Back to Journals » Clinical Ophthalmology » Volume 17
Cross-Sectional Analyses of Factors Related to Digital Eye Strain Symptoms Among Children Using Online Learning Devices During the COVID-19 Pandemic in Thailand
Authors Chattinnakorn S , Chaicharoenpong K, Pongpirul K
Received 18 April 2023
Accepted for publication 13 June 2023
Published 21 June 2023 Volume 2023:17 Pages 1769—1776
DOI https://doi.org/10.2147/OPTH.S416877
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Supapan Chattinnakorn,1 Kullawan Chaicharoenpong,2 Krit Pongpirul3
1Department of Ophthalmology, Prapokklao Hospital, Chanthaburi, 22000, Thailand; 2Department of Community Medicine, Prapokklao Hospital, Chanthaburi, 22000, Thailand; 3Department of Preventive and Social Medicine, Chulalongkorn University, Bangkok, 10330, Thailand
Correspondence: Supapan Chattinnakorn, Department of Ophthalmology, Prapokklao Hospital, Chanthaburi, 22000, Thailand, Tel +66813405538, Fax +6639324861, Email [email protected]
Purpose: Globally, the COVID-19 pandemic has influenced academic studies. Since 2019, most schools in Thailand have implemented online learning. Thus, several students are experiencing eye problems, including stinging, blurred vision, and epiphora. This study investigated the prevalence, eye symptoms, and characteristics associated with digital eye strain (DES) in children using digital devices.
Patients and Methods: In this cross-sectional study, a self-administered electronic questionnaire via google forms was used to collect demographic data, digital device information, and DES characteristic information in children of age 8– 18 years using online digital devices. The data collection was conducted between December 2021 and January 2022. Moreover, multivariable logistic regression analysis was performed to evaluate the potential characteristics associated with DES in children.
Results: From a total of 844 parents, 782 parents completed the questionnaire. The mean age of the children was 12.42 ± 2.82 years (8– 18 years). During the pandemic, the most common duration of using digital devices was > 8 hours (39.90%), compared to only 2– 4 hours (36.70%) before. The prevalence of DES was 42.2% (330/782), divided into mild (29.8%), moderate (8.1%), and severe (4.3%) symptoms. The most common symptoms of DES included: a burning sensation in the eyes (55.24%), fear of worsening eyesight (53.07%), and excessive blinking of eyes (48.33%). The associated characteristics with DES were advanced age (OR=1.21, P< 0.001), refractive error with (OR=2.04, P=0.004) and without (OR=6.11, P< 0.001) correction, and unknown refractive error (OR=2.85, P< 0.001).
Conclusion: The use of digital devices are inevitable; therefore, regulating the duration of study and entertainment using digital devices, especially in older ages, and correcting refractive error in children, is necessary to ameliorate DES.
Keywords: computer vision syndrome, COVID-19 pandemic, online study, digital devices
Introduction
Globally, the COVID-19 pandemic has been affecting people since late 2019. In many Asian countries, including Thailand, lockdown policies were used to control the outbreak due to its easy spread, high virulence, and the public health system’s failure to support large numbers of infected patients.1 These reasons overwhelmingly affected the academic system, forcing the on-site study program to go online completely. Although online learning hours are similar to those spent on-site, children increasingly use digital devices for entertainment. In 2016, before COVID-19, Ichpujani et al reported the incidence of DES in India to be 17.9% and 43.6%, with digital device usage being 2–4 hours/day.2 In contrast, during COVID-19, Mohan et al reported the incidence of DES to be 50.23%, and the mean duration of digital device usage was 3.9 hours compared to 1.9 hours before COVID-19.3 Similarly, Ganne et al reported DES to be 50.6% among students attending online classes compared to 33.2% in the general population (P<0.0001).4 Smartphone was the most common digital devices in children at 58.3–61.7%.2,3,5
Parents and children often visited ophthalmologists during the pandemic for eye symptoms, including headache, heaviness of eyelid, tearing, itching, and blurred vision.3,5,6 Nevertheless, few studies have been conducted on DES in children, especially younger children.2–6
This study aimed to report the symptoms and characteristics associated with DES in higher, primary, and secondary school children using a self-administered electronic questionnaire.
Material and Methods
This observational, cross-sectional survey study was approved by the Chanthaburi Research Ethics Committee/region in eastern Thailand (approval number: 086/64) and was conducted in accordance with the Declaration of Helsinki on Biomedical Research Involving Human Subjects. The study was conducted between December 2021 and January 2022 and included most participants from Chanthaburi, whereas the rest were from Bangkok and other provinces in Thailand. The questionnaires were anonymous and self-administered electronically. In addition, the parents were informed about the objective of the questionnaire, and electronic informed consent was obtained from parents or guardians. The questionnaire was administered to parents via Google survey form through the school’s parents’ online activities. This study enrolled 8–18-year-old students in grades 3–12 who underwent online learning. The reason for choosing this age group was because they could understand and cooperate with the parents/guardian to complete the DES questionnaire.
The electronic questionnaire consisted of four parts: Informed consent, demographic data of children, digital device information, and DES questionnaire in the Thai language. The DES questionnaire was approved by a Thai ophthalmologist, and pilot tested among parents/guardians, before being administered to the study participants.
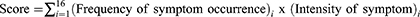
The computer vision syndrome questionnaire (CVS-Q) used in this study was developed by Segui et al.7 This CVS-Q evaluates the intensity and frequency of 16 eye symptoms, including burning sensation, itching in the eyes, foreign body sensation, watering, excessive blinking, redness, pain in the eye, heaviness in the eyelid, dryness, blurring of vision, double vision, difficulty in near vision, intolerance to light, colored halos, worsening of vision, and headache.
The frequency had three levels: Never (did not occur) = 0; Occasionally (sporadic or once a week) = 1; and Often or Always (2–3 times per week or almost daily) = 2. Moreover, the intensity had two levels: Moderate (not disturb daily life) =1 and Intense (2–3 times per week or almost daily) = 2.
CVS-Q Formula Calculation
The increase in scores corresponded with the increase in the severity of DES.
We estimated the sample size using the Z hypothesis.8
where Z = Z statistic for a level of confidence (95% = 1.96), P = expected prevalence or proportion (proportion of one; 50%, P = 0.5), d = precision (proportion of one; 5%, d = 0.05), and N = 384.
The sum of CVSQ scores ≥ 6 indicated the children experiencing DES. The severity of DES was divided based on total scores: mild = 6–12; moderate = 13–18; severe = ≥18.3
Statistical Analyses
All data were analyzed using the STATA version 16 (Stata Corp., College Station, Tx, USA). In addition, univariate and multivariate logistic analyses were performed. The odds ratio (OR) from multivariable ordinal logistic regression was used to calculate the following characteristics: age, sex, refractive error, and duration of using digital devices. P value <0.05 was considered statistically significant.
Results
In total, 844 children responded to the questionnaires through their parents/guardians. Among them, 782 met the inclusion criteria after excluding 61 children with eye disease affecting vision and one with incomplete answers in the questionnaire, as shown in Figure 1. The mean age of the participants in our study was 12.42 ± 2.82 years (8–18 years) from grades 3–12. Demographic data and clinical profiles are shown in Table 1.
 |
Table 1 Demographic and Clinical Profiles of Children Using Online e-Learning During the COVID-19 Pandemic |
 |
Figure 1 Flow diagram for data collection. Abbreviation: CVSQ, computer vision syndrome questionnaire. |
According to the questionnaire results, the prevalence of DES was 42.2%. In addition, mild, moderate, severe, and no symptoms were found in 233 (29.8%) (DES score, 6–12), 63 (8.1%) (DES score, 13–18), 34 (4.3%) (DES score, >18), and 452 (57.8%) (DES score, 0–5) children, respectively. The most common symptom of DES was “burning sensation in the eyes” (n = 432, 55.24%), followed by “thinking of worsening of eyesight” (n = 415, 53.07%) and “excessive blinking of eyes” (n = 378, 48.33%), as shown in Figure 2.
 |
Figure 2 Number of children affected by various symptoms of digital eye strain. |
The characteristics associated with DES in our study were advanced age (OR = 1.21 [1.10–1.22], P<0.001), refractive error with correction (OR = 2.04 [1.25–3.30], P = 0.004), refractive error without correction (OR = 6.11 [3.17–11.76], P<0.001), unknown refractive error (OR = 2.85 [1.99–4.10], P<0.001), and screen distance >18 inches (OR = 1.38 [1.00–2.00], P = 0.05), as shown in Table 2.
 |
Table 2 Multivariable Ordinal Logistic Regression Analysis of Risk Factors of Digital Eye Strain (Odds Ratio and 95% Confidence Interval) Based on Demographic and Clinical Profiles |
Discussion
Since COVID-19 has spread worldwide, many countries, including Thailand, have adopted the online system throughout 2021 and occasionally during the 2022 pandemic, including kindergartens, primary schools, and high schools.
DES, or computer vision syndrome, is defined as a group of eye symptoms caused by prolonged usage of computers, tablets, e-readers, and cell phones.9 The prevalence is reported to be approximately 50%.10 Sheedy et al divided the symptoms into two groups: external and internal symptoms. The external symptoms include a burning sensation in the eyes, dry eyes, irritation, and tearing. The internal symptoms associated with accommodation or binocular vision disorder include headache, eye strain, eye fatigue, etc, similar to a study conducted by Portello et al.11 The results of the study showed the most frequent symptom to be a burning sensation (55.24%), followed by a fear of worsening eyesight (53.07%) and excessive blinking (48.33%). Our results directly correlate with those of a study by Shantakumari et al in which undergraduate students in the United Arab Emirates reported burning sensation as the most frequent symptom12 followed by headache, and with Zayed et al in Egypt, who reported headache and burning sensation.13 In contrast, an Indian study by Mohan et al3 reported itching and headache as symptoms, whereas Gupta et al6 reported heaviness of the eyelid and redness as the most frequent symptoms. Moreover, “thinking of worsening of eyesight”, the second most common symptom, correlated with Wangsan et al, who reported on the degree of the severity, with the most intense symptom being the thought of worsening eyesight.14
Associated Characteristics
Age
The characteristics associated with DES in our study included advanced age (OR = 1.21; 95% CI [1.06–1.19], P<0.001), which means each year it will increase the risk by 21% for DES, directly correlating with several studies such as one by Li et al15 reported in China where an increased DES score correlated with older age, with an adjusted OR of 1.05 for per-year increase, P = 0.02, and Mohan et al3 reported that young adults (>14 years, P = 0.04) experienced more severe DES due to the longer duration of the online study.
Refractive Error
Refractive error is a major risk factor, especially without correction (OR = 6.34; 95% CI [3.32, 12.12], P = 0.001), followed by unknown refractive error (never had a refraction error check) (OR = 2.79 [1.94–4.01]), (P=0.001) and refractive error with correction (OR = 2.16; 95% CI [1.33–3.49], P = 0.002). The refractive error without correction by glasses (uncorrected visual acuity ≤ 0.65), especially in myopia (0.5 D – or less)-affected eye strain or asthenopia more than emmetropia16 correlates with the findings of Li et al,15 which demonstrated that refractive error is characteristic of DES. Furthermore, a study conducted by university students found that astigmatism is also characteristically associated with DES (OR = 1.75 [1.05–2.92]), (P=0.033); however, another study found no correlation of asthenopia with refractive errors, amblyopia, and strabismus.17 Nevertheless, we recommend correcting the refractive error (myopia and or astigmatism) using glasses for online study or digital devices, as it can improve visual focusing and decrease DES effectively.
Online Duration
During the COVID-19 pandemic, the rise in total duration, including online learning and entertainment, was >8 hours (n = 312 [39.90%]), 6–8 hours (n = 224 [28.64%]), and 4–6 hours (n = 149 [19.05%]). The use of digital devices for more than 8 hours (OR = 1.61 [95% CI 0.58–4.41], P = 0.054) may have potential clinical significance. Furthermore, information bias, recall bias, and inadequate sample sizes in older age may affect the statistical significance.
In many studies, increasing online screen time is an important risk factor for DES. For example, Wangsan et al reported that each extra hour increased DES by 12%, while other studies report that spending screen time >5 to 6 hours is a significant characteristic of DES.3,11,18 Moreover, other problems such as learning disabilities,19 sleep disturbance, and increased progression of myopia are arising.20
During the COVID-19 pandemic, Thai children spend the most digital duration for online study purposes, and the duration was 6–8 hours (n = 235 [30.05%]), followed by 4–6 hours (220 [28.13%]) per day, which is similar to the usual time spent on-site. We suggest that schools reduce online study duration and encourage outdoor activities to reduce the risk factor of DES in children.
Moreover, we recommend that parents pay attention to breaking the online duration in children using the 20-20-20 rule. In this technique, one should look away from their digital monitor after 20 min at a 20 feet distance for 20s to reduce eye fatigue and DES.21
Therefore, in our study, the characteristics associated with DES were not related to the male sex (OR 1.31 [0.97–1.77] P=0.08) and digital devices (OR = 1.07 [0.77–1.48], P=0.77). However, Fischer-Grote and Lee found that the female sex was a risk factor22 as opposed to the male sex in their study, similar to the study conducted by Mohan (P = 0.0004). In another study, smartphone usage was significantly associated with DES3 because smartphones have a smaller screen; therefore, children have a shorter viewing distance, which requires more accommodation and affects the extraocular muscle, resulting in conjugation and transient myopia, eye strain, headache, and facility problem.12,23
Near vision results in more accommodation. In our study, the distancing of <18 inches was not statistically significant (OR = 1.34, 95% CI [0.97–1.84], P=0.074).
This study has several limitations. First, this was a cross-sectional study without comparison with a control group. Second, this study was conducted using a self-administered subjective questionnaire by parents or guardians, which may have introduced recall and information bias. In addition, correlations between objective and subjective measures of visual fatigue are not always apparent.24 Third, there was no geographic control in the online survey. Finally, methodological error from discrepancies in reporting symptoms by the child and parent’s perspectives can occur, especially when it involves younger children. The severity of the eye symptoms communicated to the parents by the children is often lower than that experienced and may not reflect the true state of the symptom.
Conclusion
The refractive error and older age were risk factors for DES in children using digital devices during the COVID-19 pandemic in Thailand. The online duration may have potential clinical significance.
In addition, correcting the refractive error by wearing glasses, resting the eyes, and limiting online time can ameliorate DES problems, especially in older children with a higher risk factor.
Acknowledgments
We would like to thank the parents, teachers, and guardians who participated in the study. We also thank Surasak Im-iam, the statistician at the Department of Thai Traditional Medicine, Prapokklao Hospital, for supporting the study design and statistical analysis.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Coronavirus disease (COVID-19): schools. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19-schools.
2. Ichhpujani P, Singh RB, Foulsham W, Thakur S, Lamba AS. Visual implications of digital device usage in school children: a cross-sectional study. BMC Ophthalmol. 2019;19:76. doi:10.1186/s12886-019-1082-5
3. Mohan A, Sen P, Shah C, Jain E, Jain S. Prevalence and risk factor assessment of digital eye strain among children using online e-learning during the COVID-19 pandemic: digital Eye Strain Among Kids (DESK study-1). Indian J Ophthalmol. 2021;69:140–144. doi:10.4103/ijo.IJO_2535_20
4. Ganne P, Najeeb S, Chaitanya G, Sharma A, Krishnappa NC. Digital eye strain epidemic amid COVID-19 pandemic - a cross-sectional survey. Ophthalmic Epidemiol. 2021;28:285–292. doi:10.1080/09286586.2020.1862243
5. Demirayak B, Yılmaz Tugan B, Toprak M, Çinik R. Digital eye strain and its associated factors in children during the COVID-19 pandemic. Indian J Ophthalmol. 2022;70:988–992. doi:10.4103/ijo.IJO_1920_21
6. Gupta R, Chauhan L, Varshney A. Impact of e-schooling on digital eye strain in coronavirus disease era: a survey of 654 students. J Curr Ophthalmol. 2021;33:158–164. doi:10.4103/joco.joco_89_20
7. Seguí Mdel M, Cabrero-García J, Crespo A, Verdú J, Ronda E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol. 2015;68:662–673. doi:10.1016/j.jclinepi.2015.01.015
8. Daniel WD. Biostatistics: A Foundation of Analysis in the Health Sciences.
9. American Optometric Association. Computer vision syndrome (Digital eye strain); 2022. Available from: https://www.aoa.org/healthy-eyes/eye-and-vision-conditions/computer-vision-syndrome?sso=y.
10. Sheedy JE, Hayes JN, Engle J. Is all asthenopia the same? Optom Vis Sci. 2003;80:732–739. doi:10.1097/00006324-200311000-00008
11. Portello JK, Rosenfield M, Bababekova Y, Estrada JM, Leon A. Computer-related visual symptoms in office workers. Ophthal Physiol Opt. 2012;32:375–382. doi:10.1111/j.1475-1313.2012.00925.x
12. Shantakumari N, Eldeeb R, Sreedharan J, Gopal K. Computer use and vision-related problems among university students in Ajman, United Arab Emirate. Ann Med Health Sci Res. 2014;4:258–263. doi:10.4103/2141-9248.129058
13. Zayed HAM, Saied SM, Younis EA, Atlam SA. Digital eye strain: prevalence and associated factors among information technology professionals, Egypt. Environ Sci Pollut Res. 2021;28:25187–25195. doi:10.1007/s11356-021-12454-3
14. Wangsan K, Upaphong P, Assavanopakun P, et al. Self-reported computer vision syndrome among Thai university students in virtual classrooms during the COVID-19 pandemic: prevalence and associated factors. Int J Environ Res Public Health. 2022;19:3996. doi:10.3390/ijerph19073996
15. Li R, Ying B, Qian Y, et al. Prevalence of self-reported symptoms of computer vision syndrome and associated risk factors among school students in China during COVID-19 pandemic. Ophthalmic Epidemiol. 2022;29:363–373. doi:10.1080/09286586.2021.1963786
16. Abdi S, Lennestrand G, Pansell T, Rydberg A. Orthoptic findings and asthenopia in a population of Swedish schoolchildren aged 6 to 16 years. Strabismus. 2008;16:47–55. doi:10.1080/09273970802020243
17. Ip JM, Robaei D, Rochtchina E, Mitchell P. Prevalence of eye disorder in young children with eyestrain complaints. Am J Ophthalmol. 2006;142:495–497. doi:10.1016/j.ajo.2006.03.047
18. Al Tawil L, Aldokhayel S, Zeitouni L, Qadoumi T, Hussein S, Ahamed SS. Prevalence of self-reported computer vision syndrome symptoms and associated risk factors among university students. Eur J Ophthalmol. 2020;30:189–195. doi:10.1177/1120672118815110
19. Handler SM, Fierson WM; Section on on Ophthalmology, Council on Children with Disabilities, American Academy of Ophthalmology, American Association of Certified Orthoptics. Learning disabilities, dyslexia, and vision. Pediatrics. 2011;127:e818–e856. doi:10.1542/peds.2010-3670
20. Cai T, Zhao L, Kong L, Du X. Complex interplay between COVID-19 lockdown and myopic progression. Front Med. 2022;9:853293. doi:10.3389/fmed.2022.853293
21. Anshel JR. Visual Ergonomics in the workplace. AAOHN J. 2007;55:414–420. doi:10.1177/216507990705501004
22. Fischer-Grote L, Kothgassner OD, Felnhofer A. Risk factors for problematic smartphone use in children and adolescents: a review of existing literature. Neuropsychiatr. 2019;33:179–190. doi:10.1007/s40211-019-00319-8
23. Sterner B, Gellerstedt M, Sjöström A. Accommodation and the relationship to subjective symptoms with near work for young school children. Ophthal Physiol Opt. 2006;26:148–155. doi:10.1111/j.1475-1313.2006.00364.x
24. Sheppard AL, Wolffsohn JS. Digital eye strain: prevalence, measurement and amelioration. BMJ Open Ophthalmol. 2018;3:e000146. doi:10.1136/bmjophth-2018-000146
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.