common etiology of TBI injuries in this group was ground-level fall (258 patients; 67.7%), which is in accordance with the current literature.3,8–10,12,13 The majority of injuries occurred at home or outside, with similar frequencies. In our cohort of patients, more patients had suffered their injury outside in comparison to a similar study.3 A selection bias of the study periods (spring months) may explain this because people are more likely to spend their days outside when the weather is getting better. The most common CT finding was subarachnoid hemorrhage (25 patients; 6.6%) followed by subdural hemorrhage (17 patients; 4.5%), which are the most common intracranial lesions among general geriatric populations treated for head injuries.8–10,12
Cutaneous impact in the location of interest (involvement of the temporo-parietal or occipital region) was present among 178 (46.7%) patients. Although more patients had their impact location outside the location of interest (203 patients; 53.3%), they had a lower prevalence of intracranial bleeding (13 vs 23 patients; 6.4% vs 12.9%; p = 0.030). CIL of interest was a predictor of intracranial bleeding in the multivariable logistic regression model (p = 0.033; OR: 2.17; 95% CI: 1.06–4.42; area under the ROC curve (AUC): 0.59). We observed a significantly higher number of subarachnoid hemorrhages in the CIL of interest group, compared with outside. Our model was not mutually exclusive, since several patients had multiple types of intracranial bleeding; therefore, we did not analyze this finding further. Nevertheless, this accidental finding warrants further investigations.
Examination of the CIL in connection with geriatric head injuries and TBI is a relatively new area, which has not been studied in detail in this population. Ibañez Pérez De La Blanca et al studied risk factors for intracranial lesions and mortality in older patients with mild traumatic brain injuries and did not find an association between cranio-facial lesions and such outcomes. However, only 56% (258/504) of patients in this study had some.12 De Wit et al studied elderly patients admitted to the ED due to ground-level falls with suspected or confirmed traumatic brain injury (2176 patients) and reported the association of the presence of head laceration or bruise with an increased risk of intracranial lesions with OR at 4.33 (95% CI: 2.7–7.0) in the multivariable analysis.10 A specific CIL was not assessed in this study. Lampart et al reported an association of “visible injury signs above the clavicles” with an increased risk of intracranial bleeding.11 Cipriano et al also reported a higher prevalence of immediate intracranial bleeding in the cohort of anticoagulated geriatric patients with clear evidence of trauma above the clavicles.14 Both did not assess a specific CIL.
Dubucs et al suggested that CIL of injury may help to identify the risk for mTBI-related intracranial lesions in older patients.8 In their first study among 365 geriatric patients with mTBI, they reported increased relative risk of intracranial bleeding among patients with cutaneous temporo-parietal or occipital impact in comparison with cutaneous frontal impact (RR = 2.54; 95% CI 1.20 to 5.42).8 Dubucs et al recently examined the CIL of interest theory (temporo-parietal and occipital) in the validation study for their mild-TBI model. Compared with the location of interest, ORs of intracranial injuries for other locations were significantly lower.9 Our study is in line with these findings. The role of CIL is more examined among pediatric patients. Non-frontal scalp hematoma was adopted as one of the six factors associated with a clinically important TBI in the prediction rule derived by the Pediatric Emergency Care Applied Research Network (PECARN).15 CIL in temporal, parietal, and occipital zones (location of interest in our work) is a relatively well-established factor among pediatric clinical prediction rules concerning traumatic brain injury.16–18
Biomechanics and pathophysiology behind the increased risk of intracranial injury in patients with CILs in the area of interest are poorly understood, and several hypotheses have been proposed, including deficient postural reflexes in elderly people unable to sufficiently reduce the kinetic energy of the fall in that direction. Special anatomical and physiological features of head tissues and the brain may also play a role.9 Data examining the issue of the direction of the fall and its effect on the incidence of intracranial bleeding are inconclusive. Some studies indicate a higher risk of injuries in forward falls, others backward, but specific CIL was not assessed.2,3 Frontal impacts may be associated with some of the kinetic energy absorbed by postural adaptation reflexes of the upper limbs.8 Deterioration of physiological functions in the elderly, including the deterioration of the quality of visual, auditory, and balance functions may reduce the possibilities of more flexible reactions and thus the ability to avoid or cushion the fall, although its specific role in regard to the direction of a fall has not been studied in detail.19 The frontal impact may also have a decreased risk of intracranial bleeding due to the thickness of the frontal bone, which is greater than the temporal, parietal and occipital bones.20 The structure and thickness of bone tissues may also be connected to the interhemispheric subdural hematoma, which typically occurs in the elderly by the injury of bridging veins and commonly appears in the parietal and occipital regions.13
Anticoagulation and antiplatelet medications are historically connected with a potential for an increased risk of traumatic intracranial bleeding, and the debate is still ongoing with numerous research papers examining the effects of this factor among geriatric patients with TBI.9,10,12,14,21–25 Our study did not find a statistically significant association between the incidence of intracranial bleeding and the use of anticoagulants or antiplatelets among both CIL locations. These findings are in line with numerous recent research papers examining the issue within the population of geriatric traumatic brain injury.9–11
Limitations
Our study had several limitations. For this study, we purposefully included all consecutive adult patients over 65 years who have sustained suspected or confirmed traumatic brain injury and did not rule out patients based on their TBI severity according to the presenting GCS score (minimal, mild, moderate, severe). We wanted to portray the most common, general cohort of this specific subpopulation which reflects the clinical reality of geriatric TBI (older patients who come to the ED because of suspected or confirmed head injury irrespective of their presentation or severity). The retrospective nature of this study posed numerous challenges. The absence of standardization of electronic records and patient notes influenced the data, which resulted in a higher number of undocumented variables and missing data. There was no patient follow-up, which could document delayed intracranial hemorrhage, despite its low prevalence according to the current literature, even in the anticoagulated group of patients.14,22,26 Further research in this area is needed to suggest a standardized diagnostic tool, which may consider incorporating CIL as one of its parameters.
Conclusions
The cutaneous impact location of head injury can be considered as a potential parameter to predict intracranial lesions among geriatric patients with traumatic brain injury. Physicians should be aware of this association when assessing elderly patients with head injuries. More studies are needed to develop a clinical management tool incorporating cutaneous impact location of injury to guide the diagnosis of TBI in this population.
Abbreviations
95% CI, 95% Confidence Interval; CIL, cutaneous impact location; CT, computed tomography; DOACs, direct oral anticoagulants; ED, emergency department; EMS, emergency medical services; GCS, Glasgow Coma Scale; IQR, interquartile range; LMWH, low molecular weight heparin; OR, odds ratio; ROC, Receiver operating characteristics; RR, relative risk; TBI, traumatic brain injury.
Data Sharing Statement
The dataset collected during the study is available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Patients have signed the necessary informed consent to the processing and use of health data for the purpose of this study and publication. The study protocol was approved by the Ethics Committee of Louis Pasteur University Hospital in Kosice, Slovakia (code of approval: 2020/EK/12086), and confirmed that all ethical requirements were respected and followed herein, including the adherence to ethical standards according to the Declaration of Helsinki (1964) and its later amendments.
Consent for Publication
All authors have given consent.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was not supported by any funding.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Majdan M, Plancikova D, Brazinova A. Epidemiology of traumatic brain injuries in Europe: a cross-sectional analysis. Lancet Public Health. 2016;1(2):e76–e83. doi:10.1016/S2468-2667(16)30017-2
2. Yang Y, Mackey DC, Liu-Ambrose T, Leung P-M, Feldman F, Robinovitch SN. Clinical risk factors for head impact during falls in older adults: a prospective cohort study in long-term care. J Head Trauma Rehabil. 2017;32(3):168–177. doi:10.1097/HTR.0000000000000257
3. Hwang H-F, Cheng C-H, Chien D-K, Yu W-Y, Lin M-R. Risk factors for traumatic brain injuries during falls in older persons. J Head Trauma Rehabil. 2015;30(6):E9–E17. doi:10.1097/HTR.0000000000000093
4. Hawley C, Sakr M, Scapinello S, Salvo J, Wrenn P. Traumatic brain injuries in older adults—6 years of data for one UK trauma centre: retrospective analysis of prospectively collected data. Emerg Med J. 2017;34(8):509–516. doi:10.1136/emermed-2016-206506
5. Centers for Disease Control and Prevention. Report to congress on traumatic brain injury in the United States: epidemiology and rehabilitation. Natl Center Injury Prev Control. 2015;2:1–72.
6. Klang E, Beytelman A, Greenberg D. Overuse of head CT examinations for the investigation of minor head trauma: analysis of contributing factors. J Am Coll Radiol. 2017;14(2):171–176. doi:10.1016/j.jacr.2016.08.032
7. Stiell IG, Clement CM, Grimshaw JM. A prospective cluster-randomized trial to implement the Canadian CT Head Rule in emergency departments. CMAJ. 2010;182(14):1527–1532. doi:10.1503/cmaj.091974
8. Tamminen J, Lydén E, Kurki J, Huhtala H, Kämäräinen A, Hoppu S. Cutaneous impact location: a new tool to predict intracranial lesion among the elderly with mild traumatic brain injury? Scand J Trauma Resusc Emerg Med. 2020;28(1):1–9. doi:10.1186/s13049-019-0696-1
9. Dubucs X, Lecuyer L, Balen F, et al. Validation of the cutaneous impact location to predict intracranial lesion among elderly admitted to the Emergency Department after a ground-level fall. Injury. 2023;54:1306–1313. doi:10.1016/j.injury.2023.02.023
10. Wit K, Parpia S, Varner C. Clinical predictors of intracranial bleeding in older adults who have fallen: a cohort study. J Am Geriatr Soc. 2020;68(5):970–976. doi:10.1111/jgs.16338
11. Lampart A, Kuster T, Nickel CH, Bingisser R, Pedersen V. Prevalence and severity of traumatic intracranial hemorrhage in older adults with low‐energy falls. J Am Geriatr Soc. 2020;68(5):977–982. doi:10.1111/jgs.16400
12. Ibañez Pérez De La Blanca MA, Fernández Mondéjar E, Gómez Jimènez FJ, Alonso Morales JM, Lombardo MDQ, Viso Rodriguez JL. Risk factors for intracranial lesions and mortality in older patients with mild traumatic brain injuries. Brain Injury. 2018;32(1):99–104. doi:10.1080/02699052.2017.1382716
13. Karibe H, Hayashi T, Narisawa A, Kameyama M, Nakagawa A, Tominaga T. Clinical characteristics and outcome in elderly patients with traumatic brain injury: for establishment of management strategy. Neurol Med Chir (Tokyo). 2017;57(8):418–425. doi:10.2176/nmc.st.2017-0058
14. Cipriano A, Park N, Pecori A. Predictors of post-traumatic complication of mild brain injury in anticoagulated patients: dOACs are safer than VKAs. Intern Emerg Med. 2021;16:1061–1070. doi:10.1007/s11739-020-02576-w
15. Kuppermann N, Holmes JF, Dayan JF, et al. Identification of children at very low risk of clinically-important brain injuries after head trauma: a prospective study. Lancet. 2009;374:1160–1170. doi:10.1016/S0140-6736(09)61558-0
16. Burns ECM, Grool AM, Klassen TP. Scalp hematoma characteristics associated with intracranial injury in pediatric minor head injury. Acad Emerg Med. 2016;23(5):576–583. doi:10.1111/acem.12957
17. Schutzman SA, Nigrovic LE, Mannix R. The infant scalp score: a validated tool to stratify risk of traumatic brain injury in infants with isolated scalp hematoma. Acad Emerg Med. 2021;28(1):92–97. doi:10.1111/acem.14087
18. Meral Atiş G, Altay T, Atiş ŞE. Comparison of CATCH, PECARN, and CHALICE clinical decision rules in pediatric patients with mild head trauma. Eur J Trauma Emerg Surg. 2022;48(4):3123–3130. doi:10.1007/s00068-021-01859-x
19. Lockhart TE, Smith JL, Woldstad JC. Effects of aging on the biomechanics of slips and falls. Hum Factors. 2005;47(4):708–729. doi:10.1518/001872005775571014
20. Mahinda HA, Murty OP. Variability in thickness of human skull bones and sternum–An autopsy experience. J Forensic Med Toxicol. 2009;26(2):26–31.
21. Minhas H, Welsher A, Turcotte M. Incidence of intracranial bleeding in anticoagulated patients with minor head injury: a systematic review and meta‐analysis of prospective studies. Br J Haematol. 2018;183(1):119–126. doi:10.1111/bjh.15509
22. Liu S, McLeod SL, Atzema CL. Delayed intracranial hemorrhage after head injury among elderly patients on anticoagulation seen in the emergency department. Can J Emerg Med. 2022;24(8):853–861. doi:10.1007/s43678-022-00392-z
23. Nishijima DK, Gaona SD, Waechter T, et al. The incidence of traumatic intracranial hemorrhage in head-injured older adults transported by EMS with and without anticoagulant or antiplatelet use. J Neurotrauma. 2017;35(5):750–759. doi:10.1089/neu.2017.5232
24. Probst MA, Gupta M, Hendey GW. Prevalence of intracranial injury in adult patients with blunt head trauma with and without anticoagulant or antiplatelet use. Ann Emerg Med. 2020;75(3):354–364. doi:10.1016/j.annemergmed.2019.10.004
25. Peck KA, Calvo RY, Schechter MS. The impact of preinjury anticoagulants and prescription antiplatelet agents on outcomes in older patients with traumatic brain injury. J Trauma Acute Care Surg. 2014;76(2):431–436. doi:10.1097/TA.0000000000000107
26. Puzio TJ, Murphy PB, Kregel HR. Delayed intracranial hemorrhage following blunt head trauma while on direct oral anticoagulants: a systematic review and meta-analysis. J Am Coll Surg. 2021;232(6):1007. doi:10.1016/j.jamcollsurg.2021.02.016
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
