Back to Journals » Clinical Ophthalmology » Volume 18
Customizing Clinical Outcomes with Implantation of Two Diffractive Trifocal IOLs of Identical Design but Differing Light Distributions to the Far, Intermediate and Near Foci
Authors Kaymak H, Potvin R , Neller K, Klabe K, Anello RD
Received 21 December 2023
Accepted for publication 12 March 2024
Published 3 April 2024 Volume 2024:18 Pages 1009—1022
DOI https://doi.org/10.2147/OPTH.S456007
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Hakan Kaymak,1,2 Richard Potvin,3 Kai Neller,1,2 Karsten Klabe,1 Robert Donald Anello4 On behalf of the NINO Study Group
1Internationale Innovative Ophthalmochirurgie GbR, Duesseldorf, Germany; 2Institute of Experimental Ophthalmology, Saarland University, Homburg/Saar, Germany; 3Science in Vision, Frisco, TX, USA; 4Global Clinical and Medical Affairs, Hoya Surgical Optics, Irvine, CA, USA
Correspondence: Robert Donald Anello, HOYA Surgical Optics, 110 Progress, Suite 175, Irvine, CA, 92618, USA, Tel +1 909-224-6149, Email [email protected]
Purpose: To evaluate clinical outcomes after bilateral or contralateral implantation of the Gemetric™ (G) and Gemetric™ Plus (GPlus) diffractive trifocal intraocular lenses (IOLs).
Methods: This was a prospective, randomized, multi-center open-label study comparing clinical results and subjective patient responses around 6 months after implantation of the study lenses (toric and non-toric) in three different groups (bilateral G, bilateral GPlus and contralateral G/GPlus implantation). Results included the manifest refraction, uncorrected and distance corrected monocular and binocular visual acuity (VA) at distance, intermediate and near; the defocus curve; contrast sensitivity; and patient reported outcomes regarding spectacle independence, satisfaction and visual disturbances.
Results: There was no statistically significant difference in the mean refraction spherical equivalent between the two lens models (p = 0.33) or between the toric and non-toric lenses (p = 0.06). Monocular VA was better at distance with the G lens and better at near with the GPlus lens (p < 0.01). Mean binocular VA was better than 0.1 logMAR at all distances for all groups, both uncorrected and distance corrected. The mean binocular distance corrected VA was better than 0.15 logMAR from 0.0 D to − 3.50 D for all groups. All VA data for the contralateral group was as good or better than for the bilateral GPlus group. Questionnaire results showed no difference between groups for the frequency, severity, or degree of bother of visual disturbances (p > 0.24).
Conclusion: The two diffractive trifocal IOLs studied here may be used either bilaterally or contralaterally for the correction of presbyopia in cataract patients, providing excellent visual acuity with low levels of visual disturbances and high rates of overall spectacle independence. Bilateral Gemetric implantation resulted in slightly better distance and intermediate vision while contralateral implantation provided slightly better near vision. There was no apparent advantage to implanting the GPlus IOL bilaterally.
Keywords: Gemetric™, Gemetric™ Plus, trifocal, presbyopia-correcting, diffractive, trifocal, Vivinex™
Introduction
Patients presenting for cataract surgery who wish to reduce their dependence on spectacles for distance, intermediate and near viewing may choose from a wide range of options, from simple monofocal IOLs, to enhanced monofocal IOLs, to extended depth of focus (EDOF) IOLs, to bifocal and trifocal IOLs. These lenses are listed here in the generally accepted order of their ability to provide near vision.1–3 With any of the presbyopia correcting IOL options there is a higher likelihood of reduced contrast sensitivity and more visual disturbances relative to a monofocal IOL.3 The highest level of spectacle freedom is expected to be obtained with bilateral trifocal IOLs.4
The ability to provide good near vision with a trifocal IOL is important to many patients. Results from early research designed to objectively quantify the percentage of time spent viewing near/intermediate and far objects indicated that participants spent more than 40% of their time on near tasks (43%, ±15%), exceeding the time spent on intermediate (30%, ±15%) and distance (27% ±12%) tasks.5 As can be seen, the distribution was quite varied, which makes it important to consider the individual’s vision requirements when recommending a presbyopia-correcting IOL or IOLs.
There have been numerous approaches to customizing postoperative visual results with presbyopia correcting IOLs. With bifocal IOLs, using two different add powers was one way to increase the range of vision.6,7 More recently, surgeons have tried to mitigate the negative effects some patients experience with trifocal IOLs by using an EDOF IOL in the dominant eye and a trifocal in the non-dominant eye.8,9 While generally successful, challenges with this approach are that the patient can usually tell the difference between their two eyes, and near vision tends to suffer. Hoya has introduced a family of trifocal IOLs to address this issue. Rather than changing the focal points of the IOL, or mixing the trifocal IOL with a different IOL type, they have taken a proprietary Gaussian diffractive trifocal design and modified its structure to change the ratio of light distribution to the near, intermediate and distance foci.10
Figure 1 illustrates the key design elements of the Vivinex Gemetric™ and Gemetric™ Plus trifocal IOLs. Both are made from a hydrophobic acrylic material with a blue light filtering chromophore. Overall lens diameter is 13.0 mm with a 6.0 mm optic zone. A proprietary posterior surface treatment increases lens/capsule adhesion to reduce the potential for PCO11 and the textured edges of the optic reduce the likelihood of dysphotopsia. The base refractive power of the 6.0 mm optic provides distance vision, while intermediate and near vision are provided by the 3.2 mm central diffractive zone on the anterior surface. A proprietary Gaussian diffractive optic with edge smoothing increases diffractive efficiency and the smaller optical zone was designed to provide less pupil-dependent performance. In both lenses the diffractive optics provide 1.75D intermediate focus and 3.50D near focus at the IOL plane. The diffractive elements of the two IOLs differ slightly, resulting in more light being directed to the near focus in the Gemetric Plus design (Figure 2), with a slightly lower percentage of light directed to intermediate and far, relative to the Gemetric design. Both lenses are available in a toric version, with the astigmatism correction on the posterior surface. Astigmatism up to 2.6 D at the corneal plane can be corrected with these lenses. An online toric calculator is available for planning astigmatism correction. All lenses are provided in the Vivinex multiSert™ preloaded injector.
 |
Figure 1 Gemetric and Gemetric Plus diffractive trifocal design elements (Courtesy Hoya, used with permission). |
 |
Figure 2 Comparison of the through-focus modulation transfer function by IOL (Courtesy Hoya, used with permission). |
This study was designed to fulfill the requirements of a clinical trial conducted in accordance with ISO 22979, with the resultant data providing the capability to compare the clinical and subjective outcomes after bilateral implantation of either IOL, or contralateral implantation of both lenses.
Methods
This was a prospective, randomized, multi-center open-label study conducted at 11 sites in Spain and Germany (see Table 1, NINO study group details). It was designed to compare the clinical results and patient reported outcomes after implantation of the study lenses in three different groups. Subjects in the first group were bilaterally implanted with the Gemetric trifocal IOL (G/G), those in the second group had contralateral implantation of the Gemetric and Gemetric Plus trifocal IOLs (G/GPlus), while the third group of subjects were bilaterally implanted with the Gemetric Plus trifocal IOL (GPlus/GPlus). Toric and non-toric versions of both IOLs were included in all Groups.
 |
Table 1 Principal Investigator List, NINO Study |
Note that while the study included 3 test groups, only two different IOLs were implanted. As such, all monocular results (monocular VA, refraction) are evaluated based on the lens, rather than the study group, since the IOL implanted in the fellow eye is not material to the monocular results. All binocular results and subjective responses are reported by study group.
The clinical investigation was conducted in compliance with Good Clinical Practices (ISO 14155), and all other applicable regulations,12 conditions of approval imposed by the reviewing Institutional Review Board (IRB) or conditions of approval by the reviewing Independent Ethics Committee (IEC), and all country specific laws and regulations (ethics approvals are indicated in Table 1). The study investigators adhered to the tenets of the Declaration of Helsinki. The study was registered in a WHO database with main ID: DRKS00024535. Informed consent was obtained from all study participants prior to enrollment into the study and any study specific examinations.
Subjects included patients over 21 years of age presenting for bilateral cataract surgery with no ocular or systemic conditions that were deemed likely to affect postoperative visual acuity. The IOL power determined from biometry had to be in the available range of sphere (+15.0 D to +26.0 D) and cylinder (0.0 D to +3.0 D at the IOL plane) for the IOLs. The subjects had to have a potential binocular postoperative visual acuity of 0.1 logMAR (20/25) or better. Exclusion criteria included prior intraocular or corneal surgery, irregular astigmatism, any systemic or ocular disease likely to increase operative risk or confound the outcome of the study (eg, uncontrolled diabetes) and use of systemic and/or ocular medications that may affect vision.
Subjects were enrolled and had bilateral cataract surgery using the surgeons’ preferred techniques and follow-up consistent with the clinic’s usual standard of care and the requirements of a level B ISO study. In general, surgeons implanted the eye with the worst preoperative visual acuity first. For the G/GPlus group, there was no requirement to consider ocular dominance; the Gemetric lens was always implanted in the first eye.
Subjects were examined at 1 day and one week postoperative, and at one month and about 6 months (120 to 180 days) after the second eye surgery. Clinical outcomes of interest at 6 months were: uncorrected and distance corrected monocular and binocular visual acuity (VA) at distance, intermediate and near (UDVA, CDVA, UIVA, DCIVA, UNVA, DCNVA, respectively); the distance corrected binocular defocus curve; and binocular distance contrast sensitivity in photopic (with glare) and mesopic (with and without glare) conditions. Contrast sensitivity was measured using the Optec 6500 Functional Acuity Contrast Test (Stereo Optical, Chicago, USA). CDVA and DCNVA were also tested under mesopic conditions. In addition, a questionnaire related to spectacle independence and satisfaction at various distances, for various tasks, and under differing light conditions was administered. Visual disturbances were evaluated using the Quality of Vision questionnaire.13 This validated, Rasch-scored questionnaire provides 10 directed questions regarding specific visual disturbances and allows subjects to report the frequency, severity and degree of bother of each. Frequency ranges from Never (0) to Very Often (3), severity ranges from Not at All (0) to Severe (3) and degree of bother ranges from Not at All (0) to Very (3). Adverse events were monitored at all study visits.
Raw data was collected on site and entered into a central database. Tables of relevant data were exported to Microsoft Excel and statistical analyses were performed using the Statistical data analysis software system, version 12 (TIBCO Software Inc., Palo Alto, CA, USA). Parametric comparisons were made using analysis of variance (ANOVA) while categorical comparisons were made with appropriate non-parametric tests. In all cases an alpha (p-value) of 0.05 was considered statistically significant. Additional analysis is ongoing, so the data is not available for sharing.
Results
A total of 146 subjects were successfully recruited across all sites, with 128 subjects ultimately enrolled. Two subjects were lost to follow-up, one more had an unrelated ocular adverse event (hemi-retinal vein occlusion), and one failed to complete the final study visits, leaving 124 subjects (248 eyes) for analysis. The average follow-up length (after second eye surgery) was 143 ± 20 days, ranging from 120 to 233 days, with no statistically significant difference in follow-up length by arm (p = 0.7). There were no explants of any lens. The breakdown of enrollment is shown in Table 2. The mean age was not statistically significantly different between groups (p = 0.33). Two thirds of all lenses implanted were toric. The percentage of toric IOLs was not statistically significantly different between the two IOL models implanted (69/108 G, 95/140 GPlus, Chi-squared test, p = 0.51).
 |
Table 2 Group Summary for Analysis |
Figure 3A shows the distribution of the postoperative mean refraction spherical equivalent (MRSE), while Figure 3B shows the distribution of the postoperative refractive cylinder. There was no statistically significant difference in MRSE between the two lens models (p = 0.33) or between the toric and non-toric versions of the lenses (p = 0.06). Postoperative refractive cylinder was also not statistically significantly different between the two lens models (p = 0.57). While there was a statistically significant difference in mean postoperative refractive cylinder between the toric and non-toric IOLs (p = 0.047), the difference was < 0.1 D and deemed not clinically relevant. Ninety percent of all eyes (222/248) were within 0.50 D of the intended MRSE, with only 2 eyes more than 1.0 D from intended. Eighty-eight percent of all eyes (217/248) had 0.50 D or less of refractive cylinder postoperatively.
 |
Figure 3 The distribution of refractive outcomes at 6 months postoperative. (A) Mean refraction spherical equivalent (MRSE). (B) Postoperative refractive cylinder. |
Box-whisker plots showing the distribution of monocular visual acuities by distance and lens are shown in Figure 4 (Far VA was tested at 4 m, intermediate at 66 cm and near at 40 cm). As can be seen, the Gemetric model provided slightly better far and intermediate vision while the Gemetric Plus model provided slightly better near vision, though the differences at far and intermediate appear nominal. The greatest mean difference in both the uncorrected and distance corrected conditions was at near, with the Gemetric Plus lens providing VA a half line to almost a line better than the Gemetric lens (p < 0.01 in both cases).
 |
Figure 4 Summary of monocular visual acuity data by lens and test distance. |
Figure 5 shows the mean binocular VA results at various distances for the uncorrected and distance corrected conditions for the 3 groups. The mean binocular VA was better than 0.1 logMAR at all distances for all groups, both uncorrected and distance corrected. The GPlus/GPlus group showed slightly lower distance VA than the other two groups, but better near VA than the G/G group. Mean near VA in the G/GPlus group was also better than in the G/G group. Mean VA in the G/GPlus group was as good or better than in the GPlus/GPlus group at all test distances, both uncorrected and distance corrected.
Figure 6 shows the effect of mesopic chart luminance on visual acuity at distance and near by group. There was no statistically significant difference in the degree to which mesopic luminance reduced VA between the three study groups at distance (p = 0.88) but the GPlus/GPlus group had a significantly greater difference between photopic and mesopic VA at near relative to the G/GPlus group (p = 0.03); the difference was about 2 letters more acuity lost. For all groups the average reduction in VA at distance was just over 1.5 lines and the average reduction in VA at near was just less than 2 lines in the G/GPlus group and just over 2 lines in the other two groups. As can be seen, the G/GPlus group had significantly better near performance than the G/G group.
The binocular distance corrected defocus curve for each of the three groups is shown in Figure 7. In all three groups the mean CDVA was better than 20/20. The mean binocular distance corrected VA was better than 0.15 logMAR (~20/30 Snellen acuity) across a range of defocus from 0.0 D (distance) to −3.50 D (29 cm) for all groups. In both the G/G and G/GPlus groups, 94% of subjects (34/36), had VAs better than 0.3 logMAR (20/40) across that 3.5 D defocus range, compared to 87% of subjects (45/52) in the GPlus/GPlus group. Statistically significant differences between groups were found at defocus levels of −0.5 D, −1.0 D and −1.5 D (p < 0.05 in all cases), attributable to the difference in performance between the G/G group and the GPlus/GPlus group (Tukey’s test). A statistically significant difference was also found at a defocus of −2.50 D (p = 0.03), attributable to the difference between the G/G group and the G/GPlus group (Tukey’s test).
 |
Figure 7 Distance corrected binocular defocus curve by study group. |
Figure 8 shows the results of the contrast sensitivity (CS) testing. For photopic testing with glare the G/G and G/GPlus groups performed similarly, while results for the GPlus/GPlus group were slightly lower at higher spatial frequencies. Mesopic CS was lower for all groups, as expected, but all groups showed similar performance both with and without glare.
 |
Figure 8 Contrast sensitivity results by study group and test condition. (A) Photopic with glare, (B) Mesopic without glare, (C) MEsopic with glare. Notes: Vertical bars represent the standard error. |
The Quality of Vision (QoV) questionnaire results showed no statistically significant difference between groups for the frequency (p = 0.27), severity (p = 0.24) or degree of bother (p = 0.26) of visual disturbances reported by subjects. Aggregate scores are shown in the box-whisker plot in Figure 9. The most frequently reported visual disturbance with these lenses was halos, followed by starbursts and glare. The level of severity and degree of bother reported were also highest for halos, then starbursts and glare. Figure 10 shows the distribution of the raw values associated with these.
 |
Figure 9 Distribution of the Rasch-scored frequency, severity and degree of bother from visual disturbances. |
 |
Figure 10 Mean frequency, severity and degree of bother reported for glare, halos and starbursts. |
Figure 11 summarizes questionnaire results related to the level of spectacle independence by group, and overall, by viewing distance. Spectacle independence at far and intermediate was very similar between groups, exceeding 90% at both distances. At near, the G/GPlus group reported a higher rate of spectacle independence, with 92% of subjects (33/36) reporting never needing glasses for near work; results for the other groups were slightly lower.
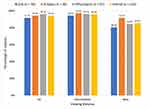 |
Figure 11 Reported spectacle use of “Never” by study group and viewing distance. |
Subjects were asked to respond to a question regarding their overall satisfaction with vision, using a 0–5 scale (“Always”, “Often”, “Sometimes”, “Seldom”, “Never”). In the G/G and G/GPlus groups, 91.7% of subjects (33/36) reported being “Always” or “Often” satisfied with their vision overall, compared to 86.6% (45/52) of subjects in the GPlus/GPlus group. No subjects reported they were “Never” satisfied and only 2 subjects overall reported being “Rarely” satisfied; this was associated with high residual refractive error (MRSE> +1.0 D in one or both eyes). When subjects were asked whether they would choose this lens (or lens combination) again, more than 94% in each group replied “Yes”.
Discussion
The current study was conducted to determine if there were any significant differences in clinical outcomes between three different implantation strategies using two diffractive trifocal IOLs: bilateral Gemetric, contralateral Gemetric/Gemetric Plus or bilateral Gemetric Plus. As is evident from the results, the lenses performed similarly in all three groups, though with some important differences.
As expected, the monocular VA data from the Gemetric Plus IOL showed better near VA than for the Gemetric IOL, with slightly lower intermediate and distance vision. Refractive predictability was similar for both IOLs, and the difference in refractive outcomes between the toric and non-toric versions of the IOLs was nominal. The refractive results and the monocular visual acuities obtained with these IOLs are similar to those reported for other diffractive trifocal IOLs in common use.14,15
Both the binocular VA and the defocus results from the current study suggest that there is no clinical advantage to using the GPlus/GPlus combination. The contralateral G/GPlus combination performed as well as the GPlus/GPlus option at near while providing better intermediate and distance acuity, with no difference in visual disturbances. The G/GPlus group also appeared less affected by mesopic luminance conditions, demonstrating significantly better near VA (1 logMAR line) relative to the G/G Group. Patients who wanted slightly better near vision would have their needs best met with the contralateral option, while patients looking for better intermediate would benefit from the bilateral Gemetric option. The binocular acuity results and the binocular defocus curves in the current study are also very similar to results reported for other trifocal IOLs.14,15 The reduced vision under mesopic conditions was also similar between lenses, and similar to previous results reported for other diffractive trifocal IOLs.16
The lower contrast sensitivity at high frequency in the GPlus/GPlus group observed in the current study is likely a function of the lower percentage of light distributed to distance vision in this IOL. Overall, the contrast sensitivity results obtained here appear similar to those achieved with other diffractive trifocal IOLs in the market.17,18 As with the VA data, the contrast sensitivity results suggest that the GPlus/GPlus combination has no advantages over the other two implant combinations.
Differences in questionnaire results across studies should be interpreted with caution, but QoV results seen in the current study are remarkably similar to those reported for a competitive diffractive trifocal IOL (Panoptix®, Alcon, Fort Worth, USA), with a slightly lower median frequency of disturbances reported, a similar level of severity and a slightly lower median degree of bother.19 The frequency, severity and degree of bother related to halos and starbursts appear similar to those reported for three competitive diffractive trifocal IOLs.14 However, glare experienced with the Gemetric lenses was reported less frequently, was less severe and was less bothersome in the current study than was reported for the other diffractive trifocals in that previous study.
Conclusion
The results of the current study show that the Gemetric and Gemetric Plus diffractive trifocal IOLs may be used either bilaterally or in a paired contralateral fashion to provide effective correction of presbyopia in patients presenting for cataract surgery. Visual acuity in all groups studied here was excellent, with low levels of visual disturbances and high rates of overall spectacle independence reported. Results further suggest that bilateral Gemetric implantation may be preferred by subjects looking for slightly better distance and intermediate vision while contralateral Gemetric/Gemetric Plus implantation may be the best option for subjects interested in slightly better near vision. There was no apparent advantage to implanting the Gemetric Plus IOL bilaterally.
Funding
The study was sponsored by Hoya Surgical Optics.
Disclosure
Hakan Kaymak has received honoraria for lectures and reimbursement for attending and travel to meetings from HOYA Surgical Optics. Richard Potvin is a consultant to Alcon and Hoya. Kai Neller and Karsten Klabe have no relevant financial disclosures. Robert Anello is an employee of Hoya Surgical Optics. The authors report no other conflicts of interest in this work.
References
1. Karam M, Alkhowaiter N, Alkhabbaz A, et al. Extended depth of focus versus trifocal for intraocular lens implantation: an updated systematic review and meta-analysis. Am J Ophthalmol. 2023;251:52–70. doi:10.1016/j.ajo.2023.01.024
2. Khandelwal SS, Jun JJ, Mak S, Booth MS, Shekelle PG. Effectiveness of multifocal and monofocal intraocular lenses for cataract surgery and lens replacement: a systematic review and meta-analysis. Graefes Arch Clin Exp Ophthalmol. 2019;257(5):863–875. doi:10.1007/s00417-018-04218-6
3. Schallhorn JM, Pantanelli SM, Lin CC, et al. Multifocal and accommodating intraocular lenses for the treatment of presbyopia: a report by the American academy of ophthalmology. Ophthalmology. 2021;128(10):1469–1482. doi:10.1016/j.ophtha.2021.03.013
4. Cho JY, Won YK, Park J, et al. Visual outcomes and optical quality of accommodative, multifocal, extended depth-of-focus, and monofocal intraocular lenses in presbyopia-correcting cataract surgery: a systematic review and bayesian network meta-analysis. JAMA Ophthalmol. 2022;140(11):1045–1053.
5. Ribeiro F, Ferreira TB, Silva D, Matos AC, Gaspar S, Piñero DP. Analysis of daily visual habits in a presbyopic population. J Ophthalmol. 2023;2023:6440954. doi:10.1155/2023/6440954
6. Dell SJ. Evaluation of visual and subjective outcomes with mix-and-match of three one-piece tecnis multifocal IOLs of varying add powers. Clin Ophthalmol. 2020;14:2903–2911. PMID: 33061276; PMCID: PMC7532892. doi:10.2147/OPTH.S266120
7. Vilar C, Hida WT, de Medeiros AL, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol. 2017;11:1393–1397. PMID: 28814826; PMCID: PMC5546829. doi:10.2147/OPTH.S139909
8. Acar B, Nurozler Tabakci B. Clinical outcome comparison: bilateral trifocal vs. mix-match extended depth of focus and trifocal intraocular lenses. Int Ophthalmol. 2021;41(11):3675–3686. PMID: 34180019. doi:10.1007/s10792-021-01925-8
9. Tarib I, Kasier I, Herbers C, et al. Comparison of visual outcomes and patient satisfaction after bilateral implantation of an EDOF IOL and a mix-and-match approach. J Refract Surg. 2019;35(7):408–416. doi:10.3928/1081597X-20190417-02
10. Leydolt C, Schartmüller D, Schwarzenbacher L, Röggla V, Schriefl S, Menapace R. Posterior capsule opacification with two hydrophobic acrylic intraocular lenses: 3-year results of a randomized trial. Am J Ophthalmol. 2020;217:224–231. doi:10.1016/j.ajo.2020.04.011
11. Auffarth GU, Brézin A, Lignereux F, et al. Randomized multicenter trial to assess posterior capsule opacification and glistenings in two hydrophobic acrylic intraocular lenses. Sci Rep. 2023;13(1):2822. doi:10.1038/s41598-023-29855-8
12. REGULATION (EU) 2017/745 OF THE EUROPEAN PARLIAMENT AND OF THE COUNCIL of 5 April 2017 on medical devices, amending Directive 2001/83/EC, Regulation (EC) No 178/2002 and Regulation (EC) No 1223/2009 and repealing Council Directives 90/385/EEC and 93/42/EEC; Available from: https://eurlex.europa.eu/legalcontent/ENG/TXT/PDF/?uri=CELEX:32017R0745.
13. McAlinden C, Pesudovs K, Moore JE. The development of an instrument to measure quality of vision: the Quality of Vision (QoV) questionnaire. Invest Ophthalmol Vis Sci. 2010;51(11):5537–5545. doi:10.1167/iovs.10-5341
14. Ribeiro F, Ferreira TB. Comparison of clinical outcomes of 3 trifocal IOLs. J Cataract Refract Surg. 2020;46(9):1247–1252. doi:10.1097/j.jcrs.0000000000000212
15. Ferreira TB, Ribeiro FJ, Silva D, Matos AC, Gaspar S, Almeida S. Comparison of refractive and visual outcomes of 3 presbyopia-correcting intraocular lenses. J Cataract Refract Surg. 2022;48(3):280–287. doi:10.1097/j.jcrs.0000000000000743
16. Martinez-de-la-Casa JM, Carballo-Alvarez J, Garcia-Bella J, et al. Photopic and mesopic performance of 2 different trifocal diffractive intraocular lenses. Eur J Ophthalmol. 2017;27(1):26–30. doi:10.5301/ejo.5000814
17. Piovella M, Colonval S, Kapp A, Reiter J, Van Cauwenberge F, Alfonso J. Patient outcomes following implantation with a trifocal toric IOL: twelve-month prospective multicentre study. Eye. 2019;33(1):144–153. doi:10.1038/s41433-018-0076-5
18. Boris M, Olga F, Nikolay S, et al. Visual results and subjective satisfaction after implantation of two different trifocal diffractive intraocular lenses models (AcrySof IQ PanOptix and AT LISA tri 839 MP). Eur J Ophthalmol. 2023;28:11206721231201561. doi:10.1177/11206721231201561
19. Shatz AC, Potvin R. Spectacle independence and quality of vision after bilateral implantation of a trifocal intraocular lens. Clin Ophthalmol. 2021;15:2545–2551. doi:10.2147/OPTH.S318203
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


