Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Cost-Effectiveness of Acthar Gel versus Standard of Care for the Treatment of Advanced Symptomatic Sarcoidosis
Authors Bindra J, Chopra I, Hayes K , Niewoehner J, Panaccio M, Wan GJ
Received 1 July 2023
Accepted for publication 27 September 2023
Published 17 October 2023 Volume 2023:15 Pages 739—752
DOI https://doi.org/10.2147/CEOR.S428466
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Samer Hamidi
Jas Bindra,1 Ishveen Chopra,2 Kyle Hayes,3 John Niewoehner,3 Mary Panaccio,3 George J Wan3
1Falcon Research Group, North Potomac, MD, USA; 2Manticore Consultancy, Bethesda, MD, USA; 3Mallinckrodt Pharmaceuticals, Bridgewater, NJ, USA
Correspondence: George J Wan, Mallinckrodt Pharmaceuticals, 440 Route 22 East, Bridgewater, NJ, USA, Email [email protected]
Introduction: Sarcoidosis is a multisystem, inflammatory, systemic granulomatous disease with unknown etiology. Despite the current standard of care (SoC), there is an unmet need for the treatment of advanced symptomatic sarcoidosis. This study assessed the cost-effectiveness of Acthar® Gel (repository corticotropin injection) versus SoC in patients with advanced symptomatic sarcoidosis from the United States (US) payer and societal perspectives over 2 and 3 years.
Methods: A probabilistic cohort-level state-transition approach was used for this cost-effectiveness analysis. Patients were monitored at the end of a 3-month cycle for the attainment of partial or complete response. Patients in the partial, complete, or no-response state were allowed to transition in each of these states at each 3-month cycle. Following the attainment of response, patients could have a durable response or relapse to a no-response state. Patients in a no-response state received treatment and could transition into a response or no-response state based on the probability of treatment success with the respective treatment. Clinical parameters and health utility data were sourced from the Acthar Gel in Participants with Pulmonary Sarcoidosis (PULSAR) trial (NCT03320070) and healthcare utilization, costs, and disutilities were sourced from the published literature. Base case analysis considered a payer perspective over 2 years.
Results: From a payer perspective, Acthar Gel versus SoC results in an incremental cost-effectiveness ratio (ICER) of $134,796 per quality-adjusted life-year (QALY) and $39,179 per QALY over 2 and 3 years, respectively. From a societal perspective, Acthar Gel versus SoC results in an ICER of $117,622 per QALY and $21,967 per QALY over 2 and 3 years, respectively. Sensitivity analysis findings were consistent with the base case.
Conclusion: The results from this cost-effectiveness analysis indicate that Acthar Gel is a cost-effective, value-based treatment option for advanced symptomatic sarcoidosis compared to the SoC from the US payer and societal perspectives.
Keywords: Acthar® Gel, cost-effectiveness analysis, incremental cost-effectiveness ratio, repository corticotropin injection, sarcoidosis, quality-adjusted life-years
Introduction
Sarcoidosis is a chronic granulomatous disease of unknown etiology that primarily affects the lungs (80% to 90% of cases) and may involve multiple organs.1–4 The prevalence of sarcoidosis in the United States (US) is estimated to be 60 per 100,000 adults and over 25,000 patients are diagnosed with sarcoidosis annually.5 Sarcoidosis manifests a broad spectrum of clinical manifestations that vary in severity and impair the patient’s mental and physical functioning.6 Further, sarcoidosis-related disability can result in a considerable economic burden on patients.6,7
Pharmacological treatment is primarily recommended for patients with pulmonary sarcoidosis that may experience progression.8 Treatment goals for advanced pulmonary sarcoidosis are aimed at the reduction of granulomatous inflammation and averting irreversible organ damage while preventing toxicity from medications.8 Oral glucocorticoids are the first-line treatment approved by the US Food and Drug Administration (FDA) for pulmonary sarcoidosis, but persistent glucocorticoid use over the long term is associated with an elevated risk of adverse events and increased healthcare resource burden.9,10 Acthar® Gel (repository corticotropin injection) is another treatment approved by the US FDA for symptomatic sarcoidosis.11 Acthar Gel is a naturally sourced complex mixture of adrenocorticotropic hormone analogs and other pituitary peptides that interacts with all five melanocortin receptors. The therapeutic effects of Acthar Gel in sarcoidosis may thus be attributed to the activation of several potential anti-inflammatory pathways through both glucocorticoid-dependent and independent mechanisms.11 Acthar Gel is referenced in the 2021 European Respiratory Society (ERS) treatment guidelines and the US Sarcoidosis Expert Panel Consensus Statement recommendations as an alternative treatment for patients with sarcoidosis.12,13 ERS treatment guidelines recommend Acthar Gel for sarcoidosis on a case-by-case basis when other therapies are ineffective or not tolerated to reduce the inflammatory burden and prevent organ damage while maintaining low medication toxicity.13 No drugs are currently approved for extrapulmonary sarcoidosis or sarcoidosis-associated pulmonary hypertension.13
Existing literature suggests that Acthar Gel may be a viable treatment option for advanced symptomatic sarcoidosis.14–17 A large case series study utilizing medical records for 302 patients with advanced sarcoidosis found overall status improvement in 95% of patients with a reduction of glucocorticoid use from 61.3% at the initiation of Acthar Gel to 12.9% after 3 months of Acthar Gel use.16 Further, post-hoc analysis of this case series data suggested that Acthar Gel is a better treatment option for patients with more severe disease, mainly those presenting with symptoms.17 In a recent Phase 4 multicenter, randomized, double-blind, placebo-controlled study (Acthar Gel in Participants with Pulmonary Sarcoidosis [PULSAR] trial; NCT03320070), Acthar Gel showed trends of greater improvement compared with placebo and was found to be well tolerated in the double-blind phase of the study in patients with pulmonary sarcoidosis.8 This improvement with Acthar Gel was generally maintained through the open-label extension phase. Further, patients who switched from placebo to Acthar Gel in the open-label phase showed improvements in most efficacy endpoints, and Acthar Gel treatment compared with placebo resulted in more rapid discontinuation of glucocorticoids.8
There is considerable evidence suggesting that Acthar Gel has a favorable clinical profile in symptomatic sarcoidosis; however, no study has examined the economic benefits of Acthar Gel in this patient population. It is important to evaluate interventions integrating data on clinical facets, healthcare resource use and costs, and patient’s quality of life to support decision-making for clinicians and payers. The objective of the current analysis was to estimate the cost-effectiveness of Acthar Gel versus standard of care (SoC) in patients with advanced symptomatic sarcoidosis from the US payer and societal perspectives over 2 and 3 years.
Methods
Model Structure
A cost-effectiveness model was constructed utilizing a probabilistic cohort-level state-transition approach to account for variability in input parameters. The model included clinical response, direct and indirect medical costs, and quality-adjusted life-years (QALYs) to estimate the incremental cost-effectiveness ratio (ICER) of Acthar Gel versus SoC. The time horizon was over 2 and 3 years and both US payer and societal perspectives were considered.
Initially, all patients entered the model cycle 0 in the no-response state and were assumed to initiate treatment (Acthar Gel or SoC). The probability of treatment success with the respective treatment during each treatment cycle was based on the trial.8 Patients were monitored at the end of a 3-month cycle for the attainment of partial or complete response. Patients in the partial, complete, or no-response state were allowed to transition to each of these states at each 3-month cycle. Following the attainment of a partial or complete response, patients could have a durable response or relapse to a no-response state. Patients on Acthar Gel who attained a partial or complete response were assumed to discontinue treatment, and patients on SoC treatment who attained a complete response were assumed to discontinue treatment. Patients on the Acthar Gel were also assumed to be on concomitant SoC treatments; the distribution of patients on SoC was determined based on the data from the PULSAR trial and case series.8,16 Patients in a no-response state received respective treatment and could transition into a response state based on the probability of treatment success. Costs and utilities were calculated for each state every 3 months over a time horizon of 2 and 3 years (Figure 1). The model was built in Microsoft® Excel 2019.
 |
Figure 1 Schematic of the probabilistic cohort-level state-transition model. Note: Response was assessed based on sarcoidosis treatment score. |
This study does not involve any human participants, human data, and/or human material. The data used in this article is sourced from the previously conducted studies. Thus, Institutional Review Board approval was not required for this study.
Model Inputs
Clinical Inputs
The PULSAR trial was the principal evidence source used to derive values for clinical parameters (Table 1).8 In this clinical trial, subjects received subcutaneous 80 units of Acthar Gel twice weekly or 1 mL of matching placebo through 24 weeks in a double-blind treatment phase, followed by an optional 24-week open-label extension. Subjects included in this trial were diagnosed with symptomatic pulmonary sarcoidosis, had a diagnosis of biopsy-confirmed sarcoidosis based on the American Thoracic Society criteria, disease onset ≥1 year before the screening, and a stable prednisone dose of 5–40 mg/d ≥4 weeks before the screening (stable dose for ≥3 months for those treated with any disease-modifying anti-sarcoidosis drugs) before the screening. The primary efficacy endpoint was composite sarcoidosis treatment score (STS), derived from the following measures – pulmonary function tests (percentage predicted forced vital capacity [FVC% predicted] and percentage predicted diffusing capacity of the lungs for carbon monoxide), high-resolution computed tomography and chest x-rays, patient-reported quality of life outcomes (King’s Sarcoidosis Questionnaire [KSQ] and Fatigue Assessment Scale), and extent of steroid tapering. The STS ranges from −6 to +6, with higher scores indicating greater improvement. Complete response was an STS score of ≥+3 points, partial response was an STS score of +2 points or stable disease with glucocorticoid reduction (ie, a total STS score of +1 due to ≥50% reduction in glucocorticoid dosage), and no response was STS score of ≤+1 points with no glucocorticoid taper.8
 |
Table 1 Clinical Parameters Among Patients with Symptomatic Pulmonary Sarcoidosis |
The clinical response data used in the model was derived from the modified intent-to-treat (mITT) population from a double-blind randomized phase of the PULSAR trial.8 The mITT population was defined as patients who received at least one dose of the study drug and contributed any post-baseline efficacy data. The mITT population comprised 55 patients; 27 subjects were randomized to Acthar Gel and 28 subjects were randomized to placebo.8 Transition probabilities varied by type of STS response (partial or complete) and treatment being evaluated. Other clinical inputs included airflow limitation, extrapulmonary organ involvement, pain, and depression.
Airflow limitation was defined as FVC% predicted below 70.18,19 To account for heterogeneity and multisystem facet of sarcoidosis,1–4 extrapulmonary organ involvement was considered in the model; extrapulmonary organs were included if they affected ≥10% of patients and management required medical care beyond pharmacological treatment for sarcoidosis. Based on the PULSAR trial, the distribution of patients was as follows – 25.5% had skin, 10.9% had cardiac, 18.2% had eyes, 23.6% had bones or joints, and 18.2% had liver as an extrapulmonary organ involved.
Pain and depression are common among patients with sarcoidosis and were thus considered in the model to account for disabling effects of these conditions on patients with sarcoidosis.6,20,21 Pain score was calculated based on pain-related items in KSQ, including joint pain, cough pain, chest pain, and eye pain. KSQ scale consists of a score range from 1 to 7 (1 = all of the time, 2 = most of the time, 3 = a good bit of time, 4 = some of the time, 5 = a little of the time, 6 = hardly any of the time, 7 = none of the time); lower score indicates a higher frequency of health problem, referring to increased severity. The score for each of these items was summed and categorized as no pain: 28, mild: 20–27, moderate: 12–19, and severe: 4–11. The depression score was based on the patient’s experience with depression as measured on the steroid toxicity questionnaire; scored on a scale of 0 to 4 (0 = none of the time, 1 = a little, 2 = some of the time, 3 = most of the time, 4 = all of the time); higher score indicates a higher frequency of health problem, referring to increased severity. Based on scoring, patients with depression were categorized as no depression: 0, mild: 1, moderate: 2 to 3, and severe: 4.
Healthcare Resource Utilization and Costs
Costs considered in the present model included treatment costs, direct medical costs, and indirect costs (Table 2).
 |
Table 2 Healthcare Resource Use and Cost Inputs |
Treatment costs included the cost of Acthar Gel as well as concomitant medications (corticosteroids, biologics, antimalarial, and immunosuppressants) for patients on Acthar Gel. Wholesale acquisition (WAC) costs were used for the cost of Acthar Gel. The dose strength and dosing of Acthar Gel were based on dispensing data from specialty pharmacies, from the last 12 months as of March 29, 2019.
The distribution of patients using corticosteroids, biologics, antimalarial, and immunosuppressants was sourced from the PULSAR trial23 and published medical chart review among patients with sarcoidosis.16 For Acthar Gel, a lower proportion of patients were assumed to continue on these medications in the partial response state based on the published literature, where a reduction in medication use was reported for patients 3 months post-Acthar Gel treatment.16 For SoC, no change in the frequency of medication use from no-response to partial response state was assumed. For both Acthar Gel and SoC, patients with complete responses were assumed to discontinue these medications. Information on specific medications used within each class was sourced from the literature.35 Total cost of these medications was calculated based on dosing, dosing strength, and cost per pack; information on dosing24 and cost per pack,25 sourced from literature. The average body weight and body surface area considered for the total dosage calculation were 85.0 Kg and 1.90 m2, respectively. Total costs of corticosteroids also considered corticosteroid utilization based on dosage; intermittent use with <60 days of corticosteroid use, and ≥60 days of corticosteroid use with low (≤7.5 mg/day), medium (>7.5 to ≤15 mg/day), or high (>15 mg/day) dosage.10 Distribution of patients within each of these dosage groups was derived from the PULSAR trial.23
Direct medical costs were sourced from the peer-reviewed published literature. Sarcoidosis-related healthcare costs comprised inpatient, physician office visits, laboratory, outpatient, emergency department, home health, and durable medical equipment-related costs. These costs were sourced from the published literature.5 Healthcare costs were applied to the proportion of patients in each response state with FVC% predicted value below 70. Few patients with pulmonary sarcoidosis develop advanced disease that progresses to respiratory insufficiency despite receiving best-practice pharmacologic interventions; lung transplantation may be the only therapeutic option for such patients to both prolong survival and provide improved quality of life.36 Lung transplant costs were sourced from the published literature26 and applied to patients in each response state with an FVC% predicted value of less than 50. Costs related to extrapulmonary organ involvement were also considered; some of these extrapulmonary organs affected may have more serious implications for patients with advanced and persistent sarcoidosis.37 The extrapulmonary organ-related costs were applied only to patients in a no-response state, assuming that no response results in the progression of sarcoidosis in these extrapulmonary organs. These costs related to progressive organ damage were sourced from the published literature.27–31 Pain-related costs were sourced from the published literature32 and applied to patients in each response state based on pain severity. Symptomatic neuropathic pain treatment in sarcoidosis patients includes the use of prolonged-release opioids.20,38 Costs related to the use of opioids for pain and opioid abuse were sourced from the published literature33 and applied to patients with moderate-to-severe pain; given that long-term use can lead to safety concerns.39 Depression-related costs were sourced from the published literature34 and applied to patients in each response state based on depression severity. Corticosteroids are considered first-line treatment in patients with sarcoidosis; however, prolonged use of corticosteroids can result in considerable toxicity.40,41 Corticosteroid-related toxicity costs were sourced from the published literature.10 Total costs were computed based on the distribution of patients on corticosteroids within each dosage group for each response state.
Further, indirect costs due to the productivity loss for the patients and the additional cost of caregiving were applied in the model from the societal perspective. Disability was assumed for patients with the presence of moderate-to-severe pain, fatigue, or depression. The distribution of patients with a disability was 77.8%, 40.0%, and 25.0% for no response, partial response, and complete response states, respectively. Work-related productivity loss was computed for patients who were employed (41.8%). All estimates were derived from the PULSAR trial.23 For estimating the indirect costs, the model used $4143 as the annual cost for work-related productivity loss in sarcoidosis,42 $4719 for the annual cost of caregiving,43 and $23,925 for the annual cost of work-related training.43 Further, annual costs of $25,003 attributed to substance abuse due to chronic pain were also considered.44 Costs for work-related productivity loss were applied to patients with a disability among the employed population. Costs for disability-related work training were applied to patients with disability among the employed population with respiratory impairment (FVC% predicted below 70). Costs for caregiving were applied to patients with disability and respiratory impairment. Costs for substance abuse were applied to patients with moderate-to-severe pain.
Health Utilities
For the calculation of utilities, quality of life scores from the KSQ from the PULSAR trial23 were mapped to EuroQol five-dimension (EQ-5D), accounting for the disutility based on FVC% predicted (Table 3). KSQ scores mapped to EQ-5D based on the correlation provided in the literature.45,46 FVC% predicted disutilities were sourced from the literature.47 The utilities were applied based on the scores for each patient in the cycle and were additive. Disutilities were applied to the no response state, assuming progressive disease.
 |
Table 3 Health Utilities and Disutilities |
Analyses
The primary outcome was discounted incremental ICER, defined as the difference in total costs divided by the difference in QALYs of Acthar Gel and SoC. The threshold of $150,000 per QALY was selected based on recommendations of the Institute for Clinical and Economic Review and the World Health Organization.58–61 All unit costs were inflated to 2023 US Dollars (USD) utilizing the historical Consumer Price Index for medical care from the US Bureau of Labor Statistics.62 Costs from the ex-US studies on healthcare related costs were adjusted using purchasing power parity exchange rates that account for the different costs of buying a similar basket of goods and services in each country. Costs and QALYs were discounted at 3.0%. The secondary outcome included the cost per STS response.
Base Case Analyses
ICER was evaluated over 2 years from the US payer perspective. The payer perspective comprised treatment and direct medical costs.
Scenario Analyses
ICER was evaluated over 3 years from a payer perspective. Further, ICER was also assessed from a societal perspective over 2 and 3 years. The societal perspective comprised treatment, direct medical, and indirect (caregiving, productivity loss, and work-related training) costs.
Sensitivity Analyses
Sensitivity analyses were conducted for the base case, ie, the time horizon of 2 years from a payer perspective. The values for model inputs and base case assumptions were tested in the one-way deterministic sensitivity analysis (DSA) and multivariable probabilistic sensitivity analysis (PSA). The clinical inputs were varied by ±10% and healthcare utilization and costs were varied by ±25% in the DSA. PSA assessed the joint uncertainty surrounding each parameter in the model by assigning predetermined probabilistic distributions and randomly simulating parameter values from these distributions. The complete range of uncertainty was tested for each variable to account for anticipated uncertainty. The choice of probabilistic distribution for each parameter was based on the nature of the data and its constraints. PSA was performed using 1000 model iterations.
Results
Base Case Analyses
From the payer perspective, Acthar Gel versus SoC results in an ICER of $134,796 per QALY (incremental cost: $65,915; incremental gain in QALY: 0.489) over 2 years (Table 4). Acthar Gel versus SoC had lower direct costs over 2 years (Table 5). The incremental STS response for Acthar Gel versus SoC was 1.728 and incremental cost per STS response was $38,145 over 2 years from the payer perspective.
 |
Table 4 Base Case Results for Incremental Cost-Effectiveness Among Patients with Symptomatic Sarcoidosis (2023 USD) |
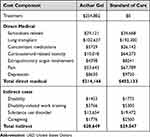 |
Table 5 Base Case per Patient-Year Costs Among Patients with Symptomatic Sarcoidosis Over 2 Years (2023 USD) |
Scenario Analyses
From the payer perspective, Acthar Gel versus SoC results in an ICER of $39,179 over 3 years. From the societal perspective, Acthar Gel versus SoC results in an ICER of $117,622 and $21,967 over 2 years and 3 years, respectively (Table 4). Acthar Gel versus SoC had lower indirect costs over 2 years (Table 5).
The incremental STS response for Acthar Gel versus SoC was 2.726 and the incremental cost per STS response was $10,751 over 3 years from the payer perspective. The incremental cost per STS response for Acthar Gel versus SoC was $33,285 and $6028 over 2 and 3 years, respectively, from the societal perspective.
Sensitivity Analyses
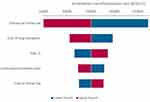
Based on the DSA findings; Acthar Gel is a cost-effective strategy over SoC at a threshold of $150,000 per QALY over 2 years from the payer perspective, consistent with the base case (Figure 2). The efficacy of Acthar Gel, lung transplant cost, the prevalence of pain, the cost related to corticosteroid-related toxicity, and the cost of Acthar Gel are major influencers of the ICER.
Based on the PSA findings, Acthar Gel is cost-effective for 73.9% of the iterations at a willingness-to-pay threshold of $150,000 per QALY over 2 years from a payer perspective, consistent with base case results (Figure 3).
Discussion
Pharmacological treatment for advanced sarcoidosis focuses on the reduction of granulomatous inflammation and averting irreversible organ damage while preventing toxicity from medications.8 Acthar Gel is a safe and effective treatment for symptomatic sarcoidosis.8,14–16 The current cost-effectiveness analysis was conducted to assess the health economics of Acthar Gel versus SoC for the short-term treatment of symptomatic sarcoidosis from both payer and societal perspectives. To the best of our knowledge, this is the first economic evaluation of interventions in sarcoidosis.
The current cost-effectiveness analysis suggests that Acthar Gel is cost-effective compared to SoC at a willingness-to-pay threshold of $150,000 per QALY over 2 years from both payer and societal perspectives. Further, the ICER for Acthar Gel was reduced from 2 to 3 years, resulting from a decrease in medical direct and/or indirect costs with improvement in QALYs compared to SoC. The findings from both DSA and PSA were consistent with the base case. The efficacy of Acthar Gel, lung transplant cost, the prevalence of pain, the cost related to corticosteroid-related toxicity, and the cost of Acthar Gel were key drivers of variation in ICER estimates.
Improved efficacy of Acthar Gel may delay lung damage, thereby reducing cost burden with improvement in patient quality of life. Further, key drivers of ICER appear to be interdependent; improvement in clinical response may improve patient health in general, stabilizing lung function, alleviating pain, and reducing persistent corticosteroid use. The initial high cost of Acthar Gel treatment for sarcoidosis is offset by the reduction in disease progression-related medical costs. Similar findings have been previously shown by Chopra et al (2019), where patients with advanced symptomatic sarcoidosis showed improvement with Acthar Gel; there was a significant reduction in corticosteroid use, and improvement in lung function after Acthar Gel treatment.16 Acthar Gel treatment may be more cost-effective with further rebates and drug price discounts.
This study adds to the nascent literature on economic assessments of interventions in sarcoidosis. This study considered different clinical facets of sarcoidosis, given the heterogeneous nature of the disease.1–4 Extrapulmonary organ involvement was considered to account for the impact on multiple organs. In addition, pain and depression related to sarcoidosis were considered in the model. Patients experience a broad spectrum of clinical manifestations of varying severity that impair both mental and physical functioning.6 Sarcoidosis is a chronic inflammatory illness and small-fiber neuropathy is one of the disabling and often chronic manifestations of the disease that presents with peripheral pain.20 The characteristic pain experience can be burning or shooting.20 Treatments are aimed to reduce pain; however, total pain relief is rarely achieved. Another disabling aspect of sarcoidosis is heightened degrees of anxiety and depression among these patients, which further contribute to costs.21
The current analysis also assessed the cost-effectiveness of Acthar Gel from the societal perspective as sarcoidosis impairs a patient’s mental and physical functioning,6 thereby limiting daily functioning.63 Sarcoidosis primarily affects adults during their prime working and family years; this may negatively impact productivity or life roles.63 Patients with even modest impairment of pulmonary function may have impaired maximal oxygen consumption.63 Organ impairment in sarcoidosis is another factor for functional impairment.63 Together, these factors may further add to the economic burden for the patient as well as their caregivers. The current cost-effectiveness analysis considered costs related to increased disability, lost productivity, and increased caregiver burden. In the current analysis, Acthar Gel was shown to be a cost-effective strategy compared to SoC over 2 and 3 years from the societal perspective at a willingness-to-pay threshold of $150,000 per QALY.
The cost of an intervention is an important consideration for access and affordability; however, the value of intervention should consider clinical, economic, and quality of life components. Interventions that are considered high “Care Value” are within the ICER range of $100,000–$150,000 and are primarily intended for a special population or for interventions that offer substantial other benefits.58–61 The ICER threshold range is estimated to be three times the nation’s per capita income based on the World Health Organization’s recommendations.60 Acthar Gel incurs additional costs but also results in a gain in QALYs compared to SoC over the short term. This information has policy implications for evaluation of interventions that improve patient’s health and lives. Costs to payers, patients, and society are central to decision-making to ensure appropriate economic planning. However, interventions that are expensive but offer benefits to patient’s health and quality of life over other treatment options, specifically for a vulnerable patient population should be assessed fairly in economic decision-making. Sarcoidosis mainly affects the lungs along with multiple organs being involved1–4 and patients are commonly prescribed glucocorticoids that result in long-term toxicity with persistent use.9,10 Together, these adversely affect patients' health and quality of life as well as incur a burden for caregivers. Based on the current analysis, Acthar Gel results in additional QALYs, thereby improving patients’ quality of life which is an important consideration for advanced symptomatic sarcoidosis. Understanding the impact of Acthar Gel on patient’s quality of life will serve as a guide for improved patient access. Acthar Gel may be a value-based option for patients with advanced symptomatic sarcoidosis at a willingness-to-pay threshold of $150,000 per QALY. It is anticipated that capturing the full impact of sarcoidosis in terms of healthcare expenses and patient well-being may further enhance the value of Acthar Gel. Further, studies assessing the costs and benefits of sarcoidosis treatment strategies may provide an evidence base for payers and other healthcare decision-makers in making recommendations for tailoring treatments to specific patient populations based on the severity of the condition.
The findings of this cost-effectiveness analysis should be interpreted taking into account the following limitations. First, clinical, SoC medication use, and health utility data were derived from the PULSAR clinical trial, which may not reflect real-world clinical practice. Further, the PULSAR clinical trial had a small sample size and may have introduced bias to the findings. However, this uncertainty was tested in both DSA and PSA. Second, a simplified care paradigm was applied for the model which may not capture the complexity of sarcoidosis. The exact magnitude of sarcoidosis is not well quantified in literature making it challenging to reliably assess the influence of sarcoidosis on health and health care. Third, clinical response was based on composite STS, which is based on different components; this measure has its strengths and limitations and thus might result in variation in cost-effectiveness estimates. Fourth, PULSAR examined outcomes at 24 weeks in the randomized phase; the model extrapolated data to assess the cost-effectiveness over 2 and 3 years, which might result in under or over-estimation of the effectiveness of Acthar Gel. Lastly, the healthcare utilization, costs, and health disutility were sourced from published literature and may result in under or over-estimation of results. However, uncertainty in the parameters was accounted for by conducting a sensitivity analysis.
Conclusions
Acthar Gel is a cost-effective, value-based treatment option for appropriate patients with advanced symptomatic sarcoidosis at a willingness-to-pay threshold of $150,000 over 2 and 3 years from the US payer and societal perspectives. Further research is required to examine the long-term clinical effectiveness and cost-effectiveness of Acthar Gel for advanced symptomatic sarcoidosis.
Author Contributions
All authors made a significant contribution to the work reported, including study conception, design, execution, acquisition of data, analysis, and interpretation, and in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was sponsored by Mallinckrodt Pharmaceuticals.
Disclosure
JB is an employee of Falcon Research Group. IC was a research collaborator for the duration of this study and has no disclosures. GJW, KH, and JN are employees at Mallinckrodt Pharmaceuticals. MP is a consultant providing services on behalf of Mallinckrodt Pharmaceuticals. The authors report no other conflicts of interest in this work.
References
1. Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ERS Executive Committee, February 1999. Am J Respir Crit Care Med. 1999;160(2):736–755. doi:10.1164/ajrccm.160.2.ats4-99
2. Valeyre D, Prasse A, Nunes H, Uzunhan Y, Brillet PY, Muller-Quernheim J. Sarcoidosis. Lancet. 2014;383(9923):1155–1167. doi:10.1016/S0140-6736(13)60680-7
3. Soto-Gomez N, Peters JI, Nambiar AM. Diagnosis and management of sarcoidosis. Am Fam Physician. 2016;93(10):840–848.
4. Wu JJ, Schiff KR. Sarcoidosis. Am Fam Physician. 2004;70(2):312–322.
5. Baughman RP, Field S, Costabel U, et al. Sarcoidosis in America. Analysis based on health care use. Ann Am Thorac Soc. 2016;13(8):1244–1252. doi:10.1513/AnnalsATS.201511-760OC
6. Sharp M, Eakin MN, Drent M. Socioeconomic determinants and disparities in sarcoidosis. Curr Opin Pulm Med. 2020;26(5):568–573. doi:10.1097/MCP.0000000000000704
7. Patel N, Kalra R, Doshi R, et al. Hospitalization rates, prevalence of cardiovascular manifestations, and outcomes associated with sarcoidosis in the United States. J Am Heart Assoc. 2018;7(2). doi:10.1161/JAHA.117.007844
8. Mirsaeidi M, Baughman RP, Sahoo D, Tarau E. Results from a phase 4, multicenter, randomized, double-blind, placebo-controlled study of repository corticotropin injection for the treatment of pulmonary sarcoidosis. Pulm Ther. 2023;9:1–17. doi:10.1007/s41030-022-00213-9
9. Rice JB, White AG, Johnson M, et al. Quantitative characterization of the relationship between levels of extended corticosteroid use and related adverse events in a US population. Curr Med Res Opin. 2018;34(8):1519–1527. doi:10.1080/03007995.2018.1474090
10. Rice JB, White AG, Johnson M, et al. Healthcare resource use and cost associated with varying dosages of extended corticosteroid exposure in a US population. J Med Econ. 2018;21(9):846–852. doi:10.1080/13696998.2018.1474750
11. Mallinckrodt Pharmaceuticals. Acthar® Gel prescribing information; 1952. https://www.acthar.com/pdf/Acthar-PI.pdf.
12. Rahaghi FF, Baughman RP, Saketkoo LA, et al. Delphi consensus recommendations for a treatment algorithm in pulmonary sarcoidosis. Eur Respir Rev. 2020;29(155):190146. doi:10.1183/16000617.0146-2019
13. Baughman RP, Valeyre D, Korsten P, et al. ERS clinical practice guidelines on treatment of sarcoidosis. Eur Respir J. 2021;58:2004079. doi:10.1183/13993003.04079-2020
14. Baughman RP, Sweiss N, Keijsers R, et al. Repository corticotropin for chronic pulmonary sarcoidosis. Lung. 2017;195(3):313–322. doi:10.1007/s00408-017-9994-4
15. Baughman RP, Barney JB, O’Hare L, Lower EE. A retrospective pilot study examining the use of Acthar gel in sarcoidosis patients. Respir Med. 2016;110:66–72. doi:10.1016/j.rmed.2015.11.007
16. Chopra I, Qin Y, Kranyak J, et al. Repository corticotropin injection in patients with advanced symptomatic sarcoidosis: retrospective analysis of medical records. Ther Adv Respir Dis. 2019;13:1753466619888127. doi:10.1177/1753466619888127
17. Bindra J, Chopra I, Hayes K, Niewoehner J, Panaccio MP, Wan GJ. Understanding predictors of response to repository corticotropin injection treatment among patients with advanced symptomatic sarcoidosis. J Health Econ Outcomes Res. 2022;9(1):90–100. doi:10.36469/jheor.2022.33295
18. Quanjer PH, Pretto JJ, Brazzale DJ, Boros PW. Grading the severity of airways obstruction: new wine in new bottles. Eur Respir J. 2014;43(2):505–512. doi:10.1183/09031936.00086313
19. Barreiro TJ, Perillo I. An approach to interpreting spirometry. Am Fam Physician. 2004;69(5):1107–1114.
20. Heij L, Dahan A, Hoitsma E. Sarcoidosis and pain caused by small-fiber neuropathy. Pain Res Treat. 2012;2012:256024. doi:10.1155/2012/256024
21. Hinz A, Brahler E, Mode R, Wirtz H, Bosse-Henck A. Anxiety and depression in sarcoidosis: the influence of age, gender, affected organs, concomitant diseases and dyspnea. Sarcoidosis Vasc Diffuse Lung Dis. 2012;29(2):139–146.
22. IBM. IBM Micromedex RED BOOK. IBM; 2021.
23. Mallinckrodt Pharmaceuticals. Data on File: Acthar Gel in Participants With Pulmonary Sarcoidosis (PULSAR); 2023.
24. El Jammal T, Jamilloux Y, Gerfaud-Valentin M, Valeyre D, Seve P. Refractory Sarcoidosis: a Review. Ther Clin Risk Manag. 2020;16:323–345. doi:10.2147/TCRM.S192922
25. Drugs.com. Drugs & Medications A to Z; 2023. Available from: https://www.drugs.com/.
26. Peel JK, Keshavjee S, Krahn M, Sander B. Economic evaluations and costing studies of lung transplantation: a scoping review. J Heart Lung Transplant. 2021;40(12):1625–1640. doi:10.1016/j.healun.2021.08.007
27. Tripathi R, Knusel KD, Ezaldein HH, Honaker JS, Bordeaux JS, Scott JF. Incremental health care expenditure of chronic cutaneous ulcers in the United States. JAMA Dermatol. 2019;155(6):694–699. doi:10.1001/jamadermatol.2018.5942
28. Foy AJ, Mandrola JM. Heavy heart: the economic burden of heart disease in the United States now and in the future. Prim Care. 2018;45(1):17–24. doi:10.1016/j.pop.2017.11.002
29. Rein DB, Zhang P, Wirth KE, et al. The economic burden of major adult visual disorders in the United States. Arch Ophthalmol. 2006;124(12):1754–1760. doi:10.1001/archopht.124.12.1754
30. Williams SA, Chastek B, Sundquist K, et al. Economic burden of osteoporotic fractures in US managed care enrollees. Am J Manag Care. 2020;26(5):e142–e149.
31. Nguyen MH, Burak Ozbay A, Liou I, et al. Healthcare resource utilization and costs by disease severity in an insured national sample of US patients with chronic hepatitis B. J Hepatol. 2019;70(1):24–32. doi:10.1016/j.jhep.2018.09.021
32. Lalonde L, Choiniere M, Martin E, Berbiche D, Perreault S, Lussier D. Costs of moderate to severe chronic pain in primary care patients - a study of the ACCORD Program. J Pain Res. 2014;7:389–403. doi:10.2147/JPR.S55388
33. White AG, Birnbaum HG, Mareva MN, et al. Direct costs of opioid abuse in an insured population in the United States. J Manag Care Pharm. 2005;11(6):469–479. doi:10.18553/jmcp.2005.11.6.469
34. Chow W, Doane MJ, Sheehan J, Alphs L, Le H. Economic burden among patients with major depressive disorder: an analysis of healthcare resource use, work productivity, and direct and indirect costs by depression severity. Am J Manag Care. 2019;16:e188–96.
35. Foundation for Sarcoidosis Research. Commonly Prescribed Sarcoidosis Medications; 2019. Available from: https://www.stopsarcoidosis.org/commonly-prescribed-sarcoidosis-medications/.
36. Meyer KC. Lung transplantation for pulmonary sarcoidosis. Sarcoidosis Vasc Diffuse Lung Dis. 2019;36(2):92–107. doi:10.36141/svdld.v36i2.7163
37. Rao DA, Dellaripa PF. Extrapulmonary manifestations of sarcoidosis. Rheum Dis Clin North Am. 2013;39(2):277–297. doi:10.1016/j.rdc.2013.02.007
38. Foundation for Sarcoidosis Research. Opioid epidemic impacts patients suffering from orphan disease of sarcoidosis; 2017. Available from: https://www.stopsarcoidosis.org/press-release-opioid-epidemic/.
39. Harned M, Sloan P. Safety concerns with long-term opioid use. Expert Opin Drug Saf. 2016;15(7):955–962. doi:10.1080/14740338.2016.1177509
40. Khan NA, Donatelli CV, Tonelli AR, et al. Toxicity risk from glucocorticoids in sarcoidosis patients. Respir Med. 2017;132:9–14. doi:10.1016/j.rmed.2017.09.003
41. Entrop JP, Kullberg S, Grunewald J, Eklund A, Brismar K, Arkema EV. Type 2 diabetes risk in sarcoidosis patients untreated and treated with corticosteroids. ERJ Open Res. 2021;7(2). doi:10.1183/23120541.00028-2021
42. Rice JB, White A, Lopez A, et al. Economic burden of sarcoidosis in a commercially-insured population in the United States. J Med Econ. 2017;20(10):1048–1055. doi:10.1080/13696998.2017.1351371
43. Birnbaum HG, Ivanova JI, Samuels S, et al. Economic impact of multiple sclerosis disease-modifying drugs in an employed population: direct and indirect costs. Curr Med Res Opin. 2009;25(4):869–877. doi:10.1185/03007990902743869
44. Luo F, Li M, Florence C. State-level economic costs of opioid use disorder and fatal opioid overdose - United States, 2017. MMWR Morb Mortal Wkly Rep. 2021;70(15):541–546. doi:10.15585/mmwr.mm7015a1
45. Patel AS, Siegert RJ, Creamer D, et al. The development and validation of the king’s sarcoidosis questionnaire for the assessment of health status. Thorax. 2013;68(1):57–65. doi:10.1136/thoraxjnl-2012-201962
46. Atkins CP, Jones AP, Wilson AM. A comparison of measurements of health-related quality of life in patients with sarcoidosis. Thorax. 2018;73(Supple 4):A189.
47. Dempsey TM, Thao V, Moriarty JP, Borah BJ, Limper AH. Cost-effectiveness of the anti-fibrotics for the treatment of idiopathic pulmonary fibrosis in the United States. BMC Pulm Med. 2022;22(1):18. doi:10.1186/s12890-021-01811-0
48. Anyanwu AC, McGuire A, Rogers CA, Murday AJ. Assessment of quality of life in lung transplantation using a simple generic tool. Thorax. 2001;56(3):218–222. doi:10.1136/thorax.56.3.218
49. Chen SC, Bayoumi AM, Soon SL, et al. A catalog of dermatology utilities: a measure of the burden of skin diseases. J Investig Dermatol Symp Proc. 2004;9(2):160–168. doi:10.1046/j.1087-0024.2003.09112.x
50. Di Tanna GL, Urbich M, Wirtz HS, et al. Health state utilities of patients with heart failure: a systematic literature review. Pharmacoeconomics. 2021;39(2):211–229. doi:10.1007/s40273-020-00984-6
51. Brown MM, Brown GC, Brown HC, Peet J, Roth Z. Value-based medicine, comparative effectiveness, and cost-effectiveness analysis of topical cyclosporine for the treatment of dry eye syndrome. Arch Ophthalmol. 2009;127(2):146–152. doi:10.1001/archophthalmol.2008.608
52. Tormalehto S, Mononen ME, Aarnio E, Arokoski JPA, Korhonen RK, Martikainen J. Health-related quality of life in relation to symptomatic and radiographic definitions of knee osteoarthritis: data from Osteoarthritis Initiative (OAI) 4-year follow-up study. Health Qual Life Outcomes. 2018;16(1):154. doi:10.1186/s12955-018-0979-7
53. Dan AA, Kallman JB, Srivastava R, Younoszai Z, Kim A, Younossi ZM. Impact of chronic liver disease and cirrhosis on health utilities using SF-6D and the health utility index. Liver Transpl. 2008;14(3):321–326. doi:10.1002/lt.21376
54. Institute for Clinical and Economic Review. Biologic therapies for treatment of asthma associated with type 2 inflammation: effectiveness, value, and value-based price benchmarks; 2018. Available from: https://icer.org/wp-content/uploads/2020/10/ICER_Asthma-Final-Report_Unredacted_08122020.pdf#page=75.
55. Institute for Clinical and Economic Review. Extended-release opioid agonists and antagonist medications for addiction treatment (MAT) in patients with opioid use disorder: effectiveness and value; 2018. Available from: https://icer.org/wp-content/uploads/2020/10/ICER_OUD_Final_Evidence_Report_120318.pdf.
56. Wetherington S, Delong L, Kini S, et al. Pain quality of life as measured by utilities. Pain Med. 2014;15(5):865–870. doi:10.1111/pme.12405
57. Kolovos S, Bosmans JE, van Dongen JM, et al. Utility scores for different health states related to depression: individual participant data analysis. Qual Life Res. 2017;26(7):1649–1658. doi:10.1007/s11136-017-1536-2
58. Dubois RW. Cost-effectiveness thresholds in the USA: are they coming? Are they already here? J Comp Eff Res. 2016;5(1):9–11. doi:10.2217/cer.15.50
59. Institute for Clinical and Economic Review. 2020-2023 value assessment framework; 2020.
60. Thokala P, Ochalek J, Leech AA, Tong T. Cost-effectiveness thresholds: the past, the present and the future. Pharmacoeconomics. 2018;36(5):509–522. doi:10.1007/s40273-017-0606-1
61. Tzanetakos C, Gourzoulidis G. Does a standard cost-effectiveness threshold exist? The Case of Greece. Value Health Reg Issues. 2023;36:18–26. doi:10.1016/j.vhri.2023.02.006
62. United States Bureau of Labor Statistics. Consumer price index - medical care; 2022. Available from: https://www.bls.gov/cpi/data.htm.
63. Gerke AK, Judson MA, Cozier YC, Culver DA, Koth LL. Disease burden and variability in sarcoidosis. Ann Am Thorac Soc. 2017;14(Supplement_6):S421–S428. doi:10.1513/AnnalsATS.201707-564OT
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.