Back to Journals » Clinical Interventions in Aging » Volume 18
Cross-Cultural Adaptation, Validity, and Reliability Testing of the Tilburg Frailty Indicator (TFI) Amharic Version for Screening Frailty in Community-Dwelling Ethiopian Older People
Authors Kasa AS , Drury P, Chang HCR, Lee SC, Traynor V
Received 13 April 2023
Accepted for publication 27 June 2023
Published 24 July 2023 Volume 2023:18 Pages 1115—1127
DOI https://doi.org/10.2147/CIA.S416942
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Ayele Semachew Kasa,1,2 Peta Drury,1 Hui-Chen Rita Chang,1,3 Shu-Chun Lee,4 Victoria Traynor1
1School of Nursing, Faculty of Science, Medicine, and Health, University of Wollongong, Wollongong (UOW), New South Wales, Australia; 2Department of Adult Health Nursing, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia; 3School of Nursing and Midwifery, Western Sydney University, Parramatta South Campus, Parramatta, New South Wales, Australia; 4School of Gerontology and Long-Term Care, College of Nursing, Taipei Medical University, Taipei, Taiwan
Correspondence: Ayele Semachew Kasa, Email [email protected]; [email protected]
Background: Frailty is a global health problem, including in African countries. Despite this, no reliable or valid frailty instruments incorporate any African language, and no research exists to cross-culturally adapt and test the validity and reliability of instruments commonly used in other countries for use within African countries. The Tilburg Frailty Indicator (TFI) is a reliable and validated instrument with the potential to be relevant for older populations living in Africa. This study aimed to develop the TFI Amharic (TFI-AM) version for use within Ethiopia.
Methods: This study employed psychometric testing and the evaluation of a translated and adapted instrument. The original English language version of the TFI was translated and culturally adapted into Amharic using the World Health Organization process of translation and adaptation of an instrument. A convenience sample of ninety-six community-dwelling older people 60 years and over was recruited. Cronbach’s alpha was used for the analysis of the internal consistency of the TFI Amharic (TFI-AM) version using IBM SPSS 26.0 (IBM Corp., Armonk, NY, USA). Face and content validities of the TFI-AM were determined.
Results: The TFI-AM total mean score was 5.76 (± 2.89). The internal consistency of the TFI-AM was very good with an overall Cronbach alpha value of 0.82. The physical domain showed the highest reliability with a 0.75 Cronbach’s alpha value while the social domain was the lowest with a 0.68 Cronbach’s alpha value. The Cronbach’s alpha reliability coefficients of the instrument ranged from 0.68 to 0.75. The item content validity index value ranged from 0.83 to 1.0 and the total content validity index average for the instrument was 0.91.
Conclusion: The TFI-AM is reliable, valid, and reproducible for the assessment of frailty among community-dwelling older populations in Ethiopia. TFI-AM proved an easy-to-administer, applicable and fast instrument for assessing frailty in community-dwelling older populations.
Keywords: Tilburg frailty indicator, Amharic version, validity, reliability, older persons, frailty, Ethiopia
Background
Global ageing trends are resulting in increased challenges of providing healthcare for older populations, particularly frail older people.1 As the population ages worldwide, the number of people classified as frail also increases, with a disproportionate rise in the burden across low-income regions such as sub-Saharan Africa (SSA).2 Over the next three decades, the second fastest rise in the number of older people is foreseen in SSA with an expected growth from 32 million in 2019 to 101 million by 2050.3 A recent review and meta-analysis on the prevalence of frailty in older people living in Africa showed the rate of frailty is rising with an overall prevalence of 38.64% [citation by authors to remain anonymised]. The average life expectancy in SSA is higher than it was two decades ago which leads to a greater proportion of frail older people in the region.4,5
Frailty is a strong predictor of adverse health outcomes, including disability, falls, mortality, hospitalisation, and institutionalisation.6–10 Consequently, the development of a valid screening instrument to identify frailty is crucial for improving the health of frail older people at risk of adverse health outcomes. There are a range of frailty instruments that can distinguish frail and non-frail older people.11–15 These screening instruments reflect different operational definitions of frailty: (1) focusing on physical functioning;16 and (2) application of multidimensional approach encompassing biological, psychological, and social domains.17,18 However, the validity of these instruments is subject to significant debate, and not one instrument is considered the gold standard.19,20 The multidimensional concept of frailty has been studied more recently.21–23 One of the multidimensional screening instruments, the Tilburg Frailty Indicator (TFI), is a frailty assessment instrument with good psychometric properties,14,21 and easy to administer, and a user-friendly for assessing frailty in community-dwelling older people.21 Moreover, of the 38 multicomponent frailty assessment instruments, the TFI has the most strong evidence for the reliability and validity of its psychometric properties.24,25
The TFI was developed by Gobben et al22 based on the Integral Conceptual Model of Frailty (ICMF).26 The TFI instrument contains 15 items that takes less than 15 minutes to complete. The TFI has been used in clinical trials to identify frail participants, monitor changes in frailty status over time, and evaluate the effectiveness of interventions.27–29 The usefulness of the TFI in intervention studies also attributed to its ease of administration, validity and reliability, multidimensional nature, and risk stratification.21,30
The FRAIL Scale,31 Edmonton Frail Scale (EFS),32,33 Clinical Frailty Scale (CFS),34,35 Groningen Frailty Indicator (GFI),36,37 PRISMA-7,38 and Tilburg Frailty Indicator (TFI),39–41 instruments were cross culturally adapted to measure frailty. The TFI was one of the multidimensional frailty measurement instruments translated and adapted for use in many non-English speaking European countries,23,39,41–44 including Asia25,45 and South America.46 To date, the TFI has not been tested in any developing countries and has never been used in studies of SSA older people. This study will be the first test of the TFI in a developing country, specifically the sub-Saharan country of Ethiopia.
This study aimed to translate the TFI into Amharic, the national language of Ethiopia, to undertake a cross-cultural adaptation and determine the validity and reliability of the TFI for use in Ethiopia. The research team are undertaking this study to enable them to use the TFI-AM version to measure the outcome of their nurse-led frailty intervention study in Ethiopia [citation by authors remains anonymised].
Methods
Study Setting, Design, and Period
The methodological research design used included translating and adapting the original English language version of the TFI into Amharic language and undertaking validity and reliability testing of the TFI-AM version. The study was carried out using a cross-sectional study design with older people living in Bahir Dar City, Amhara Region, Ethiopia from October to November 2022.
Eligibility Criteria
The year that “old age” commences is determined by a setting and the formal cutoff point legislated in social policy for each country.47 In Ethiopia, the cutoff point for old age is 60 years.48,49 The inclusion criteria for this study were older people 60 years or over, residing in Bahir Dar, Ethiopia, who were community-dwelling, able to communicate verbally, not wholly immobile (bed-ridden) and intact cognitive status.
Sample Size and Procedures
In previous studies, it has been found that a sample size of 50 or more is needed for a reliability estimate of an instrument.41,50 Furthermore, for the calculation of a reliability coefficient on a scale measurement a sample size of 50 and more is sufficient.50 Moreover, other studies suggest the minimum sample size should be at least five times larger than the number of variables being analysed.25,41 The TFI consists of a total of 15 items that will be analysed. Therefore, a minimum of 75 community-dwelling older people were required for this validity and reliability study. To ensure a larger sample, the data were collected from 96 community-dwelling older people living in Bahir Dar, Ethiopia. After obtaining a written informed consent, a survey conducted on convenient samples of community-dwelling older people using the new TFI-AM version. The TFI-AM was administered using a face-to-face interview technique conducted by a Registered Nurse who worked in a public health facility in Bahir Dar, Ethiopia. This study was in complied with The Declaration of Helsinki.
Instrument Description
The TFI comprises of 15 self-reported items separated into three distinct domains of health for older people: (i) physical domain consists of eight items related to the physical health, (ii) psychological domain consists of four items related to the psychological health; and (iii) social domain consists of three items related to social relations and social support. Eleven items of the TFI have two response categories of “yes” or “no”, while three items from the psychological domain and one item from the social domain have three response categories as “yes”, “no”, or “sometimes”. Except item 19 in the TFI, “Yes” or “sometimes” responses were allocated a score 1 point each, while item 19 in the TFI, “no” and “sometimes” responses were allocated a score of zero (0). For all other items, “no” responses were scored as zero (0). The instrument’s total score ranged from 0 to 15: the higher the score, the higher one’s frailty. Frailty is diagnosed when the total TFI score is ≥5.22,41
Instruments Development: Language Translation and Adaptation
Written permission to perform the TFI translation and adaptation was obtained from the developer of the TFI.21 A standard guideline was used for translation and cultural adaptation of the original English language version of the TFI51–53 into Amharic. Translators were given information regarding the instrument and the population to be investigated to make sure that the original concept underlying each item was maintained in the translation process.54 The translations emphasised the conceptual equivalent of a word or phrase, not a word-for-word translation.51
Two Amharic-speaking academics from universities in Ethiopia who are fluent in English language independently translated the TFI English language version into Amharic. The translations from these two individuals were merged/created into a single Amharic form by a third person who is proficient both in English and Amharic languages. The TFI translated instrument created in Amharic was back translated into English language by second person proficient in English and Amharic languages who was not involved in the other stages of the translation. The final English translated version from Amharic was sent to the developer of the original TFI for approval before the reliability study was commenced. The developer provided approval of TFI-AM version with no changes. The final Amharic version of the TFI (TFI-AM) was adapted and tested for its reliability on a selected sample of community-dwelling older people living in Bahir Dar, Ethiopia.
Validity and Reliability Assessment
Validity
Validation of the instrument was completed before administration of the final TFI_AM instrument to any study participant. Face validity and content validity were used to test the validity of the TFI-AM. To evaluate whether respondents had a clear understanding of the items in the instrument, and the time required to complete the final translated and adapted TFI-AM version was piloted on a randomly selected sample of 20 older people living in Bahir Dar.
Face Validity
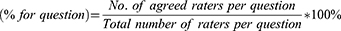
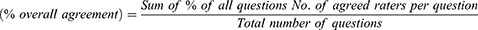
The TFI-AM version was rated by eight healthcare professionals who are either currently working or who previously worked in primary healthcare including nurses, community health workers, public health professionals, and public health researchers. The raters were provided with a cover letter and response sheet. The cover letter provided directions to guide them and outline their responsibilities on how to rate the face validity of the instrument. In determining the face validity of the instrument, the percentage (%) of agreement between raters was calculated using each question and overall agreement using the equations below.
In determining the face validity of the instrument, percentage (%) of agreement less than 80%, 80–89% and greater than or equal to 90% indicates a poor, substantial and full strength of agreement respectively. When items in an instrument are rated as a poor and substantial strength of agreement they need restructured and revised, respectively.55
Content Validity
The TFI-AM was rated by six researchers and healthcare professionals with expertise in community healthcare including the care of older people. The group of raters consisted of professionals from nursing, dietetics, physiotherapy, psychiatry, and public health. They were provided with a cover letter and response sheet. The cover letter provided directions to guide them and outline their responsibilities on how to rate the content validity of the instrument. They rated the items in the translated version in terms of clarity and relevance on a 4-point scale as (1: The item is not relevant and not clear, 2: The item is somewhat relevant and needs some revision, 3: The item is quite relevant and clear, and 4: The item is highly relevant and clear).56,57 The item level content validity index (I-CVI) was computed as the number of experts giving a rating 3 or 4 to the relevancy of each item, divided by the total number of experts.56
The I-CVI values range from 0 to 1 where I-CVI > 0.79 is acceptable and the item is relevant, 0.70 to 0.79, items need revised, and items with values below 0.70 need removed.56 A total content validity index average of the scale (S-CVI/Ave) of 0.80 or higher was taken as an acceptable level.58
Internal Consistency
The internal consistency of the instrument was measured after the data were collected from the eligible 96 community-dwelling older people who completed the TFI-AM version. It was measured using the Cronbach’s coefficient alpha. This statistic provides an indication of the average correlation among all of the items that make up the scale. Values range from 0 to 1, with higher values indicating the instrument is more reliability.59 Cronbach’s alpha values <0.60, 0.60 to < 0.70, 0.70 to <0.80, 0.80 to <0.90 and 0.90 and more indicate poor, moderate, good, very good and excellent level of internal consistency, respectively.60,61
Ethics
This study has been approved by the University of Wollongong (UOW) Human Research Ethics Committee, approval number of 2022/212. This study has also been approved by the Institutional Review Board (IRB) of College of Medicine and Health Sciences, Bahir Dar University (BDU), approval number of 563/2022. After the participants agreed to participate in this study, a written informed consent was taken.
Data Analysis
The collected data were checked for completeness and accuracy. Fully completed and cleaned data were entered into the IBM SPSS 26.0 (IBM Corp., Armonk, NY, USA) for analyses. Categorical data were presented as numbers and percentages and continuous data as mean (± SDs). Correlation of the scores of the three domains of the TFI-AM with the total score of TFI-AM was conducted using Pearson correlation test. A correlation coefficient of 0.1 to 0.3, 0.3 to 0.5, and >0.5 was considered as weak, moderate, and strong correlations, respectively.40 Cronbach’s alpha was used for the analysis of the internal consistency of the TFI-AM.61 Percentage (%) of agreement among raters were conducted to evaluate the face validity of the instrument. The item level content validity index (I-CVI) and the total content validity index average for the scale (S-CVI/Ave) were undertaken using an Excel spreadsheet to determine the validity of the instrument.
Result
Sociodemographic Characteristics
A total of 96 older people were recruited to carry out the instrument adaptation, validity and reliability testing. More than sixty-four percent (64.6%) of the study participants were female. The mean age of the study participants was 65.16 (± 5.08) with age range from 60 to 88 years. Based on the TFI cutoff point of 5 for assessing frailty, 55.2% of the study participants were frail. Of these, 56.5% were female older people. More than sixty-four percent (64.6%) of the study participants were living with their spouse. Of these, 54.8% were screened as frail. More than 80% of the study participants had caregivers/assistants to support them in their daily living. More than 60% of those who had no care giver assistant were screened for frailty (Table 1).
 |
Table 1 Sociodemographic Characteristics of the Study Participants, 2022 (n = 96) |
Face Validity
Five TFI items (item 5, 6, 7, 12 and 15) of the translated version of TFI-AM was between 80% and 89%. The score of the five items of the TFI-AM was between 80% and 89% and the scores of the rest of each item were over 90%. The overall scale agreement was found to be excellent, with overall agreement of 95.8%. The comments received on the readability and clarity of the items were discussed with the raters. A minor revision on the five items (item 5, 6, 7, 12 and 15) whose score was between 80% and 89% was undertaken after a discussion with the raters.
Content Validity
The item level content validity index (I-CVI) and total content validity index average for the scale (S-CVI/Ave) of the TFI-AM was rated. The I-CVI of the TFI-AM revealed an acceptable value ranging from 0.83 to 1.0 and an S-CVI/Ave value of 0.91 (Table 2).
 |
Table 2 Content Validity of the TFI-AM, 2022 |
Reliability Test Statistics
The total TFI-AM mean score was 5.76 (±2.89). There was a range in the mean scores across the TFI-AM domains: (i) the mean score of the physical domain which had eight items was the highest with 3.36 (±2.06); (ii) the psychological domain which has four items had a mean score of 1.32 (± 1.17) and (iii) the social domain with three items had a mean score of 1.07 (±0.42). The internal consistency of the TFI-AM was very good with an overall Cronbach alpha value of 0.82. The physical domain showed the highest reliability with a 0.75 Cronbach’s alpha value which corresponds to good reliability. The psychological and social domains showed good and moderate reliability with Cronbach’s alpha value of 0.70 and 0.68, respectively. The physical and psychological domain scores were strongly and positively correlated to the total TFI score, r (96) = 0.91, p < 0.01 and r (96) = 0.71, p < 0.01, respectively. The social domain score had moderate correlation with the total TFI-AM score, r (96) = 0.41, p < 0.01. The statistical characteristics of individual items in the TFI-AM and their mean ranged from 0.09 to 0.58 (Table 3).
 |
Table 3 Statistical Characteristics and the Reliability of Items of the Amharic Version of the Tilburg Frailty Indicator (TFI-AM), 2022 |
Discussion
Several studies have indicated that the prevalence of frailty is increasing in the global ageing population.62,63 Commonly adopted frailty assessment instruments evaluate only physical frailty and report a lower rates of frailty in community-dwelling older people, one would expect a higher rate of frailty with the TFI as it encompasses the psychological and social aspects of frailty.62 The proportion of frailty in the current study was 55.2%. Various validation studies on TFI in Brazil,46 Portuguese41 and the Netherlands64 revealed more than 30%, 40% and 35.7% of older people with frailty. The higher rates of frailty in the current study may be attributed to malnutrition in older people in the region being extremely high.65 The increasing burden of malnutrition and non-communicable diseases coupled with insufficient access to healthcare and inadequate living condition for older people in Ethiopia66,67 may contribute to higher rates of frailty. However, compared to the current result, a TFI validation study from Turkey showed that the rate of frailty was 63.6%.40 The reason for relatively lower rates of frailty in our study, compared to the Turkey study, may be associated with study participants being recruited from the community with a baseline age of ≥60 years. Whereas participants in Turkey were older people admitted to a geriatric outpatient clinic with a relatively higher age (≥70 years). These factors contribute to a higher frailty rate in Turkey study. Our sample should not be considered representative of a general population of older people because study participants were recruited and examined from only one region in Ethiopia. Thus, a true prevalence of frailty can be either lower or higher and should not be determined on the basis of a validation study.
The finding of the current study demonstrated that the TFI-AM version demonstrated a very good level of reliability and an acceptable content validity. This finding was consistent with studies conducted in other countries. A study from the Netherlands reported that 0.79,22 0.8068 and a study from Brazil showed a 0.7846 Cronbach’s alphas values of reliability statistics for the TFI instrument. Across different studies, it was found that the reliability coefficient of the TFI was acceptable.21
The reliability statistics for the Polish version of the TFI were 0.7241, 0.7423 and it was 0.6644 for the Italian version for frailty syndrome. The German translation and psychometric testing also revealed a 0.6744 reliability statistics of the TFI. In comparison to studies conducted in various countries, the current study’s reliability statistics were higher. The higher reliability of the TFI-AM in the current study could be attributed to the fact that the instrument was validated and piloted before being administered to any study participant using a culturally appropriate and contextually relevant processes. These efforts contribute to a more consistent set of questions with a higher overall level of reliability.
The current study also demonstrated an acceptable reliability for the individual domains of the TFI-AM. Accordingly, the finding showed that the physical, psychological, and social domains of the TFI-AM reliability was 0.75. 0.70 and 0.68, respectively. These findings showed a better reliability of the domains of the TFI-AM than studies conducted across other countries. The study from the Netherlands showed that the physical, psychological, and social domains of TFI were 0.74, 0.61, and 0.51,68 respectively. Another instrument validation study with 479 community-dwelling people of 75 years and older in the Netherlands showed that a 0.70 reliability statistic for the physical domain, 0.63 for the psychologic domain, and 0.34 for the social domain.22 A study from Turkey also found that the reliability statistics for physical, psychological, and social domains were 0.727, 0.675, and 0.049 respectively.69
An instrument has face validity if it seems to identify what it is intended to measure and that it will work.70 The current study demonstrated that the face validity and scale agreement was excellent. This finding is in line with a study conducted in the Netherlands demonstrating that the face validity was satisfactory.22 A study in Denmark, however, proposed that the TFI should be further tested in clinical practice.39 The content validity relates to whether a measurement instrument contains all essential components of the construct to be measured.71 The content validity of the TFI-AM demonstrated an acceptable value of I-CVI (0.83 to 1.0). According to the current study, the TFI-AM contains the important frailty items. This finding is in line with reports from various studies which reported that the TFI contains the majority of important frailty items.22,72 However, it was noted that some important items were missed from a study conducted in Denmark.73
The TFI has been validated in various populations and countries, showing good reliability and validity.21,25,74 The TFI assesses frailty across physical, psychological and social domains.75,76 This multidimensional approach to frailty contributes to clinical trials studying interventions that target different aspects of frailty.
The results of this study can contribute to the understanding of frailty across different cultural, socioeconomic and low-income settings. This can assist to identify context-specific determinants of frailty and inform culturally appropriate and contextually relevant interventions. It can also contribute to developing local research insights related to ageing and frailty. Frailty research such as frailty tool validation in low-income countries will contribute to strengthening the field of research within gerontology and geriatrics.
Strengths and Limitations
This is the first effort to translate and culturally adapt the TFI for use within SSA and specifically from the Ethiopian older persons’ perspective. This instrument translation will allow for the assessment of frailty and evaluating interventions aimed at addressing frailty among older people in Ethiopia. Importantly, this instrument adaptation translation will contribute to researchers, health care professionals and policy makers by serving as an early detection instrument. This will also assist in determining possible interventions for improving the health status of older people in low-income settings. Resulting the insufficient research outputs on frailty with no evidence of interventions to decrease frailty in SSA, a research team aimed to investigate and measure the effectiveness of a nurse-led intervention to decrease frailty status of Ethiopian older people [citation by authors to remain anonymised]. Such efforts will contribute on how to reduce and possibly avert frailty in older people from SSA perspective.
However, the results of the present study should be understood in the context of potential limitations. Other forms of reliability and validity tests need to be carried out. The test–retest reliability or the construct and predictive validity of the instrument were not assessed. Therefore, our results indicate, but do not prove, that the translated version of the TFI is a valid and reliable measure of the common attributes of frailty. Future studies could examine test–retest reliability, construct, and predictive value of the TFI with respect to other health outcomes including, relocation to nursing homes, higher rate of morbidity, admission to hospital, longer length of stay in hospital and increased rates of mortality. Moreover, study participants were recruited from one region in Ethiopia resulting in an unrepresentative result. Future research is needed to increase the sample size and confirm the generalisability in different Amharic speaking regions.
Conclusion
The findings provide initial evidence that the TFI-AM version demonstrated a very good level of reliability and acceptable content validity for assessing frailty among community-dwelling older people from the Ethiopian context. The Amharic adaptation of the TFI proved a useful, easy to administer and fast for assessing frailty on community-dwelling older people. Nevertheless, future research is needed to determine the efficacy of the TFI-AM for detecting frailty in community-dwelling Ethiopian older people.
Ageing research and the development of instruments to screen for age-related problems will benefit policymakers in low-income settings. This will assist them to emphasise on the multidimensional needs of older people and develop strategies to strengthen the healthcare of older people.
Abbreviations
I-CVI, Item level content validity index; ICMF, Integral Conceptual Model of Frailty; TFI, Tilburg Frailty Indicator; TFI-AM, Tilburg Frailty Indicator Amharic Version; SSA, Sub Saharan Africa; S-CVI/Ave, total content validity index average for the scale; UOW, University of Wollongong.
Acknowledgment
We would like to express our sincere gratitude to Professor Robbert J Gobbens for his permission to undertake this cross-cultural adaptation, validity and reliability testing of the TFI to Ethiopian context. We also extend our thanks to him for reviewing the manuscript. The authors sincerely thank all the study participants for their time and cooperation to participate in this study. Lastly, we also would like to acknowledge UOW for granting the University Postgraduate Award (UPA) Scholarship and International Postgraduate Tuition Award (IPTA).
Disclosure
The authors declare that there is no conflicts of interest in this work.
References
1. Bunt S, Steverink N, Olthof J, van der Schans HJ, Hobbelen JSM. Social frailty in older adults: a scoping review. Eur Eur J Ageing. 2017;14(3):323. doi:10.1007/s10433-017-0414-7
2. Kinsella K, He W. An aging world: 2008 U.S.Census Bureau, international population reports. Washington, DC: U.S.Government Printing Office; 2009.
3. United Nations. World Population Ageing 2019 Highlights: Department of Economics and Social Affairs; 2019.
4. Wiysonge C. People in Africa live longer. But their health is poor in those extra years; 2018. Available from: https://theconversation.com/people-in-africa-live-longer-but-their-health-is-poor-in-those-extra-years-108691.
5. Keshena N. A scoping review of age-related health conditions among geriatric populations in sub-Saharan Africa; 2019.
6. Kojima G. Frailty as a predictor of future falls among community-dwelling older people: a systematic review and meta-analysis. J Am Med Dir Assoc. 2015;16(12):1027–1033. doi:10.1016/j.jamda.2015.06.018
7. Kojima G. Frailty as a predictor of emergency department utilization among community-dwelling older people: a systematic review and meta-analysis. J Am Med Dir Assoc. 2019;20(1):103–105. doi:10.1016/j.jamda.2018.10.004
8. Kojima G. Frailty as a predictor of hospitalisation among community-dwelling older people: a systematic review and meta-analysis. J Epidemiol Community Health. 2016;70(7):722–729. doi:10.1136/jech-2015-206978
9. Peng Y, Zhong G-C, Zhou X, Guan L, Zhou L. Frailty and risks of all-cause and cause-specific death in community-dwelling adults: a systematic review and meta-analysis. BMC Geriatr. 2022;22(725):1–21. doi:10.1186/s12877-022-03404-w
10. Tavares J, Sa-Couto P, Reis JD, Boltz M, Capezuti E. The role of frailty in predicting 3 and 6 months functional decline in hospitalized older adults: findings from a secondary analysis. Int J Environ Res Public Health. 2021;18(13):7126. doi:10.3390/ijerph18137126
11. Faller JW, Do Nascimento Pereira D, de Souza S, Nampo FK, de Souza Orlandi F, Matumoto S. Instruments for the detection of frailty syndrome in older adults: a systematic review. PLoS One. 2019;14(4):1–23. doi:10.1371/journal.pone.0216166
12. Gobbens RJ, Luijkx KG, Wijnen-Sponselee MT, Schols JM. Toward a conceptual definition of frail community dwelling older people. Nurs Outlook. 2010;58(2):76–86. doi:10.1016/j.outlook.2009.09.005
13. Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10. doi:10.1016/j.ejim.2016.03.007
14. Sutton JL, Gould RL, Daley S, et al. Psychometric properties of multicomponent tools designed to assess frailty in older adults: a systematic review. BMC Geriatr. 2016;16(1):55. doi:10.1186/s12877-016-0225-2
15. Ma L. Current situation of frailty screening tools for older adults. J Nutr Heal Aging. 2019;23(1):111–118. doi:10.1007/s12603-018-1123-4
16. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol Ser. 2001;56(3):146–156. doi:10.1093/gerona/56.3.M146
17. David B, Chris MacKnight HB. Models, definitions, and criteria of frailty. Aging Clin Exp Res. 2003;15(3):3–29.
18. Roppolo M, Mulasso A, Gobbens RJ, Mosso CO, Rabaglietti E. A comparison between uni- and multidimensional frailty measures: prevalence, functional status, and relationships with disability. Clin Interv Aging. 2015;10:1669–1678. doi:10.2147/CIA.S92328
19. de Vries NM, Staal JB, van Ravensberg CD, Hobbelen JSM, Olde Rikkert MGM, Nijhuis-van der Sanden MWG. Outcome instruments to measure frailty: a systematic review. Ageing Res Rev. 2011;10(1):104–114. doi:10.1016/j.arr.2010.09.001
20. Lee H, Lee E, Jang I-Y. Frailty and comprehensive geriatric assessment. J Korean Med Sci. 2020;35(3):1.
21. Gobbens RJ, Uchmanowicz I. Assessing frailty with the tilburg frailty indicator (TFI): a review of reliability and validity. Clin Interv Aging. 2021;16:863–875. doi:10.2147/CIA.S298191
22. Gobbens RJJ, Van assen MALM, Luijkx KG, Wijnen-Sponselee MT, Schols JMGA. The tilburg frailty indicator: psychometric properties. J Am Med Dir Assoc. 2010;11(5):344–355. doi:10.1016/j.jamda.2009.11.003
23. Uchmanowicz I, Jankowska-Polańska B, Uchmanowicz B, Kowalczuk GR, Gobbens RJJ. Validity and reliability of the Polish version of the Tilburg frailty indicator (TFI). J Frailty Aging. 2016;5(1):27–32. doi:10.14283/jfa.2015.66
24. Gobbens R, Schols JM, van Assen M. Exploring the efficiency of the Tilburg Frailty Indicator: a review. Clin Interv Aging. 2017;12:1739–1751. doi:10.2147/CIA.S130686
25. Lin C, Liu C-Y, Rong J-R, et al. Psychometric properties of the taiwanese version of the tilburg frailty indicator for community-dwelling older adults. Healthc. 2021;9(9):1–11. doi:10.3390/healthcare9091193
26. Gobbens RJJ, Luijkx KG, Wijnen-Sponselee MT, Schols JMGA. Towards an integral conceptual model of frailty. J Nutr Health Aging. 2009;14(3):175–181. doi:10.1007/s12603-010-0045-6
27. Gobbens RJ, Santiago LM, Uchmanowicz I, van der Ploeg T. Predicting disability using a nomogram of the Tilburg Frailty Indicator (TFI). Healthcare. 2023;11(8):1150. doi:10.3390/healthcare11081150
28. Liu C, Gao W, Meng W, et al. Can the Tilburg Frailty Indicator predict post-operative quality of recovery in patients with gynecologic cancer? A prospective cohort study. Int J Gynecol Cancer. 2023;33(5):761–769. doi:10.1136/ijgc-2022-003822
29. Lee J, Kim GS, Kim S, Al E. Use of the Tilburg frailty indicator in longitudinal studies with older adults: a scoping review. J Adv Nurs. 2023;79:2429–2443. doi:10.1111/jan.15675
30. G R, Marcel ALM, Luijkx KG, Schols JMGA. The predictive validity of the tilburg frailty indicator: disability, health care utilization, and quality of life in a population at risk. Gerontologist. 2012;52(5):619–631. doi:10.1093/geront/gnr135
31. Alqahtani BA, Nasser TA. Assessment of frailty in Saudi community-dwelling older adults: validation of measurements. Ann Saudi Med. 2019;39(3):197–204. doi:10.5144/0256-4947.2019.197
32. Fabrício-Wehbe SCC, Schiaveto FV, Vendrusculo TRP, Haas VJ, Dantas RAS, Rodrigues RAP. Cross-cultural adaptation and validity of the “Edmonton Frail Scale - EFS” in a Brazilian elderly sample. Rev Lat Am Enfermagem. 2009;17(6):1043–1049. doi:10.1590/S0104-11692009000600018
33. Alaei H, Vakhshoori M, Heidarpour M, et al. Translation, cultural adaptation, validation and reliability of Persian version of Edmonton frailty score questionnaire among Iranian heart failure individuals. Casp J Intern Med. 2023;14(1):53–59.
34. Rodrigues MK, Nunes Rodrigues I, Vasconcelos Gomes da Silva DJ, Pinto JM, Oliveira MF. Clinical Frailty Scale: translation and cultural adaptation into the Brazilian Portuguese language. J Frailty Aging. 2020;10(1):38–43.
35. Nissen SK, Fournaise A, Lauridsen JT, et al. Cross-sectoral inter-rater reliability of the clinical frailty scale – a Danish translation and validation study. BMC Geriatr. 2020;20(1):443. doi:10.1186/s12877-020-01850-y
36. Xiang W, Cheng Y, Li Z, Han J, Li K. Cross-cultural adaptation and validation of the Groningen Frailty Indicator in Chinese nursing home residents. Aging Clin Exp Res. 2020;32(6):1035–1042. doi:10.1007/s40520-019-01178-7
37. Tian X, Qiao X, Dong L, et al. Cross-cultural adaptation and psychometric properties of the Groningen Frailty Indicator (GFI) among Chinese community-dwelling older adults. Geriatr Nurs. 2020;41(3):236–241. doi:10.1016/j.gerinurse.2019.10.002
38. Okyar Baş A, Ceylan S, Güner M, et al. The validation of the Turkish version of the PRISMA-7 questionnaire; a case-finding instrument for detecting older adults living with frailty. Eur J Geriatr Gerontol. 2023;5(1):52–58. doi:10.4274/ejgg.galenos.2022.2022-8-2
39. Andreasen J, Sørensen EE, Gobbens RJ, Lund AM, Aadahl M. Danish version of the Tilburg Frailty Indicator: translation, cross-cultural adaption and validity pretest by cognitive interviewing. Arch Gerontol Geriatr. 2014;59(1):32–38. doi:10.1016/j.archger.2014.02.007
40. Topcu Y, Tufan F, Kılıç C. Turkish version of the Tilburg Frailty Indicator. Clin Interv Aging. 2019;14:615–620. doi:10.2147/CIA.S197512
41. Uchmanowicz I, Jankowska-Polańska B, Łoboz-Rudnicka M, Al E, Manulik S, Loboz-Grudzien K. Cross-cultural adaptation and reliability testing of the Tilburg frailty indicator for optimizing care of Polish patients with frailty syndrome. Clin Interv Aging. 2014;9:997–1001. doi:10.2147/CIA.S64853
42. Coelho T, Santos R, Paúl C, Gobbens FL, Fernandes L. Portuguese version of the Tilburg frailty indicator: transcultural adaptation and psychometric validation. Geriatr Gerontol Int. 2015;53(8):951–960. doi:10.1111/ggi.12373
43. Mulasso A, Roppolo M, Gobbens RE, Rabaglietti E. The Italian version of the Tilburg frailty indicator: analysis of psychometric properties. Res Aging. 2016;38(8):842–863. doi:10.1177/0164027515606192
44. Freitag S, Schmidt GR, Gobbens RJJ. Tilburg frailty indicator. German translation and psychometric testing. Z Gerontol Geriatr. 2016;49(2):86–93. doi:10.1007/s00391-015-0889-9
45. Mazoochi F, Gobbens RJJ, Lotfi M, Fadayevatan R. Diagnostic accuracy of the Tilburg Frailty Indicator (TFI) for early frailty detection in elderly people in Iran. Arch Gerontol Geriatr. 2020;91:104187. doi:10.1016/j.archger.2020.104187
46. Santiago LM, Luz LL, Mattos IE, Gobbens RJ, van AM. Psychometric properties of the Brazilian version of the Tilburg frailty indicator (TFI). Arch Gerontol Geriatr. 2013;57(1):39–45. doi:10.1016/j.archger.2013.03.001
47. Jemal K, Hailu D, Tesfa B, Lama T, Kinati T, Mengistu E. Geriatric depression and quality of life in North Shoa Zone, Oromia region: a community cross-sectional study. Ann Gen Psychiatry. 2021;20(1):1–10. doi:10.1186/s12991-021-00357-z
48. Federal Negarit Gazeta of the Federal Democratic Republic Of Ethiopia. A proclamation to provide for public servants’ pension: proclamation No. 714/2011; 2011.
49. HelpAge International. Vulnerability of Older People in Ethiopia: The Case of Oromia, Amhara and SNNP Regional States; 2013.
50. Nagaraj S. Effect of varying sample size in estimation of reliability coefficients of internal consistency. Webmedcentral Biostat. 2011;2(July):37.
51. World Health Organization. Process of Translation and Adaptation of Instruments; 2014.
52. Sousa VD, Rojjanasrirat W. Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: a clear and user-friendly guideline. J Eval Clin Pract. 2011;17(2):268–274. doi:10.1111/j.1365-2753.2010.01434.x
53. Brislin RW. Back-translation for cross cultural research. J Cross Cult Psychol. 1970;1:185–216. doi:10.1177/135910457000100301
54. Reba K, Birhane BW, Gutema H. Validity and reliability of the Amharic version of the world health organization’s quality of life questionnaire (whoqolbref) in patients with diagnosed type 2 diabetes in felege hiwot referral hospital, Ethiopia. J Diabetes Res. 2019;2019:1–7. doi:10.1155/2019/3513159
55. Patel N, Desai S. ABC of face validity for questionnaire. Int J Pharm Sci Rev Res. 2020;65(1):164–168. doi:10.47583/ijpsrr.2020.v65i01.025
56. Zamanzadeh V, Ghahramanian A, Rassouli M, Abbaszadeh A, Alavi-Majd H, Nikanfar A-R. Design and implementation content validity study: development of an instrument for measuring patient-centered communication. J Caring Sci. 2015;4(2):165–178. doi:10.15171/jcs.2015.017
57. Alderson J, Wall D. Instrument review: getting the most from a panel of experts. Applied Appl Nurs Res. 1992;5(4):194–197. doi:10.1016/S0897-1897(05)80008-4
58. Polit DF, Beck CT. The content validity index: are you sure you know what’s being reported? Critique and recommendations. Res Nurs Health. 2006;29(5):489–497. doi:10.1002/nur.20147
59. Pallant J. Survival manual: a step by step guide to data analysis using SPSS. Automotive Industries AI; 2011.
60. Mat Nawi FA, Abdul Malek A, Faizal Samat M, MasniezaMustapha W. A review on the internal consistency of a scale: the empirical example of the influence of human capital investment on malcom baldridge quality principles in tvet institutions. Asian People J. 2020;3(1):19–29. doi:10.37231/apj.2020.3.1.121
61. Taber KS. The use of cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48(6):1273–1296. doi:10.1007/s11165-016-9602-2
62. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc. 2012;60(8):1487–1492. doi:10.1111/j.1532-5415.2012.04054.x
63. Ofori-Asenso R, Chin KL, Mazidi M, et al. Global incidence of frailty and prefrailty among community-dwelling older adults. JAMA Netw Open. 2019;2(8):e198398.
64. Gobbens JJ, Petra B, Uchmanowicz I, Santiago LM. The Tilburg Frailty Indicator (TFI): new evidence for its validity. Clin Interv Aging. 2020;15:265–274. doi:10.2147/CIA.S243233
65. Grace Elderly Care International. Building hope, one elderly at a time; 2023. Available from: https://elderlygrace.org/about-us/.
66. Abdu AO, Yimamu ID, Kahsay AA. Predictors of malnutrition among older adults aged above 65 years in eastern Ethiopia: neglected public health concern. BMC Geriatr. 2020;20(1):1–11. doi:10.1186/s12877-020-01911-2
67. Mosadeghrad AM, Gebru AA, Sari AA, Tafesse TB. Impact of food insecurity and malnutrition on the burden of Non-communicable diseases and death in Ethiopia: a situational analysis. Hum Antibodies. 2019;27(4):213–220. doi:10.3233/HAB-190369
68. Renne I, Gobbens RJ. Effects of frailty and chronic diseases on quality of life in Dutch community-dwelling older adults: a cross-sectional study. Clin Interv Aging. 2018;13:325–334. doi:10.2147/CIA.S156116
69. Arslan M, Meltem Koç E, Sözmen MK. The Turkish adaptation of the Tilburg Frailty Indicator: a validity and reliability study. Turk Geriatr Derg. 2018;21(2):173–183. doi:10.31086/tjgeri.2018240418
70. Bolarinwa O. Principles and methods of validity and reliability testing of questionnaires used in social and health science researches. Niger Postgrad Med J. 2015;22(4):195–201. doi:10.4103/1117-1936.173959
71. Polit DF. Assessing measurement in health: beyond reliability and validity. Int J Nurs Stud. 2015;52(11):1746–1753. doi:10.1016/j.ijnurstu.2015.07.002
72. Theou O, Brothers TD, Mitnitski A, Rockwood K. Operationalization of frailty using eight commonly used scales and comparison of their ability to predict all-cause mortality. J Am Geriatr Soc. 2013;61(9):1537–1551. doi:10.1111/jgs.12420
73. Andreasen J, Lund H, Aadahl M, Gobbens RJJ, Sorensen EE. Content validation of the Tilburg Frailty Indicator from the perspective of frail elderly. A qualitative explorative study. Arch Gerontol Geriatr. 2015;61(3):392–399. doi:10.1016/j.archger.2015.08.017
74. Dong L, Liu N, Tian X, et al. Reliability and validity of the Tilburg Frailty Indicator (TFI) among Chinese community-dwelling older people. Arch Gerontol Geriatr. 2017;73:21–28. doi:10.1016/j.archger.2017.07.001
75. Uchmanowicz I, Pasieczna AH, Wójta-Kempa M, et al. Physical, psychological and social frailty are predictive of heart failure: a cross-sectional study. J Clin Med. 2022;11(3):565. doi:10.3390/jcm11030565
76. Ye L, Elstgeest LEM, Zhang X, Alhambra-Borrás T, Tan SS, Raat H. Factors associated with physical, psychological and social frailty among community-dwelling older persons in Europe: a cross-sectional study of Urban Health Centres Europe (UHCE). BMC Geriatr. 2021;21(1):422. doi:10.1186/s12877-021-02364-x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.