Back to Journals » Patient Preference and Adherence » Volume 12
Creating a change in the use of ventrogluteal site for intramuscular injection
Received 28 March 2018
Accepted for publication 28 June 2018
Published 13 September 2018 Volume 2018:12 Pages 1749—1756
DOI https://doi.org/10.2147/PPA.S168885
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Johnny Chen
Gülşah Gürol Arslan,1 Dilek Özden2
1Nursing Faculty, Dokuz Eylül University, Balçovaİzmir, Turkey; 2Nursing Faculty, Dokuz Eylül University, Balçovaİzmir, Turkey
Purpose: This study was conducted to determine the impact of education on the knowledge, opinions and anxiety level of the nurses regarding the use of the ventrogluteal site for intramuscular injection.
Subjects and methods: The research was conducted with a single group using a semi-empirical pre-test, post-test design. The sample consisted of 50 nurses who worked in clinics where intramuscular injection was frequently applied and who participated in training on the use of ventrogluteal site for intramuscular injection. The data were collected by the researchers with the questionnaire form for evaluation of data, in addition to using descriptive statistical methods, paired sample t-test, Kruskal–Wallis and 2-related samples tests.
Results: It was found that 34.0% of the nurses frequently used the dorsogluteal site for intramuscular injection. It was determined that the difference between pre-training (12.40±6.89) and post-training (21.80±1.95) mean scores of the nurses regarding the ventrogluteal site injection was statistically significant (P<0.00). However, no statistically significant difference (P>0.05) was found between the pre-training (39.22±10.16) and post-training (37.52±8.54) anxiety levels.
Conclusion: It can be stated that the majority of the nurses did not prefer the ventrogluteal site for intramuscular injection; the reasons for not preferring this method were a lack of knowledge on determining the site and concern about harming the patients.
Keywords: ventrogluteal site, dorsogluteal site, intramuscular injection, nursing
Introduction
Worldwide, 12 billion treatments are made by injection every year. Of these, 5% or less are vaccinations and >95% are injections made for therapeutic purposes.1 It is of major importance that intramuscular injections (IMIs) are administered with the right technique. In the right technique, it becomes crucial to identify the IMI site accurately.2 When the proper technique is not used for IMI and the injection site is not accurately identified, sterile abseil, infection, tissue irritation, periostitis, muscle fibrosis and contracture, necrosis and gangrene, intramuscular hemorrhage and pain may occur.3–5
Although the literature indicates that all injection sites for IMI can be used in adults according to the condition of the patient, the results of evidence-based studies in recent years indicate that the area of ventrogluteal (VG) injection site is the safest injection site.6–9 The thickness of the subcutaneous tissue in this site is lower than those of the other injection sites,10,11 the nerves and veins are relatively few in number, while the muscles in the site are large and well established. It is much easier to find the limit points for application. In the literature, it is stated that the muscles in the VG site are well developed, and that it is a suitable site for especially intense and irritating drugs.12,13
Many studies have revealed the reasons why the VG site is not preferred for IMI practices. Wynaden et al6 and Engstrom et al14 reported that nurses did not routinely use this site as they believed that the VG site was not as safe as the dorsogluteal (DG) site. The anatomically small structure of the VG site, the difficulty of determining the site, and the concern that the patient may be harmed cause nurses to avoid using this site.12,14 In case of overweight patients, nurses’ level of anxiety increases.6,14,15 Similarly, in their study which analyzed the knowledge, views and practices of nurses regarding VG site injection, Tuğrul and Denat2 found that 38.8% of the nurses never used the VG site. The reason for this was that most of the nurses (72.9%) had no adequate knowledge of the VG site, and almost half of the nurses (44.7%) were worried for they had never used this site. Greenway et al15 reported that nurses did not know how to administer an injection to the VG site, and also that they thought they would harm this tissue and were reluctant to use the site.
According to the results of the study conducted by Güneş et al,17 78.2% of the nurses had never used the VG site. In the study of Gülnar and Çalişkan,18 it was found that 85.9% of the nurses most frequently used the DG site while 63.3% never used the VG site. Although there is a great quantity of information to support the use of VG site, the promotion of its use in clinical settings is relatively slow.13 Many nurses have been informed about the VG site, but are reluctant to use it.13 It is seen that the reasons for this reluctance include the difficulty and concern about determining the site. It is thought that this condition might be related to the failure in transferring the research results to clinical settings. There are a very limited number of studies analyzing the reflections of recent developments in IMIs on the application practices and the knowledge, opinions and practices of nurses regarding VG injection site, and evaluating the effectiveness of the related trainings. This study was planned with the purpose of determining the impact of education on the knowledge, opinions and practices of the nurses regarding the use of the VG site for IMI.
Subjects and methods
Type of research
The research was carried out in a semi-experimental (pre-test–post-test) pattern using the training program.
The population and sample of the research
The population of the research was composed of 120 nurses working in a private hospital in Turkey. In the study, nurses working in the operating room (n=25), outpatient clinics (n=15) and clinics without IMI practice (n=30) were excluded from the sample. The sample of the research consisted of 50 nurses.
Data collection tools
The data collection form was prepared by the researchers using the literature.2,18 The form consists of four parts.
In the first part, there are nine questions on the nurses’ descriptive characteristics (age, gender, education, length of employment) and their IMI practices. In the second part, there are five questions on the nurses’ use of the VG site for IMI.
In the third part, there are a total of 28 questions investigating their knowledge of the VG site for IMI (VG region includes gluteus medius and gluteus minimus muscles, it is safe for injection, large volume muscles such as the VG region can take up to 3 mL of medication, in order to detect the VG region, etc.). Of these statements, 14 were prepared as correct and 14 as incorrect, and the nurses were asked to respond to these statements with the options “true”, “false” or “do not know”. From a total of 28 points, the correct replies received 1 point each while the incorrect and “do not know” replies received 0 points. According to these results, the mean knowledge scores of the nurses were calculated. For the validity of the scope of the questions prepared, expert opinions were obtained from four faculty members. Necessary changes were made in the data collection form in accordance with the opinions of the experts.
In the fourth part, the “state–trait anxiety inventory” developed by Spielberger et al (1970) was used. It was adapted to Turkish by Öner and Le Compte in 1977. The state–trait anxiety inventory describes how individuals feel at a particular moment in time under certain conditions.19 There is no time limit for the response process. The emotions or behaviors expressed in the state anxiety inventory items are rated according to the intensity of the experience as 1) not at all, 2) somewhat, 3) moderately so and 4) very much so. The inventory includes direct- and reverse-worded items. Direct-worded items express negative emotions, while reverse-worded items express positive emotions. A score of 4 points in direct-worded items and a score of 1 point in reverse-worded items indicate a high level of anxiety.20
Implementation of the research
Pre-tests (data collection form, state–trait anxiety inventory) were conducted with the nurses who completed the informed consent form between 25 April and 6 May 2016. According to the pre-test results, the nurses participated in the training planned by the researchers on 17–18 May 2016. Due to the number of nurses, trainings were conducted in four sessions (2 hours of theory, 2 hours of laboratory work on a model). After the training was completed, the post-tests (data collection form, state–trait anxiety inventory) were conducted. Following the training, the nurses were given “Standard Practice Guidelines for Ventrogluteal Site Injection” developed by the researchers to help them remember the training in clinical settings. One week after the completion of the training sessions, nurses were given the post-test (data collection form, state-trait anxiety inventory) and they were asked to answer.
Data analysis
Statistical analysis was performed using the IBM Statistical Package for Social Sciences v22 software (IBM Corp., Armonk, NY, USA). Descriptive statistics were presented as the mean and SD. Percentage was used to evaluate the descriptive characteristics of the nurses, while the chi-squared significance test was used to compare the characteristics of the individuals. Student’s t-test, Kruskal–Wallis and 2-related samples test were performed in order to compare pre-test and post-test scores of the groups. A P-value of <0.05 was considered statistically significant.
Ethical considerations
Researchers obtained permission from the hospital where the study was conducted. Before the collection of data for the study, consent was obtained from the non-interventional research ethics committee of Dokuz Eylül University (reference number: 2713-GOA, 2016/14–09). The study was conducted in accordance with the Declaration of Helsinki Principles. All the nurses were given information about the study and its aims, and were told that the participation was voluntary with no negative repercussions for nonparticipation. Contact information was provided along with the questionnaire. The nurses’ oral and written informed consents were obtained.
Results
The descriptive characteristics of the nurses participating in the study are given in Table 1. The mean age of the nurses was 25.80±5.02, 92.0% were female and 56.0% were graduates of the Vocational School of Health. The average number of years in clinical practice was 3.25±3.05. A great majority of the nurses (84.0%) stated that they did not receive IMI-related training on VG site IMI.
  | Table 1 Descriptive characteristics of the nurses (N=50) |
It was found that 34.0% of the nurses frequently administered IMI, more than half (56.0%) always used the DG site and the majority of the nurses (74.0%) never preferred the VG site (Table 2).
  | Table 2 Sites used for IMI by nurse and their frequency of use |
It is observed in Table 3 that before training, most of the nurses (64%) expressed that the DG site was the safest site for injection. Few of the nurses (18.0%) stated that the VG site was a safe site for IMI. When the reasons why the nurses did not prefer the VG site were examined, it was seen that the nurses expressed that they did not know how to identify the site (32.0%) and there was a high probability of reaching the bone tissue (26.0%). It was determined that a great majority of the nurses (80.0%) did not know that the use of VG site for IMI was recommended in the literature.
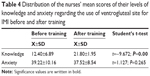
Table 4 shows that while the mean knowledge score of the nurses regarding the VG site use for IMI was 12.40±6.89 before training, it increased to 21.80±1.95 after training and the difference was statistically significant (P<0.05). It was determined that the nurses’ level of anxiety was above average before training (39.22±10.16) and it decreased after training (37.52±8.54) and the difference was not statistically significant (P>0.05).
The distribution of the mean knowledge scores regarding the VG site IMI according to certain characteristics of the nurses is shown in Table 5. There was no difference in the mean knowledge scores according to age, gender, educational status, years of study in nursing and IMI-related training status before and after training (P>0.05). The table shows that both the 18–27 age group (before training: 12.94+6.37, after training: 21.97+2.03) and the 28–37 age group (before training: 11.25+8.00, after training: 21.43+1.73) showed an increase in the information point average after training and this difference was statistically significant (P<0.05). Similarly, when considering the level of education, years of study in nursing, IMI-related training, identification of VG site, knowledge of the recommendation of the VG site in the literature and safe choices for IMI, it was found that the post-training mean knowledge scores in the intra-group evaluations increased compared to the previous one and this difference was statistically significant (P<0.05). When the gender variables were examined, it was found that the difference in mean knowledge scores was statistically significant for female nurses (before training: 12.52+6.78, after training: 21.91+1.94; P<0.05).
Discussion
The aim of the study was to assess whether the nurses’ level of knowledge regarding the use of the VG site for IMI would change after the training.
In this study, 34.0% of the nurses frequently used IMI and more than half (56.0%) of them always used the DG site. It was also found that a vast majority of the nurses (74.0%) never preferred the VG site. In literature, it is reported that the majority of nurses preferred using the DG site, which was also supported by other researchers.2,21–25 It is stated that nurses’ reluctance to use the VG site is caused by lack of confidence about the implementation of the procedure,26 lack of knowledge on safe gluteal IMI sites and its logic27 and traditional approaches.2,24 Prior to the training, it was seen that most of the nurses (64%) identified the DG site as the safest site for injection. A small number of nurses (18.0%) stated that the VG site was a safe site for IMI. In their study, Freitag et al23 also determined that nurses were not informed about the significance of the VG site. Surprisingly, in the study of Tuğrul and Denat,2 nurses stated that they most frequently used the DG site while they identified the VG as the safest site. For the past 20 years, the VG site has been considered to be a safer and more suitable injection site than the DG site.21
When the reasons why the nurses did not prefer the VG site before the training were examined, it was seen that 32% of the nurses did not know how to identify the site. Wynaden et al,6 Tuğrul and Denat2 and Freitag et al23 found that nurses had difficulty in identifying the VG site anatomically. If the medication given using IMI does not reach the correct site and absorption of medication is incomplete, the serum level of the medication may impact negatively on the patient’s health outcomes.28
In the study, the reasons why nurses did not use the VG site for IMI were examined. One of the reasons is the belief that the risk of reaching the bone tissue of the needle is high (26.0%). However, in the literature,29 it is stated that the VG site is distant from the bone tissue. Masuda et al30 reported that the injection needle to be used for people with standard body shape would not contact the iliac bone as long as it is <~45 mm. In Turkey, the needles used for IMI are 2.5–4 cm long and 21 G.
Another reason is the possibility of the patient rejecting the operation because of not being familiar with the site (24.0%). The study of Tuğrul and Denat2 reveals a similar result. Wynaden et al6 reported that site selection for IMIs was predominantly made by patients, and that the acuity of the patient was supported by the nurse. Of the nurses, 16% reported that they did not prefer the VG site as it would cause too much pain. The results of the study conducted by Tuğrul and Denat2 are also parallel. However, Güneş et al29 and Moharreri et al31 found that patients felt less pain with VG site injection when compared to the DG site injection. Coskun et al24 stated that less pain is experienced in the VG site since there are no major neurovascular structures in the site. Furthermore, the thickness of the subcutaneous (SC) in the site is small, which is another reason why less pain is experienced.10,24
It is known that muscle thickness in the injection site is significant for drug emulsion.29,30 In the study, although it is a small number, 6% of the nurses identified the small muscle size of the VG site as another reason for not using the site. In the literature, there is information on the large structure of the muscle layer in the VG site.18,30 On the other hand, Yalcin et al21 and Coskun et al24 found that there was no statistically significant difference between the muscle thickness of VG and DG sites. Furthermore, Kaya et al10 and Elgellaie et al11 reported that the muscle tissue in the VG site was thicker.
It is reported that the reasons for the common use of the DG site include its easy accessibility, the belief that it has larger muscle structure and that it would cause less pain and the influence of patients’ preferences.28
On the other hand, it was determined that a great majority of the nurses (80.0%) were not informed about the fact that the VG site use was recommended for IMI in the literature. It is stated in the literature32 that VG has been identified as a safe site for IMI since the 1960s. The use of VG site for IMIs was proposed for the first time by the Swiss anatomist against the reported problems about the DG site.32 Given the results of all studies, IMI emerges as a practice where the teachings of senior colleagues are traditionally taken into consideration and where the guidelines revealing the best clinical evidence are not used.
In our study, it was found that the mean knowledge score of the nurses about the use of VG site for IMI increased significantly after training (P<0.05). Şanlialp and Kurban33 and Altun et al34 also found that the number of correct answers of nurses increased after the IMI training. Hdaib et al35 reported that the nursing students’ level of knowledge increased after the IMI training. In their study, Gülnar and Özveren25 found that the nurses’ knowledge scores increased, and that the follow-up after 4 months revealed that the nurses started to frequently use the VG site in clinics. In the study, it was also found that, prior to the training, the anxiety levels of the nurses were higher than the average (39.22±10.16) and that their anxiety levels decreased (37.52±8.54) after the training (P>0.05). In their study conducted to create a change in the nurses’ injection technique, Wynaden et al28 reported that only 51% of the nurses used the technique despite a statistically significant change. Cocoman and Murray4 reported that it was a difficult task to change the working habits and routines of experienced professionals. In accordance with these results, it was revealed that nurses were reluctant to change and that change in practice at a clinical level was a slow process.6,15,16,28,29,36
When the mean knowledge scores of the nurses according to their year of study in nursing were examined, it was determined that the mean knowledge scores increased significantly according to the pre-training (P<0.05). Prior to the training, the mean knowledge scores of the nurses who did not have knowledge of VG site identification were relatively lower (6.87±7.08) with a statistically significant difference (P<0.05); however, it was determined that the mean knowledge scores of the nurses in this group were increased and meaningful after the training (P<0.05). When examined according to their IMI-related training status, it was seen that the mean knowledge score of the nurses increased after the training (P<0.05). Similarly, it was found that the mean knowledge score of the nurses who were not informed about the recommendation of the use of VG site in the literature9,18,37 was lower than that of the nurses who were informed before the training and the difference was statistically significant (P<0.05); it was determined that the mean knowledge scores of this group of nurses increased significantly after the education (P<0.05). In the study of Şanlialp and Kurban,33 similar findings were observed.
In the study, it was found that the mean knowledge score of the nurses who found the VG site for IMI to be safe was higher than those of the other groups at a statistically significant level (P<0.05). It was determined that the mean knowledge score of the nurses increased after the training (P<0.05).
Conclusion
Although participating in a training on the use of VG site for IMI is effective in raising the level of knowledge, its impact on creating a behavioral change is limited. For this reason, while conducting training programs on the use of VG site for IMI, it is necessary to plan more than one training session and demonstration practices. For planning a change in clinical setting, the individual and interpersonal characteristics of the participants should also be taken into consideration.
While developing the best techniques for practice, it is of equal importance to both review the scientific literature in the field and evaluate the current practice. When the best guidelines for practice are developed, it is necessary to consider the theoretical and clinical aspects of the new guidelines. Ongoing training is essential to ensure that the guidelines developed are followed by staff and that the practice is maintained over time.
Acknowledgments
We would like to thank the hospital authorities for granting approval for this study and the participants who provided full support in carrying out this study.
Author contributions
All authors (GGA, DÖ) contributed equally to this work in the concept, design, analyses, interpretation of data, drafting of manuscript or revising it critically for important intellectual content. All authors agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
Chung JW, Ng WM, Wong TK. An experimental study on the use of manual pressure to reduce pain in intramuscular injections. J Clin Nurs. 2002;11(4):457–461. | ||
Tuğrul E, Denat Y. Hemşirelerin ventrogluteal Alana enjeksiyon uygulamaya ilişkin bilgi, görüş ve uygulamalari [Nurses’ knowledge, opinion and practices regarding to injection practices in ventrogluteal site]. Dokuz Eylül University Nursing Faculty Electronic Journal. 2014;7(4):275–284. | ||
Chan VO, Colville J, Persaud T, Buckley O, Hamilton S, Torreggiani WC. Intramuscular injections into the buttocks: are they truly intramuscular? Eur J Radiol. 2006;58(3):480–484. | ||
Cocoman A, Murray J. Intramuscular injections: a review of best practice for mental health nurses. J Psychiatr Ment Health Nurs. 2008;15(5):424–434. | ||
Potter AP, Perry AG, Stockert PA, Hall AM. Fundamentals of Nursing. 8th ed. Canada: Mosby; 2013. | ||
Wynaden D, Landsborough I, Mcgowan S, et al. Best practice guidelines for the administration of intramuscular injections in the mental health setting. Int J Ment Health Nurs. 2006;15(3):195–200. | ||
Carter H, Mccoy TT. Are we on the same page? A comparison of intramuscular injection explanations in nursing fundamental texts. Medsurg Nurs. 2008;4(17):237–240. | ||
Malkin B. Are techniques used for intramuscular injection based on research evidence? Nurs Times. 2008;104(50–51):48–51. | ||
Nicoll LH, Hesby A. Intamuscular injection: an integrative research review and guideline for evidence-based practise. Appl Nurs Res. 2002;16(2):149–162. | ||
Kaya N, Salmaslioğlu A, Terzi B, Turan N, Acunaş B. The reliability of site determination methods in ventrogluteal area injection: a cross-sectional study. Int J Nurs Stud. 2015;52(1):355–360. | ||
Elgellaie A, Ashcroft E, Larkin TA. Effects of thickness of muscle and subcutaneous fat on efficacy of gluteal intramuscular injection sites. Br J Nurs. 2018;27(6):300–305. | ||
Hunter J. Intramuscular injection techniques. Nurs Stand. 2008;22(24):35–40. | ||
Güneş ÜY, Ceylan B, Bayindir P. Is the ventrogluteal site suitable for intramuscular injections in children under the age of three? J Adv Nurs. 2016;72(1):127–134. | ||
Engstrom JL, Giglio NN, Takacs SM, Ellis MC, Cherwenka DI. Procedures used to prepare and administer intramuscular injections: a study of infertility nurses. J Obstet Gynecol Neonatal Nurs. 2000;29(2):159–168. | ||
Greenway K, Merriman C, Statham D. using the ventrogluteal site for intramuscular injections. Learning Disability Practice. 2006;9(8):34–37. | ||
Donaldson C, Green J. Using the ventrogluteal site for intramuscular injections. Nurs Times. 2005;101(16):36–38. | ||
Güneş ÜY, Zaybak A, Biçici B, Çevik K. Nurses examination of application intramuscular injection process [Hemşirelerin intramüsküler enjeksiyon işlemine yönelik uygulamalarinin incelenmesi]. Journal of Ataturk University School of Nursing. 2009;12(4):84–90. | ||
Gülnar E, Çalişkan N. Ventrogluteal intramuscular injection for nurse examination of knowledge for practise [Hemşirelerin ventrogluteal bölgeye intramüsküler enjeksiyon uygulamasina yönelik bilgi düzeylerinin belirlenmesi]. Dokuz Eylül University School of Nursing Electronic Journal. 2014;7(2):70–77. | ||
Öner N, Le Compte A. Sürekli durumluk/sürekli kaygi envanteri el kitabi. 2nd ed. Istanbul: Boğaziçi University; 1998. | ||
Durmuş S, Günay O. Factors affecting job satisfaction and anxiety level in nurses [Hemşirelerde iş doyumu ve anksiyete düzeyini etkileyen factor]. Erciyes Medical Journal. 2007;29(2):139–146. | ||
Yalcin E, Köse S, Akyüz M. Comparing the distance of different intramuscular gluteal injection sites to the sciatic nerve. J Nov Physiother Phys Rehabil. 2015;2(1):014–015. | ||
Walsh L, Brophy K. Staff nurses’ sites of choice for administering intramuscular injections to adult patients in the acute care setting. J Adv Nurs. 2011;67(5):1034–1040. | ||
Freitag VL, Dalmolin IS, Badke MR, Petroni S. Ventrogluteal intramuscular injections: knowledge about the technic by nursing professionals. J Nurs UFPE online, Recife. 2015;9(2):799–805. | ||
Coskun H, Kiliç C, Senture C. The evaluation of dorsogluteal and ventrogluteal injection sites: a cadaver study. J Clin Nurs. 2016;25(7–8):1112–1119. | ||
Gülnar E, Özveren H. An evaluation of the effectiveness of a planned training program for nurses on administering intramuscular injections into the ventrogluteal site. Nurse Educ Today. 2016;36:360–363. | ||
Small SP. Preventing sciatic nerve injury from intramuscular injections: literature review. J Adv Nurs. 2004;47(3):287–296. | ||
Cornwall J. Are nursing students safe when choosing gluteal intramuscular injection locations? Australas Med J. 2011;4(6):315–321. | ||
Wynaden D, Tohotoa J, Al Omari O, et al. Administering intramuscular injections: how does research translate into practice over time in the mental health setting? Nurse Educ Today. 2015;35(4):620–624. | ||
Güneş ÜY, Kara D, Ari S, Ceyhan O. Which site is more painful in intramuscular injections? The dorsogluteal site or the ventrogluteal site? A case study from Turkey. Clin Nurs Stud. 2013;4(1):74–80. | ||
Masuda S, Yasuhara Y, Tanioka T, et al. Comparison of gluteal muscle intramuscular injection sites of Japanese healthy subjects: considerations for optimal insertion of injection needle length. Open J Psychiatr. 2016;06(02):203–212. | ||
Moharreri AR, Nasiri H, Jahanshahi M, Rahmani H, Abdollahi A, Rabiei M. The comparison of pain intensity and rate of bleeding in intramuscular injection in dorsogluteal and ventrogluteal area. Journal of Gorgan University of Medical Sciences. 2007;9(3):37–41. | ||
Wynaden D, Landsborough I, Chapman R, Mcgowan S, Lapsley J, Finn M. Establishing best practice guidelines for administration of intra muscular injections in the adult: a systematic review of the literature. Contemp Nurse. 2005;20(2):267–277. | ||
Şanlialp A, Kurban NK. Assessing Effectiveness of Education about Knowledge and Frequency of Dorsogluteal and Ventrogluteal Site Selection and Z Technique on Nurses’ IM Injection Practices [Hemşirelerin IM enjeksiyon uygulamasinda dorsogluteal ve ventrogluteal bölge seçimi ile Z tekniği ile ilgili bilgi ve uygulama sikliğinda eğitimin etkinliğinin değerlendirilmesi] [Pamukkale University Health Sciences Institute master’s thesis]. Denizli: Turkey; 2013. | ||
Altun I, Cinar ND, Öc B. Best practice techniques for administration of injections: Impact of lecture based interactive workshops on training of nurses. Pak J Med Health Sci. 2010;26(1):152–157. | ||
Hdaib MT, Al-Momany SM, Najjar YW. Knowledge level assessment and change among nursing students regarding administering intra-muscular injection at Al-Balqa’a Applied University: an interventional study. Nurse Educ Today. 2015;35(7):e18–e22. | ||
Zaybak A, Güneş UY, Tamsel S, Khorshid L, Eşer I, Yü G, I E. Does obesity prevent the needle from reaching muscle in intramuscular injections? J Adv Nurs. 2007;58(6):552–556. | ||
Greenway K. Using the ventrologluteal site for intramuscular injection. Nurs Stand. 2004;18(25):39–42. |
 © 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2018 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.