Back to Journals » Risk Management and Healthcare Policy » Volume 16
COVID-19 Pandemic Brings Challenges to the Management of Stroke—The Differences Between Stroke Cases Admitted to a Tertiary Hospital Before and During COVID-19 Pandemic in China
Authors Ouyang H, Jiang H, Huang J, Liu Z
Received 12 August 2023
Accepted for publication 11 December 2023
Published 23 December 2023 Volume 2023:16 Pages 2893—2905
DOI https://doi.org/10.2147/RMHP.S435094
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Hui Ouyang,1 Hong Jiang,1 Jin Huang,2 Zunjing Liu1
1Department of Neuromedicine, Peking University People’s Hospital, Beijing, People’s Republic of China; 2Department of Emergency, Yiyang Central Hospital, Yiyang, Hunan, People’s Republic of China
Correspondence: Zunjing Liu, Email [email protected]
Background: An international public health emergency has resulted from the emergence of the new coronavirus-2. Both direct and indirect influences have been felt on the treatment of acute stroke. However, no conclusive link between COVID-19 and the alleged decline in admissions for stroke-related reasons has been established, and the findings of recent studies are contentious. Most of those researches are not made use of authentic data. Therefore, the goal of this study is to examine how the COVID-19 pandemic has affected hospital admissions for stroke patients, to provide a basis for managing stroke patients in hospitals during COVID-19 pandemic.
Methods: This retrospective study took place at the People’s Hospital of Peking University in Beijing, China. For each patient, interventions such as the application of tissue plasminogen activator (tPA) were examined. We recorded each patient’s outcomes. The stroke patients’ hospital admissions were compared to the average of the prior year. As the time span of interest, we selected the epidemic period (January 2020 to December 2020).
Results: When compared to the previous year in the pre-COVID period, mean monthly stroke hospitalizations decreased during the pandemic by 54.42% (P< 0.001); average lengths of stay (ALOS) increased; and non-emergency admissions decreased by 78.8% (P< 0.001). The monthly volume of stroke patients exceeding the intravenous thrombolysis (IVT) window decreased by 25% and 59.73%, respectively (P < 0.001). There was a 5.3% increase in the percentage of IVT or within IVT time window in male stroke patients (p=0.019; p=0.049). During COVID-19, the proportion of non-local patients among male stroke patients decreased by 10% compared with the previous year (p=0.006).
Conclusion: The COVID-19 epidemic has had a negative impact on stroke management in China, healthcare systems must work to assess and adapt to the new reality.
Keywords: stroke, COVID-19, hospital management
Introduction
An international public health emergency has resulted from the emergence of the new coronavirus-2 (SARS-Cov-2). The pandemic has affected almost all nations, and in many of them, there have been severe limits on day-to-day activities. In the meantime, SARS-Cov-2 disease (COVID-19) primary and secondary effects had to be managed by the national health systems. During the COVID-19 pandemic, health care for non-COVID-19 cases was affected.1 The pandemic could have a big effect on how well healthcare is managed for acute strokes among other things. The indirect effects of COVID-19 may result from the deployment of resources to combat it, leaving fewer resources available for the treatment and research of patients who do not have COVID-19.2 On the other hand, due to their long hours, shift work, and heavy emotional strain, healthcare personnel have long been infamously high risk of experiencing burnout before the pandemic.3,4 The COVID-19 epidemic made it increasingly obvious that hospital administration is essential for averting shortages, effectively allocating staff, and delivering the highest quality care in a healthcare system that is overburdened.5
Worldwide, cerebrovascular illnesses rank second in terms of mortality. Up to 50% of stroke survivors experience chronic disability, placing a significant burden on public health with dire economic and social repercussions.6 The annual number of strokes and deaths due to stroke increased substantially from 1990 to 2019.7 The burden of stroke in China is also increasing in recent years.8 The COVID pandemic has created new obstacles for providing the greatest stroke care, though. The COVID-19 pandemic and the steps adopted to stop the disease’s spread have had an adverse impact on stroke medical care. Both direct and indirect influences have been felt on the treatment of acute stroke. Pathways for the management of stroke have been significantly altered by the use of numerous restrictive measures to stop the spread of COVID-19. The fear of acquiring COVID-19 infection from hospitals has been demonstrated to make patients with acute medical events including stroke and ST-segment elevation myocardial infarction (STEMI) less likely to visit hospitals.9–13
There have been indications of a considerable decline in stroke admissions since the COVID-19 epidemic, according to hospitals and stroke centers. At the local, regional, and national levels, acute stroke hospitalizations were found to have significantly decreased.14–17 Many people had the impression that hospitals were unsecure locations where high-risk patients (such as the elderly, diabetic, hypertensive, and obese) could get COVID-19.2,4 According to studies conducted in European nations, patients’ fears of infection frequently prevented them from visiting the hospital, as did the doctors who treated them. The majority of those studies, however, used electronic health record (EHR) data from integrated health care systems to characterize hospital admissions and emergency department (ED) interactions associated to stroke. This data was not original and was only provided in a generalized manner; it was not in-depth.
The strain of the pandemic is thought to have adversely affected the care of stroke patients, although the precise effect of the COVID-19 pandemic on these quality indicators is not yet known. The number of stroke cases visiting hospitals and stroke centers is dropping alarmingly. Most studies revealed a striking fall, with a notable drop in the frequency of reperfusion treatments. However, no conclusive link between COVID-19 and the alleged decline in admissions for stroke-related reasons has been established, and the findings of recent studies are contentious. According to several surveys, there has been a 10–30% decline in all types of stroke patients and a 50% decline in interventional instances such acute thrombectomy. However, several centers failed to notice modifications in the number of IS admissions.15,18–21 The majority of research made the assumption that one of the contributing factors to this drop may be the fear of getting infected from stroke victims and their families. There is, however, little research on how stroke therapy in developing countries has been impacted by the COVID pandemic. The majority of studies hypothesized that the causes for this decline may include the worry of contracting an infection from stroke victims and their family. However, there are few studies on how the COVID pandemic has affected stroke treatment in developing nations.
In Beijing, North China, our facility is a tertiary care hospital. With more than 21 million inhabitants, Beijing is the second most populated metropolis in China. The COVID-19 pandemic-related modifications in the care of stroke in major tertiary hospitals in developing country cities can be seen in our hospital’s scenario. In order to identify potential strategies to continue providing high-quality stroke care throughout a crisis, we looked into how the COVID-19 epidemic affected stroke care at our center in this study. The goal is to study the original data obtained from electronic patient records in order to determine how the COVID-19 epidemic has affected hospital admissions for stroke patients.
Method
Study Design
We performed a retrospective study comprising 789 stroke patients, after excluding 25 patients because of missing data or unclear diagnosis (The flow chart is shown in Figure 1). A recognized comprehensive stroke center, Peking University’s People’s Hospital in Beijing, China, served as the site of this retrospective observational study. The stroke patients’ hospital admissions were compared to the average of the prior year. As the time span of interest, we selected the epidemic period (January 2020 to December 2020). The pre-pandemic timeframe (January 2019 to December 2019) was contrasted with this era. Containment procedures are continued through the study’s conclusion. General neurology and neurology emergency departments’ urgent and planned hospital admissions were examined.
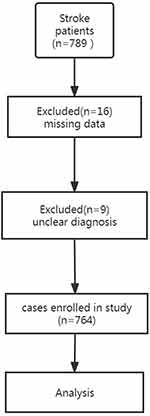 |
Figure 1 The flow chart of the inclusion process. |
We looked at the medical records on technological devices. In regard to the date of hospital admission, we noted when symptoms first appeared (if any). For each patient, interventions such as the application of tissue plasminogen activator (tPA) and mechanical thrombectomy (MT) were examined. We recorded each patient’s outcomes, including whether they were sent home, admitted to an acute rehabilitation facility, or passed away. The period of time between the onset and the first reported symptom was called the “onset-to-door time”. ALOS, or the average length of stay in the hospital, was defined. IVT was defined as the administration of intravenous thrombolysis only for acute ischemic stroke. Our database includes all stroke admissions as well as all intravenous thrombolysis (IVT) and endovascular treatment (EVT) reperfusion interventions carried out by medical professionals at Peking University, People’s Hospital between January 1 and December 31, 2020. The burden of COVID-19 peaked in China around 2020, hence this study chose to concentrate on data from both 2019 and 2020.
Study Population
All patients who have stroke symptoms are assessed to see if additional testing at a stroke center is necessary. The stroke center uses specific diagnostic testing, such as neuroimaging, to determine whether a patient is a candidate for intravenous tPA therapy and/or EVT. We chose patients for this study based on the following standards: Age requirement of 18 years or older, admission to the Peking University People’s Hospital departments of neurology and neurology emergency, and use of the DRG codes for subarachnoid hemorrhage (SAH/DI60), intracerebral hemorrhage (ICH/DI61), and ischaemic stroke (IS/DI63).22 Male and female patients were counted separately in addition to the total number of patients.
Data
Data were taken from the People’s Hospital at Peking University’s original electronic medical record. From 1 January 2019 to 31 December 2020, covering the two years of the pandemic and pre-pandemic, we gathered data on all stroke cases admitted to hospitals.
Statistical Analysis
In order to compare the figures for the year 2020 with the mean and 95% confidence interval from the previous year, the findings are expressed as total patients or percentages. A significant difference is considered with p<0.05. The Chi-squared analysis was performed to compare categories individually or to compare proportional changes between the pre-pandemic and pandemic periods. Student’s t-test was performed to compare continuous variables between the two time periods. For properly distributed data, continuous variables are reported as means and SD. Counts and percentages are used to display categorical variables. SPSS version 27.0 was used for all statistical analyses.
Results
The differences of epidemiology and outcomes of stroke hospital admission during COVID-19 prepandemic and pandemic period.
A total of 764 stroke patients who were admitted to the hospital between January 1 and December 31, 2020, were studied. When compared to the previous year in the pre-COVID period, mean monthly stroke admissions during the pandemic (Table 1) reduced by 54.42% (P< 0.001), while ALOS increased by 33.13% (P<0.001). Non-emergency admissions decreased during the pandemic by 78.8% compared to the pre-pandemic era (P<0.001), whereas emergency admissions did not change (p = 0.513). The monthly volume of patients who exceeded the IVT time window decreased by 25% and 59.73%, respectively (P<0.001). During the pandemic, there was no change in the monthly volume of patients within the IVT window or who received IVT (p=0.685; p=0.876). Age, onset-to-door time, stroke history, number of previous strokes, occupation and death toll did not change significant. (p=0.086; p=0.280; p=0.076; p=0.786; p=0.219; p=0.733; p=0.999).
 |
Table 1 Epidemiology and Outcomes of Stroke Hospital Admission During COVID-19 Prepandemic and Pandemic Period |
The age and times of hospital admission was related to onset-to-door time and ALOS in the pre-COVID period (p<0.05), but not related to onset-to-door time or ALOS in the COVID period (p>0.05) (Table 2 and Table 3).
 |
Table 2 The Association of Epidemiology and Clinical Characteristic of Stroke Patients During COVID-19 Prepandemic and Pandemic Period (1) |
 |
Table 3 The Association of Epidemiology and Clinical Characteristic of Stroke Patients During COVID-19 Prepandemic and Pandemic Period (2) |
Urban sourced patients are associated with stroke history and non-local sourced patients in the re-COVID period (p<0.05), but not associated with non-local sourced patients in the COVID period (p>0.05).
In the COVID-19 period compared to the prior year, there was a 5.3% increase in the percentage of IVT or within IVT time window in male stroke patients (p=0.019; p=0.049), but not in female stroke patients (p=0.326; p=0.435). During the period of COVID-19, the proportion of nonlocal patients in male stroke patients decreased by 10% compared with the previous year (p=0.006). However, there was no significant change in the proportion of non-local patients among female stroke patients (p=0.874). Both the number of non-emergency admissions and the monthly hospitalizations for stroke were significantly reduced in both male and female stroke patients (p< 0.001) (Table 4).
 |
Table 4 The Epidemiology and Clinical Characteristic of Male and Female Stroke Patients During COVID-19 Prepandemic and Pandemic Period |
Discussion
It’s doubtful that COVID-19 will cause a short-term pandemic. Thus, COVID-19 will probably alter how we provide stroke care for years to come. The care of patients with stroke, which affects 1 in 4 individuals over the age of 25 in their lifetime and kills approximately 5.5 million per year, has been made significantly more difficult by this pandemic.23 Studies from every nation reported that the COVID-19 pandemic had some unfavorable effects on stroke care, albeit with wide variances.18,20,21,24,25 The results of earlier studies have revealed that patients’ delayed or nonarrival at hospitals due to a variety of factors has an effect on the administration of reperfusion therapy for stroke. Numerous reports and earlier studies have shown that the public’s concern for getting the virus has led to a decline in the use of emergency medical services.10,18,26 In addition, the COVID-19 pandemic has had both direct and indirect impacts on the ability of emergency systems to deliver high quality care in acute settings.27 Being forced to isolate, diagnose, and treat patients with COVID-19 while still managing other emergent cases is taxing on both the healthcare system and healthcare professionals (CDC COVID data tracker. Centers for disease control and prevention. Published March 28.2020. https://covid.cdc.gov/covid-data-tracker Accessed January 20, 2022). The COVID-19 pandemic has been directly shown to increase the amount of healthcare workers suffering from exhaustion and subsequent burnout symptoms in several studies.28,29 The emergency medical services (EMS) is also impacted by the COVID-19 pandemic.30,31 The COVID-19 epidemic also has negative impact on the medical system of China.32 Due to the significant impact of the epidemic on stroke patients, healthcare provider and society, it is necessary to explore the optimization and adjustment of hospital management under the epidemic. Compared to previous researches, our study included the demographic and clinical characteristics of stroke patients in a more comprehensive and in-depth manner.
We compared the epidemic period that followed the start of lockdown to the prior year and found that there was a considerable drop in the number of ward admissions and a corresponding rise in the proportion of urgent patients and IVT cases. Consistent with the results of previous research,33 we discovered a 54.42% decrease in stroke admissions during the pandemic compared to the year before. Among them, there was a 78.8% drop in outpatient clinic admissions. Different from a previous study,33 our results indicated that during the COVID-19 pandemic, the average length of hospital stay of stroke patients has been prolonged rather than shortened, and the mortality of in hospital patients has not increased significantly. The reason may be the data used in that study included data from hospitals in areas with low levels of healthcare. Some hospitals did not have the condition taking isolation measures to deal with COVID-19, so they may have taken the strategy of letting patients leave the hospital as soon as possible to reduce cross infection, resulting in the shortening of the average length of stay. In addition, due to the isolation measures and fear of infection, more patients choose to seek treatment locally with poor medical conditions instead of going to large general hospitals with higher standard of medical care, leading to an increase in mortality rates. Our study was conducted in a large tertiary hospital with well-established isolation facilities and relatively high levels of diagnosis and treatment, which may explain the inconsistency of results about mortality rates.
It is improbable that the substantial decline in the incidence of stroke between the pre-pandemic and pandemic periods in our study was the result of organic decline. According to earlier studies, individuals with clinical signs of transient ischemic attack and small stroke were primarily responsible for this decline, while admissions of patients with severe stroke did not change.2,4 In the UK, where there was also an increase in the typical severity of cases presenting at hospitals, similar admission trends were seen.29 The decline in hospital admissions for stroke suggests a possible impact of the pandemic on the time-dependent stroke pathway. Our study’s findings and those of several earlier studies show a sharp decline in outpatient clinic admissions. This is probably because some patients, particularly those with minor symptoms, may decide against getting hospital treatment out of concern for COVID-19. More minor illnesses are being managed at home or local small hospitals, which may potentially be contributing to the decline in stroke admissions to tertiary care hospitals. The overall number of stroke hospital admissions may have decreased as a result of fewer improper hospitalizations or the impaired ability of healthcare providers to deliver high quality care during the pandemic. For example, In China, the shortage of critical care capacity (ICU) has been reported.34 Insufficient ICU capacity may also be one of the reasons for the decrease in admitted patients, and some critically ill patients may have died before coming to the hospital for treatment or they are force to stay at local hospitals for treatment, without chance of being transferred to large hospitals with ICU. However, during the pandemic, due to limited space and funding, the capacity of ICU in our hospital has not increased and remains fully booked. Hence, the changes in the number of ICU patients were not recorded in this study.
In other investigations, acute care for a number of urgent medical conditions—including stroke and STEMI during the pandemic—has been found to take noticeably longer than expected.25,35–38 The public’s hesitation to present in ED settings due to worries about catching COVID is more likely the cause of this.37,38 Another cause may be the change of healthcare systems during COVID pandemic. The COVID-19 pandemic has significantly burdened healthcare systems worldwide.39 In the face of the COVID-19 epidemic, the medical system struggle to cope, the medical staff paid a heavy price confronted with COVID-19.32 The impact of COVID epidemic to healthcare system, such as lack of suitable transportation options, limited ambulance resource, delays caused by isolation or wearing protective equipment may also be significant concerns. However, the onset-to-door time was shown to have decreased by 14.34% during the pandemic period in our investigation, although these results were not statistically significant. This could be explained by a sudden increase in emergency admitted stroke patients, who normally have shorter onset-to-door times, and a sharp drop in non-emergency admitted stroke patients, who typically have longer onset-to-door times. One theory is that during the COVID-19 pandemic era, people may not seek medical care for acute neurological symptoms unless they believe they are so “severe” (perhaps IVT and EVT candidate instances) that they have no other option.
Our study’s findings show that non-emergency hospital admissions and stroke patients who did not receive IVT have greatly dropped, whereas emergency hospital admissions and stroke patients who did receive IVT have not decreased. According to other studies, the use of IVT or EVT treatments has decreased.11,40 In contrast to the findings of our study, Rudilosso et al describe a decrease in stroke hospitalization and thrombectomies, notably in the senior group9 without compromising quality of care measures.
In contrast to the majority of earlier studies, our study’s findings revealed that the number of stroke patients having IVT and emergency hospital admission did not significantly decline. Our results show that during the epidemic, the proportion of stroke patients underwent IVT has increased, possibly due to the fact that stroke patients with seemingly “mild” symptoms are unwilling to come to the hospital for treatment due to fear of infection, isolation, and inconvenient medical procedures caused by the epidemic, while patients with seemingly “severe” symptoms are more likely to be urgently sent to the hospital for treatment within the thrombolytic time window during the epidemic. This may be one of the reasons for the increase in the proportion of thrombolytic patients during the epidemic in our research. In addition, the vast majority of thrombolytic patients are emergency patients, and the increase in the proportion of thrombolytic patients may also be related to the increase in the proportion of patients seeking emergency treatment. According to our findings, there was a relative rise in urgent patients during the COVID pandemic compared to non-urgent cases. This can be because China’s emergency system and hospital management are different from those in Western nations. First, during the COVID pandemic, stroke victims in China were treated and admitted to hospitals at a lower rate than those in the West due to fear of the virus and a lack of stroke knowledge. Second, during the pre-epidemic period, some patients in China who do not require emergency care seek treatment at the neurology emergency department due to relative low emergency and ambulance fees, consultation fees, and other factors. This results in a relative shortage of emergency medical resources, which may prevent some thrombolytic patients who require IVT treatment from receiving timely care. On the other hand, heavy traffic in China’s major cities prior to the outbreak may have contributed to some stroke patients’ delayed delays from onset to door, causing them to arrive after the opportunity for thrombolysis had closed. Acute stroke patients who need IVT treatment have better opportunity for prompt treatment during the epidemic since there are much fewer non-emergency individuals seeking medical attention in the neurology emergency room. Thirdly, fewer patients missed the window for receiving stroke thrombolysis during the epidemic era because individuals spent more time at home, which reduced traffic congestion and allowed ambulances to get to hospitals faster. The availability of transportation was severely constrained when the city was in lockdown. However, prehospital delay time should be decreased due to less traffic as long as there are enough ambulances and drivers. Finally, there may be isolation and complicated epidemiological investigation procedures in non-emergency outpatient clinics of Chinese hospitals. As a result of the inconvenience these procedures cause, some stroke patients may decide not to seek treatment. Stroke patients are more willing to seek medical attention at the neurology emergency department during an epidemic because there are not any onerous isolation and epidemiological investigation measures there. As a result, they are more likely to enter the green channel for stroke and receive prompt IVT treatment.
There was a strong link between the onset-to-door time and age, as well as the number of previous hospitalizations, during the pre-pandemic period. This could be attributed to elderly people’s lack of stroke education and understanding of the importance of timely stroke treatment. Patients who have been hospitalized frequently in the past may have become acclimated to physical discomfort and stroke, leading in extended onset-to-door durations. During the pandemic, the onset-to-door time, number of previous hospitalizations, and age were no longer associated. The reason could be that patients’ fear of infection and isolation measures have had a considerable impact on the onset-to-door time of stroke patients, outweighing the impact of age and previous hospital admissions. There was a strong link between stroke history and urban inhabitants, as well as age among hospitalized patients, during the pre-pandemic period, presumably due to an unhealthy diet and lack of activity among urban residents. Strokes were more common in those over the age of 65. During the epidemic, urban residence and age were no longer linked to a history of stroke. The explanation for this could be that the fear of infection, as well as isolation measures, has a significant impact on the admission of stroke patients. Many stroke patients who should have been hospitalized have opted out, causing changes in the demographic makeup of stroke patients admitted to hospitals.
Our study’s findings suggest that the pandemic may have a greater impact on male stroke sufferers. The impact of gender on acute ischemic stroke, in terms of presentation, severity, etiology, and outcome, is increasingly getting recognized.41 Therefore, Results of our research and previous researches indicate that COVID-19 is likely to have different effects on stroke patients of different gender. However, it is difficult to explain the gender difference in the impact of COVID-19 on stroke patients which were found in our study. These results about gender differences require further, large-scale, and multicenter research to confirm, and may require further research to explore the mechanism of the impact of COVID-19 on stroke patients of different gender in the future.
Our study’s findings indicate that the COVID-19 epidemic has a significant impact on stroke management. Patients may not have sought treatment as soon as they should have because of their fear of developing COVID-19. Additionally, patients who were not hospitalized might have missed out on secondary prevention services like carotid revascularization, anticoagulation for atrial fibrillation, antiplatelet therapies, lipid lowering, and blood pressure control. The rate of subsequent strokes would be significantly impacted by the absence of effective secondary stroke prevention. Patients with stroke were substantially less likely to seek care due to a lack of understanding about stroke combined with fear of the virus.
According to our data, the amount of time needed to provide critical stroke therapies, such as r-tPA (door-to-needle), did not alter significantly. When compared to the pre-pandemic period, there was no statistically significant increase in the onset-to-door time among stroke patients. Our study’s conclusions offer some management guidance for hospitals during the COVID outbreak. The findings demonstrated that while emergency stroke patients, particularly those who were within the thrombolysis time window and underwent thrombolysis, did not decrease, while stroke patients in outpatient clinics did contribute to the decline in stroke hospitalization during the pandemic period. This shows that hospitals have handled stroke situations during the COVID outbreak effectively and efficiently. The majority of stroke patients who require secondary prevention of stroke and are beyond the thrombolysis window are affected by the epidemic. The two main causes of the decline in the number of stroke patients admitted to hospitals are: first, a lack of knowledge about stroke (patients who are adequately informed about stroke tend to arrive at the hospital within the window for thrombolysis); and second, more isolation interventions in non-emergency departments that result in subpar medical procedures and limit patients’ ability to travel to the hospital for treatment. Therefore, our results indicate that during the epidemic, the hospital does not need to spend too much energy on the reconstruction of the emergency department of Neurology, but needs to pay more attention to the patients who need secondary prevention of stroke outside the thrombolysis time window at outpatient clinics. The main measures that can be taken include: providing stroke patient education, improving isolation measures procedures, and providing residents with secondary stroke prevention drugs that can be obtained outside the hospital near their place of residence. Therefore, our findings suggest that during an epidemic, the hospital should focus more on patients who require secondary prevention of stroke outside of the thrombolysis time window at outpatient clinics rather than expending excessive energy on rebuilding the emergency department of neurology. The key actions that may be performed are: educating stroke patients, enhancing isolation protocols, and giving residents access to secondary stroke prevention medications that can be purchased locally, away from the hospital.
The decline in stroke hospitalization during the pandemic has a number of causes. First, because they are worried about getting sick, the patients do not want to be admitted to the hospital. A hospital’s capacity to treat stroke patients may also be impacted by the need to reduce exposure and redistribute personnel and resources. Resource management must prioritize time-sensitive illnesses like stroke and myocardial infarction when a significant number of patients with possible COVID-19 are using up laboratory space and computed tomography (CT) scanners. In a pandemic, resource management is crucial. These resources include pertinent specialists, additional supporting staff, tools, lab analyses, personal protective equipment, etc. The care of strokes during a pandemic could be impacted by a lack of medical personnel. Numerous earlier research have conclusively demonstrated that the COVID-19 epidemic has increased the number of healthcare professionals experiencing weariness and associated burnout symptoms,28,29 which could lead to a decreased quality of care to patients.42 Infected healthcare workers may reduce the number of workers delivering stroke care. The decline in stroke hospital admissions may be due to other factors. The number of stroke cases in stroke centers has decreased since the shutdown. The management for stroke patients has been severely hampered by the COVID-19 screening procedure. The COVID-19 screening procedure may slow down consultations, lower the number of patients seen at outpatient clinics, increase the time from arrival to treatment, and even lead some patients to forego consultations because of the cumbersome screening procedures. Unrecognized ailments may have occurred due to lockdown, lack of social interaction, and distance constraints. Rapidly prohibiting the admission of elective, non-acute IS cases, these restrictive measures may have also increased the proportion of reperfusion treatments during the pandemic period.
This study emphasizes the need for a strong stroke care organization that makes care more accessible even when the healthcare system is stressed. Hospitals and society can take a number of actions to enhance stroke management during the epidemic. The key is raising stroke awareness amid a crisis. The majority of stroke centers have ceased or scaled back their efforts to educate the public about stroke. Education about stroke is perhaps never more crucial than during a pandemic. It might also encourage choices like media efforts to change people tendencies to delay seeking medical attention after experiencing stroke symptoms. During this pandemic, there is a need to increase stroke awareness and dispel the public’s anxiety. Since a stroke can be fatal, education should emphasize the need to recognize the symptoms of a stroke as well as the necessity of visiting the hospital. To inform patients about what to do during the pandemic, a strong systematic educational network needs to be built and improved. In terms of hospital administration, the COVID-19 screening procedure should not impede the start of stroke therapy. A surgical mask should be worn by patients at all times to prevent the spread of infectious diseases. The acute stroke team should collaborate closely with infectious disease specialists to create a workflow strategy that reduces delays while ensuring the medical personnel is properly protected. It is important to start resource management as soon as feasible. The assignment of designated stroke centers is necessary to preserve resources for the provision of high-quality stroke care. At the national level, a campaign should be launched to promote appropriate hospital evaluation for urgent, curable, time-sensitive illnesses like myocardial infarction and stroke. Leaders of professional organizations should collaborate closely with legislators and government representatives to ensure that society is supported. The stroke care model may need to change, nevertheless, in order to maintain the quality of the treatment and reduce the risk of infection among medical personnel.
Conclusion
The main finding of this study was that the COVID-19 outbreak had a substantial impact on stroke care in China, resulting in a considerable drop in stroke hospitalization, particularly for mild, non-emergency stroke patients and those outside the window for thrombolysis. Additionally, compared to female stroke patients, male stroke patients are more affected by the pandemic. Our analysis shows that, in contrast to the findings of other studies, there was no appreciable difference in the amount of time needed to administer r-tPA (door-to-needle), treat stroke patients inside the thrombolysis window, or administer r-tPA. The findings show that the epidemic has had a negative impact on stroke management. In conclusion, healthcare systems must work to assess and adapt to the new reality. A significant limiting element was probably patients’ refusal to visit the hospital. Increased stroke awareness campaigns, effective resource management, and the designation of stroke centers during the crisis are required.
Study Strengths and Limitations
Our analyses may not have been able to distinguish between different revascularization strategies due to the small size of the study population, and a bigger cohort may have allowed for a more accurate detection of any EVT volume alterations. Additionally, since this study only involved one center, we are hesitant to make broad implications. The findings point up significant trends, but they cannot be used to establish causality with certainty. Despite limitations, a thorough review of changes in acute stroke care is provided by the range of factors addressed. There are not many of these studies from middle-income countries, but the findings are significant enough that they might be used in developing nations. Our analysis emphasizes the value of ongoing monitoring of the stroke care system and the lessons from the COVID-19 era that may be applied to safeguard stroke care in subsequent waves or potential epidemics.
Data Sharing Statement
Authors declare that data and materials described in the manuscript are freely available to any scientist wishing to use them, without breaching participant confidentiality. The contact should be made via the corresponding author ([email protected]).
Ethics Approval and Consent to Participate
The study has been has been approved by the ethics committee of Peking University People’s Hospital, China (No. 2022-175). Since this was a retrospective study, written individual patient consent was waived. All ethic procedures were performed were in accordance with the ethical standards of the Declaration of Helsinki (World Medical Association 2013).
Acknowledgment
We thank Prof. Jun Zhang and Yongjie Li for their helpful advice.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Youth’s Cultivating Funding of Peking University, Health Science Center, BMU2022PZYB015 and the medical service and support capacity improvement project from the National Health Commission (Grant No.2199000731).
Disclosure
The authors declare that there are no conflicts of interest regarding the publication of this paper.
References
1. Kendzerska T, Zhu DT, Gershon AS. The effects of the health system response to the COVID-19 pandemic on chronic disease management. Narrat Rev. 2021;14:575–584.
2. Emanuel EJ, Persad G, Upshur R, et al. Fair allocation of scarce medical resources in the time of Covid-19. N Engl J Med. 2020;382(21):2049–2055. doi:10.1056/NEJMsb2005114
3. Lim R, Aarsen KV, Gray S, Rang L, Fitzpatrick J, Fischer L. Emergency medicine physician burnout and wellness in Canada before COVID19: a national survey. Can J Emerg Med. 2020;22(5):603–607. doi:10.1017/cem.2020.431
4. Adams JG, Walls RM. Supporting the health care workforce during the COVID-19 global epidemic. JAMA. 2020;323(15):1439–1440. doi:10.1001/jama.2020.3972
5. Peiffer-Smadja N, Lucet JC, Bendjelloul G, et al. Challenges and issues about organizing a hospital to respond to the COVID-19 outbreak: experience from a French reference centre. Clin Microbiol Infect. 2020;26(6):669–672. doi:10.1016/j.cmi.2020.04.002
6. Donkor ES. Stroke in the 21(st) century: a snapshot of the burden, epidemiology, and quality of life. Stroke Res Treat. 2018;2018:3238165. doi:10.1155/2018/3238165
7. Feigin VL, Stark BA, Johnson CO. Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet Neurol. 2021;20(10):795–820. doi:10.1016/S1474-4422(21)00252-0
8. Tu WJ, Wang LD. China stroke surveillance report 2021. Mil Med Res. 2023;10(1):33. doi:10.1186/s40779-023-00463-x
9. Teoh SE, Masuda Y, Tan DJH, et al. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: a systematic review and meta-analysis. Ann Intens Care. 2021;11(1):169. doi:10.1186/s13613-021-00957-8
10. Glober NK, Supples M, Faris G, et al. Out-of-hospital cardiac arrest volumes and characteristics during the COVID-19 pandemic. Am J Emerg Med. 2021;48:191–197. doi:10.1016/j.ajem.2021.04.072
11. Gale R, Eberlein S, Fuller G, Khalil C, Almario CV, Spiegel BMR. Public perspectives on decisions about emergency care seeking for care unrelated to COVID-19 during the COVID-19 pandemic. JAMA Network Open. 2021;4:e2120940.
12. Kiss P, Carcel C, Hockham C, Peters SAE. The impact of the COVID-19 pandemic on the care and management of patients with acute cardiovascular disease: a systematic review. Eur Heart J Qual Care Clin Outcomes. 2021;7(1):18–27. doi:10.1093/ehjqcco/qcaa084
13. Scquizzato T, Olasveengen TM, Ristagno G, Semeraro F. The other side of novel coronavirus outbreak: fear of performing cardiopulmonary resuscitation. Resuscitation. 2020;150:92–93. doi:10.1016/j.resuscitation.2020.03.019
14. Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51(7):1996–2001. doi:10.1161/STROKEAHA.120.030225
15. Rudilosso S, Laredo C, Vera V, et al. Acute stroke care is at risk in the Era of COVID-19: experience at a comprehensive stroke center in Barcelona. Stroke. 2020;51(7):1991–1995. doi:10.1161/STROKEAHA.120.030329
16. Kristoffersen ES, Jahr SH, Thommessen B, Rønning OM. Effect of COVID-19 pandemic on stroke admission rates in a Norwegian population. Acta Neurol Scand. 2020;142(6):632–636. doi:10.1111/ane.13307
17. Kerleroux B, Fabacher T, Bricout N, et al. Mechanical thrombectomy for acute ischemic stroke amid the COVID-19 outbreak: decreased activity, and increased care delays. Stroke. 2020;51(7):2012–2017. doi:10.1161/STROKEAHA.120.030373
18. de Havenon A. A rapid decrease in stroke, acute coronary syndrome, and corresponding interventions at 65 United States hospitals following emergence of COVID-19; 2020.
19. Feral-Pierssens AL, Claret PG, Chouihed T. Collateral damage of the COVID-19 outbreak: expression of concern. Eur J Emerg Med. 2020;27(4):233–234. doi:10.1097/MEJ.0000000000000717
20. Frisullo G, Brunetti V, Di Iorio R. Effect of lockdown on the management of ischemic stroke: an Italian experience from a COVID hospital. Neurol Sci. 2020;41(9):2309–2313. doi:10.1007/s10072-020-04545-9
21. Teo KC, Leung WCY, Wong YK, et al. Delays in stroke onset to hospital arrival time during COVID-19. Stroke. 2020;51(7):2228–2231. doi:10.1161/STROKEAHA.120.030105
22. Foley MM. DRG grouping and ICD-10-CM/PCS. J AHIMA. 2015;86:56–59.
23. Johnson W, Onuma O, Owolabi M, Sachdev S. Stroke: a global response is needed. Bull World Health Organ. 2016;94(9):634–63. doi:10.2471/BLT.16.181636
24. Agarwal S, Scher E, Rossan-Raghunath N, et al. Acute stroke care in a New York City comprehensive stroke center during the COVID-19 pandemic. J Stroke Cerebrovasc Dis. 2020;29(9):105068. doi:10.1016/j.jstrokecerebrovasdis.2020.105068
25. Bersano A, Kraemer M, Touzé E. Stroke care during the COVID-19 pandemic: experience from three large European countries. Eur J Neurol. 2020;27(9):1794–1800. doi:10.1111/ene.14375
26. Rangé G, Hakim R, Beygui F. Incidence, delays, and outcomes of STEMI during COVID-19 outbreak: analysis from the France PCI registry. J Am Coll Emerg Physicians Open. 2020;1(6):1168–1176. doi:10.1002/emp2.12325
27. Banfield WH, Elghawy O, Dewanjee A, Brady WJ. Impact of COVID-19 on emergency department management of stroke and STEMI. A narrative review. Am J Emerg Med. 2022;57:91–97. doi:10.1016/j.ajem.2022.04.033
28. Freund Y. The challenge of emergency medicine facing the COVID-19 outbreak. Eur J Emerg Med. 2020;27(3):155. doi:10.1097/MEJ.0000000000000699
29. Fitzpatrick K, Patterson R, Morley K, Stoltzfus J, Stankewicz H. Physician wellness during a pandemic. West J Emerg Med. 2020;21(6):83–87. doi:10.5811/westjem.2020.7.48472
30. Handberry M, Bull-Otterson L, Dai M, et al. Changes in emergency medical services before and during the COVID-19 pandemic in the United States, January 2018-December 2020. Clin Infect Dis. 2021;73(Supplement_1):S84–S91. doi:10.1093/cid/ciab373
31. Al Amiry A, Maguire BJ. Emergency Medical Services (EMS) calls during COVID-19: early lessons learned for systems planning (A Narrative Review). Open Access Emerg Med. 2021;13:407–414. doi:10.2147/OAEM.S324568
32. Li N, Yu X. Outbreak and Regression of COVID-19 epidemic among Chinese medical staff. Risk Manag Healthc Policy. 2020;13:1095–1102. doi:10.2147/RMHP.S268178
33. Tu WJ, Xu Y, Chen H, Li J, Du J. Impact of the COVID-19 pandemic lockdown on hospitalizations for cerebrovascular disease and related in-hospital mortality in China: a nationwide observational study. Arch Gerontol Geriatr. 2023;104:104832. doi:10.1016/j.archger.2022.104832
34. Tu WJ, Liu Y, Zeng X. Critical care capacity during the omicron wave of the COVID-19 pandemic in China: far from enough. Lancet Reg Health West Pac. 2023;31:100689. doi:10.1016/j.lanwpc.2023.100689
35. De Luca G, Verdoia M, Cercek M, et al. Impact of COVID-19 pandemic on mechanical reperfusion for patients with STEMI. J Am Coll Cardiol. 2020;76(20):2321–2330. doi:10.1016/j.jacc.2020.09.546
36. Erol MK, Kayıkçıoğlu M, Kılıçkap M, et al. Treatment delays and in-hospital outcomes in acute myocardial infarction during the COVID-19 pandemic: a nationwide study. Anatol J Cardiol. 2020;24(5):334–342. doi:10.14744/AnatolJCardiol.2020.98607
37. Janke AT, Gettel CJ, Haimovich A, Kocher KE, Krumholz HM, Venkatesh AK. Changes in emergency department arrival times for acute myocardial infarction during the COVID-19 pandemic suggest delays in care seeking. Circulation. 2022;15(2):e008402. doi:10.1161/CIRCOUTCOMES.121.008402
38. Gutovitz S, Pangia J, Finer A, Rymer K, Johnson D. Emergency department utilization and patient outcomes during the COVID-19 pandemic in America. J Emerg Med. 2021;60(6):798–806. doi:10.1016/j.jemermed.2021.01.002
39. Bahamdan AS. Review of the psychological impact of COVID-19 pandemic on healthcare workers in Saudi Arabia, risk manag healthc policy. Risk Manag Healthcare Policy. 2021;14:4105–4111. doi:10.2147/RMHP.S324938
40. Uchino K, Kolikonda MK, Brown D, et al. Decline in stroke presentations during COVID-19 surge. Stroke. 2020;51(8):2544–2547. doi:10.1161/STROKEAHA.120.030331
41. Mitta N, Sreedharan SE, Sarma SP, Sylaja PN. Women and stroke: different, yet similar. Cerebrovasc Dis Extra. 2021;11(3):106–111. doi:10.1159/000519540
42. Stehman CR, Testo Z, Gershaw RS, Kellogg AR. Burnout, drop out, suicide: physician loss in emergency medicine, part I. West J Emerg Med. 2019;20(3):485–494. doi:10.5811/westjem.2019.4.40970
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
