Back to Journals » Clinical Interventions in Aging » Volume 17
Correlation Analysis and Prognostic Impacts of Biological Characteristics in Elderly Patients with Acute Myeloid Leukemia
Authors Li F , Li N, Wang A, Liu X
Received 25 May 2022
Accepted for publication 21 July 2022
Published 7 August 2022 Volume 2022:17 Pages 1187—1197
DOI https://doi.org/10.2147/CIA.S375000
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Fengli Li,1 Na Li,2 Anyou Wang,1,2 Xin Liu1,2
1Department of Hematology, Anhui Provincial Hospital Affiliated to Anhui Medical University, Hefei, People’s Republic of China; 2Department of Hematology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, People’s Republic of China
Correspondence: Xin Liu, Department of Hematology, Anhui Provincial Hospital Affiliated to Anhui Medical University, Lujiang Road No. 17, Hefei, 230001, People’s Republic of China, Tel/Fax +86-551-62283863, Email [email protected] Anyou Wang, Department of Hematology, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Lujiang Road No. 17, Hefei, 230001, People’s Republic of China, Tel/Fax +86-551-62283863, Email [email protected]
Background: The significant heterogeneity of elderly AML patients’ biological features has caused stratification difficulties and adverse prognosis. This paper did a correlation study between their genetic mutations, clinical features, and prognosis to further stratify them.
Methods: 90 newly diagnosed elderly acute myeloid leukemia (AML) patients (aged ≥ 60 years) who detected genetic mutations by next-generation sequencing (NGS) were enrolled between April 2015 and March 2021 in our medical center.
Results: A total of 29 genetic mutations were identified in 82 patients among 90 cases with a frequency of 91.1%. DNMT3A, BCOR, U2AF1, and BCORL1 mutations were unevenly distributed among different FAB classifications (p < 0.05). DNMT3A, IDH2, NPM1, FLT3-ITD, ASXL1, IDH1, SRSF2, BCOR, NRAS, RUNX1, U2AF1, MPO, and WT1 mutations were distributed differently when an immunophenotype was expressed or not expressed (p< 0.05). NPM1 and FLT3-ITD had higher mutation frequencies in patients with normal chromosome karyotypes than abnormal chromosome karyotypes (p< 0.001, p=0.005). DNMT3A and NRAS mutations predicted lower CR rates. DNMT3A, TP53, and U2AF1 mutations were related to unfavorable OS. TET2 mutation with CD123+, CD11b+ or CD34- predicted lower CR rate. IDH2+/CD34- predicted lower CR rate. ASXL1+/CD38+ and SRSF2+/CD123- predicted shorter OS.
Conclusion: The study showed specific correlations between elderly AML patients’ genetic mutations and clinical features, some of which may impact prognosis.
Keywords: elderly AML, genetic mutation, FAB subtype, karyotype, immunophenotype, prognosis
Introduction
Acute myeloid leukemia is a malignant tumor of myeloid cells derived from bone marrow. Recent surveys show that the initiation and progression of AML are often related to genetic mutations that control multiple functions. For example, FLT3 and KIT promote the proliferation and survival of malignant cells. CEBPA, RUNX1, and NPM1 impair the differentiation and apoptosis of hematopoietic cells. DNMT3A, TET2, IDH1, and IDH2 regulate the epigenetic mechanism. NPM1, CEBPA, and GATA2 mutations predict favorable prognosis, FLT3-ITD, RUNX1, ASXL1, MLL, TP53, PHF6, and U2AF1 mutations predict adverse prognosis, especially FLT3-ITD, ASXL1, RUNX1, and TP53 mutations predict adverse prognosis under certain conditions.1–14 The Morphologic-Immunologic-Cytogenetic classification (MIC classification) is used to make a definitive diagnosis of AML. Many studies have focused on the correlation between MIC classification and prognosis. For example, karyotype analysis based on cytogenetics as an important reference marker for prognosis has been written into National Comprehensive Cancer Network (NCCN) and European Leukemia Net (ELN) guidelines.15,16 Among the common immunophenotypes of AML, CD19, CD38, and MPO are the immunophenotypes reported in the literature to be of favorable prognosis.17–20 The immunophenotypes that predict adverse prognosis include CD7, CD11b, CD34, CD56, and CD123.21–28 CD13, CD33, and CD117, which are particularly important for the diagnostic classification of AML patients, and their relations with prognosis are currently inconclusive.21 CD14 and CD64 are mainly expressed in M4 and M5 subtypes,29,30 and their associations with prognosis have been less reported. However, the MIC classification alone cannot effectively and accurately predict the prognosis. It also needs to be analyzed in conjunction with the genetic mutations of the patients.
AML is a senile disease (median age at diagnosis is 65–70 years).31 Unlike the precise current stratification of young and middle-aged AML patients, the clinical treatment of elderly patients is still ineffective, and their prognosis is adverse.32 In this paper, we did correlation studies with genetic mutations, clinical features, and prognosis comprehensively evaluated the clinical and biological characteristics of elderly AML patients, and provided some reference to this particular group’s prognosis and clinical treatment.
Methods
Patients
In this study, we enrolled 90 elderly (aged ≥ 60 years) AML (non-APL) patients who were newly diagnosed in the First Affiliated Hospital of University of Science and Technology of China (Anhui Provincial Hospital Affiliated to Anhui Medical University) and targeted NGS was performed on bone marrow (BM) from all enrolled patients between April 2015 and March 2021. According to the 2016 WHO classification of myeloid neoplasms and acute leukemia,33 these patients were diagnosed and classified. The clinical features of the patients, including age, gender, BM blast percentage, and so on. Details are shown in Table 1.
 |
Table 1 Clinical Characteristics |
NGS Testing
NGS testing was submitted to Shanghai Siteide Biotechnology Co., Ltd. 34 common AML genetic mutations were tested, including ASXL1, BCOR, BCORL1, CALR, CBL, CEBPA, CSF3R, DNMT3A, ETV6, EZH2, FLT3, GATA2, IDH1, IDH2, JAK2, KIT, KRAS, KMT2A, MPL, NPM1, NRAS, PDGFRA, PHF6, PIGA, RUNX1, SETBP1, SF3B1, SH2B3, SRSF2, TET2, TP53, U2AF1, WT1, and ZRSR2.
Definitions and Statistical Analysis
Overall survival (OS) was defined as the length of time between the date of diagnosis and the date of last follow-up or death. Relapse-free survival (RFS) was defined as the period from first complete remission to relapse, death, or the last follow-up time. According to the NCCN guidelines,15 the efficacy after the initial induction chemotherapy was defined classified as complete remission (CR), and non-remission (NR).
The chi-squared test or Fisher’s exact test was used to infer the correlation between categorical variables, and Mann Whitney U-test was used for continuous variables. Kaplan Meier analysis (Log rank test) and the COX proportional hazard regression analysis were used for survival analysis. SPSS 26.0 software was used for all statistical analysis, and differences with p<0.05 were considered significant.
Results
The Spectrum of Genetic Mutations in Elderly Patients with AML
As shown in Figure 1, a total of 29 genetic mutations were identified in 82 patients among 90 cases with a frequency of 91.1%. There were 17 genetic mutations in more than 5% of patients, the most commonly genetic mutation was TET2 (26.7%, 24/90), followed by DNMT3A (25.6%, 23/90), IDH2 (24.4%, 22/90), NPM1 (24.4%, 22/90), FLT3-ITD (18.9%, 17/90), CEBPA (15.6%, 14/90), ASXL1 (14.4%, 13/90), IDH1 (14.4%, 13/90), SRSF2 (14.4%, 13/90), BCOR (12.2%, 11/90), TP53 (11.1%, 10/90), NRAS (8.9%, 8/90), RUNX1 (8.9%, 8/90), U2AF1 (7.8%, 7/90), BCORL1 (7.8%, 7/90), WT1 (7.8%, 7/90), and FLT3-TKD (7.8%, 7/90).
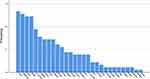 |
Figure 1 Mutation frequency of each gene in 90 elderly AML patients. |
Association of Genetic Mutations with Clinical Features of Elderly AML Patients
There were 17 genetic mutations in more than 5% of patients. We studied the relationships of these genetic mutations with clinical features of elderly AML patients, including MIC classification, cytogenetic risk, the origin of disease, and response to chemotherapy (Supplementary Tables S1 and S2). Overview of gene mutations, some clinical features (FAB classification, chromosome karyotypes, cytogenetic risk, response to chemotherapy) and overall survival in elderly AML are shown in Figure 2.
Association of Genetic Mutations with MIC Classification of Elderly AML Patients
In this study, in terms of analyzing the association between gene mutation and FAB classification, we excluded 20 cases that failed to get a specific FAB classification and conducted the study on the remaining 70 elderly AML patients. We studied the relationships of gene mutations with FAB classification of elderly AML patients and found that DNMT3A, BCOR, U2AF1, and BCORL1 mutations were unevenly distributed among different subtypes (p<0.05). DNMT3A had the highest mutation frequency in M5 subtype (50%, 13/26), followed by M4 subtype (40%, 2/5), and was rare in M1 and M2 subtypes (p=0.007). BCOR mutation mainly appeared in M5 (23.1%, 6/26), M2 (2.9%, 1/35), and was not found in M1 and M4 subtypes (p=0.048). U2AF1 and BCORL1 had the highest mutation frequency in M5 subtype (15.4%, 4/26; 19.2%, 5/26), and were rare in other subtypes (p=0.039, 0.014).
We then studied the relationship between genetic mutations and immunophenotypes and found that many genetic mutations were distributed differently when an immunophenotype was expressed or not expressed (p<0.05) (Supplementary Table S2). DNMT3A mutation was distributed differently in patients when CD123 was expressed (CD123+) or not expressed (CD123-), this difference was considered significant (p=0.036). The mutation-positive rate of IDH2 was different between CD7+ and CD7- patients (p=0.05), CD34+ and CD34- patients (p=0.033). The distributions of NPM1 mutation were different in patients with CD7+/CD7-, CD11b+/CD11b-, CD34+/CD34-, CD38+/CD38-, CD64+/CD64-, CD117+/CD117- (p=0.024, 0.002, <0.001, 0.012, 0.045, 0.03). The patients with CD34+/CD34-, CD64+/CD64-, CD123+/CD123- had different distributions of FLT3-ITD mutation (p=0.016, 0.035, 0.009). ASXL1 mutation had different distributions in patients with CD33+/CD33-, CD56+/CD56- (p=0.035, 0.028). The distributions of IDH1 mutation varied according to different patients who were CD33+/CD33-, CD123+/CD123- (p=0.035, 0.006). The distributions of SRSF2 mutation in of patients with CD33+ differed from the patients with CD33- (p=0.035). Among the patients with CD34+ or CD34-, BCOR mutation distributed differently (p=0.031). The distributions of NRAS mutation were different in patients with CD11b+/CD11b-, CD14+/CD14-, CD34+/CD34-, CD117+/CD117- (p=0.001, 0.014, 0.035, 0.008). RUNX1 mutation was distributed differently in patients with CD33+ and CD33- (p=0.042). The patients with MPO+ had different distributions of U2AF1 mutation from the patients with MPO- (p=0.004). The distributions of WT1 mutation varied from patients with CD56+ to CD56- (p=0.048) and patients with CD123+/CD123- was the same way (p=0.039).
We studied the relationships of genetic mutations with chromosome karyotypes of elderly AML patients and found that NPM1 and FLT3-ITD mutations were unevenly distributed among different chromosome karyotypes (p<0.001, p=0.005). NPM1 had a higher mutation frequency in patients with normal chromosome karyotypes (36.2%, 21/58) than abnormal chromosome karyotypes (3.1%, 1/32). The distributions of FLT3-ITD mutation were different in patients with normal chromosome karyotypes (27.6%, 16/58) and abnormal chromosome karyotypes (3.1%, 1/32).
Association of Genetic Mutations with Other Clinical Features of Elderly AML Patients
According to the 2017 ELN risk stratification, 90 elderly AML patients were classified into three risk groups: favorable-risk, intermediate-risk, and high-risk.16 We studied the relationships of genetic mutations with cytogenetic risk. We found that NPM1, CEBPA, ASXL1, TP53, NRAS, RUNX1, and U2AF1 mutations were unevenly distributed among different risk groups (p<0.001, p=0.002, p<0.001, p<0.001, p=0.037, p<0.001, p=0.008). NPM1, CEBPA, and NRAS mutations mainly appeared in favorable-risk group (50%, 20/40; 30%, 12/40; 15%, 6/40). ASXL1, TP53, RUNX1, and U2AF1 mutations mainly appeared in high-risk group (40.7%, 11/27; 37%, 10/27; 29.6%, 8/27; 18.5%, 5/27).
Acute myeloid leukemia was divided into three types according to the origins of the disease. De novo AML was defined as a disease without previous chemotherapy treatment or hematological disorders. Secondary AML (s-AML), AML with previous hematological disorders. Therapy-related AML (t-AML), AML related to the history of chemotherapy or toxic chemicals. We studied the relationship between genetic mutations and the origins of disease and found no significant difference in genetic mutations among each root.
After one or more cycles of induction chemotherapy, 47 patients achieved complete remission and 43 patients did not. Regarding the response to chemotherapy, 90 elderly AML patients were classified into two groups: CR and NR. We studied the relationships of genetic mutations with response to chemotherapy of elderly AML patients and found that DNMT3A, NPM1, and NRAS mutations were unevenly distributed among different groups (p=0.015, 0.028, 0.025). They all had higher mutation frequency in NR-group (37.2%, 16/43; 34.9%, 15/43; 16.3%, 7/43) than CR-group (14.9%, 7/47; 14.9%, 7/47; 2.1%, 1/47).
Genetic Mutation Predicted Rate of Complete Remission and Survival
We evaluated the impact of single genetic mutation on the rate of complete remission in elderly AML patients. In the total cohort of 90 elderly AML patients, the rate of CR was significantly lower in patients with DNMT3A (30.4% vs 59.7%, p=0.015) or NRAS mutation (12.5% vs 56.1%, p=0.025) than in those with wild type. And in the 63 patients in the low and intermediate-risk group, patients with DNMT3A (31.3% vs 63.8%, p=0.023) or NRAS mutation (12.5% vs 61.8%, p=0.018) also had a significantly lower rate of CR than those without the above genetic mutations.
Our study evaluated the impact of a single genetic mutation on the survival of elderly AML patients. We found DNMT3A mutation predicted significantly unfavorable OS in the total cohort of 90 elderly AML patients (1-year OS: 21.7% vs 47.8%, p=0.029) and the 63 patients in the low and intermediate-risk group (1-year OS: 25% vs 55.3%, p=0.036). In the total cohort of 90 elderly AML patients, TP53 mutation had a trend of inferior OS (1-year OS: 10% vs 45%, p=0.043), and mutant U2AF1 was also related to an unfavorable OS (1-year OS: 0 vs 44.6%, p=0.039).
Univariate survival analysis showed that DNMT3A, TP53, NRAS, and U2AF1 mutations predicted shorter OS (p=0.013, Figure 3A; p=0.021, Figure 3B; p=0.002, Figure 3C; p<0.001, Figure 3D); NPM1 predicted longer RFS (p=0.043, Figure 4A); RUNX1, U2AF1, WT1, and FLT3-TKD mutations predicted shorter RFS (p=0.02, Figure 4B; p<0.001, Figure 4C; p=0.015, Figure 4D; p=0.012, Figure 4E).
Association of Genetic Mutation with MIC Classification Predicted Rate of Complete Remission and Survival
There were specific correlations between elderly AML patients’ genetic mutations and MIC classification, including FAB subtype, immunophenotype, and chromosome karyotype. We evaluated the impacts of these correlations on complete remission rate and survival in elderly AML patients. The complete remission rate was distributed differently among different subtypes (M5: 12.5%, M2: 66.7%, M4: 0; p=0.043) in patients with TET2 mutation. The CR rate was significantly different between patients with CD123+/CD123- (20% vs 64.3%, p=0.047), CD11b+/CD11b- (0 vs 57.9%, p=0.041), and CD34+/CD34- (66.7% vs 11.1%, p=0.013) when TET2 was mutant. The complete emission rate was significantly different between patients with CD34+/CD34- (75% vs 20%, p=0.01) when IDH2 was mutant. In patients with ASXL1 mutation, CD38+ predicted shorter OS than CD38- (1-year RFS: 0 vs 66.7%, p=0.038). When SRSF2 was mutant in patients, CD123+ predicted longer OS than CD123- (1-year OS: 80% vs 12.5%, p=0.032). But the association of genetic mutations with chromosome karyotypes did not impact the CR rate and survival of elderly AML patients in this study.
Multivariate Analysis of Survival of Elderly AML Patients
Variables including BM blast percentage, WBC count, platelet count, the origin of disease, response to chemotherapy, induction chemotherapy, and genetic mutations were included in the multivariate analysis. For OS, platelet count less than 63×109/L, failure to achieve CR after 3 or more cycles of induction chemotherapy (NR), DNMT3A mutation, and TP53 mutation were independent unfavorable factors. For RFS, platelet count less than 63×109/L, RUNX1 mutation, U2AF1 mutation, and FLT3-TKD mutation were independent unfavorable factors (Table 2).
 |
Table 2 Multivariate Analysis for Survival of New Diagnosed Elderly AML Patients |
Discussion
Elderly AML patients have significant heterogeneity, often accompanied by adverse karyotype and various comorbidities, and have a low response rate to standard chemotherapy. Especially patients older than 75 years have shorter OS.34 Therefore, it is still essential to comprehensively evaluate the clinical and biological characteristics of elderly AML patients and analyze the correlations among them to make more accurate diagnostic classification and risk stratification. In this paper, we correlated genetic mutations with their MIC classification and other clinical features in elderly AML patients, and further analysis was done in combination with prognosis.
Previous studies have shown that FLT3-ITD, RUNX1, ASXL1, MLL, TP53, PHF6, and U2AF1 mutations in adult AML patients predict adverse prognosis.19 However, the impact of these genes on prognosis still needs further exploration in elderly patients. In addition to TP53 and U2AF1 mutations, we found that DNMT3A mutation significantly predicted inferior OS. RUNX1, U2AF1, and FLT3-TKD mutations were independent unfavorable factors for RFS. And TET2 mutation is an unfavorable prognostic factor for RFS in AML,35,36 but there are few studies on its association with CR rate. Our study found that TET2 mutation with CD123+ or CD11b+ in elderly AML patients predicted a low CR rate. We speculate that the adverse effects of CD123 and CD11b on prognosis may be related to their resulting lower CR rate.
DNMT3A mutation significantly predicted a lower CR rate and inferior OS. We also found that DNMT3A was common in M5 and M4 subtypes, and had a higher mutation frequency in patients with CD123+ than CD123-. Considering the adverse impacts of DNMT3A mutation and CD123+ on elderly AML patients,28 we need to pay more attention to patients with DNMT3A mutation and CD123+, and further explore follow-up treatment. And we found that IDH2 mutation had a higher mutation frequency in patients with CD34- than CD34+. The CR rate was significantly lower in patients with CD34- than CD34+, especially when IDH2 or TET2 was mutant in our study, this differed from previous studies in which CD34 predicted adverse prognosis.21 CD34 may interact with IDH2 or TET2 mutations, reducing each other’s negative effects on prognosis. NPM1 and CEBPA mutations were widely reported as favorable prognostic factors of survival in AML.2 Our study found they mainly appeared in the favorable-risk group, NPM1 mutation had a higher mutation frequency in patients with normal chromosome karyotypes than abnormal, and NPM1 mutation was associated with CD7-, CD11b+, CD34-, CD38+, CD64+, and CD117-. However, our study did not find a predictive impact of these associations on CR rate and overall survival. Previous studies have shown that FLT3-ITD mutation predicts an adverse prognosis.2 In this study, it was common in CD34-, CD64+, and CD123+ patients. The prognostic significance of CD64 has been less reported. CD64 may be associated with FLT3-ITD mutation, which predicts an adverse prognosis. FLT3-ITD mutation also had a higher mutation frequency in patients with normal chromosome karyotypes than abnormal. ASXL1 mutation mainly appeared in the high-risk group, was common in CD33- and CD56- patients in this study. CD38 was reported to be related to a favorable prognosis.18 While in our study, patients with ASXL1 mutation and CD38+ had inferior OS. We found IDH1 mutation was common in CD33- and CD123- patients, while SRSF2 mutation was also more associated with CD33- than CD33+, which had no association with prognosis in AML in our study. CD123 predicts an adverse prognosis.28 Yang et al suggested that SRSF2 mutation was not an independent prognostic factor in AML patients and not be associated with unfavorable prognosis in Chinese AML patients.37 In our study, when SRSF2 was mutant in patients, CD123+ might predict longer OS than CD123-. These results suggested that when SRSF2 was mutant in elderly AML patients, CD123 might not be associated with an adverse prognosis. Terada et al suggested that BCOR or BCORL1 gene mutation predicted inferior OS and RFS,38 In our study, BCOR mutation appeared in patients with CD34+ and not CD34-, BCOR and BCORL1 mutations both had the highest mutation frequency in the M5 subtype. Further explorations of these associations with prognosis will be completed in our subsequent research.
Consistent with previous studies,5 TP53 mutation mainly appeared in a high-risk group and also had a trend of inferior OS in our study. In terms of response to chemotherapy, NRAS had high mutation frequency in NR-group and predicted lower CR rate, but mainly appeared in the favorable-risk group. It was common in CD11b+, CD14+, CD34-, CD117- patients. Further study is needed to determine the impact of NRAS mutation on the prognosis. RUNX1 mutation mainly appeared in a high-risk group, might be an independent unfavorable factor for RFS, and was more common in patients with CD33- than CD33+. Considering the adverse impacts of RUNX1 mutation, we should pay more attention to patients with CD33-. In our study, consistent with previous studies,13 U2AF1 mutation had also the same trend of inferior OS, which was more common in patients with MPO- than MPO+. And we found it had the highest mutation frequency in the M5 subtype, so we should pay more attention to these associations. Zheng et al suggested that WT1 mutation predicted lower CR rate, inferior OS, and RFS.39 In our study, WT1 mutation was associated with CD56- and CD123+. In addition to the adverse impact on the prognosis of FLT3-ITD mutation,2 we found that FLT3-TKD mutation was also an independent prognostic risk factor.
In this study, multiple clinical features such as FAB classification, immunophenotype, and chromosome karyotype were associated with their gene mutations from multiple angles and dimensions. Then these associations were also analyzed with prognosis, and some results worthy of reference, such as our study first found that TET2 mutation with CD123+ or CD11b+ in elderly AML patients predicted a low CR rate, and CD64 may be associated with FLT3-ITD mutation, which predicts an adverse prognosis. We also found that when SRSF2 was mutant in patients, CD123+ might predict longer OS than CD123-. Therefore, we should pay attention to these three groups of elderly AML. We hope our work will contribute to prognostic prediction systems and improve the outcomes of elderly AML patients through targeted treatment.
Conclusion
The study showed specific correlations between elderly AML patients’ genetic mutations and clinical features, some of which impact prognosis.
Data Sharing Statement
The datasets used and analyzed in this study are available from the corresponding authors upon reasonable request.
Ethics Approval and Informed Consent
This study was approved, and the written informed consent was waived by the ethics committee of the first affiliated hospital of University of Science and Technology of China (2022-RE-064) due to the retrospective nature of the review, and confirmed that the data was anonymized and maintained with confidentiality. The study was conducted in accordance with the Declaration of Helsinki.
Acknowledgments
The authors thank the patients, their families, and all doctors who treated the patients.
Funding
This work was supported by the Key Research and Development Program Project of Anhui Province [No. 201904a07020102], the National Natural Science Foundation of China [No. 81600107] and the Anhui Provincial Natural Science Foundation [No. 1708085MH180].
Disclosure
The authors report no conflicts of interest in this work.
References
1. Narayanan D, Weinberg OK. How I investigate acute myeloid leukemia. Int J Lab Hematol. 2020;42(1):3–15. doi:10.1111/ijlh.13135
2. Yang F, Anekpuritanang T, Press RD. Clinical utility of next-generation sequencing in acute myeloid leukemia. Mol Diagn Ther. 2020;24(1):1–13. doi:10.1007/s40291-019-00443-9
3. Patnaik MM. The importance of FLT3 mutational analysis in acute myeloid leukemia. Leuk Lymphoma. 2018;59(10):2273–2286. doi:10.1080/10428194.2017.1399312
4. Ishikawa Y, Kawashima N, Atsuta Y, et al. Prospective evaluation of prognostic impact of KIT mutations on acute myeloid leukemia with RUNX1-RUNX1T1 and CBFB-MYH11. Blood Adv. 2020;4(1):66–75. doi:10.1182/bloodadvances.2019000709
5. De Kouchkovsky I, Abdul-Hay M. Acute myeloid leukemia: a comprehensive review and 2016 update. Blood Cancer J. 2016;6(7):e441. doi:10.1038/bcj.2016.50
6. Gaidzik VI, Teleanu V, Papaemmanuil E, et al. RUNX1 mutations in acute myeloid leukemia are associated with distinct clinico-pathologic and genetic features. Leukemia. 2016;30(11):2160–2168. doi:10.1038/leu.2016.126
7. Falini B, Brunetti L, Martelli MP. How I diagnose and treat NPM1-mutated AML. Blood. 2021;137(5):589–599. doi:10.1182/blood.2020008211
8. Ley TJ, Ding L, Walter MJ, et al. DNMT3A mutations in acute myeloid leukemia. N Engl J Med. 2010;363(25):2424–2433. doi:10.1056/nejmoa1005143
9. Cimmino L, Dolgalev I, Wang Y, et al. Restoration of TET2 function blocks aberrant self-renewal and leukemia progression. Cell. 2017;170(6):1079–1095.e20. doi:10.1016/j.cell.2017.07.032
10. DiNardo C, Lachowiez C. Acute myeloid leukemia: from mutation profiling to treatment decisions. Curr Hematol Malig Rep. 2019;14(5):386–394. doi:10.1007/s11899-019-00535-7
11. Gong XY, Wang Y, Liu BC, et al. Characteristics and prognosis in adult acute myeloid leukemia patients with MLL gene rearrangements. Chinese Journal of Hematology. 2018;39(1):9–14. doi:10.3760/cma.j.issn.0253-2727.2018.01.003
12. Van Vlierberghe P, Patel J, Abdel-Wahab O, et al. PHF6 mutations in adult acute myeloid leukemia. Leukemia. 2011;25(1):130–134. doi:10.1038/leu.2010.247
13. Ohgami RS, Ma L, Merker JD, et al. Next-generation sequencing of acute myeloid leukemia identifies the significance of TP53, U2AF1, ASXL1, and TET2 mutations. Mod Pathol. 2015;28(5):706–714. doi:10.1038/modpathol.2014.160
14. Barbosa K, Li S, Adams PD, Deshpande AJ. The role of TP53 in acute myeloid leukemia: challenges and opportunities. Genes Chromosomes Cancer. 2019;58(12):875–888. doi:10.1002/gcc.22796
15. Pollyea DA, Bixby D, Perl A, et al. NCCN guidelines insights: acute myeloid leukemia, version 2.2021. J Natl Compr Canc Netw. 2021;19(1):16–27. doi:10.6004/jnccn.2021.0002
16. Döhner H, Estey E, Grimwade D, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129(4):424–447. doi:10.1182/blood-2016-08-733196
17. Hurwitz CA, Raimondi SC, Head D, et al. Distinctive immunophenotypic features of t(8;21)(q22;q22) acute myeloblastic leukemia in children. Blood. 1992;80(12):3182–3188. doi:10.1182/blood.V80.12.3182.3182
18. Keyhani A, Huh YO, Jendiroba D, et al. Increased CD38 expression is associated with favorable prognosis in adult acute leukemia. Leuk Res. 2000;24(2):153–159. doi:10.1016/S0145-2126(99)00147-2
19. Kamijo R, Itonaga H, Kihara R, et al. Distinct gene alterations with a high percentage of myeloperoxidase-positive leukemic blasts in de novo acute myeloid leukemia. Leuk Res. 2018;65:34–41. doi:10.1016/j.leukres.2017.12.006
20. Matsuo T, Kuriyama K, Miyazaki Y, et al. The percentage of myeloperoxidase-positive blast cells is a strong independent prognostic factor in acute myeloid leukemia, even in the patients with normal karyotype. Leukemia. 2003;17(8):1538–1543. doi:10.1038/sj.leu.2403010
21. Mason KD, Juneja SK, Szer J. The immunophenotype of acute myeloid leukemia: is there a relationship with prognosis. Blood Rev. 2006;20(2):71–82. doi:10.1016/j.blre.2005.08.002
22. Plesa C, Chelghoum Y, Plesa A, et al. Prognostic value of immunophenotyping in elderly patients with acute myeloid leukemia: a single-institution experience. Cancer. 2008;112(3):572–580. doi:10.1002/cncr.23219
23. Lee YJ, Huang YT, Kim SJ, et al. Adenovirus viremia in adult CD34(+) selected hematopoietic cell transplant recipients: low incidence and high clinical impact. Biol Blood Marrow Transplant. 2016;22(1):174–178. doi:10.1016/j.bbmt.2015.08.019
24. Testa U, Fossati C, Samoggia P, et al. Expression of growth factor receptors in unilineage differentiation culture of purified hematopoietic progenitors. Blood. 1996;88(9):3391–3406. doi:10.1182/blood.V88.9.3391.bloodjournal8893391
25. Raspadori D, Damiani D, Lenoci M, et al. CD56 antigenic expression in acute myeloid leukemia identifies patients with poor clinical prognosis. Leukemia. 2001;15(8):1161–1164. doi:10.1038/sj.leu.2402174
26. Juncà J, Garcia-Caro M, Granada I, et al. Correlation of CD11b and CD56 expression in adult acute myeloid leukemia with cytogenetic risk groups and prognosis. Ann Hematol. 2014;93(9):1483–1489. doi:10.1007/s00277-014-2082-4
27. Kita K, Miwa H, Nakase K, et al. Clinical importance of CD7 expression in acute myelocytic leukemia. The Japan Cooperative Group of leukemia/lymphoma. Blood. 1993;81(9):2399–2405. doi:10.1182/blood.V81.9.2399.2399
28. Pinheiro LHS, Trindade LD, Costa F de O, et al. Aberrant phenotypes in acute myeloid leukemia and its relationship with prognosis and survival: a systematic review and meta-analysis. Int J Hematol Oncol Stem Cell Res. 2020;14(4):274–288. doi:10.18502/ijhoscr.v14i4.4484
29. Kamps WA, Humphrey GB. Heterogeneity among the acute nonlymphocytic leukemias: value of immunophenotype for diagnosis, prognosis, and therapy. Pediatr Hematol Oncol. 1988;5(1):17–28. doi:10.3109/08880018809031247
30. Krasinskas AM, Wasik MA, Kamoun M, Schretzenmair R, Moore J, Salhany KE. The usefulness of CD64, other monocyte-associated antigens, and CD45 gating in the subclassification of acute myeloid leukemias with monocytic differentiation. Am J Clin Pathol. 1998;110(6):797–805. doi:10.1093/ajcp/110.6.797
31. Prassek VV, Rothenberg-Thurley M, Sauerland MC, et al. Genetics of acute myeloid leukemia in the elderly: mutation spectrum and clinical impact in intensively treated patients aged 75 years or older. Haematologica. 2018;103(11):1853–1861. doi:10.3324/haematol.2018.191536
32. Keiffer G, Palmisiano N. Acute myeloid leukemia: update on upfront therapy in elderly patients. Curr Oncol Rep. 2019;21(8):71. doi:10.1007/s11912-019-0823-1
33. Arber DA, Orazi A, Hasserjian R, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–2405. doi:10.1182/blood-2016-03-643544
34. Klepin HD, Estey E, Kadia T. More versus less therapy for older adults with acute myeloid leukemia: new perspectives on an old debate. Am Soc Clin Oncol Educ Book. 2019;39:421–432. doi:10.1200/edbk_239097
35. Cher CY, Leung GMK, Au CH, et al. Next-generation sequencing with a myeloid gene panel in core-binding factor AML showed KIT activation loop and TET2 mutations predictive of outcome. Blood Cancer J. 2016;6(7):e442. doi:10.1038/bcj.2016.51
36. Wang RQ, Chen CJ, Jing Y, et al. Characteristics and prognostic significance of genetic mutations in acute myeloid leukemia based on a targeted next-generation sequencing technique. Cancer Med. 2020;9(22):8457–8467. doi:10.1002/cam4.3467
37. Yang J, Yao DM, Ma JC, et al. The prognostic implication of SRSF2 mutations in Chinese patients with acute myeloid leukemia. Tumour Biol. 2016;37(8):10107–10114. doi:10.1007/s13277-015-4716-0
38. Terada K, Yamaguchi H, Ueki T, et al. Usefulness of BCOR gene mutation as a prognostic factor in acute myeloid leukemia with intermediate cytogenetic prognosis. Genes Chromosomes Cancer. 2018;57(8):401–408. doi:10.1002/gcc.22542
39. Zheng YT, Li BX, Sun YJ, et al. Expression of WT1 gene in bone marrow of patients with acute myeloid leukemia and its influence on prognosis. Journal of Experimental Hematology. 2016;24(3):649-654. doi:10.7534/j.issn.1009-2137.2016.03.003
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



