Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 12
Correlation and compatibility between surface respiratory electromyography and transesophageal diaphragmatic electromyography measurements during treadmill exercise in stable patients with COPD
Authors Wu WL , Guan LL, Li XY, Lin L, Guo BP, Yang YQ, Liang ZY, Wang FY , Zhou LQ, Chen RC
Received 12 August 2017
Accepted for publication 2 October 2017
Published 6 November 2017 Volume 2017:12 Pages 3273—3280
DOI https://doi.org/10.2147/COPD.S148980
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Chunxue Bai
Weiliang Wu,1,* Lili Guan,1,* Xiaoying Li,2,* Lin Lin,1 Bingpeng Guo,1 Yuqiong Yang,1 Zhenyu Liang,1 Fengyan Wang,1 Luqian Zhou,1 Rongchang Chen1
1Guangzhou Institute of Respiratory Disease, State Key Laboratory of Respiratory Disease, The First Affiliated Hospital of Guangzhou Medical University, 2Department of Respiratory Medicine, The First Affiliated Hospital of Guangdong Pharmaceutical University, Guangzhou, China
*These authors contributed equally to this work
Purpose: To evaluate the compatibility and correlation between noninvasive surface respiratory electromyography and invasive transesophageal diaphragmatic electromyography measurements as facilitating indicators of neural respiratory drive (NRD) evaluation during treadmill exercise.
Patients and methods: Transesophageal diaphragmatic electromyogram activity (EMGdi,es) and surface inspiratory electromyogram (EMG) activity, including surface diaphragmatic EMG activity (EMGdi,sur), surface parasternal intercostal muscle EMG activity (EMGpara), and surface sternocleidomastoid EMG activity (EMGsc), were detected simultaneously during increasing exercise capacity in 20 stable patients with COPD. EMGdi,es, EMGdi,sur, EMGpara, and EMGsc were quantified using the root mean square (RMS) and were represented as RMSdi,es, RMSdi,sur, RMSpara, and RMSsc, respectively.
Results: There was a significant association between EMGdi,es and EMGdi,sur (r=0.966, p<0.01), EMGpara (r=0.967, p<0.01), and EMGsc (r=0.956, p<0.01) in the COPD patients during exercise. Bland-Altman plots showed that the lowest mean bias value was between EMGdi,es and EMGpara compared with the bias values between EMGdi,es and the other two EMG parameters. In comparing the estimation of EMGdi,es, we observed the lowest bias values (–1%) and the lowest limits of agreement values (–10% to –12%). Intraclass correlation coefficient (ICC) between EMGdi,es and EMGdi,sur was 0.978 (p<0.01), between EMGdi,es and EMGpara was 0.980 (p<0.01), and between EMGdi,es and EMGsc was 0.868 (p<0.01).
Conclusion: RMSdi,sur, RMSpara, and RMSsc could provide useful physiological markers of NRD in COPD. RMSpara shows the best compatibility and correlation with transesophageal diaphragmatic electromyography during treadmill exercise in stable patients with COPD.
Keywords: neural respiratory drive, transesophageal diaphragmatic EMG, surface diaphragmatic EMG, surface sternocleidomastoid EMG, surface parasternal intercostal muscle EMG
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by a chronic progressive and irreversible flow limitation, which is the main cause of death due to respiratory failure. The pathophysiological characteristics of COPD are airway obstruction, dynamic excessive lung inflation, and ultimately inflammation.1 Exertional dyspnea is the principal clinical symptom that affects the exercise capacity and quality of life in stable patients with COPD. Therefore, evaluation of exertional dyspnea is the most intuitive index of the effect of pulmonary rehabilitation. Exertional dyspnea was traditionally assessed via the Borg scale during the 6-minute walk test.2
It is widely accepted that the sensation of exertional dyspnea requires an awareness of the levels of neural output from the brainstem respiratory center to the peripheral respiratory muscles;3 hence, exertional dyspnea can be measured by detecting neural respiratory drive (NRD). The NRD to the diaphragm, represented by quantifying the diaphragmatic electromyogram (EMG) activity (the ratio of the root mean square [RMS] of the EMG activity to the maximum RMS of the EMG activity), is reportedly closely related to breathlessness in COPD.4 After the breathlessness threshold, incremental changes in diaphragmatic EMG activity expressed as a percentage of maximum (EMGdi%max) were significantly greater and less variable than incremental changes in ventilation as the intensity of breathlessness increased in stable patients with COPD.4 Traditionally, EMGdi was recorded using a multipair esophageal electrode catheter that was swallowed by the subject,5 leading to discomfort during EMGdi detection. Furthermore, the complex operations and indisposed feeling experienced by patients reduced follow-up visit compliance and increased the loss rate.
Noninvasive detection of the EMG activity of another inspiratory muscle, the parasternal intercostal muscle, using surface electrode recordings has advantages over EMGdi recorded using invasive esophageal catheters. Surface recordings of the EMG activity of the parasternal intercostal muscles (EMGpara) have also been shown to be closely related to breathlessness in healthy subjects and in respiratory disease;6 however, the study used the subjective Borg scale as a reference.7 Previous studies have also lacked a description of the effect of peripheral muscle activities on surface muscle recordings during exercise.
In order to evaluate the accuracy and feasibility of the application of noninvasive surface respiratory electromyography recordings in NRD evaluation during exercise, we detected the transesophageal diaphragmatic EMG activity (EMGdi,es) and surface inspiratory EMG activity, including surface diaphragmatic EMG activity (EMGdi,sur), surface sternocleidomastoid EMG activity (EMGsc), and EMGpara simultaneously during increasing exercise capacity in stable patients with COPD. The correlation and compatibility of invasive and noninvasive inspiratory EMG detection methods were analyzed during the whole exercise period.
Subjects and methods
Subjects
This clinical trial included 20 patients with COPD (age range, 40–80 years) treated at outpatient respiratory medicine departments at the First Affiliated Hospital of Guangzhou Medical University between July 2016 and December 2016. The diagnosis of COPD in all participants was made using pulmonary spirometry according to the Global Initiative for Chronic Obstructive Lung Disease guidelines.1 Inclusion criteria were: 1) post-bronchodilator forced expiratory volume in 1 s (FEV1)/forced vital capacity of 70%, and FEV1 of 50% of the predicted value; and 2) negative bronchial dilation test. Exclusion criteria were: 1) acute exacerbation of symptoms in the previous 4 weeks; 2) use of oral corticosteroids within 4 weeks; 3) smoking more than 10 cigarettes daily; and (4) history of other respiratory, cardiovascular, neuromuscular, and musculoskeletal diseases that could interfere with the exercise performance and inspiratory muscle activities.
Study design
Our study has been reviewed and published on the ClinicalTrials.gov public site (identifier: NCT03238209, date of registration: October 2, 2017). The study protocol was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University. Written informed consent was obtained from COPD patients before participation in this study. To ensure that the rights of all participants were protected, the researchers strictly adhered to the ethical principles Declaration of Helsinki in designing and conducting clinical research.
Measurements of transesophageal diaphragmatic electromyogram activity
EMGdi,es is the classic representative index that describes the activity of diaphragmatic myoelectric signals, which are the electrical manifestations of the excitation process elicited by action potentials propagating along muscle fiber membranes. The EMG signal is detected with multiple electrodes and then amplified, filtered, and displayed on a screen or digitized to facilitate further analysis. Electromyography of respiratory muscles can be used to assess the level and pattern of their activation to detect and diagnose neuromuscular pathology, and can be coupled with mechanical function tests to assess the efficacy of the muscle’s contractile function.7 NRD, expressed as EMGdi, was measured using a multipair esophageal electrode consisting of nine consecutive coils composed of five electrode pairs8 positioned in the esophagus and traversing the cardia9 (Figure 1). EMGdi signals acquired with digital sampling at 2 kHz were bandpass filtered (10 Hz–1 kHz) and amplified. Peak RMS per respiratory cycle was calculated and averaged over 1 min. The RMS of the EMGdi signal is the quantification of the total EMGdi power. Theoretically, the RMS of the EMGdi reflects the quantity of neural output from the brainstem respiratory center to the peripheral respiratory muscles activity level and also reflects the sensation of dyspnea.
Measurements of surface inspiratory electromyogram activity
Electromyogram electrodes
The electrical activity of the surface inspiratory EMG was derived transcutaneously from pairs of single disposable electrodes (Neotrode; Conmed Corporation, New York, NY, USA). The same disposable electrode was used for the common or ground electrode. The electrical activity of the sternocleidomastoid muscles and intercostal muscles were derived transcutaneously from reusable bipolar electrodes formed by two narrow rim electrode housings, each containing a 4 mm Ag–AgCl sintered electrode pallet (InVivo Metrics, Healdsburg, CA, USA), interconnected with a plastic clip (homemade UMCG, Groningen, the Netherlands) at a distance of 14 mm. After filling the electrode cavity with electrode gel, the assembly was fixed to the skin with double-sided adhesives. All EMG signals detected by electrodes were conveyed to the biological signal acquisition and analysis system (Powerlab 16/35; ADInstruments, Sydney, NSW, Australia) by shielded low noise cables.
Electrode placement
EMGdi,sur: the surface detecting electrode couple were separately placed at the intersection point of the sixth and eight intercostal space and at the anterior axillary line, at a distance of 5 cm.10
EMGpara: the surface detecting electrodes were placed bilaterally in the second intercostal space, about 3 cm parasternal, and a reference ground electrode was placed at the sternum sternal angle.11
EMGsc: the surface detecting electrodes were placed at 1/3 and 2/3 of the overall length of sternocleidomastoid, and a reference ground electrode was placed at the suprasternal fossa (Figure 1).12
Exercise testing
All patients performed a maximal incremental cycle ergometry test using the Ergoselect 200 K (Cosmed, Rome, Italy). Ergometry was performed with the patient in sitting posture, in order to minimize the effects of muscle activity necessary for body stabilization. Furthermore, to minimize muscle activity required for head positioning, the patients were instructed to look straight ahead during the measurements. The test consisted of a steady-state resting period of 3 min followed by 1 min of unloaded pedaling at 60 cycles/min for each individual; the exercise load was increased by 10 W each minute until the test had to be stopped because symptoms prevented further exercise. After test results were recorded, the EMGdi,es and each surface inspiratory EMG at maximal exercise capacity were analyzed.
Statistical analysis
SPSS 16.0 was used to perform analyses and create graphs. Statistical description of measurement was represented by mean ± standard deviation. The change in each surface inspiratory EMG and EMGdi,es over time during exercise was assessed using a nonlinear fit model. A data processing method in which a continuous curve is used to characterize or approximate the coordinates represented by discrete points was used. Regression of repeated measurements in the same subject was proceeded, and description of measurement was represented by r-value. Analyses of correlation and consistency (Bland-Altman analysis and intraclass correlation coefficients) between EMGdi,es and surface inspiratory EMG parameters (EMGdi,sur; EMGpara; and EMGsc) were conducted. A p-value <0.05 was considered significant.
Results
Patient characteristics
This study included 20 stable patients with COPD. The mean patient age was 60.7±12.3 years, and the mean FEV1 was 38.1%±12.2%.
Electromyogram change characteristics
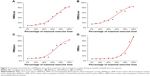
In COPD patients, EMGdi,es and surface inspiratory EMG activity increased constantly during increased treadmill exercise capacity according to the original EMG waveform (Figure 2). EMGdi,es was significantly increased from 20% of the total exercise time. EMGdi,sur was increased almost immediately after the start of the exercise test (from 10% of the total exercise time). EMGpara was significantly increased from 20% of the total exercise time (Table 1). The variation curves of EMGdi,es, EMGdi,sur, and EMGpara over the total exercise time showed an “S”-shaped increase (rose rapidly in the middle exercise stage and slowly in the later stage) (Figure 3A, B, and C). In contrast, RMSsc was increased from 50% of the total exercise time (Table 1). EMGsc increased to a greater extent and increased more rapidly than the other surface inspiratory EMG parameters over the total exercise time (Figure 3).
Association between transesophageal diaphragmatic electromyogram activity and each surface electromyogram
In the COPD patients, there was a significant association between EMGdi,es and EMGdi,sur (r=0.966, p<0.01; Figure 4A), between EMGdi,es and EMGpara (r=0.967, p<0.01; Figure 4B), and between EMGdi,es and EMGsc (r=0.956, p<0.01; Figure 4C).
Consistency test between transesophageal diaphragmatic electromyogram activity and each surface electromyogram
Bland-Altman plots showed a low mean bias value between EMGdi,es and EMGdi,sur. In comparing the estimation of EMGdi,es, we observed the lowest bias values (−9%) and the lowest limit of agreement (LoA) values (−20% to 2%). Bland-Altman analysis revealed that 12/220 (5.45%) points were not included in the 95% LoA. The difference between EMGdi,es and EMGdi,sur measurements was clinically acceptable, indicating that there was good consistency (Figure 5A).
Bland-Altman plots showed a lower mean bias value between EMGdi,es and EMGpara compared with the bias value between EMGdi,es and EMGdi,sur. In comparing the estimation of EMGdi,es, we observed the lowest bias values (−1%) and the lowest LoA values (−10% to −12%). Bland-Altman analysis revealed that 12/220 (5.45%) points were not included in the 95% LoA. The difference between EMGdi,es and EMGpara measurements was clinically acceptable, indicating that there was good consistency (Figure 5B).
Bland-Altman plots showed the highest mean bias value between EMGdi,es and EMGsc compared with the bias values between EMGdi,es and the other two surface EMGs. In comparing the estimation of EMGdi,es, we observed the lowest bias values (−11%) and the lowest LoA values (−18% to 39%). Bland-Altman analysis revealed that 0/220 (0%) points were not included in the 95% LoA. The difference between EMGdi,es and EMGsc measurements was bigger than the differences between EMGdi,es and the first two EMG measurements (Figure 5C).
Intraclass correlation coefficient (ICC) between EMGdi,es and EMGdi,sur was 0.978 (95% CI: 0.985,0.991, p<0.01). ICC between EMGdi,es and EMGpara was 0.980 (95% CI: 0.974,0.984, p<0.01). ICC between EMGdi,es and EMGsc was 0.868 (95% CI: 0.831,0.897, p<0.01). The difference between EMGdi,es and three surface respiratory EMG measurements was clinically acceptable.
Discussion
The major finding of the present study was that surface inspiratory EMG activity (represented by RMSdi,sur, RMSpara, and RMSsc) was closely related to RMSdi,es, which denotes exertional breathlessness in stable patients with COPD. An increase in surface EMGsc better indicated breathlessness than EMGpara and EMGsc, as the EMGsc variation curve appeared as a platform in low double-digits exercise time and then significantly increased in 80%–90% of exercise time, corresponding to a degree of dyspnea of 28.50±1.54% to 75.90±4.52%. The present results support the hypothesis that surface measurements of respiratory muscle activities is a reliable method of detecting breathlessness in COPD.
The traditional esophageal electrode catheter method is an invasive procedure, as the catheter is placed into the esophagus through the nostril, which causes discomfort during EMGdi detection. New methods of EMG detection using body surface electrodes have decreased the pain associated with the procedure and increased patient compliance. Previous studies indicate that the surface EMGpara, which is closely related to inspiratory drive, could provide a clinically useful biomarker in evaluating treatment response during acute exacerbations of COPD.13 Research has also indicated that increased inspiratory neck muscle activity is associated with insufficient levels of inspiratory pressure support during ventilator weaning,14 asynchronous ventilation,15 and weaning failure16 in intensive care unit patients with mechanical ventilation.
The diaphragm is the principal inspiratory muscle, contributing to 70% of ventilation17 and conducting the majority of inspiratory work in normal humans. Hence, the NRD, quantified as the EMGdi,es, is closely related to exertional breathlessness in COPD. Increases in EMGdi,es discriminate between successive Borg breathlessness scores better than increases in ventilation, which plateau as a consequence of marked neuroventilatory uncoupling due to impaired pulmonary mechanics. The development of esophageal catheters wired as multiple, overlapping pairs of bipolar electrodes that are analyzed using digital analysis algorithms18–21 has greatly improved the reliability and signal-to-noise ratio of the technique compared with earlier methods.22,23 Quantification of NRD using surface recordings of another inspiratory muscle, the parasternal intercostal muscle, has the advantage over EMGdi,es of being noninvasive. Surface recordings of EMGpara have also been shown to be closely related to breathlessness in COPD and cystic fibrosis.6,11 The present study showed that EMGdi,sur, EMGpara, and EMGsc activities were associated with increases in dyspneic sensation in COPD patients, coinciding with the findings of previous studies.
In COPD patients, EMGdi,sur was increased almost immediately after the start of the exercise test (from 10% of the total exercise time), while EMGdi,es significantly increased in 20% of the total exercise time. This indicates that noninvasive methods for recording EMGdi could provide similar results to the invasive measurements. As the principal inspiratory muscle that contributes the majority of ventilation effort, the diaphragm maintains a certain intensity of electric activity in the resting state, and it exhibits a rapid response to treadmill exercise. Noninvasive methods for recording the EMG activity of external intercostal muscles provided similar results; EMGpara rose rapidly in the middle exercise stage and slowly in the later stage, similarly to EMGdi,es. This indicates that the diaphragm and the external intercostal muscles are synergistic in spontaneous breathing and exertional dyspnea. NRD, as represented by EMGdi,sur and EMGpara, was reliable except for interference from the crosstalk effect. In contrast, RMSsc significantly increased from 50% of the total exercise time. EMGsc increased to a greater extent and increased more rapidly in the post-exercise stage. This result is in accordance with respiratory physiology, as the sternocleidomastoid muscles are accessory muscles of respiration and are active during relatively serious exertional dyspnea or high-intensity respiratory load. This indicates that patients experienced moderate to serious dyspnea during clinical observation of the activity of the sternocleidomastoid muscles. In the present study, sternocleidomastoid muscles activity was observed in 80%–90% of the exercise time, equivalent to 59.90±2.15 to 79.30%±3.80% of RMSdi,es. This indicates that patients were experiencing moderate to serious dyspnea while rhythmic contractile activity of the sternocleidomastoid muscles (consistent with breathing) could be clinically observed.
The diaphragmatic muscle, parasternal intercostal muscles, and sternocleidomastoid muscles contribute varying degrees to the inspiratory process and show different functions and characteristics. However, these three types of inspiratory muscles are synergistic, and evaluation of each type of inspiratory muscle could theoretically reflect NRD or dyspnea. In our study, measurement of the EMG activity of each inspiratory muscle had a strong correlation with EMGdi,es. In actual clinical conditions, surface EMG has a high sensitivity and is easily interfered with by crosstalk.24 Detecting the EMG activities of the diaphragmatic, parasternal intercostal, and sternocleidomastoid muscles simultaneously contributed to avoiding the effect of crosstalk during exercise. The best EMG recording could then be selected to represent the degree of dyspnea.
Conclusion
EMG measurement of the inspiratory muscles, represented by quantifying the surface EMG activities of the diaphragm, parasternal intercostal muscles, and sternocleidomastoid muscles as RMSdi,sur, RMSpara, and RMSsc, is closely related to RMSdi,es in COPD. Therefore, RMSdi,sur, RMSpara, and RMSsc could provide a useful physiological marker of NRD in COPD. RMSpara shows the best compatibility and correlation to EMGdi,es during treadmill exercise in stable patients with COPD.
Acknowledgments
The study was supported by the Science and Technology Project of Guangdong Province (2017A020211018), the Guangzhou Healthcare Collaborative Innovation Major Project (201604040012), and the State’s Key Project of Research and Development Plan (2017YFSF11078).
Author contributions
RCC conceived the study and determined the study program. WLW, LLG, and XYL drafted and submitted the manuscript. LL, YQY, and BPG acquired the training devices and detecting instruments. ZYL and FYW collected and analyzed data. WLW interpreted data. All authors contributed toward data analysis, drafting and critically revising the paper, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interests in this work.
References
Global Initiative for Chronic Obstructive Lung Disease. GOLD 2017 Global Strategy for the Diagnosis, Management and Prevention of COPD. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/. Accessed November 16, 2016. | ||
Pereira JS, de Aguiar Lemos F, Naso FCD, et al. Effect of six-minute walk test on neuromuscular properties of patients with chronic obstructive pulmonary disease. Clin Respir J. Epub 2015 Dec 1. | ||
Parshall MB, Schwartzstein RM, Adams L, et al. An Official American Thoracic Society statement: update on the mechanisms, assessment, and management of dyspnea. Am J Respir Crit Care Med. 2012;185:435–452. | ||
Jolley CJ, Luo YM, Steier J, et al. Neural respiratory drive and breathlessness in COPD. Eur Respir J. 2015;45(2):355–364. | ||
Luo YM, Moxham J. Measurement of neural respiratory drive in patients with COPD. Respir Physiol Neurobiol. 2005;146:165–174. | ||
Reilly CC, Ward K, Jolley CJ, et al. Neural respiratory drive, pulmonary mechanics and breathlessness in patients with cystic fibrosis. Thorax. 2011;66:240–246. | ||
Lindström L, Magnusson R. Interpretation of myoelectric power spectra: a model and its applications. Proc IEEE. 1977;65:653–662. | ||
Luo YM, Chen RC, Zhong NS. Measurement of diaphragm compound muscle action potential with magnetic stimulation of the phrenic nerve and multipara esophageal electrode in intensive care unit. Zhonghua Jie He He Hu Xi Za Zhi. 2005;28(8):505–508. | ||
Garland AJ, Doshi A, Turcanu V. Neural respiratory drive measurement for COPD assessment and monitoring. Pneumologia. 2015;64(1):14–17. | ||
Tang J, Lu YR, Luo YM. Respiratory effort assessed by surface diaphragm EMG in patients with sleep apnea. Zhonghua Jie He He Hu Xi Za Zhi. 2009;32(10):732–735. | ||
Duiverman ML, van Eykern LA, Vennik PW, Koëter GH, Maarsingh EJW, Wijkstra PJ. Reproducibility and responsiveness of a noninvasive EMG technique of the respiratory muscles in COPD patients and in healthy subjects. J Appl Physiol. 2004;96:1723–1729. | ||
Yoon TL, Kim KS, Cynn HS. Slow expiration reduces sternocleidomastoid activity and increases transversus abdominis and internal oblique muscle activity during abdominal curl-up. J Electromyogr Kinesiol. 2014;24(2):228–232. | ||
Murphy PB, Kumar A, Reilly C, et al. Neural respiratory drive as a physiological biomarker to monitor change during acute exacerbations of COPD. Thorax. 2011;66:602–608. | ||
Brochard L, Harf A, Lorino H, Lemaire F. Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis. 1989;139(2):513–521. | ||
Chao DC, Scheinhorn DJ, Stearn-Hassenpflug M. Patient ventilator trigger asynchrony in prolonged mechanical ventilation. Chest. 1997;112:1592. | ||
Parthasarathy S, Jubran A, Laghi F, Tobin MJ. Sternomastoid, rib cage, and expiratory muscle activity during weaning failure. J Appl Physiol. 2007;103:140–147. | ||
Wade OL. Movements of the thoracic cage and diaphragm in respiration. J Physiol. 1954;124(2):193–212. | ||
Luo YM, Li RF, Jolley C, et al. Neural respiratory drive in patients with COPD during exercise tests. Respiration. 2010;81:294–301. | ||
Reilly CC, Ward K, Jolley CJ, et al. Neural respiratory drive, pulmonary mechanics and breathlessness in patients with cystic fibrosis. Thorax. 2011;66:240–246. | ||
Sinderby C, Beck J, Spahija J, et al. Voluntary activation of the human diaphragm in health and disease. J Appl Physiol. 1998;85:2146–2158. | ||
Sinderby C, Spahija J, Beck J, et al. Diaphragm activation during exercise in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2001;163:1637–1641. | ||
Agostoni E, Sant’Ambrogio G, Del Portillo Carrasco H. Electromyography of the diaphragm in man and transdiaphragmatic pressure. J Appl Physiol. 1960;15:1093–1097. | ||
Petit JM, Milic-Emili G, Delhez L. Role of the diaphragm in breathing in conscious normal man: an electromyographic study. J Appl Physiol. 1960;15:1101–1106. | ||
Farina D, Merletti R, Indino B, Graven-Nielsen T. Surface EMG crosstalk evaluated from experimental recordings and simulated signals reflections on crosstalk interpretation, quantification and reduction. Methods Inf Med. 2004;43(1):30–35. |
 © 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2017 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.