Back to Journals » Neuropsychiatric Disease and Treatment » Volume 18
Correlation Between Refractory Laryngopharyngeal Reflux Disease and Symptoms of Anxiety and Depression
Authors Huang F, Liao Q, Gan X, Wen W
Received 17 November 2021
Accepted for publication 18 March 2022
Published 26 April 2022 Volume 2022:18 Pages 925—932
DOI https://doi.org/10.2147/NDT.S349933
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Fengling Huang, Qiu Liao, Xingkun Gan, Wensheng Wen
Department of Otolaryngology, Head and Neck Surgery, The First Affiliated Hospital of Guangxi Medical University, Nanning, Guangxi, 530000, People’s Republic of China
Correspondence: Wensheng Wen, Department of Otolaryngology, Head and Neck Surgery, The First Affiliated Hospital of Guangxi Medical University, Shuangyong Road, No. 6, Nanning, Guangxi, 530000, People’s Republic of China, Tel +86 0771-53556511, Email [email protected]
Background and Study Aims: The occurrence, development, and prognosis of refractory laryngopharyngeal reflux disease (LPRD) may be related to anxiety and depression. Our study aims to investigate anxiety and depressive symptoms in LPRD and clarify the correlations among them.
Patients and Methods: Twenty-eight patients were diagnosed with LPRD and subsequently referred to the Department of Mental Health for treatment. The patients were divided into the Self-rating Anxiety Scale (SAS)/Self-rating Depression Scale (SDS) positive group (+) and the SAS/SDS negative group (−). All patients were treated (oral administration) with a standard dose of proton pump inhibitor (PPI, omeprazole 20 mg bid) plus one tablet of Deanxit (flupentixol-melitracen) after breakfast. Treatment efficacy was evaluated after one month of drug treatment. The therapeutic effect of PPI treatment alone was compared with that treated with PPI + Deanxit.
Results: Among 28 patients with refractory LPRD, the main reflux symptoms and signs were specific. There were differences in gender distribution and age distribution among the 28 patients with refractory LPRD, and there were 17 patients (60.7%) in the SAS/SDS (+) group and 11 patients in the SAS/SDS (−) group (39.3%). Regarding efficacy evaluation after one month of PPI + Deanxit treatment, the differences in indices before and after treatment were statistically significant (all p< 0.05).
Conclusion: Anxiety and depressive symptoms influence the occurrence, development, and treatment efficacy of refractory LPRD. Attention to and targeted treatment of anxiety and depressive symptoms can help improve the treatment outcomes of patients with refractory LPRD.
Keywords: refractory, laryngopharyngeal reflux, anxiety, depression
Introduction
Laryngopharyngeal reflux (LPR) refers to the phenomenon of stomach contents flowing back to areas above the upper esophageal sphincter (including the nasal cavity, mouth, pharynx, larynx, trachea, and lungs).1 Laryngopharyngeal reflux disease (LPRD) is a common diagnosis in outpatient otolaryngology clinics, and its incidence increases year by year. Domestic and foreign attention to and research on LPRD is also increasing.2 However, the pathogenesis of LPRD remains unclear, as it is a disease with multiple etiological factors.3
Development throughout the modern era has also promoted a fast-paced lifestyle. People face more challenges and pressure and have gradually recognized the physiological-psychological-social disease mode in the understanding of diseases. When LPRD cannot be controlled for a long period, namely, when symptoms do not exhibit obvious remission after proton pump inhibitor (PPI) treatment for 2 months or longer, psychological disorders are common sequelae. Generally, anxiety and depressive symptoms are frequent. In addition, patients with LPRD are likely to present chest distress, dizziness, and other physical-discomfort symptoms without organic pathological changes on cardiovascular and cerebrovascular examinations.
Therefore, this study aims to investigate the relationship between refractory LPRD, anxiety and depressive symptoms, and autonomic nerve dysfunction.
Patients and Methods
General Information
Twenty-eight patients diagnosed with suspected LPRD at the Department of Otolaryngology at our hospital via the reflux symptom index (RSI), and a reflux symptom rating scale (reflux finding score, RFS) from March 2009 to September 2019 were randomly selected. The inclusion criteria were as follows: between 20 and 65 years of age, either gender, education level of elementary school and above, and able to complete forms to provide relevant information. Through an examination by the same senior chief physician of our department, patients were diagnosed with LPRD when they presented typical manifestations of pharyngeal foreign body sensation, persistent clearing of the throat combined with clinical manifestations and RSI scores and/or reflux symptom rating scale scores (RFS) indicative of LPRD. Furthermore, after treatment with a PPI (omeprazole 20 mg bid), as prescribed by doctors in our hospital or other hospitals, for at least two months, the patients felt no significant symptom relief. The exclusion criteria were as follows: recent occurrence of a neck mass or malignant tumor of the throat revealed by electronic laryngoscopy; a history of neck and throat surgery; the presence of serious underlying diseases such as brain diseases or congenital mental disorders, heart disease, and abdominal diseases, especially stomach disease; and difficulty completing and cooperating for the relevant examinations.
Data Description and Statistics
General information regarding all subjects, including name, gender, age, RSI value, and RFS, was collected and entered into a computer to establish a database. RSI≥13 and/or RFS≥7 was considered LPRD. After evaluations by the same senior chief physician in the Department of Otorhinolaryngology Head and Neck Surgery at our hospital, patients were treated with omeprazole (20 mg bid for 4 weeks), after which the efficacy was evaluated again via the RSI and RFS. Patients for whom the RSI value and RFS did not significantly decrease were diagnosed with refractory LPRD. The 28 patients who met the diagnostic criteria were all referred to the Department of Mental Health. Through specialists in the mental health department, the Self-rating Anxiety Scale (SAS), the Self-rating Depression Scale (SDS), and a 90-item symptom check list (SCL-90) were used to assess whether refractory LPRD was related to anxiety and depression. For the SAS, a total score ≥50 indicated an anxiety state (mild: 50≤SAS≤60, moderate: 61≤SAS≤70; severe: SAS≥70), and a total SDS score of ≥53 indicated a depressed state (mild state: 53≤SDS≤62, moderate: 63≤SDS≤72; severe: SDS≥72) (standard total score = original score * 1.25; with the result being an integer). In addition to the standard dose of the PPI omeprazole (20 mg bid), all 28 patients were treated with Deanxit (1 tablet qd orally after breakfast) for the treatment of psychological anxiety and depressive symptoms. After one month of treatment with medication, patients returned to the hospital for a follow-up visit. Efficacy was assessed by the same senior chief physician through clinical manifestations and pre- and post-RSI and RFS values.
Results
Analysis of Gender and Age
Among the 28 patients with refractory LPRD, there were 9 male patients (32.1%), including 5 patients (17.8%) who were 25–35 years old, 2 patients (7.2%) who were 36–45 years old, 1 patient (3.6%) who was 46–55 years old, and 1 patient (3.6%) who was 56–65 years old; there were 19 (67.9%) female patients, including 4 patients (14.3%) who were 25–35 years old, 3 patients (10.7%) who were 36–45 years old, 10 patients (35.7%) who were 46–55 years old, and 2 patients (7.1%) who were 56–65 years old. Among the female patients, those who were 46–55 years old accounted for the largest proportion; those in this age range were in the perimenopausal period. Among the male patients, those who were 25–35 years old accounted for the largest proportion; those in this age range were considered young adults (Table 1).
 |
Table 1 Analysis of Gender and Age Range for 28 Patients with Refractory LPRD |
Analysis of Disease Status
(1) Psychological and psychological factors: Among the 28 patients with refractory LPRD, 10 had mild anxiety (35.7%), and 6 had moderate anxiety (21.4%); there were 10 cases of mild depression (35.7%) and 5 cases of moderate depression (17.9%) (Table 2).
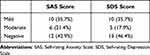 |
Table 2 Score and Severity of Anxiety and Depressive Symptoms [Case (%)] |
(2) Clinical manifestations: Among the 28 patients with refractory LPRD, the main symptoms of reflux were moderate to severe pharyngeal foreign body sensation (75.0%), persistent clearing of the throat (32.1%), and stomach upset with acid regurgitation and belching (35.7%) (Table 3). Patients with signs of reflux presented with moderate to severe thick mucus adhesion in the larynx (100%) and erythema/hyperemia of the laryngeal mucosa confined to the arytenoid cartilage (96.4%) (Table 4).
 |
Table 3 Number of Cases, Total Score, and the Proportion of Moderate to Severe Symptoms Based on the RSI |
 |
Table 4 Number of Cases, Total Score, and the Proportion of Moderate to Severe Findings Based on the RFS |
(3) Among the 28 patients with refractory LPRD, 17 (60.7%) were in the SAS/SDS (+) group and 11 (39.3%) were in the SAS/SDS (−) group (32.1%), with no significant difference in gender or age between the groups (Tables 5 and 6). Regarding the evaluation of efficacy after one month of PPI + Deanxit treatment, the RSI scores for the SAS/SDS (+) group were 15.53 ± 1.62 and 10.29 ± 1.05 before and after treatment, respectively, with an average decrease of 5.24 points, and the RFS scores were 6.53 ± 1.18 and 3.82 ± 0.73, respectively, with an average decrease of 2.71 points. The RSI scores for the SAS/SDS (−) group were 14.18 ± 1.72 and 10.36 ± 1.75 before and after treatment, respectively, with an average decrease of 3.82 points. The RFS scores before and after treatment were 6. 09 ± 1.30 and 3.64 ± 0.67, respectively, with an average decrease of 2.45 points. The differences in indices before and after treatment were statistically significant (all p<0.05). Therapeutic effect analysis: Before treatment, the RSI value and RFS were higher in the SAS/SDS (+) group than in the SAS/SDS (−) group; after treatment, the SAS/SDS (+) group had a larger decrease in the RSI value and RFS than the SAS/SDS (−) group. After standard treatment, the 28 patients had an overall approximate decrease of 31.3% and 41.0% for the RSI value and RFS, respectively, indicating a significant therapeutic effect. There was no significant difference in RSI or RSF scores between the two groups after treatment (p>0.05) (Tables 7 and 8).
 |
Table 5 Comparison of Gender in the SAS/SDS (−) Group (n=11) and the SAS/SDS (+) Group (n=17) |
 |
Table 6 Comparison of Age in the SAS/SDS (−) Group (n=11) and the SAS/SDS (+) Group (n=17) |
 |
Table 7 Comparison of Scores Before and After Treatment in the SAS/SDS (−) Group (n=11) and the SAS/SDS (+) Group (n=17) |
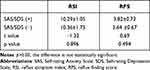 |
Table 8 Comparison of the RSI Values and RFS Values in the SAS/SDS (+) Group and SAS/SDS (−) Group After Treatment |
Discussion
In the present study, we found that anxiety and depressive symptoms influenced the occurrence, development, and treatment efficacy of refractory LPRD. Thus, attention to and targeted treatment of anxiety and depressive symptoms might help improve the treatment outcomes of patients with refractory LPRD.
LPRD is a common and frequently occurring disease in otolaryngology clinics and head and neck surgery centers and involves the movement of gastric contents in areas above the upper esophageal sphincter (including the pharynx, larynx, nasal cavity, and trachea), resulting in local mucosal injury. Typical clinical manifestations include pharyngeal foreign body sensation, persistent clearing of the throat, hoarseness or dysphonia, chronic long-term cough, dyspnea, and laryngospasm. Electronic laryngoscopy often reveals mucosal hyperplasia behind vocal cord commissures, hypertrophy, diffuse congestion, and edema of the vocal cords. In severe cases, there are laryngeal signs such as granuloma, larynx hypertrophy, and subglottic stenosis. LPRD is often manifested as a pharyngeal foreign body sensation, chronic cough, and other symptoms without specificity. Due to the mild symptoms of LPRD and manifestations and characteristics that do not include redness, heat, swelling, or pain, individuals with LPRD often receive attention and treatment only when it affects their lives. At the time of seeking treatment, patients with LPRD often have suffered from the disease for a long period of time.
Acid suppressive therapy with PPIs has been internationally recognized as the preferred drug treatment for LPRD. However, in recent years, due to the comprehensive influence of various factors such as diet,4 sleep,5,6 and work stress,7 some patients still show no significant improvement in LPRD symptoms after acid-suppressive therapy; in one study, PPIs and a placebo showed no significant difference in improving the symptoms of LPRD patients.8 Further, because of the limitations of clinical tools, many symptoms and extrapharyngeal manifestations were not considered.9 Although knowledge on nonacidic LPR has recently progressed, a treatment plan based on PPIs has not been developed.2 The therapeutic effect of PPIs alone to inhibit acid reflux is not ideal and therefore has also been evaluated incorrectly. The efficacy of selective serotonin reuptake inhibitor (SSRIs) in patients with LPRD has also been observed, but their side effects were quite significant. Deanxit tablets are more widely and safely used in clinical practice, with fewer side effects; therefore, we first observe their clinical application. Refractory LPRD requires further exploration of its etiology, pathogenesis, and influencing factors, as well as new treatment regimens.10 If long-term and aggressive treatment does not lead to significant improvements, we suggest that other factors should be considered during the diagnosis of refractory LPRD.
The incidence of LPRD in our outpatient department is increasing year by year. This phenomenon is not only occurring in China, as it was reported as early as 2012 that the prevalence of LPRD in the British population was as high as 34.39%.11 In the most recent survey in 2020, the incidence in the Brazilian population was approximately 26.8%.12 The incidence of LPRD varies in different populations. LPR is often diagnosed and treated in outpatient departments. The incidence of LPR in a certain population can only include the number of outpatient patients, but in fact, LPR also exists in patients hospitalized for other obvious symptoms or lesions.13 Further, LPR does not only exist in adult patients. A study from Shanghai Children’s Hospital pointed out that even in children with chronic cough, the incidence of LPR was as high as 36.8% (68/185).14 Therefore, full attention should be paid to LPR.
In this study, reflux symptoms and signs were more severe for patients who also had anxiety and depression symptoms. Further, therapeutic efficacy for refractory LPRD was positively related to psychological and psychological factors such as anxiety and depressive symptoms. This result is consistent with current research progress on the correlation between LPRD and mental psychological factors. Deanxit has anti-anxiety and anti-depression effects and can effectively improve mental perception abnormalities;15 its mechanism may be related to increased vagus-nerve excitability, autonomic nerve dysfunction, or potential mental and psychological abnormalities in these patients.16 After Deanxit treatment, the mental state of the patient improves, gastrointestinal autonomic nerve dysfunction is regulated, and visceral hypersensitivity is reduced. Mental factors can change hormone secretion and the kinetic response in the gastrointestinal tract through cerebral intestine reflexes and stress while regulating esophageal sensations, causing patients to perceive low-tone esophageal stimuli and feel pain and discomfort.17,18 Studies have shown that depression is associated with autonomic function control disorders, which may be related to the nervous system and the pathological basis of functional impairment.19 Although disorders such as anxiety and depression belong to psychological classification, psychological activities are built on the physiological activities of the brain, and psychological illness has a significant neurophysiological basis.20,21
In our research, in patients with lower SAS and SDS scores (who did not reach the threshold for anxiety and depression), the use of Deanxit could also significantly improve LPRD symptoms. Whether these patients have potential anxiety and depressive symptoms, and whether negative scores are due to subjective factors or cultural factors, require further exploration. After treatment, no statistically significant difference in RSI and RFS was observed between the SAS/SDS (+) and (−) groups. We suggest that among diseases affected by multiple factors, treatment of one cause has a peak therapeutic effect, and a radical cure effect cannot be achieved despite an obvious improvement of symptoms. Drug therapy has certain limitations for anxiety and depression symptoms. Thus, some scholars have applied behavioral, cognitive therapy, and neuromodulation to adjust the mental state of LPRD patients, achieving some degree of efficacy.22
In terms of LPRD incidence of gender, the majority of patients in our study with LPRD were perimenopausal women. An association between LPRD and female hormones cannot be ruled out. Women often have more autonomic nerve dysfunction than men because of hormone imbalances; in male patients, the age of onset is mainly 25–35 years old, indicating that work stress cannot be ruled out as a cause of LPRD. Stress is often associated with mental anxiety. Whether work stress is the cause of LPRD and whether mental anxiety impacts the occurrence and development of LPRD are issues worth addressing. In future clinical treatments, multifactorial effects should be considered. Endocrine functions should be regulated to improve treatment efficacy. Furthermore, studies have shown that the discomfort experienced by females, namely, intestinal gastrointestinal symptoms such as abdominal distension and hiccups, is significantly more severe than that experienced by males.23 Gastrointestinal symptoms relate to visceral sensitivity, which is associated with emotional disorders. Emotional disorders are associated with symptoms of depression, anxiety, and social anxiety.24 Based on this, we can also explain why the incidence of refractory LPRD is higher in females than in males.
Autonomic nerve dysfunction could manifest differently in different etiologies. Psychological stress, sleep disorders, metabolic disorders, and cardiopulmonary dysfunction may lead to autonomic nerve dysfunction.25 Laryngeal reflux was previously proposed as an extraesophageal symptom of gastroesophageal reflux (GERD), and laryngeal reflux and GERD were thought to be related to each other but have distinct processes. The physiological pathology of GERD is related to the dysfunction of the antireflux barrier mechanism. Currently, an increasing number of studies have examined the autonomic nerve functional status of patients with GERD, which have indicated that a reduction in parasympathetic nerve function may be a unique mechanism of the disease.26 In 2002, several scholars proposed that the laryngeal symptoms caused by LPRD are a manifestation of the vagal reflex.27 Studies have shown that when autonomic dysfunction occurs in GERD, autonomic nerve involvement is positively correlated with reflux symptoms.28 Wan-Ju et al proposed that autonomic nerve dysfunction is a pathogenic mechanism of LPRD and then specifically applied 24-hour dynamic electrocardiography to analyze heart rate variability, concluding that autonomic nerve dysfunction is not present in LPRD patients.29 In future studies, we will confirm whether a correlation exists among anxiety, depression, autonomic nervous function, and LPR.
According to the above discussion, only by investigating the etiology and pathogenesis combined with targeted treatment can any disease be fundamentally understood. LPRD is associated with a variety of otorhinolaryngologic diseases, including pediatric adenoidal hypertrophy, chronic sinusitis, asthma, and otitis media. Further, vocal diseases, including vocal polyps, vocal cord leukoplakia, contact granuloma, and Reinke’s edema, all have a non-negligible correlation with LPRD. LPRD is even a risk factor for the development of precancerous laryngeal lesions and laryngeal cancer, as well as many other otolaryngology diseases, gradually affecting patients quality of life, and its treatment involves blocking the root cause of a variety of diseases.
This study aimed to examine the factors related to refractory LPRD, but the sample size was too small, and the molecular-pathogenesis research was limited; therefore, we could not determine exactly how the relevant factors interacted with each other. In future studies of the diagnosis and treatment of refractory LPRD, we will concentrate on emotional and psychological factors, autonomic nervous function, and gastrointestinal sensitivity probe factors to clearly define the etiology and pathogenesis of the disease. At the same time, the application of the multidisciplinary, comprehensive treatment, such as medical and surgical therapy and even mental health therapy, should be applied. In this manner, we can further improve the standardized diagnosis and treatment of the disease, as well as improve therapy for patients.
Limitations
The sample size of this experiment was relatively small, which may influence the results of the study, especially regarding the proportion of cases and severity of the disease. The experimental control belongs to the self-controlled control; due to the complicated examination conditions, it was difficult for patients to cooperate and complete the examination. Furthermore, nucleic acid testing needs to be completed before improving laryngoscopy. The diagnosis and treatment process takes a long time, and some patients are reluctant to cooperate and complete the relevant examinations, yielding a small sample size. In addition, this experiment failed to improve the anxiety and depression symptom score and autonomic nervous function test after treatment and failed to make a detailed analysis of the relationship among them. Finally, it was unknown whether the patients had anxiety and depression before they were treated in our department due to pharyngeal foreign body sensation.
Ethical Conduct of Research
This study complies with the Declaration of Helsinki and was approved by the Ethics Committee of the First Affiliated Hospital of Guangxi Medical University. All participating patients gave informed consent, voluntarily participated in the study, and signed an informed consent form.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Liu H, Yang Q, Luo J, et al. Association between emotional eating, depressive symptoms and Laryngopharyngeal reflux symptoms in college students: a cross-sectional study in Hunan. Nutrients. 2020;12(6):1595. doi:10.3390/nu12061595
2. Lechien JR, Akst LM, Hamdan AL, et al. Evaluation and management of Laryngopharyngeal reflux disease: state of the art review. J Otolaryngol Head Neck Surg. 2019;160(5):762–782.
3. Li Y, Xu G, Zhou B, et al. Effects of acids, pepsin, bile acids, and trypsin on laryngopharyngeal reflux diseases: physiopathology and therapeutic targets. Eur Arch Oto-Rhino-Laryngol. 2021. doi:10.1007/s00405-021-07201-w
4. Peng Y, Xu D, Liu X, et al. [An epidemiological survey of laryngopharyngeal refux disease in otorhinolaryngology head and neck surgery clinics in Chongqing area]. J Clin Otolaryngol Head Neck Surg. 2021;35(4):351–354. Chinese.
5. Cui X, Zhang Y, Yan X, et al. Relationship between sleep status and laryngopharyngeal reflux disease in adult patients in Otolaryngology clinic. Chin J Otolaryngol Head Neck Surg. 2019;54(10):754–759. doi:10.3760/cma.j.issn.1673-0860.2019.10.009
6. Zhang Y, Jiang X, Chen H, et al. Chronic REM-sleep deprivation induced laryngopharyngeal reflux in rats: a preliminary study. Auris Nasus Larynx. 2021;48(4):683–689. doi:10.1016/j.anl.2020.10.011
7. Lechien JR, Bobin F, Muls V, Saussez S, Hans S. Laryngopharyngeal reflux disease is more severe in obese patients: a prospective multicenter study. Laryngoscope. 2021;131(11):e2742–e2748. doi:10.1002/lary.29676
8. Lyu Y, He J, Wei X, Zhang S, Fang Y, Yang X. Meta-analysis of the efficacy of proton pump inhibitors for the laryngopharyngeal reflux disease. Chin Archives Otolaryngo Head Neck Surg. 2018;25(3):150–156.
9. Snow GE, Dbouk M, Akst LM, et al. Response of Laryngopharyngeal symptoms to transoral incisionless fundoplication in patients with refractory proven gastroesophageal reflux. Ann Otol Rhinol Laryngol;2021. 34894211037414. doi:10.1177/00034894211037414
10. Vinciane RLJ, Giovanni M, François D, et al. The management of suspected or confirmed laryngopharyngeal reflux patients with recalcitrant symptoms: a contemporary review. Clin Otolaryngol. 2019;44(5):784–800.
11. Kamani T, Penney S, Mitra I, Pothula V. The prevalence of laryngopharyngeal reflux in the English population. Eur Arch Oto-Rhino-Laryngol. 2012;269(10):2219–2225. doi:10.1007/s00405-012-2028-1
12. Lechien JR, Perazzo PS, Ceccon FP, et al. Management of laryngopharyngeal reflux in Brazil: a national survey. Braz J Otorhinolaryngol. 2020. doi:10.1016/j.bjorl.2020.11.017
13. Wang YG, Guo YH, Li CF, et al. [Investigation of laryngopharyngeal reflux prevalence and risk factors in otolaryngology]. J Clin Otolaryngol Head Neck Surg. 2020;34(1):33–35. Chinese.
14. Bingru Y, Birong W, Min L. Incidence and risk factors of laryngopharyngeal reflux in children with chronic cough. Chin Archives Otolaryngo Head Neck Surg. 2019;26(2):101–109.
15. Chen X, Cheng J, Gong J. Deanxit can improve the dizziness, anxiety, and quality of life of patients with chronic subjective dizziness. Am J Transl Res. 2021;13(8):9348–9355.
16. Wang C. Clinical application of Deanxit. J Psychiatry. 2016;29(4):314–317.
17. Shaw MJ, Talley NJ, Beebe TJ, et al. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001;96(1). 52–57.
18. Mayer EA. Spinal and supraspinal modulation of visceral sensation. Gut. 2000;47(Suppl):4.
19. Hyung-Eun P, Joong-Seok K, Yoon-Sang O, et al. Autonomic nervous system dysfunction in patients with Parkinson disease having depression. J Geriatr Psychiatry Neurol. 2016;29(1). 11–17.
20. Panzer A, Viljoen M. Associations between psychological profiles and diseases: examining hemispheric dominance and autonomic activation as underlying regulators. Med Hypotheses. 2003;61(1):75–79. doi:10.1016/S0306-9877(03)00111-7
21. Campanella S, Guerit J-M. How clinical neurophysiology may contribute to the understanding of a psychiatric disease such as schizophrenia. Clin Neurophysiol. 2008;39(1). 31–39.
22. Hu J, Zhen M, Chen Y, Yu L, Yang H. Reconsidering on the drug therapy of adult laryngopharyngeal reflux disease. Chin J Otolaryngol Head Neck Surg. 2018;53(8):635–639. doi:10.3760/cma.j.issn.1673-0860.2018.08.017
23. Maria A, Felix A, Jules A, André A, Wulf R, Ulrich S. Epidemiology of gastrointestinal symptoms in young and middle-aged Swiss adults: prevalences and comorbidities in a longitudinal population cohort over 28 years. BMC Gastroenterol. 2018;18(1):21.
24. Michael Z, Charles J, Brooke GFS. Gut interpretations: how difficulties in emotion regulation may help explain the relation of visceral sensitivity with depression and anxiety among young adults with gastrointestinal symptoms. Psychol Health Med. 2018;23(7):840–845.
25. Lakoski SG, Jones LW, Krone RJ, Stein PK, Scott JM. Autonomic dysfunction in early breast cancer: incidence, clinical importance, and underlying mechanisms. Am Heart J. 2015;170(2):231–241.
26. Djeddi DD, Kongolo G, Stéphan-Blanchard E, Ammari M, Léké A. Involvement of autonomic nervous activity changes in gastroesophageal reflux in neonates during sleep and wakefulness. PLoS One. 2013;8(12):e83464. doi:10.1371/journal.pone.0083464
27. Koufman JA. Laryngopharyngeal reflux 2002: a new paradigm of airway disease. Ear Nose Throat J. 2002;81(9 Suppl):2–6.
28. Sun X, Ke M, Wang Z. Relationships among autonomic nervous function, reflux symptoms and esophageal motility in patients with gastro-esophageal reflux disease. Basic Clin Med. 2006;2006(9):967–970.
29. Wan-Ju H, Chih-Hung S, Kun-Ta C, et al. Evaluating the autonomic nervous system in patients with laryngopharyngeal reflux. J Otolaryngol Head Neck Surg. 2013;148(6). 997–1002.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
