Back to Journals » Therapeutics and Clinical Risk Management » Volume 18
Correlations Between Coronary Artery Disease, Coronary Artery Calcium Score, and Lipoprotein(a) Level in Korea
Authors Kim J , Choi SW , Lee YS , Lee JM, Chung H, Woo JS, Kim WS, Choi YY, Kim W
Received 12 May 2022
Accepted for publication 20 August 2022
Published 1 October 2022 Volume 2022:18 Pages 981—987
DOI https://doi.org/10.2147/TCRM.S374372
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Garry Walsh
Joan Kim,1 Seung Woo Choi,1 Young Shin Lee,1 Jung Myung Lee,1 Hyemoon Chung,1 Jong Shin Woo,1 Woo-Shik Kim,1 Yun Young Choi,2 Weon Kim1
1Department of Cardiology, Kyung Hee University Hospital, Seoul, Korea; 2Department of Medicine, Graduate School, Kyung Hee University, Seoul, Korea
Correspondence: Weon Kim, Tel +82 2 958 8176, Email [email protected]
Background: Lipoprotein(a) (Lp(a)) levels are associated with coronary artery disease (CAD) and aortic valve calcification. This study aimed to determine the correlation between Lp(a) levels and coronary artery calcium (CAC) scores in patients who underwent coronary computed tomography angiography (CCTA).
Methods: This was a single-center observational study. The patients had not been previously diagnosed with CAD and underwent CCTA and Lp(a) measurement in a three-month timeframe. Coronary angiography and further management were performed according to the physician’s decision. Of the 252 patients, 81 and 171 patients underwent coronary revascularization and received medical treatment only, respectively. To examine the relationship between Lp(a) and CAC score and between Lp(a) and CAD, we divided the patients by Lp(a) level (50 mg/dL) and CAC score (400).
Results: No relationship was observed between Lp(a) and CAD or other risk factors for CAD. There were no differences in the ratio of patients who underwent coronary revascularization or in the CAC score according to an Lp(a) level of 50 mg/dL. There was no difference in Lp(a) level at a CAC score of 400. The proportion of patients who underwent coronary revascularization was high in the high CAC score group (50.6% vs 23.7%, p = 0.000). No association was observed between Lp(a) level and CAC score in the Spearman correlation (0.000, p < 0.998).
Conclusion: Correlations between Lp(a) level and CAC score and between Lp(a) and CAD were not observed in this Korean cohort study. However, a high CAC score was correlated with coronary revascularization.
Keywords: lipoprotein(a), coronary calcium score, coronary artery disease
Introduction
Lipoprotein(a) (Lp(a)) is a particle that is structurally similar to low-density lipoprotein cholesterol (LDL) and contains apolipoprotein(a) bound to apolipoprotein B100 via a disulfide bond.1 Some studies have suggested that high concentrations of plasma Lp(a) are associated with a high risk of aortic valve stenosis2 and coronary artery disease (CAD).3,4 There are several hypotheses regarding the pathophysiology of Lp(a). Similar to LDL, Lp(a) can be pro-atherogenic because excess Lp(a) is deposited into the subendothelial arterial space and oxidized.5 In addition, Lp(a) can be prothrombotic because the structure of apolipoprotein(a) is similar to plasminogen and may compete with plasminogen, thus leading to interference with the fibrinolytic system.6
However, the relationships between Lp(a) and CAC, and between Lp(a) and CAD, are very complex and have not yet been precisely established. Many studies have shown different relationships between Lp(a) levels and CAD, particularly with regard to race.7 For example, according to Virani et al, the Lp(a) levels of Black subjects were higher than those of white subjects, and had a stronger positive correlation with cardiovascular disease events compared to that observed in white subject.8 In contrast, a large prospective cohort study in China (n = 3884) found that plasma Lp(a) levels were not strongly associated with CAD, death, or stroke.11 In addition, various studies have found different correlations of Lp(a) with coronary artery calcification. In a community-based study, sex-specific associations between Lp(a) and coronary artery calcium (CAC) score were supported,12 and another study reported that Lp(a) was strongly associated with high CAC score in women with type 2 diabetes mellitus (DM).13 Meanwhile, some studies reported negative results.10,14
The purpose of this study was to determine the correlation between Lp(a) level and CAC score in Korean patients, and to determine the relationship between Lp(a) and CAD.
Materials and Methods
Study Participants
This was a single-center, cross-sectional, observational study. The patients consisted of 252 individuals who visited Kyung Hee University Hospital from March 2020 to February 2021 for the evaluation of chest pain, CAD risk evaluation for non-cardiac surgery, stroke, or healthcare examination. Among the visitors for healthcare examination, those who had cardiac hypertrophy on CXR or high CAC score (>400) or significant stenosis on coronary computed tomography angiography (CCTA) were included. The patients underwent CCTA and an Lp(a) test in a three-month timeframe. They had not previously been diagnosed with CAD (defined as myocardial infarction (MI), coronary revascularization, angiographic significant stenosis, or positive stress test), and were 27 to 89 years old. Of the 252 eligible patients, 81 patients underwent coronary revascularization and 171 received medical treatment only. Coronary angiography was performed according to the physician’s decision. Coronary revascularization was performed on lesions with stenosis greater than 70% and/or FFR <0.8. Coronary revascularization was not performed on lesions clinically judged to be impossible for PCI or those for which it was thought that intervention would not be beneficial (eg, distal lesions or too-small vessels).
The exclusion criterion was a history of coronary disease.
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Kyung Hee University Hospital (protocol code: KHUH 2021-10-077).
Clinical and Laboratory Values
Information on the age, sex, DM, hypertension (HTN), prior stroke history, smoking, and alcohol consumption of the patients was obtained from their medical records. Body mass index was obtained by dividing weight (kg) by the square of height (m2). The creatinine, glucose, total cholesterol, triglyceride, high-density lipoprotein cholesterol, LDLcholesterol, and high-sensitivity C-reactive protein concentrations were measured using an AU-5800 Chemistry Analyzer (Beckman Coulter Inc., Brea, CA, USA). The Lp(a) level was measured by an immunoturbidimetry technique calibrated with the IFCC reference material, using the same analyzer. HbA1c was measured using an automated Glycohemoglobin Analyzer HLC-723G8 (Tosoh G8; Tosoh Bioscience, Inc., Japan).
Computed Tomography Scans
Computed tomography (CT) scans were performed with a 128-slice scanner (Ingenuity CT cor 128, Philips Medical Systems, Cleveland, OH, USA), and the standard scanning parameters were 64 mm × 0.625 mm section collimation, 400 ms rotation time, 120 kV tube voltage, and 39.5 mAs (395 mA × 0.1 s) tube current under ECG-gated dose modulation. The Agatston score was calculated using standard calcium scoring.
Statistical Analysis
Statistical analyses of the data were performed using SPSS (version 22.0; IBM Corp., Armonk, NY, USA). Data are reported as mean ± standard deviation for continuous variables and as proportions for categorical variables. The Spearman correlation statistical method was used to analyze the correlations between Lp(a) and the risk factors of CAD and between Lp(a) and CAC score. Student’s t-tests and chi-square tests were used to compare the coronary intervention group and medical management only group, the low and high Lp(a) groups, and the low and high CAC groups.
Results
Baseline Participant Characteristics
Table 1 shows a summary of the baseline characteristics. The mean age was 68.2 years, and 58.7% of the patients were male. The mean CAC score was 478.4, and the Lp(a) level was 24.8 mg/dL. The number of patients who underwent coronary intervention was 81 (32%).
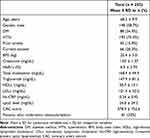 |
Table 1 Baseline Participant Characteristics |
Evaluation of anginal chest pain was the most common reason for CCTA (n = 161, 64%). Following this, the other reasons for examination were risk evaluation of non-cardiac surgery (n = 50, 19.8%), coronary evaluation of patients with stroke (n = 26, 10.3%), and healthcare examination (n = 15, 5.9%).
Associations Between Lp(a) and CAD and Various CAD Risk Factors
Spearman correlations did not reveal any associations between Lp(a) and other lipid, metabolic, or inflammatory parameters. The analysis was also conducted by dividing the patients into the medical treatment only and coronary revascularization groups. However, the results were almost the same between the two groups (Table 2).
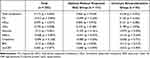 |
Table 2 Spearman Correlations of Lipid, Metabolic, and Inflammatory Parameters with Plasma Lp(a) Levels |
As many studies suggest that Lp(a) levels above 50 mg/dL be designated as abnormal,9 we divided the patients into two groups according to an Lp(a) level of 50 mg/dL to determine the differences between the two groups. There was no difference between the two patient groups with regard to the lipid, metabolic, or inflammatory parameters. In addition, there were no significant differences in the number of patients who underwent coronary intervention (69 (31.1%) vs 12 (40.0%), p = 0.326) or the CAC scores (474.2 ± 744.3 vs 509.8 ± 824.2, p = 0.808) between the two groups (Table 3).
 |
Table 3 Lipid, Metabolic, and Inflammatory Parameters; CAC Score; and Number of Patients Who Underwent Coronary Revascularization According to Lp(a) Level |
Associations Between Lp(a) Level and CAC Score
Figure 1 shows biased distributions of Lp(a) level and CAC score. All patients were divided into two groups according to a calcium score of 400, which is a level generally considered to have prognostic value.10,11 There was no significant difference in the Lp(a) level between the two groups (25.4 ± 26.0 vs 23.6 ± 20.0, p = 0.601). However, the mean age of the high CAC score group was higher than that of the low CAC score group (70.9 ± 8.9 vs 67.0 ± 10.1, p = 0.003), the proportion of men was higher (49 (62.0%) vs 65 (37.6%), p = 0.004) in the high CAC score group, and the ratio of patients who had HTN was higher (68 (86.1%) vs 122 (70.5%), p = 0.008) in the high CAC score group. The number of patients who underwent coronary intervention was higher in the high CAC score group (40 (50.6%) vs 41 (23.7%), p = 0.000) (Table 4).
 |
Table 4 Lipid, Metabolic, and Inflammatory Parameters; Lp(a) Level; and Number of Patients Who Underwent Coronary Revascularization According to CAC Score |
The correlation between Lp(a) and CAC score could not be observed in all patients by using the Spearman correlation (Spearman correlation: 0.053, p = 0.403). The results were the same in the group receiving medical therapy only (Spearman correlation: 0.057, p = 0.46) and in the coronary intervention group (Spearman correlation: 0.002, p = 0.986).
Discussion
Lp(a) is found in atherosclerotic plaques and is associated with vascular smooth muscle proliferation and endothelial cell damage.12 In a recent large-scale study targeting multi-ethnic participants, Lp(a) was related to CAD independently of CAC score.13 However, other studies suggest that the relationship between Lp(a) and CAD may appear differently depending on age, sex, race, and comorbidities.7,14–16 The results of our study showed no strong relationship between Lp(a) and CAD in a Korean cohort, and this finding can be explained by the results of previous studies.
In our study, no correlation was found between Lp(a) and CAC scores. There are two recent studies on the correlation between Lp(a) and CAC in Korea. The study of Chung et al showed that in asymptomatic male patients over 45 years of age, the level of Lp(a) was significantly higher for patients with CAC scores greater than 0 than the Lp(a) level of patients with CAC scores of 0 (16.74 ± 20.53 vs 13.97 ± 16.10, p = 0.006).18 Sung et al19 also demonstrated a positive correlation between Lp(a) level and CAC score in a large cohort in Korea. However, unlike our study, these two studies were conducted on asymptomatic health check-up patients, and the cut-off of the patients’ CAC scores was much lower than that in our study (0 vs 400). In general, CAC score indicates the burden of atherosclerosis in the coronary artery,17 and the general cutoff for increasing CAD risk has been identified as approximately 350–400; therefore, it can be said that these studies showed correlation between preclinical atherosclerosis and Lp(a). By contrast, our study divided patients on the basis of a CAC of 400, and the clinical significance of our study is the comparison of the differences of the actual clinical outcome, that is, whether a coronary revascularization was performed.
The number of patients included in the present study was only 252, and this small sample size was a disadvantage of this study. Nevertheless, the results clearly indicate relationships between CAD and other well-known risk factors for CAD (eg, CAC score, age, gender, and HTN). This suggests that the patients in this study sufficiently reflect the characteristics of the general population. Another disadvantage of this study was the heterogeneity of the patients. However, the included patients mostly had angina, high coronary risk in the preoperative evaluation, or stroke. Only 5.9% of patients underwent CT scans for health check examination and these patients had risk for CAD (eg, cardiac hypertrophy, high CAC score, and/or significant stenosis on CCTA). Therefore, most of the subjects were at high risk of coronary disease. This is supported by the fact that the average CAC score of the patients in this study was 478.4, which is quite high.
In this cross-sectional study, the analysis was conducted by dividing the patients into one group that received the intervention and a second group that did not. All patients who received the intervention were stable angina patients, and patients with acute coronary syndrome were not included. Therefore, follow-up cohort studies on endpoints such as survival rate, MI, and stroke are necessary in future. In addition, as the level of Lp(a) in the blood is largely determined by the gene, in future studies, it is necessary to conduct Lp(a) genetic study, such as Apo(a) size polymorphism or SNP analysis, on Korean cohort and compare the results with those of large-scale international studies.20,21
In conclusion, significant correlations between Lp(a) level and CAC score and between Lp(a) and CAD were not observed in this Korean cohort study. However, a high CAC score was significantly correlated with coronary revascularization.
Data Sharing Statement
The data are not publicly available because data export was not approved by the Institutional Review Board. The data presented in this study are available on request from the Institutional Review Board.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Kyung Hee University Hospital (protocol code: KHUH 2021-10-077 and date of approval: 2021.11.01).
Informed Consent Statement
Patient consent was waived because this study is a RETROSPECTIVE study; consent waiver was approved by the Institutional Review Board.
Funding
This work was supported by the National Research Foundation of Korea (NRF), funded by the Ministry of Education (2020R1F1A1076495).
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Utermann G. The mysteries of lipoprotein(a). Science. 1989;246(4932):904–910. doi:10.1126/science.2530631
2. Thanassoulis G, Campbell CY, Owens DS, et al. Genetic associations with valvular calcification and aortic stenosis. N Engl J Med. 2013;368(6):503–512. doi:10.1056/NEJMoa1109034
3. Kamstrup PR, Tybjærg-Hansen A, Nordestgaard BG. Elevated lipoprotein(a) and risk of aortic valve stenosis in the general population. J Am Coll Cardiol. 2014;63(5):470–477. doi:10.1016/j.jacc.2013.09.038
4. Nordestgaard BG, Langsted A. Lipoprotein (a) as a cause of cardiovascular disease: insights from epidemiology, genetics, and biology. J Lipid Res. 2016;57(11):1953–1975. doi:10.1194/jlr.R071233
5. Nielsen LB. Atherogenecity of lipoprotein(a) and oxidized low density lipoprotein: insight from in vivo studies of arterial wall influx, degradation and efflux. Atherosclerosis. 1999;143(2):229–243. doi:10.1016/S0021-9150(99)00064-7
6. Berglund L, Ramakrishnan R. Lipoprotein(a): an elusive cardiovascular risk factor. Arterioscler Thromb Vasc Biol. 2004;24(12):2219–2226. doi:10.1161/01.ATV.0000144010.55563.63
7. Sharrett AR, Ballantyne CM, Coady SA, et al. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2001;104(10):1108–1113. doi:10.1161/hc3501.095214
8. Virani SS, Brautbar A, Davis BC, et al. Associations between lipoprotein(a) levels and cardiovascular outcomes in black and white subjects: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2012;125(2):241–249. doi:10.1161/CIRCULATIONAHA.111.045120
9. Nordestgaard BG, Chapman MJ, Ray K, et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur Heart J. 2010;31(23):2844–2853. doi:10.1093/eurheartj/ehq386
10. Torngren K, Rylance R, Björk J, et al. Association of coronary calcium score with endothelial dysfunction and arterial stiffness. Atherosclerosis. 2020;313:70–75. doi:10.1016/j.atherosclerosis.2020.09.022
11. Lo-Kioeng-Shioe MS, Rijlaarsdam-Hermsen D, van Domburg RT, et al. Prognostic value of coronary artery calcium score in symptomatic individuals: a meta-analysis of 34,000 subjects. Int J Cardiol. 2020;299:56–62. doi:10.1016/j.ijcard.2019.06.003
12. Cambillau M, Simon A, Amar J, et al. Serum Lp(a) as a discriminant marker of early atherosclerotic plaque at three extracoronary sites in hypercholesterolemic men. The PCVMETRA Group. Arterioscler Thromb. 1992;12(11):1346–1352. doi:10.1161/01.ATV.12.11.1346
13. Mehta A, Vasquez N, Ayers CR, et al. Independent association of lipoprotein(a) and coronary artery calcification with atherosclerotic cardiovascular risk. J Am Coll Cardiol. 2022;79(8):757–768. doi:10.1016/j.jacc.2021.11.058
14. Shai I, Schulze MB, Manson JE, et al. A prospective study of lipoprotein(a) and risk of coronary heart disease among women with type 2 diabetes. Diabetologia. 2005;48(8):1469–1476. doi:10.1007/s00125-005-1814-3
15. Frohlich J, Dobiásová M, Adler L, et al. Gender differences in plasma levels of lipoprotein (a) in patients with angiographically proven coronary artery disease. Physiol Res. 2004;53(5):481–486.
16. Qasim AN, Martin SS, Mehta NN, et al. Lipoprotein(a) is strongly associated with coronary artery calcification in type-2 diabetic women. Int J Cardiol. 2011;150(1):17–21. doi:10.1016/j.ijcard.2010.02.021
17. Burge MR, Eaton RP, Schade DS. The role of a coronary artery calcium scan in type 1 diabetes. Diabetes Technol Ther. 2016;18(9):594–603. doi:10.1089/dia.2016.0110
18. Chung YH, Lee B-K, Kwon HM, et al. Coronary calcification is associated with elevated serum lipoprotein (a) levels in asymptomatic men over the age of 45 years: a cross-sectional study of the Korean national health checkup data. Medicine. 2021;100(9):e24962. doi:10.1097/MD.0000000000024962
19. Sung KC, Wild SH, Byrne CD. Lipoprotein (a), metabolic syndrome and coronary calcium score in a large occupational cohort. Nutr Metab Cardiovasc Dis. 2013;23(12):1239–1246. doi:10.1016/j.numecd.2013.02.009
20. Enas A, Varkey B, Dharmarajan TS, et al. Lipoprotein(a): an independent, genetic, and causal factor for cardiovascular disease and acute myocardial infarction. Indian Heart J. 2019;71(2):99–112. doi:10.1016/j.ihj.2019.03.004
21. Nathan O. Coding variation in ANGPTL4, LPL, and SVEP1 and the risk of coronary disease. N Engl J Med. 2016;374(12):1134–1144.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

