Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 14
COPD patients’ experiences, self-reported needs, and needs-driven strategies to cope with self-management
Authors Sigurgeirsdottir J , Halldorsdottir S , Arnardottir RH , Gudmundsson G , Bjornsson EH
Received 10 January 2019
Accepted for publication 16 April 2019
Published 16 May 2019 Volume 2019:14 Pages 1033—1043
DOI https://doi.org/10.2147/COPD.S201068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Jonina Sigurgeirsdottir,1,2 Sigridur Halldorsdottir,3 Ragnheidur Harpa Arnardottir,3–5 Gunnar Gudmundsson,1,6 Eythor Hreinn Bjornsson2
1Faculty of Medicine, University of Iceland, Reykjavik, Iceland; 2Reykjalundur Rehabilitation Center, Mosfellsbaer, Iceland; 3School of Health Sciences, University of Akureyri, Akureyri, Iceland; 4Department of Rehabilitation, Akureyri Hospital, Akureyri, Iceland; 5Department of Medical Sciences, Respiratory-, Allergy-, and Sleep Research, Uppsala University, Uppsala, Sweden; 6Department of Respiratory Medicine, Landspitali University Hospital, Reykjavik, Iceland
Background: COPD is a common cause of morbidity and mortality. The aim of this study was to explore patients’ experiences, self-reported needs, and needs-driven strategies to cope with self-management of COPD.
Patients and methods: In this phenomenological study, 10 participants with mild to severe COPD were interviewed 1–2 times, until data saturation was reached. In total, 15 in-depth interviews were conducted, recorded, transcribed, and analyzed.
Results: COPD negatively affected participants’ physical and psychosocial well-being, their family relationships, and social life. They described their experiences of COPD like fighting a war without weapons in an ever-shrinking world with a loss of freedom at most levels, always fearing possible breathlessness. Fourteen needs were identified and eight clusters of needs-driven strategies that participants used to cope with self-management of COPD. Coping with the reality of COPD, a life-threatening disease, meant coping with dyspnea, feelings of suffocation, indescribable smoking addiction, anxiety, and lack of knowledge about the disease. Reduced participation in family and social life meant loss of ability to perform usual and treasured activities. Having a positive mindset, accepting help and assuming healthy lifestyle was important, as well as receiving continuous professional health care services. The participants’ needs-driven strategies comprised conducting financial arrangements, maintaining hope, and fighting their smoking addiction, seeking knowledge about COPD, thinking differently, facing the broken chain of health care, and struggling with accepting support. Procrastination and avoidance were also evident. Finally, the study also found that participants experienced a perpetuating cycle of dyspnea, anxiety, and fear of breathlessness due to COPD which could lead to more severe dyspnea and even panic attacks.
Conclusion: COPD negatively affects patients’ physical and psychosocial well-being, family relationships and, social life. Identifying patients’ self-reported needs and needs-driven strategies can enable clinicians to empower patients by educating them to improve their self-management.
Keywords: COPD, patients’ needs, self-management, pulmonary rehabilitation, qualitative research
Introduction
COPD is a common cause of morbidity and mortality worldwide. Its disease trajectory is characterized by a gradual decline in health and progressive organ failure, with acute exacerbations and decreased chances of survival.1–3 Studies have shown a correlation between acute exacerbations of COPD and depression and anxiety.4 However, more research is needed to determine the association between dyspnea and patients’ biopsychosocial well-being.5 The struggle experienced by patients with COPD is characterized by uncertainty, chaos, fluctuations in health, and multiple setbacks. They also struggle to cope with the necessity of managing multiple medications and comorbidities.3 Thus, there is a chance that the therapeutic needs of COPD patients may not be met by medication therapy alone, but rather by continuous and flexible interdisciplinary treatment.6,7 According to the GOLD guidelines,8 the disease is most often connected with tobacco smoking and studies have found that shame because of suffering from a self-inflicted disease is the main factor that delays or hinders COPD patients in taking action against their smoking habits.9 Self-management (SM) for COPD is a construct that has gained attention in the extant rehabilitation literature. SM is individuals’ active management of a chronic illness in collaboration with their family members and clinicians.10 SM interventions involve education, physical therapy, and monitoring and the results of studies conducted in relation to SM have emphasized the importance of patients being in control of their own life.11–13 Studies also imply that delays in the introduction of SM can lead to patients being readmitted to hospital more frequently.14 Pulmonary rehabilitation (PR) has proven effective for patients at every stage of COPD, improving quality of life and functional status by reducing symptoms of COPD.2,8,15,16 The GOLD guidelines have conceptualized PR as a set of interventions aimed at improving COPD patients’ SM through a comprehensive patient assessment and patient‐tailored therapies.8 The key concepts of PR are according to Spruit et al17 a comprehensive intervention, thorough patient assessment and patient-tailored therapies that aim at improving COPD patients’ physical and psychological health, and promoting their long-term health-enhancement through SM-oriented resources like exercise training, behavior modification and education, not only combined with hospital or special clinics. In addition, physical exercise should be initiated during acute hospitalization, and a follow-up should be provided after discharge by a pulmonary specialist, and a specialized pulmonary nurse to monitor and recognize signs of exacerbation over the course of the disease.2,16 In spite of the presence of useful clinical guidelines for the effective management of COPD, implementation of said guidelines appears to be lacking. Thus, there is a strong likelihood that COPD patients neither receive appropriate SM education nor receive timely assessments for PR.18 As patient-centered services gain acceptance in the field of rehabilitation, a new ideology has been proposed by Sigurgeirsdottir and Halldorsdottir,19 whereby in preparation for rehabilitation, an evaluation of the patient’s well-being is central. This evaluation is based on the patient–clinician relationship, with a particular focus on the patient’s view of what they need.19,20 In spite of informative results from a review on the shifting roles of patients from passive to active consumers,21 research on patients’ needs has been lacking in the extant literature.22 In preparation for this study, only a few studies were found to focus on the needs of patients.6,20,23–25 Thus, the research question of the present study was to explore COPD patients’ experiences, self-reported needs, and needs-driven strategies to cope with SM.
Material and methods
The research methodology used to answer the research question was the Vancouver School of Doing Phenomenology (hereafter referred to as the Vancouver School). The Vancouver School is a methodology comprised of a unique blend of phenomenology, hermeneutics, and constructivism, and its roots can be traced to Spiegelberg’s26 work on phenomenology, Ricoeur’s27,28 work on hermeneutic phenomenology, and Schwandt’s29 work on constructivism. The Vancouver School focuses on increasing knowledge and understanding of human phenomena. The aim of the school is to improve services, such as health care services, by exploring participants’ experiences.30
Data collection and analysis
The research process in the Vancouver School is characterized by semi-structured in-depth interviews with 5–15 participants, and 1–2 interviews with each participant, often 12–15 interviews conducted altogether.30 The research process in the Vancouver School is further characterized by seven cognitive elements that are established as a circular process. This process is repeated throughout the research (Figure 1). The implementation of the study is presented in 12 research steps (Table 1). The Vancouver School views the interviews with each participant as a crucial aspect of the case study, and the method of the Vancouver School is based on an analysis of individual cases (steps 1–7) followed by an inter-case analysis (steps 8–12). The results are then extracted (deconstruction) and assembled into a single reconstruction for the overall presentation of the results (reconstruction). Through text analysis methods, researchers can develop an understanding of the topic at hand and communicate said understanding to others. To effectively achieve this outcome, researchers need to use abstract thought-processes, especially reasoning, intuition, and introspection.30 In this study, a total of 15 interviews were conducted by the first author with 10 COPD patients (3 women, 7 men). Participants’ age ranged between 59 and 74 years and their smoking history ranged between 20 and 120 pack-years. Each participant was the subject of 1–2 interviews that ranged from 28 to 58 mins, and each transcribed interview ranged from between 8 pages (2,968 words) to 18 pages (8,759 words). Data saturation was accomplished when enough data had been gathered to enable researchers to answer the research question; in all 52,800 words of interview research data. Table 1 provides further information about the methods of data collection and analysis used in the study.
 | Table 1 The 12 research steps of the Vancouver School of Doing Phenomenology, and how these steps were followed in the present study |
 | Figure 1 The Vancouver School of Doing Phenomenology. The Vancouver School involves 12 steps, and in each step, the cycle is repeated.Note: Modified from Halldorsdottir S. The Vancouver School of doing Phenomenology. In: Fridlund BHCE, editor. Qualitative Research Methods in the Service of Health. Lund: Studentlitteratur; 2000: page 56.30 |
Study settings and participants
Patients who were on the waiting list for PR at a medium-sized rehabilitation center were consecutively invited to take part in the study until data saturation was accomplished. The PR at this particular rehabilitation center is smoke-free, and smoking cessation therapy is included in the PR program. The inclusion criteria were the diagnosis of ICD-10 J44.9, which represents COPD, ≥18 years of age, and not diagnosed with cancer. The mean age of the 10 participants was 69.2 years; 5 participants lived alone, and 5 lived with a spouse. Fev1 ranged from 21% to 83% of predicted value, representing GOLD guidelines stage I–IV where I is a mild disease and IV is most severe.8 The participants in this study had mild (n=1), moderate (n=3), or severe (n=6) COPD. All had visited a physician because of their lung problems in the year prior to the study, and five of them had visited a physician two or more times in the year prior to the study. More information about the participants is presented in Table 2.
 | Table 2 Overview of the participants’ characteristics |
Ethical considerations
Ethical clearance was obtained from the Icelandic National Bioethics Committee (reference number: 17–120). The researchers set strict requirements for informed consent: The participants must have voluntarily agreed to be involved, and they must have been fully aware of what they were consenting to. It was explained, both in written form and orally, what the study was about. The consent form clearly stated that participation could be stopped at any time.
Results
COPD negatively affected the participants’ physical and psychosocial well-being as well as their family relationships and social life. The participants described their experiences of being a COPD patient as being similar to fighting a war without weapons in an ever-shrinking world with loss of freedom at most levels and always being afraid of possible breathlessness. The study identified 14 needs (Table 3) and 8 clusters of needs-driven strategies that participants used to cope with SM of COPD (Figure 2). The participants’ needs-driven coping strategies include helpful and unhelpful aspects. The helpful strategies comprise conducting financial arrangements, maintaining hope, and fighting their smoking addiction, seeking knowledge about COPD, thinking differently, facing the broken chain of healthcare, and struggling with accepting support. Coping with the reality of COPD, a life-threatening disease, meant coping with dyspnea, feelings of suffocation, indescribable smoking addiction, anxiety, and lack of knowledge about the disease. Having a positive mindset, accepting help and assuming healthy lifestyle was important, as well as receiving continuous professional health care services. Unhelpful strategies were also applied as some participants’ main coping-strategy when they were unable to find more helpful solutions. Procrastination and avoidance are examples of such strategies that are evident and described by the participants as their tendency to procrastinate fearful things like stopping smoking and avoiding participation in former treasured activities like family and social life. Finally, the study also found a perpetuating cycle of dyspnea, anxiety, and fear of breathlessness (Figure 3) among patients. This cycle often led to more severe dyspnea and even panic attacks.
 | Table 3 Needs identified by the participants |
 | Figure 2 Participants’ self-management needs when coping with COPD, their needs-driven coping strategies, and other available strategies. |
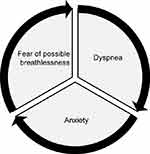 | Figure 3 The perpetuating cycle of dyspnea, anxiety, and fear of possible breathlessness that can cause a panic attack. |
Coping with the reality of COPD, a life-threatening disease
It was clear that the participants were coping with multiple losses because of their COPD like reduced participation in family and social life and loss of ability to perform usual treasured activities. When asked to consider possible reasons for their COPD, most of the participants believed it was due to their smoking habit. Despite the knowledge that smoking was likely to lead to lung disease, the diagnosis of COPD had struck them as an “unforeseen collapse,” [Participant 1, hereafter [P1], and all the participants described their sense of powerlessness in coping with COPD. The importance of “not giving up” [P1] was mentioned by several participants, as well as “learning to breathe better,” [P2] “accepting PR,” [P2] and using some aids and equipment that could improve things for them. The reality of COPD and participants’ inability to work and earn money was hard for them to accept, and subsequent financial worries were prominent in some participants’ stories. COPD also negatively affected the participants’ physical and psychosocial well-being.
Coping with dyspnea: feelings of suffocation and low-energy levels
The participants felt that their most urgent need was learning how to cope with dyspnea, constant feelings of suffocation, and loss of energy. They felt they were “suddenly transmuted into an elderly person” [P1&3] and stated that shortness of breath was the most difficult aspect of COPD. All the participants were afraid of possible breathlessness, and even the thought of possible energy deprivation and oxygen desaturation before partaking in exercise could lead them to experience stress and anxiety. For some, this stress became so severe that they panicked or became “maddened with fear” [P10]. “Because of the fear, you need help to start physical exercise again. At first, I was literally scared to death, because I had experienced that the breath stopped and then the fear grasps you at once.“ [P10]
Coping with an ever-shrinking world: the loss of freedom
As their COPD progressed, many participants found that their disease made their world smaller, and they struggled to cope with their loss of freedom. Carrying out simple tasks necessitated many breaks, and being forced to stay at home because of their dyspnea or need for long-term oxygen therapy was difficult for them. Gradually, fewer activities became feasible for them, and formerly important activities became impossible. All the participants experienced a tendency to procrastinate and feel bitter and shameful, and many resented that COPD affected their way of being and thinking. “As soon as I start some physical activity, my heart starts beating wildly, and my oxygen saturation drops down… that is why it becomes so comfortable just to remain sitting in the corner” [P2].
Coping with an indescribable smoking addiction: committing a slow suicide
All the participants had a long history of smoking; their pack-years averaged more than 60. Most of them had known for a long time that they would benefit from ceasing their smoking habit. They had tried to stop smoking at least once and for them, their addiction was indescribable, and they felt controlled by an “unbelievable tobacco dependency,” [P2&10], metaphorically described by a participant in the following way: “I have known it for about 40 years, that I have been committing… a slow suicide… through the tobacco. That is what every smoker knows” [P3]. Some participants were surprised with how achieving abstinence eventually became incredibly easy. For one participant, seeing a chest radiograph of her lungs was a very powerful motivator to achieve abstinence:
I never saw an x-ray of my own lungs until I went to [the lung specialist] some 2–3 years ago. Then I first saw how my lungs looked, and he explained to me what was wrong and how he would have liked to see them… it was shocking! I would have liked to have seen it… sooner and have this fine explanation that I was given. Then I understood this fully. What… I… had… done, I wish that people could have such education… sooner. [P1]
Coping with the lack of knowledge: the importance of being told the truth
The participants’ knowledge about COPD and its prognosis varied. Some felt that education regarding the disease had been provided too late. They stated that their desire to know about the disease was a prerequisite for SM. While many participants used the internet as a source of education, their internet searches were sometimes unfruitful. Thus, the participants mostly depended on their lung specialist or general practitioner (GP) for education. Dependency on other health care professionals was also mentioned, especially specialized physical therapists and nurses. The participants also emphasized the “importance of being told the truth” [P2] about the disease, and the provision of possible coping strategies was an important aspect of SM. “I regret having started [smoking] for the first time.“ [P1].
Coping with the need for a positive mindset and healthy lifestyle
The participants strove not to dwell in self-pity, and many had found their own way of changing negative feelings into positive ones. They worked to be thankful, look forward to things, break negative habits, and not let regret bring them down. They tried to view COPD as a project they needed to cope with: “COPD is only a project. I have decided not to think about it in any other way” [P5]. “You have to face the reality and respond to it” [P3]. The participants expressed the necessity of continuing with their normal activities, such as having fun, gardening, meeting friends, and going out for coffee. “You have it all in your hands to turn it into something positive for yourself, not to take the other road [of social isolation]” [P2]. The participants were aware of their own responsibilities for their lifestyle, mobility, sleep, and eating habits. Maintaining a reasonable weight was a challenge, particularly after they ceased smoking, and it was important to be on guard against feelings of anxiety and financial stress. “Changing their mindset” [P2] and “sorting things out” [P2] were phrases used by participants who felt lucky “not needing to smoke” [P5] anymore. Some mentioned the importance of developing new habits, especially physical exercise: “I would say that the number 1 coping strategy is physical exercise” [P10].
Coping with the need for good healthcare: the importance of continuity in professional healthcare practice
The participants voiced a need to be known by their health professionals, particularly their lung specialists and GPs. Having regular follow-ups was important to participants, and some mentioned the need for a regular condition check. Some had experienced effective services that involved personal connections with health care professionals who organized regular follow-ups, including physical therapists who conducted pulmonary exercises and lung specialists or nurses who gave them a sense of security by being accessible. Some participants criticized the health care provided by GPs, where they had experienced a lack of interest and continuity.
Coping with the need for help and social support: maintaining hope and courage
While the disease negatively affected participants’ physical and psychosocial well-being as well as their family relationships and social life, they valued the support they received from friends and family. Their willingness to talk openly about COPD was an important milestone. “I have a friend who has the same disease [COPD]. We often have long talks and support each other” [P1]. The participants had their own ways of coping with the daily challenges of COPD. They stated that learning to live with the disease without surrendering to it involved maintaining hope and not becoming discouraged. This meant coping with changing roles and accepting help with routine tasks, such as going to the grocery store. Some of the male participants referred to their wives as being huge sources of support. Some male participants also said that their wives were responsible for taking care of managing their COPD medications. It is clear that the participants also placed great trust in their lung specialists. Some participants had been reluctant to accept the offer of rehabilitation and even explained that they had not been able to bear the thought of being pushed into ceasing their smoking habits. The support they received from family members was often very important:
Going to rehabilitation causes me so much anxiety… and when the telephone rang, I had a bit of a shock! The time had come… but then I just called my daughters and they said, “Mum, that will just be good for you.” [P2]
Discussion
This study adds knowledge to the extant literature and deepens understanding regarding patients experiences of having COPD, their needs, and their needs-driven strategies to cope with SM. Participants described their experiences of COPD as being similar to fighting a war without weapons in an ever-shrinking world with a loss of freedom at most levels, always fearing possible breathlessness that could even evolve into a panic attack. This study found that COPD negatively affected the participants’ physical and psychosocial well-being as well as their family relationships and social life. The results of this study concur with some researchers, who have called for patients’ psychosocial needs to be deemed as important as medication and breathing exercises.20 This study identified 14 needs and 8 clusters of needs-driven strategies that the participants used to cope with SM which has been called for in the literature.6,7,20,22–25
The current literature provides a relatively substantive view of dyspnea as the main symptom of COPD from a medical perspective.2 The results of this study confirm the findings from a previous study, which stated that participants are confronted with a perpetuating cycle of fear of dyspnea, which leads to anxiety, which leads to breathlessness, which leads to more severe dyspnea, which, for some, evolves into a panic attack.20 The participants clearly explained how their fear can lead to hypo-activity, bitterness, procrastination, and reluctance to participate in formerly important activities. This has also been indicated in recent studies.22,31 The results of this study contribute new information to the perpetuating cycle of COPD and we call for further studies into the biopsychosocial attributes of dyspnea, as other researchers have also done.5,24,32 This study also clearly outlines participants’ pleas for help and ideas about additional solutions while it highlights the unfilled educational gap (in spite of existing COPD guidelines) concerning severe nicotine addiction, early-onset COPD, and the progress of COPD. The results reveal that for many participants, nicotine addiction was “incredible.” Although all the participants knew that quitting smoking was a vitally important way of improving their health, putting that theory into practice was troublesome. Other researchers have also come to similar conclusions and we ponder if earlier and more focused interdisciplinary interventions for smoking cessation are needed.22,33 For many participants, their reluctance to stop smoking was perhaps owing to the shame they felt in relation to their self-inflicted disease, as has been suggested in another study.9 This needs to be further explored. Being diagnosed with COPD imposed on participants the need to learn how to cope with their dyspnea, energy deprivation, and multiple losses regarding former activities, work and pleasure, as well as gradually increasing despair. This despair was related to the participants’ ever-shrinking world, caused by the decline in physical activity, which has been addressed in other studies.4,6 Better adherence to clinical guidelines regarding guided physical training might be helpful and would benefit from further investigation, as suggested by other researchers.9,24 A focus on the patients’ worries in relation to their inability to work and earn money is relatively new in the literature, but COPD patients’ financial worries have been mentioned in relation to funding their COPD care.20,32 The results of this study support previous findings regarding the importance of the patient–clinician relationship and advanced care planning.1 The results also support the need for a more focused interdisciplinary team to work in rehabilitation services and SM support, as suggested in another study.34 The results indicate, as previously suggested, that coping with COPD must be viewed as a process that takes time: learning how to cope with life when suffering from COPD and maintaining hope is important, and changing roles may necessitate accepting help with difficult tasks.22,24 Based on the findings of this study, it can be said that some COPD patients lack the appropriate SM education, and assessment for PR as needed, which has already been identified by other researchers.18 The expressed needs for personal contact and continuity in health care services confirm the findings of a previous qualitative study.19 The study also indicates that the therapeutic needs of some COPD patients’ may not be fulfilled by traditional lung-disease therapy alone, but rather by continuous and flexible interdisciplinary treatment.6,7,24 Whereas this study focused on COPD patients’ experiences, self-reported needs, and needs-driven strategies to cope with SM, there is a need for conducting a study to explore the experiences of family members and clinicians of having a significant other or a patient that suffers from COPD and what has helped them to enhance the COPD patients’ SM.
Implications for clinical practice
The current results contribute to the field, as they highlight the need for the provision of appropriate SM education for COPD patients. From the list of coping needs identified by the participants in this study, a practical checklist was developed and designed to form the basis for clinicians’ dialogue with COPD patients so as to empower said patients in SM (Table 4). The checklist is seen by the authors as “food for thought” and may promote the necessary dialogue concerning patients’ needs and needs-driven strategies for SM.
 | Table 4 The participants’ needs as COPD patients: a practical checklist as a basis of dialogue between clinicians and patients |
Strengths and limitations
The strength of this study is that it provides valuable insights into the complicated situations of patients with COPD. It may be considered a limitation that all participants were recruited from a waiting list for PR, indicating a certain population bias, as only a minority of COPD patients is referred to PR.35 The fact that the rehabilitation clinic in question includes compulsory smoking cessation in the PR-program might also have affected the view of the participants.
Conclusion
COPD negatively affects patients’ physical and psychosocial well-being, as well as their family relationships and social life. Being diagnosed with COPD imposes on participants the need to learn how to cope with their smoking addiction, dyspnea, energy deprivation, and the gradually increasing despair that accompanies the disease. Identifying COPD patients’ self-reported needs and needs-driven strategies may provide clinicians with better tools to empower them to cope with SM.
Acknowledgments
We would like to extend our sincere thanks to the participants for sharing their experiences. We are thankful to the Oddur Ólafsson Fund and the B-Section of the Scientific Fund of INA for their financial support. We would also like to thank the Rehabilitation Center for cooperating with us throughout the study.
Author contributions
All the authors were responsible for the study conception and design. The first author conducted the interviews. All authors contributed to data analysis, drafting and revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work. The first author wrote the first draft of the paper, and the other authors critically reviewed the paper and approved it.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Janssen DJ, Engelberg RA, Wouters EF, Curtis JR. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns. 2012;86(1):19–24. doi:10.1016/j.pec.2011.01.007
2. Gudmundsson G. [Acute exacerbations of chronic obstructive pulmonary disease - review]. Laeknabladid. 2015;101(7–8):357–362.
3. Kendall M, Carduff E, Lloyd A, et al. Different experiences and goals in different advanced diseases: comparing serial interviews with patients with cancer, organ failure, or frailty and their family and professional carers. J Pain Symptom Manag. 2015;50(2):216–224. doi:10.1016/j.jpainsymman.2015.02.017
4. Pooler A, Beech R. Examining the relationship between anxiety and depression and exacerbations of COPD which result in hospital admission: a systematic review. Int J Chron Obstruct Pulmon Dis. 2014;9:315–330. doi:10.2147/COPD.S60179
5. Hayen A, Herigstad M, Pattinson KT. Understanding dyspnea as a complex individual experience. Maturitas. 2013;76(1):45–50. doi:10.1016/j.maturitas.2013.09.002
6. Giacomini M, DeJean D, Simeonov D, Smith A. Experiences of living and dying with COPD: a systematic review and synthesis of the qualitative empirical literature. Ont Health Technol Assess Ser. 2012;12(13):1–47.
7. Christensen VL, Rustoen T, Cooper BA, et al. Distinct symptom experiences in subgroups of patients with COPD. Int J Chron Obstr. 2016;11:1801–1809. doi:10.2147/COPD.S105299
8. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report. GOLD executive summary. Am J Respir Crit Care Med. 2017;195(5):557–582. doi:10.1164/rccm.201701-0150WS
9. Arne M, Emtner M, Janson S, Wilde-Larsson B. COPD patients perspectives at the time of diagnosis: a qualitative study. Prim Care Respir J. 2007;16(4):215–221. doi:10.3132/pcrj.2007.00033
10. Schulman-Green D, Jaser SS, Park C, Whittemore R. A metasynthesis of factors affecting self-management of chronic illness. J Adv Nurs. 2016;72(7):1469–1489. doi:10.1111/jan.12902
11. Huygens MW, Vermeulen J, Swinkels IC, Friele RD, van Schayck OC, de Witte LP. Expectations and needs of patients with a chronic disease toward self-management and eHealth for self-management purposes. BMC Health Serv Res. 2016;16:232. doi:10.1186/s12913-016-1484-5
12. Richardson J, DePaul V, Officer A, et al. Development and evaluation of self-management and task-oriented approach to rehabilitation training (START) in the home: case report. Phys Ther. 2015;95(6):934–943. doi:10.2522/ptj.20130235
13. Bourbeau J,van der Palen J. Promoting effective self-management programmes to improve COPD. Eur Respir J. 2009;33(3):461–463. doi:10.1183/09031936.00001309
14. Jonkman NH, Westland H, Trappenburg JC, et al. Characteristics of effective self-management interventions in patients with COPD: individual patient data meta-analysis. Eur Respir J. 2016;48(1):55–68. doi:10.1183/13993003.01860-2015
15. Ryrso CK, Godtfredsen NS, Kofod LM, et al. Lower mortality after early supervised pulmonary rehabilitation following COPD-exacerbations: a systematic review and meta-analysis. BMC Pulm Med. 2018;18(1):154. doi:10.1186/s12890-018-0718-1
16. Arnardottir RH, Boman G, Larsson K, Hedenstrom H, Emtner M. Interval training compared with continuous training in patients with COPD. Respir Med. 2007;101(6):1196–1204. doi:10.1016/j.rmed.2006.11.004
17. Spruit MA, Singh SJ, Garvey C, et al. An official American Thoracic Society/European Respiratory Society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care. 2013;188(8):e13–e64. doi:10.1164/rccm.201309-1634ST
18. Halding AG, Grov EK. Self-rated health aspects among persons living with chronic obstructive pulmonary disease. Int J Chronic Obstr. 2017;12:1163–1172. doi:10.2147/COPD.S129325
19. Sigurgeirsdottir J, Halldorsdottir S. Existential struggle and self-reported needs of patients in rehabilitation. J Adv Nurs. 2008;61(4):384–392. doi:10.1111/j.1365-2648.2007.04531.x
20. Gardiner C, Gott M, Payne S, et al. Exploring the care needs of patients with advanced COPD: an overview of the literature. Respir Med. 2010;104(2):159–165. doi:10.1016/j.rmed.2009.09.007
21. McMullan M. Patients using the Internet to obtain health information: how this affects the patient-health professional relationship. Patient Educ Couns. 2006;63(1–2):24–28. doi:10.1016/j.pec.2005.10.006
22. Apps LD, Harrison SL, Mitchell KE, Williams JEA, Hudson N, Singh SJ. A qualitative study of patients‘ experiences of participating in SPACE for COPD: a self-management programme of activity, coping and education. ERJ Open. 2017;3(4):1–11.
23. Ek K, Sahlberg-Blom E, Andershed B, Ternestedt BM. Struggling to retain living space: patients‘ stories about living with advanced chronic obstructive pulmonary disease. J Adv Nurs. 2011;67(7):1480–1490. doi:10.1111/j.1365-2648.2010.05604.x
24. Russell S, Ogunbayo OJ, Newham JJ, et al. Qualitative systematic review of barriers and facilitators to self-management of chronic obstructive pulmonary disease: views of patients and healthcare professionals. NPJ Prim Care Respir Med. 2018;28(1):2. doi:10.1038/s41533-017-0069-z
25. Harb N, Foster JM, Dobler CC. Patient-perceived treatment burden of chronic obstructive pulmonary disease. Int J Chronic Obstr. 2017;12:1641–1652. doi:10.2147/COPD.S130353
26. Spiegelberg H. The Phenomenological Movement: A Historical Introduction by Herbert Spiegelberg.
27. Ricoeur P, ed. Existence and Hermeneutics (translated by K. McLaughlin). London: Routledge & Kegan Paul; 1980. BJ, editor. Contemporary Hermeneutics: hermeneutics as method, philosophy and critique.
28. Ricoeur P. Hermeneutics and the Human Sciences: Essays on Language, Action and Interpretation (edited, translated and introduced by JB T, editor). Cambridge: Cambridge University Press; 1990.
29. Schwandt T, editor. Constructivist, Interpretivist Approaches to Human Inquiry. Thousand Oaks CA: Sage; 1994. Denzin NK LYE, editor. Handbook of Qualitative Research.
30. Halldorsdottir S. The Vancouver School of doing Phenomenology. In: Fridlund BHCE, editor. Qualitative Research Methods in the Service of Health. Lund: Studentlitteratur; 2000:46–81.
31. Lindqvist G, Hallberg LRM. Feelings of guilt due to self-inflicted disease. J Health Psychol. 2010;15(3):456–466. doi:10.1177/1359105309353646
32. Norweg A, Collins EG. Evidence for cognitive-behavioral strategies improving dyspnea and related distress in COPD. Int J Chronic Obstr. 2013;8:439–451. doi:10.2147/COPD.S30145
33. Jonsdottir R, Jonsdottir H. The experience of women with advanced chronic obstructive pulmonary disease of repeatedly relapsing to smoking. Scand J Caring Sci. 2007;21(3):297–304. doi:10.1111/scs.2007.21.issue-3
34. Wortz K, Cade A, Menard JR, et al. A qualitative study of patients‘ goals and expectations for self-management of COPD. Prim Care Respir J. 2012;21(4):384–391. doi:10.4104/pcrj.2012.00070
35. Rochester CL, Vogiatzis I, Holland AE, et al. An Official American Thoracic Society/European Respiratory Society Policy Statement: enhancing implementation, use, and delivery of pulmonary rehabilitation. A J Respir Crit Care. 2015;192(11):1373–1386. doi:10.1164/rccm.201510-1966ST
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
