Back to Journals » Clinical Ophthalmology » Volume 17
Conventional Phacoemulsification Surgery Versus Femtosecond Laser Phacoemulsification Surgery: A Comparative Analysis of Cumulative Dissipated Energy and Corneal Endothelial Loss in Cataract Patients
Authors Léda RM , Machado DCS, Hida WT , Motta AFP, Pacini TDF, Amorim RF
Received 18 March 2023
Accepted for publication 8 June 2023
Published 19 June 2023 Volume 2023:17 Pages 1709—1716
DOI https://doi.org/10.2147/OPTH.S408717
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Rayssa Medeiros Léda,1 Daniela Cristina Schroff Machado,2 Wilson Takashi Hida,3 Antônio Francisco Pimenta Motta,4 Thiago de Faria Pacini,5 Rivadavio Fernandes Amorim1
1Department of Medical Sciences, Universidade de Brasília (UnB), Brasília, DF, Brazil; 2Department of Ophthalmology, Luz Hospital de Olhos e Laser, Goiânia, Goiás, Brazil; 3Department of Ophthalmology, Hospital Oftalmológico de Brasília, Brasília, DF, Brazil; 4Department of Ophthalmology, Rita Lavinia Hospital Dia, Salvador, Bahia, Brazil; 5Department of Ophthalmology, Hospital Pacini, Brasília, DF, Brazil
Correspondence: Rivadavio Fernandes Amorim, Pós-Graduação em Ciências Médicas, Faculdade de Medicina, Universidade de Brasília, Campus Darcy Ribeiro, Asa Norte, Brasília, DF, CEP: 70910-900, Brasil, Tel +55 61 3107-1913 ; +55 61 981533379, Email [email protected]
Purpose: To analyze whether femtosecond laser-assisted surgery leads to less cumulative dissipated energy (CDE) and decreased endothelial cell loss compared to conventional surgery.
Patients and Methods: This non-blinded, non-randomized, quasi-experimental clinical trial was conducted at one center and involved one surgeon. Patients with cataracts and 50– 80 years old were included, and the exclusion criteria were radial keratotomy, trabeculectomy, drain tube implant, corneal transplant, posterior vitrectomy, and re-implantation of intraocular lens. In total, 298 patients were recruited between October 2020 and April 2021, and the data collected included sex, laterality, age, ocular comorbidities, systemic comorbidities and CDE. An endothelial cell count was performed before and after surgery. Patients were divided according to femtosecond laser-assisted phacoemulsification or conventional phacoemulsification. The femtolaser patients were submitted to the equipment, and then, immediately after treatment, phacoemulsification surgery was performed. In the conventional method, the “divide and conquer” technique was used. The statistical analysis was made using an analysis of covariance linear model, using SAS version 9.4 (SAS Institute, Inc., 1999). Values with p < 0.05 were considered significant.
Results: A total of 132 patients were analyzed. The only statistically relevant predictors of CDE were the severity of the cataract (p < 0.0001) and age of ≥ 75 years (p = 0.0003). The following factors were not significant: technique with or without laser (p = 0.6862), sex (p = 0.8897), systemic arterial hypertension (p = 0.1658), and diabetes (p = 0.9017). Grade 4 cataracts were associated with higher CDE than grade 3 cataracts, which in turn were associated with higher CDE than grade 2 cataracts. A comparison of pre- and post-operative specular microscopy with and without laser revealed no significant discrepancy (p = 0.5017).
Conclusion: Femtosecond laser-assisted cataract surgery did not reduce CDE or endothelial cell loss compared to conventional surgery regardless of severity.
Keywords: laser therapy, lasers, cataract extraction, cataract
Introduction
Cataracts are a public health problem and the main cause of reversible visual loss. Approximately 41 to 52 million people worldwide are blind due to cataracts, and 18 million of them are bilaterally blind. In Brazil, 300.000 people or approximately 2% of the population are blind due to cataracts. Femtosecond laser-assisted cataract surgery (FLACS) was developed to be safer than conventional cataract surgery with more consistent results. FLACS consists of a real-time optical coherence tomography software program, which analyzes the eye from the anterior segment to the posterior capsule of the lens, and performs several steps of manual surgery to improve accuracy, safety, and refraction test results. Its technology is of fundamental relevance because the laser has a low-pulse intensity compared to other ophthalmic lasers, which allows for reduced energy dissipation and less collateral damage to the ocular tissues.1–3
The use of the FLACS is proposed to offer several advantages: reduction of effective phacoemulsification time; decrease of cumulative dissipated energy (CDE); lower rates of endothelial loss, corneal thickening, and edema; and attenuation of inflammation. It works by using ultrashort pulses of near-infrared light to disrupt the tissue with micrometer precision, providing minimal collateral damage.4
Reducing the effective phacoemulsification time assumes a lower energy load directed to the eye, which can be measured using CDE, which in turn can monitor the efficiency of cataract surgery, both in relation to the surgeon and the surgical center. CDE is an indicator of quality control and can be used to audit phacoemulsification. Its elevation correlates to increased operative time and postoperative recovery because of increased energy dissipation in the eye and increased tissue damage.5
The reduction in endothelial cell count can be caused not only by age, but often be seen as a result of cataract surgery, long-term contact lens wear, diabetes mellitus, inflammation, and keratoconus. In cataract surgery, endothelial cells can be damaged by instrument or intraocular lens contact, irrigation turbulence, movement of nuclear fragments, mechanical trauma from ultrasound waves, and increased thermal activity. A low CDE value during surgery translates into less energy used and is considered better for corneal recovery. However, a high CDE generates statistically significant corneal endothelial loss. A high amount of ultrasound energy used in phacoemulsification during cataract surgery leads to endothelial cell damage and corneal edema. The importance of lower ultrasound energy release in the procedure is well established in the literature, with evidence of reduced corneal edema and endothelial cell loss.6–8
A major issue to be clarified is whether using FLACS results in lower CDE and consequently less endothelial cell loss than those associated with conventional surgery. Owing to the increased life expectancy of the population, preserving the corneal endothelial cells, which are responsible for preventing stromal edema and maintaining corneal transparency, is of paramount importance to provide better long-term visual outcomes.6,7,9
In patients who have advanced cataracts and/or corneal endothelial dystrophies or require a high infusion volume and extensive operative time, the risk of endothelial damage is higher, making the use of laser as a great option for the treatment of these patients, especially because of the lower exposure of the ocular structures to ultrasonic energy.4,7
With today’s fast paced lifestyle demands, patients are eager to return to their workplaces and everyday activities as soon as possible. However, to evaluate from an economic point of view, FLACS has significant associated financial costs, including initial purchase costs of the laser itself, servicing, depreciation and the individual patient interfaces, which leads to question its financial viability, especially in health-care systems funded by the state. Schweitzer et al conducted a study in five university hospitals in France that analyzed the cost-effectiveness of laser use and concluded that FLACS was more expensive (with an additional average of 305 euros per surgery), less effective, and without clinical benefit. Roberts et al also concluded that using a previously established economic model, the FLACS service cost £ 144.60 more than conventional surgery per case.8,10,11
This study aimed to analyze whether the use of FLACS results in lower CDE and less loss of corneal endothelial cells than those associated with the conventional method, especially in cases of grade 2 or grade 3 cataracts that are not associated with other ocular comorbidities. Thus, hospitals could make precise indications for its use and optimize costs without generating losses in the quality of the results.12
Materials and Methods
This was a non-randomized (quasi-experimental), non-blinded clinical trial, conducted at a single center by a single professional. This study adheres to the principles of the Declaration of Helsinki and was approved by the Research Ethics Committee of Universidade de Brasília/DF (approval 4.242.627). As CNS Resolution No. 466/2012 was considered, the participants’ anonymity was maintained. Written informed consent was obtained from all the patients or their companions prior to surgery.
Patients with an indication for cataract surgery and aged between 50 and 80 years were included in the study. The exclusion criteria were the following preoperative ocular comorbidities: radial keratotomy, trabeculectomy, drainage tube implantation, corneal transplantation, posterior vitrectomy, and intraocular lens explantation or re-implantation.
Altogether, 298 patients were recruited between October 2020 and April 2021, and the sample was calculated using the EPI INFO TM VERSION 7.2.0.1 public domain software (http://www.cdc.gov/epiinfo/index.html) to reach the 95% confidence level. Patients were allocated to a group after joint discussion between the surgeon and patient, considering individual peculiarities. Subsequently, the patients were divided according to the scheduled surgical technique: femtosecond laser-assisted phacoemulsification or conventional phacoemulsification.
The performance of the laser procedure was not blinded, as the steps performed by the surgeon were visible at the time of surgery. However, the collection and analysis of the data obtained and the outcomes were performed by another professional. All the patients were evaluated at 1 and 7 days and 6 months postoperatively. Data collected included sex, laterality, age, ocular and systemic comorbidities, visual acuity, pre- and postoperative refraction and specular microscopy, and CDE.
Lens opacity grading was performed according to the Lens Opacities Classification System III (LOCS III). The CDE was obtained as a result of the product of the mean ultrasound (US) power by the US time per surgery, multiplied by 0.4 (because it was torsional US). The endothelial cell count was made before surgery and 6 months after the procedure, using EM-4000 Tomey specular microscope.13
The parameters defined when using the LenSx® femtolaser (Alcon, Fort Worth, TX, USA) were as follows: anterior capsulotomy of 4.9 mm; main corneal incision of 2.5 mm and secondary incision of 0.8 mm; fragmentation pattern of the lens of 14 J; distance of the anterior capsule of 500 μm and the posterior capsule of 800 μm; space of 10 μm between the laser application points and 14 μm between the horizontal layers; and diameter of the treatment area of 5.2 mm. Immediately after treatment, phacoemulsification surgery with the Centurion® Vision System (Alcon, Fort Worth, TX, USA) was performed. First, a hydrodissection was carried out to mobilize the cortical parts. Then, the pre-cut parts were removed. With the irrigation suction, the cortex could be removed until a clear lens capsule was available. At the end of the surgery, an intraocular lens was implanted in the capsular bag. In the conventional method, the main corneal incision measured 2.2 mm, and secondary incision 1 mm; the “divide and conquer” technique was used, finishing with the implantation of the intraocular lens.
Statistical Analysis
In the present study, the eyes of the same patient were matched to the same surgical technique. In the data analysis, correlation was considered to test the validity of the results. A propensity score was calculated for each patient using a logistic regression model for the use of the laser technique, in which the following independent variables were included: age, sex, and presence of systemic arterial hypertension and/or diabetes. Patients were matched 1 to 1 by propensity score using the “greedy” matching technique based on a calibration of 0.2 standard deviations (SDs) of the propensity score.
Continuous and qualitative variables are presented as means ± standard errors and frequencies (%), respectively. Techniques were compared using fitting linear mixed-effects models for continuous variables, binary logistic models with a generalized estimation equation (GEE) for binary qualitative variables, and logistic models of proportional odds with a GEE for ordinal qualitative variables. Napierian logarithmic transformation was employed for continuous variables that did not have a Gaussian distribution.
The means after surgery for some ophthalmologic parameters were compared between the techniques using a linear analysis of covariance mixed-effects models with an unstructured covariance structure. The dependent variable was the ophthalmologic measurements obtained postoperatively, the independent variable was the surgical technique used (with or without laser), and the covariate was the ophthalmologic measurements at baseline.
Mean CDE values were compared between techniques and cataract severity using linear mixed-effects models with an unstructured covariance structure. The model equation followed the standard form of a factorial experiment with main effects and the interaction of technique and severity. When the p-value of the interaction was significant, Bonferroni correction was used to fit the comparisons between the severity levels.
The linear mixed-effects multiple regression model with a random intercept and unstructured covariance structure was used to evaluate the effect on the CDE of the following independent variables: type of surgery, sex, age, cataract severity, and presence of hypertension and/or diabetes. P-values <0.05 were considered significant. Analyses were performed using SAS version 9.4 (SAS Institute, Inc., 1999).
Results
A total of 274 eyes (137 pairs) from 216 patients were analyzed. Of these, 240 eyes (192 patients) had no ocular comorbidities, which corresponded to 118 right eye and 122 left eye surgeries. After restricting the sample to patients without ocular comorbidities, and analyzing the propensity score, 168 procedures (132 patients) were performed: 82 right eyes and 86 left eyes. Data regarding age, sex, hypertension and/or diabetes after propensity scoring are presented in Table 1.
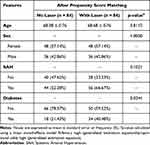 |
Table 1 Epidemiological Characteristics of the Sample After Propensity Score Matching |
The mean age ± SD of patients who underwent surgery with and without laser was similar at 68.68 ± 0.76 years and 68.38 ± 0.76 years, respectively (p = 0.81). Surgery without laser was performed on 48 women and 36 men, and the same number of men and women underwent surgery with laser (p = 1). In the surgeries without laser, 18 patients had diabetes and 66 did not have it. In the surgeries with laser, 34 patients had diabetes and 50 did not have it (p = 0.02).
The average CDE of cataracts operated on with and without laser and the number of cataracts considered to be grade 2, 3 or 4 after propensity scoring are recorded in Table 2. The mean CDE ± SD of cataracts operated on without laser was 7.03 ± 0.57, and with laser was 6.80 ± 0.55 (p = 0.80). A total of 52 (61.90%) grade 2 cataracts, 26 (30.95%) grade 3 cataracts, and 6 (7.14%) grade 4 cataracts were operated on using the conventional technique, and 42 (50.60%) grade 2 cataracts, 28 (33.73%) grade 3 cataracts, and 13 (15.66%) grade 4 cataracts were operated on using the femtosecond laser.
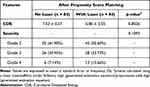 |
Table 2 Sample Characteristics by Technique Type After Propensity Score Matching |
After fitting the regression model, the only statistically relevant predictors of CDE that were identified were cataract severity (p < 0.0001) and age of ≥75 years (p = 0.0003). Grade 4 cataracts were associated with a higher CDE than that associated with Grade 3 cataracts, which, in turn, was associated with a higher CDE than that associated with Grade 2 cataracts. Patients aged <75 years had a lower CDE than that of patients above this age (p = 0.0003). The following factors were not significant: technique with or without laser (p = 0.67), sex (p = 0.89), hypertension (p = 0.17), and diabetes (p = 0.90).
Overall, 77 ocular comorbidities were identified, including 30 cases of glaucoma (38.9%), 16 post-refractive surgery (20.8%), 15 retinopathies (19.5%), 9 corneal pathologies (11.7%), 6 eyelid disorders (7.8%), and 1 amblyopia (1.3%).
The preoperative microscopy of patients who underwent conventional surgery revealed a mean ± SD of 2.605.27 ± 21.58 cells/mm2 in the preoperative period. In the adjusted postoperative period, 6 months after the surgeries, the mean ± SD was 2194.84 ± 70.82 cells/mm2, a 15.75% reduction in the endothelial cell count. Patients who opted to undergo laser treatment had a mean ± SD specular microscopy of 2607.88 ± 19.35 cells/mm2 preoperatively, and a postoperatively adjusted mean ± SD of 2256.21 ± 56.72 cells/mm2, which means a 13.48% decrease in the number of the endothelial cells. The difference between the groups was not considered significant (p = 0.50). Finally, we adjusted the CDE by age, sex, hypertension, and diabetes and paired the mean CDE values by severity and technique for maximum similarity to a randomized trial (Table 3).
 |
Table 3 Average CDE Values by Severity and Technique After Pairing: Mixed-Effects Linear Model Fitting Results |
After adjusting the data by the propensity score, grades 2, 3 and 4 cataracts that were operated using the conventional technique had a mean CDE ± SD of 5.17 ± 0.61, 8.79 ± 0.85, and 14.71 ± 1.72, respectively. Grades 2, 3 and 4 cataracts that were operated on using laser had a mean CDE ± SD of 4.73 ± 0.67, 6.77 ± 0.80, and 13.09 ± 1.16, respectively.
Discussion
This study found that the mean CDE value was significantly higher in patients aged ≥75 years than in patients aged <75 years (p = 0.0003). This is consistent to a review of cases in San Francisco and China by Bui et al, in which the mean age of the patients was 70.7 ± 10.6 years. Increased age of the operated patients was significantly associated with a higher CDE, especially when these patients were aged >70 years (increase of log CDE from 0.20 to 0.31, p < 0.001).14
The present discovery regarding diabetes was that the mean CDE values did not differ significantly between patients with and without diabetes (p = 0.90) or hypertension (p = 0.17). On the other hand, Bui et al reported that diabetes was associated with a higher intraoperative CDE (increase of log CDE of 0.07 in diabetes patients, p = 0.007).14
However, due to the propensity score matching, which focused on age and sex to almost randomize the sample, the number of diabetic patients in the laser group became 88.89% higher than the without laser group, which made them unbalanced in this point of view. Due to this issue, the disproportion of this feature makes it one of the limitations of the study.
In this study, paired data indicated that the mean CDE values according to cataract severity did not differ between the techniques (p = 0.55). However, although lacking in statistical significance, the CDE values for those treated with laser were always lower for the three severity levels than those observed in individuals treated without laser. Furthermore, the CDE score did not differ significantly between patients operated on with and without laser before and after pairing (p = 0.69).15
In contrast, Hida et al compared 400 surgeries performed with and without laser (two groups of 200) and reported a significant reduction in the CDE in femtosecond laser surgeries.
The possible factors that could justify this difference in results were mainly different methods of the nucleus fragmentation and parameters in FLACS. In the case of LenSx®, in the study by Hida et al, the cylindrical diameter was 6.0 mm, the fragmentation pattern of the lens was 12 µJ, and the separation of the layers was 20 µm, whereas they were 5.2 mm, 14 µJ, and 14 µm in the current study, respectively. As for the Centurion® parameters, Hida et al used the prechop technique, a suction rate of 35 cc/min, maximum vacuum of 350 mmHg, and torsional amplitude of 100%, whereas in the current study, they were 46 cc/min, 400 mmHg, and 70%, respectively.15
Similar to Hida et al, Mencucci et al reported that the CDE value of the conventional group was significantly higher than that of the FLACS group (9.72 ± 2.42 vs 7.99 ± 1.94, p = 0.017). However, in a study by Ang et al conducted in the Philippines, only the surgeries on grade 4 cataracts according to the LOCS III system had significantly reduced CDE in the FLACS group compared to those in the conventional surgery group.4,15
Bui et al analyzed the correlation between the increase in CDE according to cataract severity and reported that the more advanced the cataract, the greater the increase in CDE. Cataracts grade 2, 3, and 4 exhibited increased CDE (increase in log CDE of 0.12–0.41 from grade 2 cataracts, p < 0.001). Moreover, the mean CDE values differed significantly between at least two severity levels; the mean CDE of grade 2 cataracts was lower than that of grade 3 cataracts (p = 0.0174), which in turn was lower than that of grade 4 cataracts (p < 0.0001).14,16
Despite the findings of this study, there are some situations in which the use of FLACS is highly recommended. This device may be particularly beneficial in complex cases with greater risk for corneal endothelial decompensation, like hypermature cataracts, Fuchs dystrophy, highly brunescent nuclei and loose zonular, as it spares the zonules from the additional stress of manually tugging on the anterior capsule. These patients were part of exclusion criteria from the present study.17
In the current study, although the laser group had less endothelial cell loss (mean loss of 15.75% of cells in the group without laser vs 13.48% in those with laser), this difference was not significant. The percentage of endothelial cell loss in both groups was consistent with the findings in the literature: according to Mencucci et al, the reported losses vary between 4% and 25%, and according to Schoroeter’s et al, between 1.4% and 23%. In Schroeter’s study, there was a 12.7% cell loss in the FLACS group and a 17.4% loss in the conventional group.8,18
This wide range of corneal endothelial cell loss identified in the literature can possibly be due to intraoperative destructive toxic and mechanical variables, such as turbulent fluid flows, the solution volume, use of appropriate viscoelastic, turbulent lens fragments, ultrasonic energy from conventional ultrasound cataract surgery, effective phacoemulsification time, total surgery time, intraocular lens implantation, pharmacological influences and direct mechanical trauma from manipulations of instruments in the eye, all related to total case time and technique.8,18–20
Mencucci et al compared the corneal endothelial loss in conventional surgery versus FLACS and observed a greater loss in the conventional group at the three time points (7 days, 1 month, and 6 months postoperatively; all p < 0.05). When the density of endothelial cells was adjusted to the preoperative values, greater density was identified in the FLACS group at all three time points (all p < 0.05), suggesting that the laser generates less endothelial loss and also results in greater endothelial density in the immediate and late postoperative periods. Furthermore, endothelial cell loss is directly proportional to CDE and US power (r = 0.389, p = 0.013).18
However, Abell et al reported a significant reduction in endothelial cell loss and corneal edema in the early postoperative period after femtosecond laser surgery (1 day and 3 weeks). Nevertheless, at 6 months postoperatively, no significant difference was observed. Abell et al reported that any kind of stress, especially surgical stress, can increase edema and endothelial cell loss. The reason for the lower cell loss in the laser group may be the shorter total operative time and the consecutive reduction in phacoemulsifier power, causing less ultrasonic vibrations and therefore inducing a decrease in cell stress and incidence of postoperative corneal edema.19
Schroeter et al compared FLACS with the conventional method in terms of endothelial cells and found that gathering all grades of cataract, no statistically significant difference between the femtosecond laser and conventional group in terms of corneal endothelial cell count was observed. The only time that it was found a statistical difference was for grade 2 cataracts at 4 weeks post operation (p = 0.048); however, this difference was not considered statistically different anymore when it reached 12 weeks post operation (p = 0.093). Furthermore, we did not find differences in coefficient of variation of endothelial cell area and percentage of hexagonal cells between the two groups.8
Similar to these studies, Schweitzer et al observed no difference in endothelial cell counts in the CDE of FLACS or conventional surgeries. Moreover, no significant differences in corneal thickness and total US time were observed between the FLACS group and conventional surgery group. Regarding quality of life, Schweitzer et al have reported that cataract surgery increased the ability of patients to perform activities of daily living, regardless of the surgical technique used.10
Conclusion
The use of the femtosecond laser to assist in cataract surgery does not result in lower CDE compared to that associated with conventional surgery regardless of the severity of the cataract. Likewise, the endothelial cell associated with femtosecond laser surgery does not differ significantly from that associated with conventional surgery.
The limitations of the study were, at first, the unbalanced numbers of diabetic patients compared to the control group after propensity score matching; moreover, only the divide and conquer method of the nucleus fragmentation was used in this study, which could be an explanation for the difference among our results and another findings from literature, where direct chop or horizontal chop were applied.
Ethics Approval and Consent to Participate
The study was performed in accordance with the Declaration of Helsinki as well as accepted standards of ethics. The Ethics Committee of Research of University of Brasília (UnB N° 4.242.627) approved the study protocol.
Consent to Publish
All the patients provided written informed consent for the publication of their clinical data.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Carlos Carricondo P. Análise dos custos e complicações da cirurgia de catarata realizada por residentes [Analysis of costs and complications of cataract surgeries performed by residents]. [Doctoral dissertation]. Universidade de São Paulo; 2010. Portuguese.
2. Soares DAR. Laser de femtosegundo na cirurgia à catarata [Femtosecond laser in cataract surgery]. Mestrado Integrado em Medicina. Universidade do Porto; 2016.
3. Grewal DS, Schultz T, Basti S, Dick HB. Femtosecond laser-assisted cataract surgery-current status and future directions. Surv Ophthalmol. 2016;61(2):103–131. doi:10.1016/j.survophthal.2015.09.002
4. Mencucci R, De Vitto C, Cennamo M, Vignapiano R, Buzzi M, Favuzza E. Femtosecond laser-assisted cataract surgery in eyes with shallow anterior chamber depth: comparison with conventional phacoemulsification. BMJ Cataract Refract Surg. 2020;46(12):1604–1610. doi:10.1097/j.jcrs.0000000000000341
5. Chen M, Chen M. Comparison of CDE data in phacoemulsification between an open hospital-based ambulatory surgical center and a free-standing ambulatory surgical center. Clin Ophthalmol. 2010;4(1):1287–1289. doi:10.2147/OPTH.S15076
6. Chen M, Sweeney HW, Luke B, Chen M, Brown M. A retrospective randomized study to compare the energy delivered using CDE with different techniques and OZil® settings by different surgeons in phacoemulsification; 2009. Available from: http://www.dovepress.com/.
7. Popovic M, Campos-Möller X, Schlenker MB, Ahmed IIK. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14567 eyes. In: Ophthalmology. Vol. 123. Elsevier Inc.; 2016:2113–2126.
8. Schroeter A, Kropp M, Cvejic Z, Thumann G, Pajic B. Comparison of femtosecond laser-assisted and ultrasound-assisted cataract surgery with focus on endothelial analysis. Sensors. 2021;21:996. doi:10.3390/s21030996
9. Jaime Lozano Alcázar A, Del Valle México C, Jaime Lozano-Alcázar A. La cirugía de catarata hasta 1748 [Cataract surgery until 1748]. Cirugía y Cirujanos. 2001;69:1.
10. Schweitzer C, Brezin A, Cochener B, et al. Femtosecond laser-assisted versus phacoemulsification cataract surgery (FEMCAT): a multicentre participant-masked randomised superiority and cost-effectiveness trial; 2020. Available from: https://nextcloud.chu-bordeaux.
11. Roberts HW, Wagh VK, Mullens IJM, Borsci S, Ni MZ, O’Brart DPS. Evaluation of a hub-and-spoke model for the delivery of femtosecond laser-assisted cataract surgery within the context of a large randomised controlled trial. Br J Ophthalmol. 2018;102(11):1556–1563. doi:10.1136/bjophthalmol-2017-311319
12. Bartlett JD, Miller KM. The economics of femtosecond laser-assisted cataract surgery. Curr Opin Ophthalmol. 2016;27(1):76–81. doi:10.1097/ICU.0000000000000219
13. Moreno-Torres AJ. Faco microaxial con ultrasonido longitudinal. Revista Mexicana de Oftalmologia. 2014;88(1):20–24. doi:10.1016/j.mexoft.2014.04.003
14. Bui AD, Sun Z, Wang Y, et al. Factors impacting cumulative dissipated energy levels and postoperative visual acuity outcome in cataract surgery. BMC Ophthalmol. 2021;21(1). doi:10.1186/s12886-021-02205-w
15. Hida WT, Tzelikis PF, Vilar C, et al. Outcomes study between femtosecond laser-assisted cataract surgery and conventional phacoemulsification surgery using an active fluidics system. Clin Ophthalmol. 2017;11:1735–1739. doi:10.2147/OPTH.S136136
16. Shajari M, Rusev V, Mayer W, Diakonis V, Petermann K, Kohnen T. Impact of lens density and lens thickness on cumulative dissipated energy in femtosecond laser–assisted cataract surgery. Lasers Med Sci. 2019;34(6):1229–1234. doi:10.1007/s10103-019-02715-6
17. Ang RET, Quinto MMS, Cruz EM, Rivera MCR, Martinez GHA. Comparison of clinical outcomes between femtosecond laser-assisted versus conventional phacoemulsification. Eye Vision. 2018;5(1). doi:10.1186/s40662-018-0102-5
18. Mencucci R, Ponchietti C, Virgili G, Giansanti F, Menchini U. Corneal endothelial damage after cataract surgery: microincision versus standard technique. J Cataract Refract Surg. 2006;32(8):1351–1354. doi:10.1016/J.JCRS.2006.02.070
19. Abell RG, Kerr NM, Howie AR, Kamal MAAM, Allen PL, Vote BJ. Effect of femtosecond laser-assisted cataract surgery on the corneal endothelium. J Cataract Refract Surg. 2014;40(11):1777–1783. doi:10.1016/j.jcrs.2014.05.031
20. Conrad-Hengerer I, Al Juburi M, Schultz T, Hengerer FH, Dick HB. Corneal endothelial cell loss and corneal thickness in conventional compared with femtosecond laser–assisted cataract surgery: three-month follow-up. J Cataract Refract Surg. 2013;39(9):1307–1313. doi:10.1016/J.JCRS.2013.05.033
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
