Back to Journals » Clinical Ophthalmology » Volume 18
Correlation of Ocular Biometry with Axial Length in Elderly Japanese
Authors Tanaka T, Nishitsuka K , Obata H
Received 22 October 2023
Accepted for publication 26 January 2024
Published 3 February 2024 Volume 2024:18 Pages 351—360
DOI https://doi.org/10.2147/OPTH.S446031
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Takahiro Tanaka, Koichi Nishitsuka, Hiroto Obata
Department of Ophthalmology, Saitama Medical Center, Saitama Medical University, Kawagoe-shi, Saitama, Japan
Correspondence: Koichi Nishitsuka, Department of Ophthalmology, Saitama Medical Center, Saitama Medical University, 1981 Kamoda, Kawagoe-shi, Saitama, Japan, Tel +81-49-228-3682, Fax +81-49-225-5722, Email [email protected]
Purpose: Ocular parameters are not only useful for diagnosing diseases but also for guiding treatment approaches. A lot of previous studies have reported ocular parameters and its relations before cataract surgery. However, despite ethnic differences in ocular biometry, few reports have dealt with Japanese. Hence, this retrospective cross-sectional study aimed to measure parameters of preoperative cataract patients and examines the correlations between each parameter in Japanese elderly people.
Patients and Methods: The 210 subjects had their ocular axial lengths measured with OA-2000. The endpoints were ocular axial length (AL), central corneal thickness (CCT), average anterior corneal radius of curvature (CR), white-to-white (WTW), anterior chamber depth (ACD), and lens thickness (LT). Our analyses utilized the eye with the longer AL in each person. Each parameter was analyzed for correlations in a round-robin manner. Regression analyses were performed on parameters correlated with AL.
Results: The parameters correlated with AL were CR (r = 0.33, P < 0.0001), WTW (r = 0.29, P < 0.0001), ACD (r = 0.59, P < 0.0001), and LT (r = − 0.30, P < 0.0001). These parameters related to AL in all simple regression equations (CR (P < 0.0001), WTW (P = 0.0002), ACD (P < 0.0001), LT (P = 0.0001)). In multiple regression analyses, CR, ACD, and LT might relate to AL (CR (P = 0.0002), ACD (P < 0.0001), LT (P = 0.018)). LT tended to be thinner as AL increased, while CR, WTW, and ACD tended to increase.
Conclusion: This information may be useful in developing strategies for ophthalmic surgery, as it provides information on the location of intraocular tissues. Various parameters have been used in intraocular lens (IOL) power calculations in recent years and knowledge of the interrelationship among parameters may be useful in determining IOL power according to ethnicity in the future.
Keywords: preoperative cataract patients, central corneal thickness, average anterior corneal radius of curvature, white-to-white, anterior chamber depth, lens thickness
Introduction
Originally, ocular biometry required the use of multiple instruments such as ultrasound, or laser for measuring ocular axial length (AL), anterior chamber depth (ACD), and lens thickness (LT), autorefractometers for refractive power, and pachymeters for corneal thickness. Each parameter had to be measured separately using different instruments. However, in recent years, the OA-2000 (TOMEY Corporation, Nagoya, Japan) and IOL Master 700 (Carl Zeiss Meditec AG, Jena, Germany) based on Swept-source optical coherence tomography (SS-OCT) have been developed. These instruments allow for the measurement of multiple parameters without the need for multiple instruments.
Measurement of parameters can provide valuable insights into various diseases. For instance, thin corneal thickness has been associated with open-angle glaucoma,1 while a shallow anterior chamber is significantly related to angle-closure glaucoma.2 Moreover, long-axial eyes have been found to have thinned choroid and sclera.3,4 Parameters are not only useful for diagnosing diseases but also for guiding treatment approaches. For example, knowledge of LT is essential in developing strategies for cataract surgery. Additionally, when inserting instruments into the anterior chamber, it is important to consider the positional relationship between the cornea, iris, and lens to avoid damaging ocular tissues.
OA-2000 offers the advantage of simultaneously measuring multiple parameters within seconds using the SS-OCT method. This eliminates the need for multiple devices and reduces the burden on patients during testing. The use of a single method also ensures consistency in measurement techniques and reduces the potential for systematic errors.
Although there have been a lot of previous ocular biometric studies dealing with correlations between AL and various parameters, there have been no reports from Japan dealing with multiple ocular parameters simultaneously using a single machine. Papers reported from Japan in the past, to the best of our knowledge, have been concerned with the distribution of ocular biometry5,6 and its correlation with age.7 It has been reported that there are ethnic differences in ocular parameters,1,8–11 and the correlations between parameters in Japanese may help us understand the characteristics of the Japanese eye shape. In this study, OA-2000 was utilized to comprehensively measure parameters in preoperative cataract patients and investigated the correlations between each parameter in Japanese elderly people.
Methods
This study was conducted as a retrospective cross-sectional review. The subjects were 210 patients who visited our outpatient department from April 1, 2018 to March 31, 2020 and had their AL measured before cataract surgery. OA-2000 (TOMEY Corporation, Nagoya, Japan) was used for AL measurement. The measurement method was done with nonmydriasis. The measurement was completely automatic. No manual modifications were made. The study focused on six parameters: AL, central corneal thickness (CCT), average anterior corneal radius of curvature (CR), transverse corneal diameter known as white-to-white (WTW), ACD, and LT. All these parameters were measurable, and the longer AL was mainly employed for each person. Signal-to-noise ratio (SNR) value over 2.1 was used as a criterion for adoption.12
The statistical analysis methods were as follows. First, a Spearman’s rank correlation coefficient test was conducted to analyze the correlation of each parameter in a round-robin manner. Second, simple regression analyses were performed on the parameters correlated with AL, with AL as the objective variable and each parameter as the explanatory variable. Finally, multiple regression analyses were conducted between AL and the selected parameters, with AL as the objective variable and the appropriate parameters as the explanatory variables.
All analyses were performed using JMP Pro version 16 (SAS Institute Inc., Cary, NC, USA). The statistical significance level was < 0.05. This study was conducted in accordance with the Declaration of Helsinki and received approval from the Ethics Committee of Saitama Medical University (approval number: 2414). The consent of the subjects was obtained in an opt-out format. The need for informed consent was waived by the Ethics Committee of Saitama Medical University because of the retrospective nature of the study. Confidentiality of each patient’s personal information obtained in this study was ensured so that it would not be leaked to third parties.
Results
Correlation Analyses
Table 1 shows the overall mean values. Table 2 presents the correlation results between AL and each parameter. Parameters correlated with AL were CR (r = 0.33, P < 0.0001), WTW (r = 0.29, P < 0.0001), ACD (r = 0.59, P < 0.0001), and LT (r = −0.30, P < 0.0001). Weak positive correlations were observed between AL and CR, AL and WTW, and a positive correlation between AL and ACD. A weak negative correlation was found between AL and LT. No correlation was found between AL and CCT (r = 0.12, P = 0.095). Other significant correlations included CR and WTW (r = 0.43, P < 0.0001), WTW and ACD (r = 0.22, P = 0.0017), and ACD and LT (r = −0.72, P < 0.0001). The present study identified the strongest negative correlation between ACD and LT.
 |
Table 1 Overall Means, Maximum and Minimum Values, and Coefficient of Variations |
 |
Table 2 Correlation Coefficients Between Each Parameter |
Simple Regression Analyses
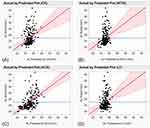
Simple regression analyses were performed on CR, WTW, ACD, and LT that were correlated with AL. Table 3 shows the results of simple regression analyses, and Figure 1 shows the results of plotting predicted AL and actual AL values. The parameters possibly related to AL in all simple regression equations (CR (P < 0.0001), WTW (P = 0.0002), ACD (P < 0.0001), LT (P = 0.0001)). However, all had low coefficients of determination (CR (R2 = 0.092), WTW (R2 = 0.063), ACD (R2 = 0.27), and LT (R2 = 0.067)). Based on the plots of predicted AL and actual AL values, it is difficult to predict AL for either parameter (Figure 1). Thus, none of the simple regression equations hold.
 |
Table 3 Simple and Multiple Regression Analyses |
Multiple Regression Analyses
Multiple regression analyses were performed by selecting parameters. Table 3 shows multiple regression analyses, while Figure 2 illustrates the results of plotting predicted AL and actual AL values.
First, multiple regression analysis was performed on all parameters (Multiple Regression Analysis No.1). CCT and WTW had no effect on AL (CCT (P = 0.073), WTW (P = 0.25)).
Second, a multiple regression analysis was also performed, excluding CCT and WTW (Multiple Regression Analysis No.2). CR, ACD, and LT may have related to AL (CR (P = 0.0002), ACD (P < 0.0001), LT (P = 0.018)). The coefficient of determination adjusted for degrees of freedom was low (Adjusted R2 = 0.33). However, upon examining the plots of predicted AL and actual AL values (Figure 2), a slight linear relationship between the two variables can be observed. Hence, this multiple regression equation may explain some trends.
Discussion
Although correlations between AL and parameters have been reported in the past, few studies have reported all of these parameters simultaneously (Table 4). Yin et al13 reported correlations for the same parameters as ours. The study differed from ours in that it found a significant relationship between AL and CCT. The other correlation coefficients are significant as in the present study, but the values are slightly different. Ocular geometry may differ slightly even among the same Asian population.
 |
Table 4 A Sampling of Previous Studies Dealing with Correlation Analyses Between AL and Parameters, Including Parameters Similar to Those in the Present Study |
In our simple regression analyses, AL was influenced by CR, WTW, ACD, LT. Similar findings have been reported in previous studies (CR,13 WTW,13,18 ACD,13,18,27 and LT13). However, except for the study by Yin et al13 almost all of these parameters have not been examined together. In these studies, the same parameters as in our study were measured using a single machine. Additionally, Yin et al13 and Nangia et al27 have reported that CCT was associated with AL, but the steepness of regression line in each study was small. Therefore, the effect of CCT on AL seems to be small.
The relationship between AL and CCT was investigated by Shimmyo et al35 (R2 = 0.00728) and Chen et al31 (R2 = 0.0028). However, similar to the current results, there were no significant correlations found between AL and CCT. Recent studies with correlation analyses reported significant but low correlations between AL and CCT.13–15,19,20,27,30,31,34,35 Therefore, it is believed that AL does not vary with changes in CCT.
There have been some reports on correlation analysis of significant negative relationship between AL and corneal power.18,27,30,33 Furthermore, multiple studies with correlation analyses have reported significant positive correlations between AL and CR.13,20,26,37 Considering these facts, the increase in CR associated with AL elongation is thought to result in corneal flattening and decrease corneal power.
In relation to the relationship between AL and WTW, Park et al30 (R2 = 0.0786) reported similar findings to the present study. As AL increases, WTW also increases. Similarly, Jivrajka et al33 (R2 = 0.1792) reported a similar relationship between AL and ACD. As AL increases, ACD seems to increase as well. Previous studies with correlation analyses showed significant positive correlations between AL and WTW,13–15,17,18,22,25,28–30 and between AL and ACD.13–15,17,18,21–31,33,36,37 However, Wei et al38 reported that there is no linear increasing relationship between AL and WTW, with WTW reaching its maximum at ALs of 24.5 to 26 mm and gradually decreasing. Therefore, the present result on the association between AL and WTW may not necessarily apply in all cases.
The relationship between AL and LT was discussed in Jivrajka et al33 (R2 = 0.0321), which made a similar report. Previous studies with correlation analyses pointed out several significant negative correlations between the two,13,14,16,17,22,27,32,33,36,37 suggesting that LT becomes thinner as AL increases. However, Meng et al39 reported no linear decreasing relationship between AL and LT. According to their report, LT deceased with increasing AL in normal and moderate myopic eyes, while it conversely increased in the other AL groups. Therefore, the present result on the association between AL and LT may not also apply in all cases.
Our multiple regression analysis revealed that CR, ACD, and LT were significant parameters for predicting AL. Previous studies conducted multiple regression analyses with AL as the dependent variable, but the overlapping parameters with our study were different. Specifically, Yin et al13 included CCT, CR, ACD, and LT as significant parameters; Nangia et al27 included ACD and LT; and Park et al30 included ACD. The explanatory variables used in each study were different. However, all reports included ACD, suggesting that it is the parameter most closely related to AL. Additionally, among these studies, only Park et al30 used multiple instruments to measure the same parameters as we did.
Since studies of Yin et al13 and Nangia et al27 did not mention R2, we did not know how well the regression equation could predict AL. Park et al30 obtained a much higher coefficient of determination with age, spherical equivalent of refractive error, corneal curvature (diopter), ACD, and retinal nerve fiber layer (RNFL) thickness as explanatory variables (R2 = 0.918). From this point of view, AL cannot be predicted with a high probability using only the data obtained from OA-2000 as in our study.
We would like to share useful information in clinical practice from these results. There is something that should be considered during cataract surgery for the long-axial eye. Since WTW increases as AL increases, it is difficult to give a guideline for the size of continuous curvilinear capsulorhexis (CCC) with WTW. To accurately determine the size of CCC, a CCC marker should be used. Since ACD deepens with AL elongation, it should be noted that the lens is in a deeper position in the long-axial eye. In addition, since the lens is thinner in the long-axial eye, we must be aware of posterior capsule rupture during cataract surgery. In situations where it is not possible to measure all parameters, this information is also useful in developing surgical strategies because it provides information about the location of intraocular tissues.
We would like to mention the possibility that this study may be related to the determination of intraocular lens (IOL) power in the future. The conventional IOL power calculation formulas, represented by the Sanders-Retzlaff-Kraff/Theoretical (SRK/T) formula,40 have been based on preoperative AL, corneal power, and expected postoperative anterior chamber depth (effective lens position). Recently, with the introduction of the Barrett Universal II formula,41 IOL power calculations are now based on AL, corneal power, and ACD (LT and WTW are optional). More recently, the Hill-Radial Basis Function (Hill-RBF) method42 and the Kane formula43 using artificial intelligence have been introduced. Hill-RBF method outputs IOL power considering subject’s parameters, relying on the large training dataset of AL, corneal power, ACD, and postoperative spherical equivalent power (details unknown). The Kane formula adds gender to AL, corneal power, and ACD, and optionally considers LT and CCT to obtain IOL power. IOL formulas have transitioned from an era in which only AL and corneal power were considered as parameters to an era in which a variety of parameters are considered to determine IOL power. Further development of parameter research such as ours may lead to the selection of the optimal IOL power for each ethnic group.
This report is based on data derived from a single machine. It does not consider age, gender, stature, weight, refractive power, and social life circumstances (eg, medical history, educational background, and frequency of reading books), as reported in previous reports.5,7,13,14,18,21,25–27,29,44–46 In addition, unlike previous reports,5,6,15,17,38,39 we did not perform our analyses stratified by each axial length. Therefore, it is possible that good results were not obtained. Moreover, since our hospital is a medical institution that handles difficult cases, there may be a selection bias.
Conclusion
In summary, LT tended to be thinner as AL increased, while CR, WTW, and ACD tended to increase. These findings not only provide an opportunity to notice points to be considered in cataract surgery in cases of the long-axial eye, but also may lead to determination of IOL power for each ethnic group with awareness of the relationship between parameters in the future.
Abbreviations
AL, ocular axial length; CCT, central corneal thickness; CR, average anterior corneal radius of curvature; WTW, white-to-white; ACD, anterior chamber depth; LT, lens thickness.
Data Sharing Statement
The datasets that support the findings of this current study are available from the corresponding author on reasonable request.
Additional Information
Correspondence and requests for materials should be addressed to K.N.
Acknowledgments
We are indebted to Dr. Atsushi Yamasaki for scientific advice. He belongs to Hakuai Hospital, Yonago-shi, Tottori, Japan, and was a professor of ophthalmology at Saitama Medical Center, Saitama Medical University. We would like to thank Mrs. Ayako Marubayashi for research assistance. She is a certified orthoptist at Saitama Medical Center. We would like to thank enago by Crimson Interactive Japan Co., Ltd., Chiyoda-ku, Tokyo, Japan, for their proofreading services.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
Prof. Koichi Nishitsuka reports personal fees from Santen Medical, Senju Medical, Otsuka Medical, Kowa Medical, Alcon, HOYA medical, and Chugai Medical, outside the submitted work. The authors declare no other competing interests in this work.
References
1. Aghaian E, Choe JE, Lin S, Stamper RL. Central corneal thickness of Caucasians, Chinese, Hispanics, Filipinos, African Americans, and Japanese in a glaucoma clinic. Ophthalmology. 2004;111(12):2211–2219. doi:10.1016/j.ophtha.2004.06.013
2. Xu L, Cao WF, Wang YX, Chen CX, Jonas JB. Anterior chamber depth and chamber angle and their associations with ocular and general parameters: the Beijing Eye Study. Am J Ophthalmol. 2008;145(5):929–936. doi:10.1016/j.ajo.2008.01.004
3. Funata M, Tokoro T. Scleral change in experimentally myopic monkeys. Graefes Arch Clin Exp Ophthalmol. 1990;228(2):174–179. doi:10.1007/BF00935729
4. Phillips JR, McBrien NA. Form deprivation myopia: elastic properties of sclera. Ophthalmic Physiol Opt. 1995;15(5):357–362.
5. Nakao SY, Miyake M, Hosoda Y, et al. Myopia Prevalence and Ocular Biometry Features in a General Japanese Population: the Nagahama Study. Ophthalmology. 2021;128(4):522–531. doi:10.1016/j.ophtha.2020.08.023
6. Kamiya K, Hayashi K, Tanabe M, et al. Nationwide multicentre comparison of preoperative biometry and predictability of cataract surgery in Japan. Br J Ophthalmol. 2022;106(9):1227–1234. doi:10.1136/bjophthalmol-2021-318825
7. Kawamorita T, Uozato H, Oshika T, et al. Evaluation of ocular biometry in the Japanese population using a multicenter approach: prospective observational study. PLoS One. 2022;17(7):e0271814. doi:10.1371/journal.pone.0271814
8. Tong L, Saw SM, Siak JK, Gazzard G, Tan D. Corneal thickness determination and correlates in Singaporean schoolchildren. Invest Ophthalmol Vis Sci. 2004;45(11):4004–4009. doi:10.1167/iovs.04-0121
9. Casson RJ. Anterior chamber depth and primary angle-closure glaucoma: an evolutionary perspective. Clin Exp Ophthalmol. 2008;36(1):70–77. doi:10.1111/j.1442-9071.2008.01672.x
10. Gaurisankar ZS, van Rijn GA, Lima JEE, et al. Correlations between ocular biometrics and refractive error: a systematic review and meta-analysis. Acta Ophthalmol. 2019;97(8):735–743. doi:10.1111/aos.14208
11. Meng W, Butterworth J, Malecaze F, Calvas P. Axial length of myopia: a review of current research. Ophthalmologica. 2011;225(3):127–134. doi:10.1159/000317072
12. Olsen T, Thorwest M. Calibration of axial length measurements with the Zeiss IOLMaster. J Cataract Refract Surg. 2005;31(7):1345–1350. doi:10.1016/j.jcrs.2004.12.066
13. Yin G, Wang YX, Zheng ZY, et al. Ocular axial length and its associations in Chinese: the Beijing Eye Study. PLoS One. 2012;7(8):e43172. doi:10.1371/journal.pone.0043172
14. Kim S, Oh R, Kim MK, Yoon CH. SS-OCT-based ocular biometry in an adult Korean population with cataract. J Cataract Refract Surg. 2023;49(5):453–459. doi:10.1097/j.jcrs.0000000000001135
15. Miao A, Tang Y, Zhu X, Qian D, Zheng T, Lu Y. Associations between anterior segment biometry and high axial myopia in 3438 cataractous eyes in the Chinese population. BMC Ophthalmol. 2022;22(1):71. doi:10.1186/s12886-022-02300-6
16. Feng X, Wang Y, Liang J, Xu Y, Ortega-Usobiaga J, Cao D. Analysis of Lens Thickness Distribution Based on Swept-Source Optical Coherence Tomography (SS-OCT). J Ophthalmol. 2021;2021:4717996. doi:10.1155/2021/4717996
17. Lei Q, Tu H, Feng X, Ortega-Usobiaga J, Cao D, Wang Y. Distribution of ocular biometric parameters and optimal model of anterior chamber depth regression in 28,709 adult cataract patients in China using swept-source optical biometry. BMC Ophthalmol. 2021;21(1):178. doi:10.1186/s12886-021-01932-4
18. Natung T, Shullai W, Nongrum B, Thangkhiew L, Baruah P, Phiamphu ML. Ocular biometry characteristics and corneal astigmatisms in cataract surgery candidates at a tertiary care center in North-East India. Indian J Ophthalmol. 2019;67(9):1417–1423. doi:10.4103/ijo.IJO_1353_18
19. Hashmani N, Hashmani S, Murad A, Asghar N, Islam M. Effect of Demographic Variables on the Regional Corneal Pachymetry. Asia Pac J Ophthalmol. 2019;8(4):324–329. doi:10.1097/APO.0000000000000252
20. Muthu Krishnan V, Jayalatha K, Vijayakumar C. Correlation of Central Corneal Thickness and Keratometry with Refraction and Axial Length: a Prospective Analytic Study. Cureus. 2019;11(1):e3917. doi:10.7759/cureus.3917
21. Huang Q, Huang Y, Luo Q, Fan W. Ocular biometric characteristics of cataract patients in western China. BMC Ophthalmol. 2018;18(1):99. doi:10.1186/s12886-018-0770-x
22. Ferreira TB, Hoffer KJ, Ribeiro F, Ribeiro P, O’Neill JG. Ocular biometric measurements in cataract surgery candidates in Portugal. PLoS One. 2017;12(10):e0184837. doi:10.1371/journal.pone.0184837
23. Chen H, Lin H, Lin Z, Chen J, Chen W. Distribution of axial length, anterior chamber depth, and corneal curvature in an aged population in South China. BMC Ophthalmol. 2016;16(1):47. doi:10.1186/s12886-016-0221-5
24. Fernández-Vigo JI, Fernández-Vigo J, Macarro-Merino A, Fernández-Pérez C, Martínez-de-la-Casa JM, García-Feijoó J. Determinants of anterior chamber depth in a large Caucasian population and agreement between intra-ocular lens Master and Pentacam measurements of this variable. Acta Ophthalmol. 2016;94(2):e150–5. doi:10.1111/aos.12824
25. Cui Y, Meng Q, Guo H, et al. Biometry and corneal astigmatism in cataract surgery candidates from Southern China. J Cataract Refract Surg. 2014;40(10):1661–1669. doi:10.1016/j.jcrs.2014.01.039
26. Pan CW, Wong TY, Chang L, et al. Ocular biometry in an urban Indian population: the Singapore Indian Eye Study (SINDI). Invest Ophthalmol Vis Sci. 2011;52(9):6636–6642. doi:10.1167/iovs.10-7148
27. Nangia V, Jonas JB, Sinha A, Matin A, Kulkarni M, Panda-Jonas S. Ocular axial length and its associations in an adult population of central rural India: the Central India Eye and Medical Study. Ophthalmology. 2010;117(7):1360–1366. doi:10.1016/j.ophtha.2009.11.040
28. Hoffmann PC, Hütz WW. Analysis of biometry and prevalence data for corneal astigmatism in 23,239 eyes. J Cataract Refract Surg. 2010;36(9):1479–1485. doi:10.1016/j.jcrs.2010.02.025
29. Fotedar R, Wang JJ, Burlutsky G, et al. Distribution of axial length and ocular biometry measured using partial coherence laser interferometry (IOL Master) in an older white population. Ophthalmology. 2010;117(3):417–423. doi:10.1016/j.ophtha.2009.07.028
30. Park SH, Park KH, Kim JM, Choi CY. Relation between axial length and ocular parameters. Ophthalmologica. 2010;224(3):188–193. doi:10.1159/000252982
31. Chen MJ, Liu YT, Tsai CC, Chen YC, Chou CK, Lee SM. Relationship between central corneal thickness, refractive error, corneal curvature, anterior chamber depth and axial length. J Chin Med Assoc. 2009;72(3):133–137. doi:10.1016/S1726-4901(09)70038-3
32. Praveen MR, Vasavada AR, Shah SK, et al. Lens thickness of Indian eyes: impact of isolated lens opacity, age, axial length, and influence on anterior chamber depth. Eye. 2009;23(7):1542–1548. doi:10.1038/eye.2008.315
33. Jivrajka R, Shammas MC, Boenzi T, Swearingen M, Shammas HJ. Variability of axial length, anterior chamber depth, and lens thickness in the cataractous eye. J Cataract Refract Surg. 2008;34(2):289–294. doi:10.1016/j.jcrs.2007.10.015
34. Oliveira C, Tello C, Liebmann J, Ritch R. Central corneal thickness is not related to anterior scleral thickness or axial length. J Glaucoma. 2006;15(3):190–194. doi:10.1097/01.ijg.0000212220.42675.c5
35. Shimmyo M, Orloff PN. Corneal thickness and axial length. Am J Ophthalmol. 2005;139(3):553–554. doi:10.1016/j.ajo.2004.08.061
36. Osuobeni EP. Ocular components values and their intercorrelations in Saudi Arabians. Ophthalmic Physiol Opt. 1999;19(6):489–497. doi:10.1046/j.1475-1313.1999.00453.x
37. Carney LG, Mainstone JC, Henderson BA. Corneal topography and myopia. A cross-sectional study. Invest Ophthalmol Vis Sci. 1997;38(2):311–320.
38. Wei L, He W, Meng J, Qian D, Lu Y, Zhu X. Evaluation of the White-to-White Distance in 39,986 Chinese Cataractous Eyes. Invest Ophthalmol Vis Sci. 2021;62(1):7. doi:10.1167/iovs.62.1.7
39. Meng J, Wei L, He W, Qi J, Lu Y, Zhu X. Lens thickness and associated ocular biometric factors among cataract patients in Shanghai. Eye Vis. 2021;8(1):22. doi:10.1186/s40662-021-00245-3
40. Retzlaff JA, Sanders DR, Kraff MC. Development of the SRK/T intraocular lens implant power calculation formula. J Cataract Refract Surg. 1990;16(3):333–340. doi:10.1016/s0886-3350(13)80705-5
41. Barrett GD. An improved universal theoretical formula for intraocular lens power prediction. J Cataract Refract Surg. 1993;19(6):713–720. doi:10.1016/s0886-3350(13)80339-2
42. Hill WE IOL Power Selection by Pattern Recognition. Presented at ASCRS EyeWorld Corporate Education, New Orleans, Louisiana; 2016. Available from: https://www.youtube.com/watch?v=Evtd_0Qnh1o.
43. Melles RB, Kane JX, Olsen T, Chang WJ. Update on Intraocular Lens Calculation Formulas. Ophthalmology. 2019;126(9):1334–1335. doi:10.1016/j.ophtha.2019.04.011
44. Lim LS, Saw SM, Jeganathan VS, et al. Distribution and determinants of ocular biometric parameters in an Asian population: the Singapore Malay eye study. Invest Ophthalmol Vis Sci. 2010;51(1):103–109. doi:10.1167/iovs.09-3553
45. Namba H, Sugano A, Murakami T, et al. Ten-year longitudinal investigation of astigmatism: the Yamagata Study (Funagata). PLoS One. 2022;17(1):e0261324. doi:10.1371/journal.pone.0261324
46. Sng CC, Foo LL, Cheng CY, et al. Determinants of anterior chamber depth: the Singapore Chinese Eye Study. Ophthalmology. 2012;119(6):1143–1150. doi:10.1016/j.ophtha.2012.01.011
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.