Back to Journals » Infection and Drug Resistance » Volume 15
Correlation Between Individual Child-Level Antibiotic Consumption and Antibiotic-Resistant Among Commensal Escherichia coli: Results from a Cohort of Children Aged 1–3 Years in Rural Ujjain India
Authors Khare S , Diwan V, Pathak A , Purohit MR, Stålsby Lundborg C
Received 25 April 2022
Accepted for publication 11 September 2022
Published 28 October 2022 Volume 2022:15 Pages 6255—6266
DOI https://doi.org/10.2147/IDR.S372093
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Shweta Khare,1,2 Vishal Diwan,1,3 Ashish Pathak,1,4 Manju Raj Purohit,1,5,* Cecilia Stålsby Lundborg1,*
1Health Systems and Policy (HSP): Medicines, Focusing Antibiotics, Department of Global Public Health, Karolinska Institutet, Stockholm, 171 77, Sweden; 2Department of Public Health and Environment, Ruxmaniben Deepchand Gardi Medical College, Ujjain, Madhya Pradesh, 456006, India; 3Division of Environmental Monitoring and Exposure Assessment (Water and Soil), ICMR—National Institute for Research in Environmental Health, Bhopal, Madhya Pradesh, 462030, India; 4Department of Pediatrics, Ruxmaniben Deepchand Gardi Medical College, Ujjain, Madhya Pradesh, 456006, India; 5Department of Pathology, Ruxmaniben Deepchand Gardi Medical College, Ujjain, Madhya Pradesh, 456006, India
*These authors contributed equally to this work
Correspondence: Shweta Khare, Health Systems and Policy (HSP): Medicines, Focusing Antibiotics, Department of Global Public Health, Karolinska Institutet, Stockholm, 171 77, Sweden, Tel +91 9893986241, Email [email protected]
Background: The global expansion of antibiotic-resistant bacteria is a serious concern and is increasing worldwide in both pathogenic and commensal bacteria. The study determined the correlation between individual child-level antibiotic consumption and antibiotic resistance among the commensal Escherichia coli (E.coli) in a cohort of 125 children in rural Ujjain, India.
Methods: During a two-year period between August 2014 and September 2016, stool samples were collected at seven-time points from a cohort of 125 children; aged 1– 3. A total of six colonies of E.coli per stool sample were collected for antibiotic susceptibility testing. Antibiotic consumption data was collected during the healthcare-seeking follow–up done during the same period. At each of the seven-time points correlation between antibiotic consumption (Defined Daily Dose-DDD/100 patient-days) and antibiotic resistance (number of resistant isolates) was analyzed independently using the Spearman correlation coefficient. Further, mixed-effects logistic regression models were built to study correlation between child-level consumption of penicillin with the number of E.coli isolates resistant to ampicillin, consumption of cephalosporin with resistance to cefotaxime and ceftazidime, consumption of fluoroquinolones with resistance to nalidixic acid and consumption of cotrimoxazole with resistance to cotrimoxazole.
Results: Out of 756 illness episodes reported in 125 children 42% were with antibiotic prescriptions and reported a total antibiotic consumption of 55DDD/100 patient-days. The most common antibiotics used were cefixime (J01DD08;72 DDD/100patient/days) followed by ofloxacin (J01MA01;51DDD/100patient-days), cefpodoxime (J01DD13;38DDD/100patient-days) and amoxicillin (J01CA04;28DDD/100patient-days). The highest percentage of resistance was found to the ampicillin (67%) followed by nalidixic acid (52%) and cefotaxime (44%) and when summarized, more than 90% were resistant to cefotaxime, ceftazidime, and co-trimoxazole in commensal E.coli isolates. The consumption of cephalosporins showed weak positive correlation with the resistance to cefotaxime (Coefficient±SE=0.13 ± 0.09,p< 0.001).
Conclusion: Our findings showed no correlation between individual-level antibiotic consumption and resistance development in commensal E.coli in a rural community environment.
Keywords: Escherichia coli, Kirby Bauer disk diffusion method, healthcare-seeking behaviour, common childhood illness, caregivers, under-5 children, antibiotic prescribing, antibiotic resistance, rural population, India
Introduction
Antibiotic resistance is a major public health problem worldwide since the number of bacteria that are resistant to multiple drugs is increasing at an alarming rate.1 Bacterial resistance strains are not just prevalent in hospital settings; rather, a wide diversity of resistant strains can be found in the community.1 Each year, it is estimated that over 50,000 babies die of sepsis caused by bacteria resistant to first-line medicines.1 While precise population burden estimates are unavailable, it is believed that neonates and the elderly will be most impacted. By the year 2050, it is estimated that antimicrobial resistance will claim two million lives in India.2
Antibiotic resistance is caused by a multitude of factors, including current medical practices of health-care providers, antibiotic usage patterns, community perceptions, over-the-counter sales of antibiotics, socio-demographic characteristics and hygiene and clean water practices.3–5 One of the most significant reasons contributing to the rise of antibiotic resistance is the misuse and overuse of antibiotics in the community. This can be estimated by regular monitoring, which is lacking in community settings, especially in rural areas, which are home to around 70% of the total population of India.6 Another reason is the high burden of infectious diseases. Infectious diseases continue to be the primary cause of death in children under 5 in India. Acute infections like bacterial sepsis, respiratory tract infections, and diarrhoea are the top causes of death in children under the age of five.6 A high infectious disease burden is reported as the biggest threat and it showed inappropriate and irrational use of antibiotics, which led to increased antibiotic resistance.7 An individual’s healthcare-seeking behaviour (HSB) is also influenced by all of these elements. When it comes to healthcare-seeking in India, many people especially in rural areas start with home care, and/or the informal health-care system, which frequently involves the inappropriate use of medication, especially antibiotics, a major contributor to antibiotic resistance.8–11 Physiological and sociocultural factors, such as community exposure and ambulatory care, contribute significantly to an increase in antibiotic resistance.12,13 Public data from Indian communities are scarce, even though there is a widely documented high-level resistance in India. Antibiotic stewardship policies can be more effective when they are based on a clear understanding of the link between usage and resistance. This study’s results bridge the gap in our understanding of the prevalence of antibiotic resistance and its association with antibiotic consumption in a rural community setting.
Escherichia coli (E.coli), a common gastrointestinal inhabitant, and a key player in the spread of antibiotic resistance have been used to monitor and track the development of antibiotic resistance in study cohort. Faecal flora acts as a reservoir for resistant gene variants.1 When commensal gut bacteria like E.coli are exposed to antibiotics, they acquire antibiotic-resistant genes, and this resistance may be passed on to a more pathogenic organism.14 Several bacteria, including E.coli, have been recognized by the World Health Organization (WHO) as the most serious threat to the global spread of antibiotic resistance.15 Antibiotic resistance has previously been reported in commensal E.coli strains isolated from children who were not sick, animals, and water supplies.16 Therefore, this study aims to determine the correlation between individual child-level antibiotic consumption and antibiotic resistance among the commensal E.coli in a cohort of 125 children at 7 time-points over the period of 2 years in rural areas of Ujjain, India.
Materials and Methods
Study Design
Prospective correlation study, where a prospective analysis of the correlation between individual child-level antibiotic consumption and antibiotic resistance of the commensal E.coli cultured from stool samples collected from the cohort of children 1–3 years of age at 7-time points over a period of 2 years from August 2014 to September 2016 was conducted.
Study Setting
The study was carried out in 6 villages in the Ujjain district of Madhya Pradesh (MP) in central India.17 MP is the fifth most populous state in India, with a population of 72.6 million people; with the majority of the population living in rural areas (75%).18 Ujjain district has 131 villages. The study villages were selected purposively from within the rural demographic surveillance site (DSS) Palwa of Ruxmaniben Deepchand Gardi Medical College (RDGMC). One of the villages within the DSS was selected and named “Central village” as it had the highest concentration (80%) of health-care providers (both formal and informal). Then, for the selection of the study villages, first, a 5 km zone diameter was created around the central villages and then all the villages within the 5 km zone diameter were enlisted.17
Study Sample
The details of sampling are described in detail elsewhere.17 In short, the study included 6 villages. All the samples from the selected villages were analyzed at RDGMC’s central research laboratory (CRL). Villages located within a 5-kilometre distance (aerial distance) of the central village (described above); had a population of at least 500 people; a minimum of 15 children in the age range of 1–3 years are available in the village and had a transport time of less than 45 minutes to the CRL, RDGMC were the criteria used to select the villages for this study. The children aged 1–3 years from within the 6 study villages were selected using the following inclusion criteria: 1) having lived in the village for at least one year; 2) planned to stay in the village for at least two years, and 3) willing to take part in the study after written informed consent from parents/guardians. Simple random sampling based on random number tables was then used to select the 125 children from within the eligible children list.17
Sample Size Calculation
Estimates of proportions from a single batch of 100 children (but equally applicable to antibiotic prescriptions) have a precision of ± 10%. Using a repeated sampling of 100 children at seven-time points has 80% power to detect a linear trend in any observation in the proportion of 0.1 per time unit (step between sampling, negative or positive). The numbers of children included in the cohort were increased to 110 to accommodate for possible attrition over time. The sample size of 110 children gives a sufficiently high precision in estimates and at least an 80% power in comparisons between data points.17
Data Collection
Stool Sample Collection and Transportation
Stool sample was collected from the selected child under the supervision of the first author and the trained research assistants during the study period. One stool sample per child included in the cohort (n = 125) was collected at seven-time points at an interval of four months (covering distinct seasons): time point 1 – monsoon 2014 (late June to September), time point 2 – winter 2015 (October to February), time point 3 – summer 2015 (March to June), time point 4 – monsoon 2015, time point 5 – winter 2016, time point 6 – summer 2016 and time point 7 – monsoon 2016.19 The stool sampling kit which included: 1) autoclaved plastic container with a wide opening and a spoon; 2) sterile polythene sheet measuring 15*15 cm in dimension (all enclosed in a pre-sterilized polythene zip-lock bag) was used to collect the stool samples. The kits were distributed to the child’s caregivers one day before the stool sample collection. Parents were trained on how to collect stool samples using the stool sampling kit. The training was repeated at all 7-time points before the stool sample collection day. A cold chain of 4–6°C (for 4–5 hours) was maintained from stool sample collection to the transportation of the samples to the CRL, RDGMC, Ujjain for further processing.16,17,20
Preparation of the Samples
Microbiological processing started immediately after receiving the samples in the CRL. The samples were plated on selected and differentiated HiCrome® coliform chromogenic media (HiMedia Laboratories Pvt. Ltd., Mumbai, India) and E.coli colonies were identified (blue-violet colonies). Six E. coli colonies were isolated, processed, validated using polymerase chain reaction (PCR), purified, and kept for further examinations by inoculating at 37°C for 24 hours on chromogenic agar.17 The Kirby-Bauer disc diffusion technique,21 using disc strengths recommended by the Clinical and Laboratory Standards Institute (CLSI),22 was used for conducting antibiotic susceptibility test (AST) on all six verified E. coli isolated from each stool sample. The isolates were tested against the following five antibiotics: ampicillin, cefotaxime, ceftazidime, nalidixic acid and co-trimoxazole (Table 1). Antibiotics were chosen in accordance with the CLSI standards and from the list of common antibiotics used in the hospital attached with RDGMC for gram-negative coliform infections. Two technical specialists independently assessed the diameter of the inhibitory zones to the closest millimeter. The process was repeated if there was a difference of more than three millimeters between two readings. If there was still a disparity in the zone diameter, the CLSI recommended minimum inhibitory concentration approach was used to confirm the susceptibility pattern. All isolates with readings of intermediate susceptibility were regarded as resistant for calculations.17
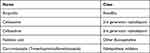 |
Table 1 Antibiotics and Their Respective Class for Which the Antibiotic Susceptibility Test Was Applied |
Individual Child-Level Antibiotic Consumption
The data on the individual child-level antibiotic consumption was simultaneously collected during the study period by following the HSB of the mother of cohort of the 125 children.17,23 The HSBs of the mothers for the acute illnesses in the children were documented using ‘HSB diaries’, with twice-weekly follow-ups (ie, with a recall period of 2 days) of the children for 113 weeks during the study period, done by the first author along with 6 research assistants. The HSB diary documented the route taken by a caregiver in seeking healthcare for a child’s illness through several health-care systems, reasons for choosing a particular healthcare as well as treatment details, with a focus on antibiotics consumed. All consumed drugs, including antibiotics, were verified during the subsequent biweekly visit. That is, the prescribed dose of the medicine consumed by the child was tallied with the left medicine in the wrapper/bottle.17,23
Data Management
During the study, the household was excluded from the study if they left the study area before all the data could be collected (Figure 1). However, for one particular round of data collection, if the caregiver was unable to provide the child’s stool sample, they were categorized as “Sample Not Obtained” and continued in the cohort. A sample was eliminated from the analysis of a particular time point if it was not received at the CRL or it was not feasible to isolate E.coli from the sample (Figure 1).
 |
Figure 1 Flow chart describing the study cohort and number of E.coli strains isolated from sample and included in the analysis, under study in rural Ujjain, India. |
A drug use (DU) proportion was calculated for each drug as the number of individual antibiotic use divided by the total number of antibiotic uses reported during the study period. The results are presented with antibiotics with more than or equal to 40 DU proportions. The WHO Collaborating Centre for Drug Statistics Methodology, Anatomical Therapeutic Chemical (ATC) classification was used to categorize each given antibiotic with the defined daily dose (DDD) according to the fifth level of the ATC classification, J01 (antibacterial for systemic use).24 All DDDs were calculated and adjusted to per 100 patient-days and were also adjusted for the pediatric doses.25
The resistance to a single antibiotic was identified as either an intermediate or resistant isolate and recorded as a result of the AST. Isolates with “intermediate” resistance were considered “resistant” for the analysis.
Statistical Analysis
Data were analyzed using Stata V.14.1 (Stata, College Station, Texas). Frequency and percentages were presented for categorical data. Resistance to selected antibiotic class and antibiotic consumption were analyzed over time points (time-variable) using linear regression individually with resistance and antibiotic consumption as dependent variable and time points as independent variable. Shapiro–Wilk for normality test was used to test the normal distribution of data.
Correlation Between Antibiotic Resistance and Consumption
Spearman correlation coefficient was used to look for the association between individual child-level penicillin consumption with ampicillin resistance, cephalosporin consumption with cefotaxime and ceftazidime resistance, fluoroquinolones consumption with nalidixic acid resistance and cotrimoxazole consumption with cotrimoxazole resistance. Further, the association between the above pairs of antibiotics and corresponding resistance was explored using mixed-effects logistic regression models. In total 5 mixed-effects logistic regression models were used to assess the correlation between individual child-level penicillin, cephalosporin, fluoroquinolones and cotrimoxazole consumption (DDD/100 patient-days) as explanatory variable (independent variable) and number of E.coli isolates resistant to ampicillin, cefotaxime, ceftazidime, nalidixic acid and cotrimoxazole as the outcome variable (outcome variable), respectively. In the models, the individual child was considered as a random effect considering the hierarchical data structure (isolates share the same child). Coefficient ± standard error (SE) was calculated and a p-value of ≤0.05 was considered statistically significant.
Ethical Considerations
The study has been approved by the Institutional Ethics Committee of RDGMC, Ujjain (approval number DNR-311/2013). Verbal and written informed consent were taken from the parents and/or legal guardians of the participating children after informing them about the purpose of the study and also that it did not include any invasive or otherwise dangerous procedures. It was made clear to the parent or guardian that their participation was voluntary and that all information provided would be kept strictly confidential. And the children who were found to be in need of medical attention were referred to paediatric services in collaboration with the RDGMC. The study complies with the Declaration of Helsinki.
Results
A total of 125 children (46% girls and 54% boys) were enrolled in the study with half of the children (n = 62) were under the age of one year, while the other half (n = 63) were between the ages of two and three years. A total of 756 illness episodes were reported in 125 children during the study period. The most common illness reported in the study was acute respiratory tract infections (ARTIs; 59%, 444/756), followed by fever (11%, 80/756) and gastrointestinal infections (10%, 74/756).
Total 799 stool samples were collected from 125 children during 7 time-points (Figure 1). A total of 4794 E.coli isolates were predicted to be retrieved from the 799 stool samples; however, 60 (1.3%) E.coli isolates could not be extracted due to lack of growth. Therefore, 4734 (98.7%) E.coli isolates were studied for their AST (Figure 1).
Antibiotic Consumption and Resistance
Antibiotics were prescribed in 42% (n = 320) of illness episodes out of a total of 756 illness episodes reported in 125 children. During the study, 337 antibiotic courses were prescribed and consumed. Parenteral (2%, n = 6/337) and topical formulations (6%, n = 20/337) were prescribed less compared to oral formulations (92%, n = 317/337). During the study period, the total antibiotics consumption in the study cohort was 55 DDD/100 patient-days. Overall, cephalosporins (44%, n = 149/337) were the most common class used, followed by penicillins (23%, n = 77/337). The most common antibiotics used were cefixime (J01DD08; 72 DDD/100 patient-days) followed by ofloxacin (J01MA01; 51DDD/100 patient-days), cefpodoxime (J01DD13; 38 DDD/100 patient-days) and amoxicillin (J01CA04; 28 DDD/100 patient-days) (Table 2). During the study period, total antibiotic consumption did not show any significant change over the period of 2 years. A significant decrease in consumption was found for cefixime (p = 0.034) and also for the total cephalosporin consumption (p = 0.023; Table 2; Figure 2).
 |
Table 2 Distribution of Antibiotic Consumption (DDD/100 Patient-Days) for Each of Antibiotic Class at 7-Time Points in Selected Cohort of Children (1–3 Years) During the Study Period |
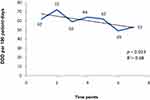 |
Figure 2 Overall cephalosporin consumption in the study cohort of children of 1–3 years of age at 7-time points, in defined daily doses (DDD) per 100 patient-days, in rural Ujjain, India. |
The obtained prevalence of antibiotic resistance per isolate to the selected antibiotic class and individual antibiotic by seven-time points are presented in Table 3. The highest rate of resistance was found for ampicillin (67%) followed by nalidixic acid (52%) and cefotaxime (44%). The lowest rates of resistance were found for co-trimoxazole (27%). Every child in the study had at least one isolate resistant to ampicillin and nalidixic acid. Cefotaxime, ceftazidime, and co-trimoxazole have all been shown to have resistance rates greater than 90%. No significant changes in proportions of resistance for the above antibiotics over a 2-year period (time-variable) could be identified.
 |
Table 3 Percentage Distribution of E.coli Isolates Resistant to the Selected Antibiotic Class at 7-Time Points |
Correlation Between Antibiotic Consumption and Resistance
Spearman correlation coefficient revealed significant association for individual child-level consumption of cephalosporins (60 DDD/100 patient-days) with cefotaxime resistance (2062 resistant isolates) (ρ = 0.04; 95% confidence interval (CI), 0.01–0.07; p value = 0.004). However, no statistically significant correlation was identified for penicillin consumption (39 DDD/100 patient-days) with ampicillin resistance (3190 resistant isolates; ρ = −0.08; 95% confidence interval (CI), −0.11 - −0.05; p value = 0.07); cephalosporins consumption (60 DDD/100 patient-days) with ceftazidime resistance (1834 resistant isolates; ρ = 0.02; 95% CI, −0.01–0.05;p value = 0.232); fluoroquinolones consumption (94 DDD/100 patient-days) with nalidixic acid resistance (2459 resistant isolates; ρ = −0.02; 95% CI, −0.04–0.01; p value = 0.23) and co-trimoxazole consumption (108 DDD/100 patient-days) with co-trimoxazole resistance (1292 resistant isolates; ρ = −0.001 [95% CI, −0.04–0.01]; p value = 0.92).
Mixed-effects logistic regression models also showed a weak positive correlation between cephalosporins consumption and resistance to cefotaxime (Coefficient ± SE = 0.13 ± 0.09, p<0.001; Table 4). In other words, every 0.13 DDD/100 patient-days increase in the cephalosporin consumption, results in a unit increase of the cefotaxime resistance. No significant correlations were found for penicillins, fluoroquinolones and co-trimoxazole consumption and corresponding resistance.
Discussion
To our knowledge, this is the first rural community-based study, where a possible correlation between individual child-level antibiotic consumption data and antibiotic resistance among the commensal E.coli in a cohort of 125 children in Ujjain, India, has been investigated. We found that out of 756 illness episodes reported in 125 children, 42% of episodes were with antibiotic prescriptions and the total antibiotic consumption was of 55 DDD/100 patient-days. The consumption of cephalosporins was positively correlated with the resistance to cefotaxime.
Antibiotic Consumption
A seasonal variation in overall antibiotic consumption (DDD/100 patient-days) during a 2-year period in the study cohort was seen. A peak in total antibiotic consumption during the winter 2015 (60 DDD/100 patient-days) and monsoon 2015 (66 DDD/100 patient-days) was seen (Table 2). The peak can be attributed to a rise in the number of illness episodes among the study cohort during winter and monsoon seasons as reported during the HSB follow-ups.23 Similar peaks in antibiotic prescribing have been observed from a hospital-based outpatient antibiotic use study in Ujjain.26
We have not seen any significant change in the total antibiotic consumption during the study period, but a decrease in antibiotic consumption was seen after Monsoon 2015. However, a significant decrease was found only in the consumption of the cephalosporin group of antibiotics. This could be explained by the Hawthorne effect.27 We monitored the illness episodes in the cohort and also the prescriptions provided by the health-care providers to the children included in the study area over a 2-year period. The Hawthorne effect might have reduced prescribing by the health-care providers of the children in the cohort, although no direct intervention was done to influence the prescribing.
We reported 42% antibiotic prescribing in our study between 2014 and 2016. This proportion of antibiotic prescribing is lower than that reported in previous studies done in the same geographical area.26,28–30 This lowered antibiotic prescribing rates could be due to the fact that earlier studies were health-care facility based as compared to our community-based study. Also, the present study measured antibiotic consumption, which is a better measure compared to antibiotic prescribing data. A lower antibiotic consumption rate in community-based study is expected as many illnesses in the community go untreated mainly due to community perception of the severity of illness episode being less serious.23 Also, illness episodes perceived as more serious end up presenting to a health-care provider, which in our rural communities are mostly the informal health-care providers.23,28 Healthcare-seeking from informal health-care providers typically increases the risk of antibiotic prescribing even for a viral illness.28 The majority of the illnesses reported were ARTIs. For the ARTI episodes, in 44% of these cases, no antibiotics were given as no treatment was sought.23 However, antibiotics were given in 24% of the ARTI cases, which were typically viral, as the caregivers took the child to the health-care providers, of which 89% of the antibiotic prescriptions were from informal health-care providers.23
Antibiotic Resistance
E.coli has been proved to be a useful marker bacterium for studying the development and emergence of antibiotic resistance due to its widespread distribution in the human gut and its susceptibility to commonly used antibiotics.31 At any given time, there are a number of E.coli strains in the human digestive system. However, there are some strains that are permanent residents of the human digestive tract, while others are only present in specific circumstances.32 It is, therefore, unlikely that resistance in one E.coli isolate will translate to resistance in all other E.coli isolates obtained from the same individual over the course of time. In our study, resistance to ampicillin was found in 67% of isolates, while resistance to nalidixic acid was found in 52%. Ampicillin and nalidixic acid-resistant E.coli bacteria were found in all children at one or more time points during the study. On the other hand, when taken together, 90% of the children’s commensal E.coli isolates were resistant to atleast one of the following antibiotics: cefotaxime, ceftazidime, and co-trimoxazole. A study conducted in 2018 in the rural areas of the state of Sikkim on pre-school and school-going children showed similar results.33 However, these occurrence rates are much higher than the rates reported in the previous studies. One of the previous study conducted in 2013 was done in the same study area and reported resistance rate of 72% in E.coli isolates from children aged 3 to 14 years.12,34,35 This high antibiotic resistance rate in central India may be attributed to the rapid proliferation of the antibiotic resistance gene pool over the past 9–10 years, especially in commensal E.coli.33 Concerningly, such a resistance pattern has a direct impact on the child’s health indicators.36
Our study results showed a weak positive correlation between the individual child-level cephalosporin consumption and cefotaxime resistance, which are consistent with the findings of the previous studies which showed a significant correlation between the consumption of 3rd generation cephalosporin and 3rd generation cephalosporin resistance rate in E.coli.37,38 In past years, many studies have examined the association between antibiotic use and the development of resistance and have found that the rate and amount of antibiotic use in the population is a key factor of rising antibiotic resistance in bacteria.30,39–43 However, most of these studies were conducted in hospital settings. A meta-analysis showed a significant positive association between antibiotic resistance and antibiotic consumption at the community level with a pooled effect size (odds ratio) of 2.33 (z = 25.71, p 0.01, 95% confidence interval 2.19 to 2.49).44 Our study results showed no correlation between penicillin consumption and ampicillin resistance in commensal E.coli. However, while studying the changes in the ampicillin resistance rate, there was an observable rise in the resistance rate at the 6th and 7th-time points (Table 3), but no rise in penicillin consumption was noted during the same time period. But there was a notable rise in penicillin consumption at the 4th time point (Table 2). The rise in the resistance rate at the 6th and 7th-time points can be a lag effect of the increase in penicillin consumption at the 4th time point. However, we cannot determine whether the change was significant or not as the time period was short enough to show any interaction between antibiotic use and resistance.45 Our study also showed high resistance rates despite the reported total antibiotic consumption rate of only 45% in the study cohort, this could be the spillover effect, which has been shown to have consequences at the family and community level, where antibiotic use in one population selectively develops resistance that is passed to the other.46
Methodological Considerations
Our study has the following strengths: the study analyzed the association between the individual child-level consumption of antibiotics and resistance, at the community level in a defined cohort over a prospective longitudinal period. We collected the prospective data for antibiotic consumption and resistance and could analyse the relationship with real-life observations, over time. The reporting of antibiotic consumption was validated by twice-weekly follow up of the study cohort, which has enabled analysis of individual drug consumption to be correlated with antibiotic resistance. The information on antibiotic consumption was not self-reported by the caregivers. However, it was collected by actual pill count. During the HSB follow-ups, the antibiotic consumption data was recorded repeatedly from the same group of caregivers (caregivers of 125 children), which increases the reliability of the data and also helps control the factors that contribute to the variation in responses. Moreover, the recall period of 2 days lowered the likelihood of recall bias.
Our study has some limitations also as: the ATC/DDD approach was used in the study because it is the best available tool for comparing antibiotic use across different settings (communities, hospitals and national boundaries), as well as antibiotic use trends over time. However, there is only one DDD assigned to each generic compound, so this approach does not account for the fact that a patient’s age, diagnosis, and degree of sickness all have an effect on the appropriate dose. Furthermore, the DDD methodology does not provide pediatric doses. So, all DDDs were calculated and adjusted to per 100 patient-days and were also adjusted for the pediatric doses. Another limitation of our study is that for some of the antibiotics consumed we did not have ASTs, this was because AST was decided before the start of the study and adding some of the AST was not feasible.
Conclusion
To conclude, we showed that there is no correlation between antibiotic consumption and the subsequent development of resistance in commensal E.coli at the rural community setting for the cephalosporin group of antibiotics. Further studies are needed to understand the factors causing the spillover effect like factors related to family, community and environment. We believe that effective antimicrobial stewardship strategies and antibiotic prescribing guidelines are needed at the local level, where our data on the association between antibiotic resistance rates and antibiotic consumption at the community level can be very useful.
Abbreviations
E.coli, Escherichia coli; WHO, World Health Organization; DDD, Defined daily doses; DSS, Demographic surveillance site; RDGMC, Ruxmaniben Deepchand Gardi Medical College; MP, Madhya Pradesh; CRL, Central research laboratory; PCR, Polymerase chain reaction; CLSI, Clinical and laboratory standards institute; AST, Antibiotic susceptibility test; HSB, Healthcare-seeking behaviour; ATC, Anatomical therapeutic chemical classification; DU, Drug use; SE, Standard error; ARTI, Acute respiratory tract infections.
Acknowledgments
The project was funded by Swedish Research Council (grant nos 521-2012-2889, 2017-01327 and 2021-00889). The authors thank the participating caregivers and children for participating and providing their valuable time. We would also like to thank Medical Director, Dr. V.K. Mahadik and the management of R.D.Gardi Medical College, Ujjain for providing administrative assistance for the study. We would like to acknowledge the enormous amount of work done by the teams assisted in the field by Sunita, Vikram, Bharat, Pooja, Maya, Mamta, Mukesh, and Bhaarat; the CRL team, Praveen Chauhan, Girish Jain, Nimita Deora, Deepika Tiwari, and Imran Nagori, who all assisted in the microbiology part and the data management team, Ankit Garg and Giriraj Singh Sisodiya at R.D. Gardi Medical College. We are also grateful for the assistance in data collection and support in the field by Priyank Soni, Devis Saha, and Vivek Parashar. We also would like to thank Dr Ashok J Tamhankar for his assistance on several occasions, particularly for his critical comments and suggestions on papers.
Funding
The project was funded by the Swedish Research Council (grant no 521-2012-2889, 2017-01327 and 2021-00889). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Laxminarayan R, Duse A, Wattal C, et al. Antibiotic resistance – the need for global solutions. Lancet Infect Dis. 2013;13(12):1057–1098. doi:10.1016/S1473-3099(13)70318-9
2. Center for Disease Dynamics, Economics & Policy 2015. State of the World’s Antibiotics. Washington, DC: Center for Disease Dynamics, Economics & Policy; 2015. Available from: https://www.cddep.org/wp-content/uploads/2017/06/swa_edits_9.16.pdf.
3. National treatment guidelines for antimicrobial use in infectious diseases. National Center for Disease Control, Directorate General of Health Services, Ministry of Health & Family Welfare. Government of India; 2016. Available from: http://pbhealth.gov.in/AMR_guideline7001495889.pdf.
4. Jacob JT, Muliyil J. Public health is infrastructure for human development. Indian J Med Res. 2009;130(1):9–11.
5. Centre for Disease. Report on “Antibiotic resistance threats in the United States”; 2013. Available from: https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf.
6. Van Boeckel TP, Gandra S, Ashok A, et al. Global antibiotic consumption 2000 to 2010: an analysis of national pharmaceutical sales data. Lancet Infect Dis. 2014;14:742–750. doi:10.1016/S1473-3099(14)70780-7
7. Dutta SS. India launches strategy to curb antimicrobial resistance. BMJ. 2017;357:j2049. doi:10.1136/bmj.j2049
8. World Health Organisation. Improving the containment of antimicrobial resistance. WHA; 2005. Available from: https://www.searo.who.int/entity/medicines/topics/wha_58_27.pdf.
9. Dekker AR, Verheij TJ, van der Velden AW. van der Velden AW. Inappropriate antibiotic prescription for respiratory tract indications: most prominent in adult patients. Fam Pract. 2015;32(4):401–407. doi:10.1093/fampra/cmv019
10. Viberg N, Kalala W, Mujinja P, Tomson G, Lundborg CS. ”Practical knowledge” and perceptions of antibiotics and antibiotic resistance among drugsellers in Tanzanian private drugstores. BMC Infect Dis. 2010;10. doi:10.1186/1471-2334-10-270
11. Wattal C, Goel N. Tackling antibiotic resistance in India. Expert Rev Anti Infect Ther. 2014;12(12):1427–1440. doi:10.1586/14787210.2014.976612
12. Sahoo KC, Tamhankar AJ, Sahoo S, Sahu PS, Klintz SR, Lundborg CS. Geographical variation in antibiotic-resistant Escherichia coli isolates from stool, cow-dung and drinking water. Int J Environ Res Public Health. 2012;9(3):746–759. doi:10.3390/ijerph9030746
13. Stålsby Lundborg C, Tamhankar AJ. Understanding and changing human behaviour--antibiotic mainstreaming as an approach to facilitate modification of provider and consumer behaviour. Ups J Med Sci. 2014;119(2):125–133. doi:10.3109/03009734.2014.905664
14. Tenover FC, McGowan JE. Reasons for the emergence of antibiotic resistance. Am J Med Sci. 1996;311(1):9–16. doi:10.1016/S0002-9629(15)41625-8
15. World Health Organisation. Antimicrobial resistance: global report on surveillance; 2014. Available from: https://apps.who.int/iris/bitstream/handle/10665/112642/9789241564748.eng.pdf..
16. Purohit MR, Chandran S, Shah H, et al. Antibiotic resistance in an Indian rural community: a ‘one-health’ observational study on commensal coliform from humans, animals, and water. Int J Environ Res Public Health. 2017;14:4. doi:10.3390/ijerph14040386
17. Stalsby Lundborg C, Diwan V, Pathak A, et al. Protocol: a ‘One health’ two year follow-up, mixed methods study on antibiotic resistance, focusing children under 5 and their environment in rural India. BMC Public Health. 2015;15:1321. doi:10.1186/s12889-015-2632-2
18. Encyclopedia Britannica. Madhya Pradesh [Internet]. Britannica Academic; 2017. Available from: https://academic.eb.com/levels/collegiate/article/MAdhya-Pradesh/111205.
19. Arora SK, Jha B. Indian meteorological department; 2018. Available from: http://mausam.imd.gov.in/.
20. Purohit MR, Lindahl LF, Diwan V, Marrone G, Lundborg CS. High levels of drug resistance in commensal E. coli in a cohort of children from rural central India. Sci Rep. 2019;9. doi:10.1038/s41598-019-43227-1
21. Bauer AW, Kirby WM, Sherris JC, Turck M. Antibiotic susceptibility testing by a standardized single disk method. Am J Clin Pathol. 1966;45(4):493–496. doi:10.1093/ajcp/45.4_ts.493
22. CLSI. Performance standards for antimicrobial susceptibility testing. Twenty-third informational supplement (CLSI Document M100-S23). Clinical and Laboratory Standards Institute; 2013:1–184.
23. Khare S, Pathak A, Purohit MR, et al. Determinants and pathways of healthcare-seeking behaviours in under-5 children for common childhood illnesses and antibiotic prescribing: a cohort study in rural India. BMJ Open. 2021;11(12):e052435. doi:10.1136/bmjopen-2021-052435
24. World Health Organisation. World Health Organization Anatomical Therapeutic Chemical (ATC) classification system: guidelines for ATC classification and DDD assignment 2018. Oslo, Norway: WHO Collaborating Centre for Drug Statistics Methodology, ATC classification index with DDDs; 2018. Available from: https://www.whocc.no/ddd/list_of_ddds_combined_products/.
25. World Health Organisation. Defined Daily Doses (DDD). Available from: https://www.who.int/tools/atc-ddd-toolkit/about-ddd.
26. Pathak A, Mahadik K, Dhaneria SP, et al. Antibiotic prescribing in outpatients: hospital and seasonal variations in Ujjain, India. Scand J Infect Dis. 2011;43(6–7):479–488. doi:10.3109/00365548.2011.554854
27. McCambridge J, Witton J, Elbourne DR. Systematic review of the Hawthorne effect: new concepts are needed to study research participation effects. J Clin Epidemiol. 2014;67(3):267–277. doi:10.1016/j.jclinepi.2013.08.015
28. Khare S, Purohit M, Sharma M, et al. Antibiotic prescribing by informal healthcare providers for common illnesses: a repeated cross-sectional study in Rural India. Antibiotics. 2019;8:3.
29. Sharma M, Damlin A, Pathak A, et al. Antibiotic prescribing among pediatric inpatients with potential infections in two private sector hospitals in central India. PLoS One. 2015;10(11):e0142317. doi:10.1371/journal.pone.0142317
30. Pathak A, Mahadik K, Dhaneria SP, Sharma A, Eriksson B, Lundborg CS. Surveillance of antibiotic consumption using the “focus of infection” approach in 2 hospitals in Ujjain, India. PLoS One. 2012;7(6):e38641. doi:10.1371/journal.pone.0038641
31. Oluyege AO, Ojo-Bola O, Oludada OE. Carriage of antibiotic resistant commensal E. coli in infants below 5 months in Ado-Ekiti. Int J Curr Microbiol Appl. 2015;4:1096–1102.
32. Caugant DA, Levin BR, Selander RK. Genetic diversity and temporal variation in the E. coli population of a human host. Genetics. 1981;98(3):467–490. doi:10.1093/genetics/98.3.467
33. Singh AK, Das S, Singh S, et al. Prevalence of antibiotic resistance in commensal Escherichia coli among the children in rural hill communities of Northeast India. PLoS One. 2018;13(6):e0199179. doi:10.1371/journal.pone.0199179
34. Seidman JC, Anitha KP, Kanungo R, Bourgeois AL, Coles CL. Risk factors for antibiotic-resistant E. coli in children in a rural area. Epidemiol Infect. 2009;137(6):879–888. doi:10.1017/S0950268808001519
35. Shakya P, Barrett P, Diwan V, et al. Antibiotic resistance among Escherichia coli isolates from stool samples of children aged 3 to 14 years from Ujjain, India. BMC Infect Dis. 2013;13(1):477. doi:10.1186/1471-2334-13-477
36. Dufour A, Snozzi M, Koster W, et al.. Assessing Microbial Safety of Drinking Water: Improving Approaches and Methods. Dufour A, edited by. World Health Organization: Geneva; 2003
37. Mariya JN, Bhanupriya B, Shewade DG, Belgode HN. Relationship between antimicrobial consumption and the incidence of antimicrobial resistance in Escherichia coli and Klebsiella pneumoniae isolates. J Clin Diagn Res. 2015;9(2):DC08–DC12.
38. Yang P, Chen Y, Jiang S, Shen P, Lu X, Xiao Y. Association between the rate of third generation cephalosporin-resistant Escherichia coli and Klebsiella pneumoniae and antibiotic consumption based on 143 Chinese tertiary hospitals data in 2014. Eur J Clin Microbiol Infect Dis. 2020;39(8):1495–1502. doi:10.1007/s10096-020-03856-1
39. Kenyon C, Buyze J, Spiteri G, Cole MJ, Unemo M. Population-level antimicrobial consumption is associated with decreased antimicrobial susceptibility in Neisseria gonorrhoeae in 24 European Countries: an ecological analysis. J Infect Dis. 2020;221(7):1107–1116. doi:10.1093/infdis/jiz153
40. Mascarello M, Simonetti O, Knezevich A, et al. Correlation between antibiotic consumption and resistance of bloodstream bacteria in a University Hospital in North Eastern Italy, 2008–2014. Infection. 2017;45(4):459–467. doi:10.1007/s15010-017-0998-z
41. Pathak A, Chandran SP, Mahadik K, Macaden R, Lundborg CS. Frequency and factors associated with carriage of multi-drug resistant commensal Escherichia coli among women attending antenatal clinics in central India. BMC Infect Dis. 2013;13:199. doi:10.1186/1471-2334-13-199
42. Yang P, Chen Y, Jiang S, Shen P, Lu X, Xiao Y. Association between antibiotic consumption and the rate of carbapenem-resistant Gram-negative bacteria from China based on 153 tertiary hospitals data in 2014. Antimicrob Resist Infect Control. 2018;7:137. doi:10.1186/s13756-018-0430-1
43. Barnsteiner S, Baty F, Albrich WC, et al. Antimicrobial resistance and antibiotic consumption in intensive care units, Switzerland, 2009 to 2018. Euro Surveill. 2021;26:46.
44. Bell BG, Schellevis F, Stobberingh E, Goossens H, Pringle M. A systematic review and meta-analysis of the effects of antibiotic consumption on antibiotic resistance. BMC Infect Dis. 2014;14:13. doi:10.1186/1471-2334-14-13
45. Mera RM, Miller LA, White A. Antibacterial use and Streptococcus pneumoniae penicillin resistance: a temporal relationship model. Microb Drug Resist. 2006;12(3):158–163. doi:10.1089/mdr.2006.12.158
46. Olesen SW, Lipsitch M, Grad YH. The role of “spillover” in antibiotic resistance. Proc Natl Acad Sci. 2020;117(46):29063. doi:10.1073/pnas.2013694117
 © 2022 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
© 2022 The Author(s). This work is published by Dove Medical Press Limited, and licensed under a Creative Commons Attribution License.
The full terms of the License are available at http://creativecommons.org/licenses/by/4.0/.
The license permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.

