Back to Journals » Nature and Science of Sleep » Volume 10
Criteria for self-reported quantitative sleep characteristics of individuals who sought medical help for disturbed sleep – a survey of a representative sample of the Swedish population
Authors Miley-Åkerstedt A, Hetta J, Åkerstedt T
Received 9 February 2018
Accepted for publication 3 July 2018
Published 26 September 2018 Volume 2018:10 Pages 295—301
DOI https://doi.org/10.2147/NSS.S165158
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Steven A Shea
Anna Miley-Åkerstedt,1,2 Jerker Hetta,1 Torbjörn Åkerstedt1,3
1Department of Clinical Neuroscience, Karolinska Institute, Stockholm, Sweden; 2Psychology Clinic, Karolinska Hospital, Stockholm, Sweden; 3Stress Research Institute, Stockholm University, Stockholm, Sweden
Background: The public often seeks rule-of-thumb criteria for good or poor sleep, with a particular emphasis on sleep duration, sleep latency, and the number of awakenings each night. However, very few criteria are available.
Aim: The present study sought to identify such criteria.
Methods: Whether or not a person has sought medical help for sleep problems was selected as an indicator of poor sleep. The group that was studied constituted a representative sample of the general Swedish population (N=1,128), with a response rate of 72.8%.
Results: Logistic regression analysis, with an adjustment for age and gender, showed an increased OR for a weekday sleep duration of ≤6 hour, (OR >2, and for <5 hour: OR >6). For weekend sleep, the value was ≤6 hour (OR >2). For awakenings per night, the critical value was ≥2 (OR >2, and for ≥5 awakenings: OR >9), and for a sleep latency the critical value was ≥30 minutes (OR >2, and for ≥45 minutes: OR >6). Adding difficulties falling asleep and early morning awakening (considered qualitative because of the reflected “difficulty”), led to the elimination of all the quantitative variables, except for the number of awakenings. The addition of “negative effects on daytime functioning” and “sleep being a big problem” resulted in the elimination of all the other predictors except age.
Conclusion: It was concluded that weekday sleep ≤6 hour, ≥2 awakenings/night, and a sleep latency of ≥30 minutes, can function as criteria for poor sleep, but that qualitative sleep variables take over the role of quantitative ones, probably because they represent the integration of quantitative indicators of sleep.
Keywords: sleep duration, sleep latency, awakenings, sleep quality
Introduction
Many individuals take a keen interest in their sleep and want to know what constitutes good sleep, and whether they sleep well enough. Usually, the interest is focused on relatively “objective” sleep variables, or at least variables that may be quantified and used for the rule-of-thumb self-determination of sleep sufficiency. The key variables tend to be sleep duration, sleep latency, and number of awakenings. Here, we will refer to these variables as “quantitative” in contrast to variables reporting sleeping difficulties, which will be referred to as “qualitative” (even if they may be quantitative in their frequency across a week). At present, we know very little about the critical levels of these variables and no such information is found among the clinical criteria for insomnia.1 Moreover, there seems to be very few relevant studies that have been conducted on this topic. However, in one such study of university students, it was found that quantitative indicators like sleep duration, sleep latency, and the number of awakenings predicted global sleep quality.2 In another small study of insomniacs, sleep duration and the number of awakenings predicted global sleep quality in women, and sleep efficiency did so in males.3
None of the 2 studies aforementioned tried to establish the criteria for good sleep, but rather tried to identify important predictors using multivariate approaches. They also targeted specific subgroups rather than the general population. Therefore, there seems to be a need for a study of a sample more representative of the general population. A sharper criterion against which predictors could be evaluated could be whether or not an individual has sought medical help for sleeping difficulties. Seeking such help suggests a high level of dissatisfaction with sleep, and a behavioral effort to mitigate it. Seeking medical help also has implications for health economics. In one such recent study, the criterion used was whether the respondent thought that they needed treatment for sleep difficulties.4 The results showed that difficulties initiating sleep was a strong predictor, difficulties maintaining sleep was a moderate predictor, but early morning awakenings was not a significant predictor. Sleep duration, sleep latency, or the number of awakenings was not studied.
Some indication of the criteria could be gained from consensus statements like the one on sleep latency, which suggested that self-reported sleep latency >30 minutes may be clinically relevant.5,6 For sleep duration, the Pittsburgh Sleep Quality Scale used <7 hour of self-reported sleep as a criterion of modestly reduced sleep quality, while durations <5 hour represent more severe reduction.7 For number of awakenings, there seems to be no suggested criteria. It is also likely that criteria may vary depending on age and gender.8
The purpose of the present study was to investigate, in a representative sample, at what levels of the subjective quantitative sleep indicators medical help for disturbed sleep had been sought. In particular, the focus was on sleep duration (weekday and weekend), the number of awakenings per night, and sleep latency, as well as on their relative contribution toward having sought medical help. We also investigated whether qualitative ratings of sleep (frequency of difficulties initiating sleep or of early awakening) would be more closely associated with having sought medical help, and if the perceived daytime consequences of sleep problems, or the global rating of sleep as a problem in life, would be associated with seeking medical help for sleep difficulties. The study was part of a larger study of insomnia organized by the Swedish Council on Health Technology Assessment (SBU) and carried out by Statistics Sweden. Other publications from this database have focused on the prevalence of insomnia in Sweden.9
Methods
Design and participants
The survey was carried out by Statistics Sweden. A representative sample of 1,556 individuals in an age range of 18–84 years was contacted. It was proportionally stratified for age and sex. The procedure involved a computer-assisted phone survey. Each interview started with information about the purpose of the study, followed by verbal consent to the interview. Thereafter, the interview proceeded with the main questions. A total of 1,128 individuals completed the survey (72.8%).
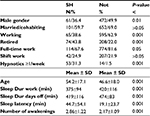
The group having sought help was more frequently: women, not working, retired, having part-time work (Table 1). They were also older, had shorter sleep duration during workdays and days off as well as longer sleep latency, and more awakenings per night. See Mallon et al for more details.9 The study was approved by The Regional Ethical committee of Stockholm, Sweden (#2014/256-31/5).
Measures
The interview contained 39 questions that included demographics, work conditions, sleep complaints, daytime impairment due to sleep, sleep duration, diseases, and visits to a physician for sleep problems. The main outcome variable “sought help” (SH) was formulated as: “Have you seen an MD for sleep problems”?
Sleep duration was obtained via the question “how many hours do you normally sleep?”, separately for weeknights and days off/weekends. The answer was expressed as a continuous variable. In addition, the participants were asked about the number of awakenings per night (1= never, 2= once, 3= twice, 4=3–4 times, 5= at least 5 times), and the time it usually takes to fall asleep (h:min). All of the sleep questions referred to what occurred over the last month.
The subjective sleep quality ratings were the following: “How often do you experience”: “difficulties falling asleep” (1= never, 2= <once a week, 3=1–2 times per week, 4=3–5 times per week, 5= daily or almost daily), “…early morning awakenings” (same response alternatives). Daytime consequences were assessed by the question: “Have your sleep complaints interfered with your daily life during the last month?” (1= no interference; 2= minor interference; 3= moderate interference; 4= severe interference; and 5= very severe interference). One question on the severity of sleep problems was phrased: “To what extent do sleep difficulties constitute a problem in life (scale 1–5; not at all, to very much). Most variables were used in a paper on the prevalence of insomnia in Sweden.9
Use of prescription sleep medication was ascertained by the question “How often during the last month have you used prescription sleep medication?” (1= never or l< once per month, 2= <once per week, 3=1–2 times per week, 4=3–5 times per week, and 5= daily or almost daily).
Statistics
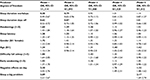
Logistic regression was used to relate categories of sleep duration, awakenings, and sleep latency to “sought help” (coded 0/1 for no/yes), separate for each predictor, and with an adjustment for age and gender. The results are shown in Figure 1. In addition, 5 multiple logistic models were evaluated. Model 1: (one variable at a time [unadjusted]): Sleep duration weekend and weekday, sleep latency, and the number of awakenings, age, sleep quality, early morning awakening, and negative effects on daytime functioning. Model 2: background and quantitative ratings (mutually adjusted). Model 3: all predictors except “negative effects on daytime functioning” and “sleep is a big problem” (mutually adjusted). Model 4: all predictors except “sleep is a big problem” (mutually adjusted). Model 5: all predictors (mutually adjusted). Reference = not sought help (0).
The categories for total sleep time (TST) during days off was <6 hour (N=161), 6–6.9 hour (N=233), 7–7.9 hour (355), 8–8.9 hour (N=240), and ≥9 hour (N=125). For TST during the working week, the categories were <5 hour (N=110), 5–5.9 hour (189), 6–6.9 hour (417), 7–7.9 hour (N=304), and ≥8 hour (N=95). The categories for sleep latency were 0–5 minutes (N=364), 5–10 minutes (N=210), 10–29 minutes (N=212), 30–45 minutes (N=188), and ≥46 minutes (N=141). For the number of awakenings, the categories were ≥5 times per night (N=40), 3–4 times per night (N=134), 2 times per night (N=391), 1 time per night (N=371), and 0 times (N=335). Age and gender were entered as covariates.
The number of participants was not sufficient for stratifying for age and gender in the logistic regression analyses. Instead, we computed an ANOVA with help-seeking behavior, age, and gender as factors as well as sleep duration, sleep latency, and the number of awakenings as dependent variables.
Results
The mean ± SD for the key variables were as follows: sleep duration weekday =414±21.1 minutes, sleep duration days off =466±91 minutes, sleep latency =23.0±31.8, number of awakenings =2.28±1.14. The correlation between the 2 sleep duration variables was r=0.55 (P<.001). The number of individuals in total and of those who had sought help in the different categories of sleep duration on weekdays was as follows:<5 hour =110/47, 5–5.9 hour =189/36, 6–6.9 hour =417/46, 7–7.9 hour =303/29, and ≥8 hour =95/11. For weekends/days off, the corresponding values were: 5–5.9 hour =161/63, 6–6.9 hour =233/30, 7–7.9 hour =355/38, 8–8.9 hour =240/24, and ≥9 hour =125/14.
The logistic regression of sleep duration, sleep latency, and number of awakenings vs having sought medical help showed significant ORs for sleep duration ≤6 hour and particularly for <5 hour for workdays, and for ≤6 hour for days off (see Figure 1 and Table 2 – model 1). For awakenings, the OR was significantly increased for ≥2 awakenings, with a peak at ≥5 awakenings. For sleep latency, ≥30 minutes was significant. In addition, age and gender had significant ORs. Older age and being female were associated with having sought help for poor sleep. The qualitative variables were all significant in this model.
In model 2, sleep duration, sleep latency, and the number of awakenings, age, and gender were entered together and all showed significant ORs. In Model 3, the qualitative variables “difficulties falling asleep” (1-5) and “premature awakening” were entered and they showed significant ORs, but only the number of awakenings remained significant among the quantitative sleep variables. In Model 4, the negative effects on daytime functioning was added and showed a significant OR, while only age remained significant among the other variables. Older individuals more frequently sought medical help for sleeping difficulties. In Model 5, the global estimate of sleep (“is sleep a problem in life”) was entered and showed a significant OR, resulting in a reduction of the OR for negative daytime effects and a remaining effect of age.
To analyze the contribution of age and gender, an ANOVA was applied with “sought help” (yes/no), age (<47 vs ≥47 years) and gender as factors, and with the quantitative variables as dependent variables. The only significant interaction was that for sleep latency, such that women showed longer sleep latency for the group seeking medical help (see Table 3). No other interactions became significant. Seeking medical help for sleep problems was highly significant for all variables. Gender was significant for sleep latency (longer for women), and age was significant for TST on days off (lower for older participants) and for the number of awakenings (higher for older participants).
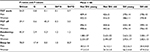  | Table 3 Results from ANOVA with SH (or not), G and A as factors Notes: aP<.05, bP<.01, CP<.001. Abbreviation: A, age; G, gender; SH, sought help, TST, total sleep time. |
In considering the possibility that not all individuals with short sleep perceived this as a problem, we computed the percentage of individuals in that group that had no complaints. This showed that 23 individuals (20.9%) reported never getting too little sleep, and 19 (17.3%) saw no problems at all with their sleep. The corresponding figures for those who reported a sleep latency of >30 minutes was 80 (49.1%), and it was 63/38.7% for their sleep not being a problem at all. For >2 awakenings per night, the corresponding values were 84/62.7% for never too little sleep, and 42/43.6% for their sleep not being a problem at all.
Discussion
The results show that the OR for seeking medical help for sleeping difficulties became significant at 6 hours of sleep during days of work. For days off <6 hour was significant. Sleep latency ≥30 minutes, and >2 awakenings were significantly associated with seeking medical help for sleeping difficulties. The quantitative measures lost their significant prediction when qualitative sleep measures were entered, and the single item “sleep as a big problem in life” became the only significant predictor when entered, except for negative effects on daytime functioning and age.
The >6-fold increase in risk at 5–6 hour of sleep during weekdays, and particularly at <5 hour, suggests the importance of sleep duration for having made the decision to seek medical help. No similar results (predicting seeking medical help for poor sleep) seem to be available in the literature, but sleep duration has been a predictor of reported sleep quality, even if no criteria were identified.2,3 The findings are also in line with the <5 hour criterion of too short sleep duration in the Pittsburgh sleep quality index.7 One may also compare the present findings with those of studies of sleep duration and mortality, in which ≤6 hour are related to increased mortality.10 Weekend sleep showed similar but weaker associations with seeking medical help, which seems logical since it only constitutes 2/7 of the days of the week. Interestingly, in insomniacs, short (objective) sleep of ≤5 hour has been linked to more autonomic arousal and severe health problems than in insomniacs with normal sleep duration.11
Even if ≤5 hour of sleep should be taken as an indication of sleep problems, it is also obvious that a majority of this group had not sought medical help, and that ~20% saw their sleep duration as sufficient, and did not see any problem at all with their sleep. Presumably, this group is made up of “efficient” sleepers. This should be an interesting question for a polysomnographic approach. Sleep duration during days off did not reach significance in the adjusted models, in contrast to weekday sleep duration. This suggests that the latter is more important for seeking medical attention, probably because it represents 5/7 of the days of the week, and because work is likely to curtail sleep for most individuals.
A sleep latency exceeding 30 minutes as a characteristic of those seeking medical attention seems to be well in line with the research criteria for insomnia.12 A criterion for the number of awakenings and seeking medical attention does not seem to exist, but the number of awakenings has been related to self-reported sleep quality.2,3 In the present case, seeking medical attention was increased already at 2 awakenings per night, and at ≥5 awakenings per night, there was a 9-fold increase in the OR for seeking medical help for sleep difficulties.
When the quantitative variables were adjusted for (together with age and gender) in model 2 in the regression analysis, all of them remained significant, except for weekend sleep duration. The latter suggests a lower importance for this variable with respect to seeking help, but it appears that weekday sleep duration, the number of awakenings, and sleep latency contributed independently to explaining help-seeking behavior.
Sleep duration and sleep latency were no longer significant predictors in model 3 when the qualitative variables “difficulties falling asleep” and “early morning awakening” were entered. This suggests that variables explicitly involving sleep difficulties are stronger predictors of seeking help than the quantitative variables, except for the number of awakenings. This became even more evident when problems with daytime functioning was entered, and particularly when the global evaluation of sleep as a big problem was entered.
The importance of the qualitative variables does not necessarily mean that quantitative sleep is unimportant. Rather, the qualitative variables probably constitute an integration of all the aspects of sleep, and may be the decisive component for seeking medical attention. This is also reflected in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for insomnia,1 which do not include the quantities of sleep duration, sleep latency, or number of awakenings. It is also reflected in popular clinical self-rating scales for sleep, eg, the widely used Insomnia Severity Index.13 Furthermore, the study focusing on the need for treatment for disturbed sleep showed essentially the same sleep quality variables as predictors.4 Quantitative sleep variables were not included in that study. Still, quantitative variables remain of great interest for the public when searching for easily understood rule-of-thumb advice.
The more frequent help seeking among women and older individuals agrees with previous research,8 but it is noteworthy that gender became excluded as a predictor in the present study when all of the quantitative variables were added in model 2. Age retained its predicted value throughout the analysis and constitutes a stable predictor of having sought medical help. The quantitative criteria may need to be modified for age.
It should be emphasized that one limitation of the present study is that the results concern individuals who have sought medical attention, regardless of when. The results do not predict who will seek medical attention. Another limitation is that the quantitative sleep variables were confined to experiences within the last month, whereas the question of seeking medical attention for sleep problems concerned any point in one’s life. As such, it is impossible to know exactly what types of sleep problems led to these individuals seeking medical attention. Nevertheless, this study provides a good first insight into the importance of considering quantitative data when trying to understand subjective definitions of good vs bad sleep.
Conclusion
The present study has shown that having sought help for poor sleep is associated with ≤6 hour of sleep (during weekdays), longer sleep latency than 30 minutes, and at least 2 awakenings per night. We believe these findings may be useful when communicating with the public about what may be deemed adequate sleep. However, the results also indicate that more qualitative perceptions of one’s sleep are important for seeking help. Therefore, quantitative measures should be used with caution and the public should be advised to be more observant on more qualitative perceptions of sleep, in particular on the negative daytime consequences of poor sleep. Such criteria are included among the diagnostic criteria of insomnia as described in DSM-5.1
Acknowledgments
This study was supported by the Swedish Agency for Health Technology Assessment (SBU), Stockholm Stress Center, and the Swedish Research Council for Health, Working Life, and Welfare (Forte).
Disclosure
The authors report no conflicts of interest in this work.
References
American Psychiatric Association. DSM-5 Task Force. Diagnostic and Statistical Manual of Mental Disorders : DSM-5. 5th ed. Washington, DC: American Psychiatric Association; 2013. | ||
Tsai LL, Li SP, Sp L. Sleep patterns in college students: gender and grade differences. J Psychosom Res. 2004;56(2):231–237. | ||
Woosley JA, Lichstein KL, Taylor DJ, Riedel BW, Bush AJ. Predictors of perceived sleep quality among men and women with insomnia. Behav Sleep Med. 2012;10(3):191–201. | ||
Sandlund C, Westman J, Hetta J. Factors associated with self-reported need for treatment of sleeping difficulties: a survey of the general Swedish population. Sleep Med. 2016;22:65–74. | ||
Edinger JD, Bonnet MH, Bootzin RR, et al. Derivation of Research Diagnostic Criteria for Insomnia: Report of an American Academy of Sleep Medicine Work Group. Sleep. 2004;27(8):1567–1596. | ||
Lineberger MD, Carney CE, Edinger JD, Means MK. Defining insomnia: quantitative criteria for insomnia severity and frequency. Sleep. 2006;29(4):479–485. | ||
Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. | ||
Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. | ||
Mallon L, Broman JE, Akerstedt T, Hetta J. Insomnia in sweden: a population-based survey. Sleep Disord. 2014;2014:843126. | ||
Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Sleep duration and all-cause mortality: a systematic review and meta-analysis of prospective studies. Sleep. 2010;33(5):585–592. | ||
Vgontzas AN, Fernandez-Mendoza J. Insomnia with Short Sleep Duration: Nosological, Diagnostic, and Treatment Implications. Sleep Med Clin. 2013;8(3):309–322. | ||
Buysse DJ, Ancoli-Israel S, Edinger JD, Lichstein KL, Morin CM. Recommendations for a standard research assessment of insomnia. Sleep. 2006;29(9):1155–1173. | ||
Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–608. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.