Back to Journals » OncoTargets and Therapy » Volume 9
Correlation between pretreatment serum LDL-cholesterol levels and prognosis in nasopharyngeal carcinoma patients
Authors Tang Q, Hu Q, Piao Y, Hua Y
Received 11 October 2015
Accepted for publication 10 March 2016
Published 2 May 2016 Volume 2016:9 Pages 2585—2591
DOI https://doi.org/10.2147/OTT.S98079
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Jianmin Xu
Qiu Tang, Qiao-Ying Hu, Yong-feng Piao, Yong-Hong Hua
Department of Head and Neck Cancer Radiotherapy, Zhejiang Cancer Hospital, Hangzhou, Zhejiang, People’s Republic of China
Purpose: To investigate the correlations between long-term survival outcomes in patients with nasopharyngeal carcinoma (NPC) and pretreatment serum low-density lipoprotein cholesterol (LDL-C) levels.
Patients and methods: Between January 2008 and December 2011, 935 patients with newly diagnosed NPC who were treated with intensity-modulated radiation therapy were included in this retrospective clinical analysis. Patients were divided into two groups based on pretreatment LDL-C levels: normal LDL-C (≤3.64 mmol/L; n=816) and elevated LDL-C (>3.64 mmol/L; n=119). Associations between pretreatment LDL-C levels and treatment outcome were analyzed by univariate and multivariate analyses.
Results: The overall patient follow-up rate was 95.1%, and 726 patients received more than 5 years of follow-up. Five-year overall survival (OS), local control (LC), and distant metastasis-free survival (DMFS) rates of the entire patient population were 87.1%, 91.1%, and 87.2%, respectively. Rates of 5-year OS, LC, and DMFS for the elevated versus normal LDL-C groups were 77.0% vs 89.1% (P<0.001), 85.8% vs 91.9% (P=0.041), and 81.1% vs 88.1% (P=0.038), respectively. Compared with normal LDL-C levels, elevated LDL-C levels were identified as an independent prognostic factor of a poorer OS (hazard ratio [HR] =2.171; 95% confidence interval [CI] =1.424–3.309), LC rate (HR =1.762; 95% CI =1.021–3.942), and DMFS (HR =1.594; 95% CI =1.003–2.532).
Conclusion: This study found that elevated pretreatment LDL-C levels are negative prognostic indicators of NPC. Elevated LDL-C levels may be useful indicators of locoregional control and distant metastasis in NPC patients.
Keywords: LDL-cholesterol, nasopharyngeal carcinoma, prognosis
Introduction
One of the more prevalent afflictions in Southeast Asia is nasopharyngeal carcinoma (NPC), a unique type of head and neck cancer.1,2 Radiotherapy is the main treatment for NPC, and in recent years, intensity-modulated radiotherapy (IMRT) has been widely used, thus improving the clinical management of NPC, especially the local control (LC) rate. Treatment failure and disease progression of NPC have shifted from local recurrence and distant metastasis (DM) following 2-dimensional radiotherapy (2DRT) to DM following IMRT.3–5
At present, clinical stage, age, treatment interruption, and other factors are the most commonly accepted prognostic factors of NPC; however, there are other factors that may affect the prognosis of this disease. For example, over the course of radiotherapy, the degree of anemia in patients was found to affect sensitivity to radiotherapy,6,7 and more severe anemia was associated with poorer radiotherapy effects. These and other factors highlight the need to develop new therapeutic approaches for improving the prognosis of patients with NPC.
A number of epidemiological studies have investigated a causal link between cancer incidence and lipid levels. Studies have shown that increased dietary fat or cholesterol is correlated with an increased risk of certain malignancies, including lung,8 colorectal,9 breast,10 and prostate cancers.11 However, few studies have explored the causal and mechanistic associations between increased lipid levels and cancer behavior. Hyperlipidemia might favor lymph node metastasis in men with early gastric cancer.12 High levels of low-density lipoprotein cholesterol (LDL-C) can induce breast cancer proliferation and invasion and promote breast cancer progression.13 LDL-C is a significant predictor of survival in women with epithelial ovarian cancer.14
Pretreatment LDL-C levels may serve as a prognostic factor for cancer patients. In this study, we retrospectively investigated the correlation between pretreatment LDL-C levels and long-term outcomes in patients with NPC.
Patients and methods
Ethics statement
This study was approved by the Institutional Review Board of the Zhejiang Province Cancer Centre. Written informed consent was obtained from all patients in accordance with the Declaration of Helsinki.
Patients
From January 2008 to December 2011, 935 patients with NPC were treated with IMRT. This cohort included 658 male and 277 female patients aged 11–70 years (median, 49 years). Of the 935 NPC patients, 64 and 871 had World Health Organization pathological type II and III, respectively. The clinical staging features of these cancers (stage, T stage, and N stage) are reported in Table 1. The mean pretreatment LDL-C level for all patients was 2.72 mmol/L (range: 1.05–5.92 mmol/L). There were 816 patients in the normal LDL-C group (≤3.64 mmol/L) and 119 patients in the elevated LDL-C group (>3.64 mmol/L). The clinical data of the two groups are shown in Table 1. In this cohort study, 25 (3.1%) and 28 (23.5%) patients were statin users among the NPC patients with normal and elevated LDL-C levels, respectively. One statin user with normal LDL-C levels died of cerebral infarction 56 months after treatment; one non-statin user with elevated LDL-C levels was treated with aspirin enteric-coated tablets to prevent thrombosis, a beta blocker to protect heart function, and statins to lower blood lipids because of coronary heart disease that appeared 25 months or more after treatment.
Radiotherapy method
All patients underwent radical IMRT. The prescription dose of the gross tumor volume of the nasopharynx, metastatic lymph nodes, clinical target volume, and prophylactic irradiating region were 68–72 Gy, 60–66 Gy, 60 Gy, and 54 Gy, respectively, in 28–33 fractions. The prescribed dose is the minimum absorbed dose received by 95% of the planning target volume.
Chemotherapy
Eight hundred and twenty-two patients received two to three cycles of neoadjuvant chemotherapy regimens, including 528 cases of cisplatin and 5-fluorouracil regimens (consisting of 80 mg/m2 cisplatin via intravenous infusion on day 1 and 750–1,000 mg/m2 5-fluorouracil daily via intravenous infusion on days 1–3), 166 cases of docetaxel and cisplatin regimens (consisting of 80 mg/m2 cisplatin via intravenous infusion on day 1 and 75 mg/m2 docetaxel daily via intravenous infusion on day 1), 126 cases of docetaxel, cisplatin, and 5-fluorouracil regimens (consisting of 60 mg/m2 cisplatin via intravenous infusion on day 1, 60 mg/m2 docetaxel daily via intravenous infusion on day 1, and 600 mg/m2 5-fluorouracil daily as a 120-hour intravenous infusion on days 1–5), and two cases of gemcitabine and cisplatin regimens (consisting of 1,000 mg/m2 gemcitabine daily via intravenous infusion on days 1 and 8 and 80 mg/m2 cisplatin via intravenous infusion on day 1). Five hundred and eighteen patients received 30 mg/m2 cisplatin once a week for concurrent chemoradiotherapy, with a median cycle number of six (31 cases completed seven cycles, 288 cases completed six cycles, 16 cases completed five cycles, 89 cases completed four cycles, and 86 cases completed less than four cycles).
Research content
The 935 patients were divided into normal LDL-C (≤3.64 mmol/L; n=816) and elevated LDL-C (>3.64 mmol/L; n=119) groups. The prognostic influence of pretreatment LDL-C levels on clinical outcomes was compared between groups.
Statistical analysis
Categorical variables between the two LDL-C groups were compared using the χ2 test. The Kaplan–Meier method was employed to determine the rates of overall survival (OS), LC, and DM-free survival (DMFS). Survival curves were compared using the log-rank test. The prognostic significance of different factors was determined using Cox proportional hazards regression models. A statistically significant effect was defined as a P-value <0.05. All statistical analyses were performed using SPSS 19.0 (IBM Corporation, Armonk, NY, USA).
Results
Follow-up results
The follow-up deadline was May 15, 2015. The median patient follow-up interval was 61 months (range: 5–88 months). Forty-six patients were lost to follow-up, yielding a follow-up rate of 95.1%; 726 patients were followed up for more than 5 years.
Survival status
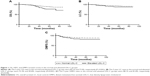
Of the 935 patients in this study, 83 (8.9%) developed locoregional failure and 119 (12.7%) developed DM. The 5-year OS, LC, and DMFS rates of the entire patient cohort were 87.1%, 91.1%, and 87.2%, respectively. The 5-year OS, LC, and DMFS rates of patients with normal versus elevated LDL-C levels were 77.0% vs 89.1% (χ2=12.501, P<0.001), 85.8% vs 91.9% (χ2=4.172, P=0.041), and 81.1% vs 88.1% (χ2=0.313, P=0.038), respectively. Table 2 indicates the 5-year OS, LC, and DMFS rates of the LDL-C groups among the patients. The survival curves for patients with normal and elevated LDL-C are shown in Figure 1A–C.
  | Table 2 Relationship between LDL-C level and survival |
Effect of pretreatment LDL-C levels on prognosis
Univariate analysis indicated that elevated LDL-C levels before treatment adversely affected the OS, LC, and DMFS rates (P<0.001, P=0.036, and P=0.044, respectively) of patients with NPC. Furthermore, multivariate analysis indicated that a high pretreatment LDL-C level was an independent prognostic factor of a lower OS (hazard ratio [HR] =2.171; 95% confidence interval [CI] =1.424–3.309), poorer LC rate (HR =1.762; 95% CI =1.021–3.942), and reduced DMFS (HR =1.594; 95% CI =1.003–2.532) in patients with NPC. These data indicate that an elevated pretreatment LDL-C level is a poor prognostic factor in patients with NPC. The results of the univariate and multivariate analyses of pretreatment LDL-C and other factors regarding clinical outcomes for patients with NPC are given in Table 3.
Discussion
In this study, the effect of pretreatment LDL-C levels on outcomes of patients with NPC was analyzed retrospectively. The results of this study show that the DMFS, LC, and OS rates of patients with NPC with normal LDL-C levels were significantly superior to those of patients with elevated LDL-C before treatment. High pretreatment LDL-C was an independent prognostic factor for reduced DMFS, poorer LC, and lower OS in patients with NPC, suggesting the potential value of LDL-C as a prognostic indicator of clinical outcomes in NPC patients. We did not identify correlations between abnormal HDL-C, total cholesterol, triglycerides, or apolipoprotein A-I levels and prognosis.
Furthermore, our results indicate that, in addition to the T stage, N stage, age, and sex, LDL-C is an independent risk factor for poorer OS, LC, and DMFS rates. Although the exact cause is unclear, this is an interesting finding from an oncological perspective. Cholesterol is an essential structural component of the cell membrane,15 and studies suggest that lipids promote tumor growth,16 produce energy, and maintain redox homeostasis.17 Increasing evidence supports the idea that tumor cell growth is partly dependent on exogenous LDL.18,19 Low-density lipoprotein receptors (LDLRs) are overexpressed in cancer cells,20–22 and this has been attributed to the large quantities of cholesterol and fatty acids that are required for supporting the rapid proliferation that occurs during tumorigenesis in a variety of tumor cells.21,23 LDL exposure induces cell proliferation, migration, and loss of adhesion, and is a hallmark of epithelial-to-mesenchymal transition.24 Scoles et al observed that treatment with oxidized LDL significantly reduced the chemosensitivity of both platinum-sensitive CAOV3 and platinum-resistant SKOV3 cells.19 From these reports, it can be deduced that high LDL-C levels are likely to promote the survival of NPC cells by stimulating tumor cells, thus affecting the sensitivity of chemotherapy, resulting in a poor LC rate.
The interaction between vascular endothelial cells and tumor cells is an important step in tumor metastasis. When tumor cells enter blood vessels, some of the cells rapidly disappear in the circulatory system and other cells quickly establish a position in the blood vasculature, and migrate through the blood vessel wall into the surrounding tissue to form new colonies. The first step in this process, adhesion to vascular endothelial cells, is achieved by tumor surface adhesion molecules such as integrins, endothelial cell adhesion molecules, and vascular cell adhesion molecule-1. In human endothelial cells, LDL can induce a significant increase in the expression of a number of adhesion-related markers, including intercellular adhesion molecule-1,25 vascular adhesion molecule-1,26 and P-selectin.27 Pulawski et al28 demonstrated that single LDL apheresis significantly lowered plasma concentrations of soluble vascular cell adhesion molecule-1, soluble intercellular adhesion molecule-1, and P-selectin. This suggests that high LDL levels may enhance the adhesiveness of vascular endothelial cells, thereby increasing the ability to capture and permit the transit of extravasating tumor cells. More recently, Reverter et al29 showed that altered cholesterol levels at the trans-Golgi network/endosome boundary triggered syntaxin 6 (Stx6) accumulation in VAMP3, transferrin, and Rab11-positive recycling endosomes, increasing the interaction between Stx6 and VAMP3, and interfering with the recycling of AvB3 and a5b1 integrins and cell migration, possibly in an Stx6-dependent manner. The fine-tuning of cholesterol levels at the trans-Golgi network/recycling endosome boundary together with a subset of cholesterol-sensitive SNARE proteins may regulate cell migration and invasion. In vivo studies showed that breast tumors were larger, more proliferative, and more likely to develop into lung metastases in hypercholesterolemic mice.13 Although necessary for normal cellular adhesion, integrins can help cancer cells metastasize. Elevated LDL-C levels seem to contribute to integrin movement and transmission in cancer cells, leading to cell migration and invasion.29 Our study, which compared NPC patients with normal and elevated LDL-C levels, suggests that elevated LDL-C levels may facilitate DM of NPC cells. This provides a theoretical explanation for why the DMFS rate was significantly higher in the elevated LDL-C group in this study.
Our study is limited by its retrospective design and the relatively small sample size of the high LDL-C group. In addition, LDL-C levels alone cannot adequately reflect the status of blood lipids before treatment. Furthermore, statin users with normal LDL-C levels when diagnosed with NPC may have additional comorbidities that influence survival. Moreover, diversity of the treatment modality and chemotherapy may affect the clinical outcome. However, these data demonstrate the prognostic impact and clinical significance of pretreatment LDL-C levels in patients with NPC, and reducing the level of pretreatment LDL-C may improve the LC rate and reduce DM of NPC. Further prospective studies should be under way to investigate the effect of statins on the prognosis of patients with NPC with high LDL-C by detecting changes in serum LDL-C levels.
Acknowledgments
The authors thank Miss Yan Wang for performing follow-up and Miss Qian Ying for managing the data. The authors especially thank all of the participants in the study.
Disclosure
The authors report no conflicts of interest in this work.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. | ||
Razak AR, Siu LL, Liu FF, Ito E, O’Sullivan B, Chan K. Nasopharyngeal carcinoma: the next challenges. Eur J Cancer. 2010;46(11):1967–1978. | ||
Su SF, Han F, Zhao C, et al. Long-term outcomes of early-stage nasopharyngeal carcinoma patients treated with intensity-modulated radiotherapy alone. Int J Radiat Oncol Biol Phys. 2012;82(1):327–333. | ||
Xiao WW, Huang SM, Han F, et al. Local control, survival, and late toxicities of locally advanced nasopharyngeal carcinoma treated by simultaneous modulated accelerated radiotherapy combined with cisplatin concurrent chemotherapy: long-term results of a phase 2 study. Cancer. 2011;117(9):1874–1883. | ||
Wolden SL, Chen WC, Pfister DG, Kraus DH, Berry SL, Zelefsky MJ. Intensity-modulated radiation therapy (IMRT) for nasopharynx cancer: update of the Memorial Sloan-Kettering experience. Int J Radiat Oncol Biol Phys. 2006;64(1):57–62. | ||
Brizel DM, Dodge RK, Clough RW, Dewhirst MW. Oxygenation of head and neck cancer: changes during radiotherapy and impact on treatment outcome. Radiother Oncol. 1999;53(2):113–117. | ||
Glaser CM, Millesi W, Kornek GV, et al. Impact of hemoglobin level and use of recombinant erythropoietin on efficacy of preoperative chemoradiation therapy for squamous cell carcinoma of the oral cavity and oropharynx. Int J Radiat Oncol Biol Phys. 2001;50(3):705–715. | ||
Kucharska-Newton AM, Rosamond WD, Schroeder JC, et al. HDL-cholesterol and the incidence of lung cancer in the Atherosclerosis Risk in Communities (ARIC) study. Lung Cancer. 2008;61(3):292–300. | ||
Steinmetz KA, Potter JD. Egg consumption and cancer of the colon and rectum. Eur J Cancer Prev. 1994;3(3):237–245. | ||
Zielinski CC, Stuller I, Rausch P, Muller C. Increased serum concentrations of cholesterol and triglycerides in the progression of breast cancer. J Cancer Res Clin Oncol. 1988;114(5):514–518. | ||
Gaziano JM, Hennekens CH. Dietary fat and risk of prostate cancer. J Natl Cancer Inst. 1995;87(19):1427–1428. | ||
Kitayama J, Hatano K, Kaisaki S, Suzuki H, Fujii S, Nagawa H. Hyperlipidaemia is positively correlated with lymph node metastasis in men with early gastric cancer. The British journal of surgery. Feb 2004;91(2):191–198. | ||
dos Santos CR, Domingues G, Matias I, et al. LDL-cholesterol signaling induces breast cancer proliferation and invasion. Lipids in health and disease. 2014;13:16. | ||
Li AJ, Elmore RG, Chen IY, Karlan BY. Serum low-density lipo protein levels correlate with survival in advanced stage epithelial ovarian cancers. Gynecologic oncology. Jan 2010;116(1):78–81. | ||
Lingwood D, Simons K. Lipid rafts as a membrane-organizing principle. Science. 2010;327(5961):46–50. | ||
Ifere GO, Barr E, Equan A, et al. Differential effects of cholesterol and phytosterols on cell proliferation, apoptosis and expression of a prostate specific gene in prostate cancer cell lines. Cancer Detect Prev. 2009;32(4):319–328. | ||
Santos CR, Schulze A. Lipid metabolism in cancer. FEBS J. 2012;279(15):2610–2623. | ||
Gal D, MacDonald PC, Porter JC, Simpson ER. Cholesterol metabolism in cancer cells in monolayer culture. III. Low-density lipoprotein metabolism. Int J Cancer. 1981;28(3):315–319. | ||
Scoles DR, Xu X, Wang H, et al. Liver X receptor agonist inhibits proliferation of ovarian carcinoma cells stimulated by oxidized low density lipoprotein. Gynecol Oncol. 2010;116(1):109–116. | ||
Sega EI, Low PS. Tumor detection using folate receptor-targeted imaging agents. Cancer Metastasis Rev. 2008;27(4):655–664. | ||
Notarnicola M, Messa C, Orlando A, et al. Effect of genistein on cholesterol metabolism-related genes in a colon cancer cell line. Genes Nutr. 2008;3(1):35–40. | ||
Chu HL, Cheng TM, Chen HW, et al. Synthesis of apolipoprotein B lipoparticles to deliver hydrophobic/amphiphilic materials. ACS Appl Mater Interfaces. 2013;5(15):7509–7516. | ||
Vitols S, Norgren S, Juliusson G, Tatidis L, Luthman H. Multilevel regulation of low-density lipoprotein receptor and 3-hydroxy-3-methylglutaryl coenzyme A reductase gene expression in normal and leukemic cells. Blood. 1994;84(8):2689–2698. | ||
Kalluri R, Weinberg RA. The basics of epithelial-mesenchymal transition. J Clin Invest. 2009;119(6):1420–1428. | ||
Yuan Y, Verna LK, Wang NP, et al. Cholesterol enrichment upregulates intercellular adhesion molecule-1 in human vascular endothelial cells. Biochim Biophys Acta. 2001;1534(2–3):139–148. | ||
Haller H, Schaper D, Ziegler W, et al. Low-density lipoprotein induces vascular adhesion molecule expression on human endothelial cells. Hypertension. 1995;25(4 Pt 1):511–516. | ||
Gebuhrer V, Murphy JF, Bordet JC, Reck MP, McGregor JL. Oxidized low-density lipoprotein induces the expression of P-selectin (GMP140/PADGEM/CD62) on human endothelial cells. Biochem J. 1995;306(Pt 1):293–298. | ||
Pulawski E, Mellwig KP, Brinkmann T, Kleesiek K, Horstkotte D. Influence of single low-density lipoprotein apheresis on the adhesion molecules soluble vascular cellular adhesion molecule-1, soluble intercellular adhesion molecule-1, and P-selectin. Ther Apher. 2002;6(3):229–233. | ||
Reverter M, Rentero C, Garcia-Melero A, et al. Cholesterol regulates Syntaxin 6 trafficking at trans-Golgi network endosomal boundaries. Cell Rep. 2014;7(3):883–897. |
 © 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2016 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.