Back to Journals » Open Access Journal of Contraception » Volume 14
Contraceptives Knowledge and Perception: A Cross-Sectional Study Among Future Pharmacists in Jordan
Authors Al-Shami KM , Al-Ashwal FY , Bitar AN , Alshakhshir S
Received 18 July 2023
Accepted for publication 8 October 2023
Published 24 October 2023 Volume 2023:14 Pages 159—167
DOI https://doi.org/10.2147/OAJC.S431243
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Igal Wolman
Kamal M Al-Shami,1,2 Fahmi Y Al-Ashwal,3,4 Ahmad Naoras Bitar,5 Sami Alshakhshir6
1Department of Clinical Pharmacy, Faculty of Pharmacy, Jordan University of Science and Technology, Irbid, Jordan; 2Division of Tumor Metabolism and Microenvironment, German Cancer Research Center, Heidelberg, Germany; 3Department of Clinical Pharmacy, College of Pharmacy, Al-Ayen University, Thi-Qar, Iraq; 4Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, University of Science and Technology, Sana’a, Yemen; 5Department of Clinical Pharmacy, Faculty of Pharmacy and Biomedical Sciences, Malaysian Allied Health Sciences Academy, Selangor, Malaysia; 6Department of Clinical Pharmacy, College of Pharmacy, Aqaba University of Technology, Aqaba, Jordan
Correspondence: Fahmi Y Al-Ashwal, Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, University of Science and Technology, Sana’a, Yemen, Tel +967-771661055, Email [email protected]
Background: Unintended pregnancy has huge burdens on healthcare resources and society. Contraception is essential to reduce it, and pharmacists are usually the first healthcare providers who are asked for advice about contraceptives. Therefore, the study aimed to evaluate future pharmacists’ knowledge, awareness, and perceptions of contraceptive methods and assess the factors influencing their knowledge, awareness, and perceptions.
Methods: This cross-sectional study was conducted among senior pharmacy students at four universities. Data was collected over three months using a structured and validated questionnaire. Both inferential (Mann–Whitney U-test and Kruskal–Wallis test) and descriptive analyses were employed.
Results: A total of 310 eligible participants completed the questionnaire, and more than half of them (N=172; 55.5%) were final-year students. The Mann–Whitney U-test revealed that final-year students had significantly better knowledge (U= 14,261.5, p< 0.002) and a higher level of awareness (U= 13,971.5, p< 0.007) than fourth-year students. Interestingly, the Kruskal–Wallis test showed that the type of training (hospital, community, none) had a statistically significant impact on awareness scores (p< 0.001).
Conclusion: Final-year students had higher knowledge and were more aware of contraception than fourth-year students. Also, community pharmacy training was associated with better awareness about contraceptives. Therefore, future studies should explore the impact of incorporating more targeted contraceptive education into earlier years of pharmacy education to bridge the knowledge gap observed between final-year and fourth-year students. Additionally, research should also investigate the effectiveness of specific community pharmacy training modules on contraceptive awareness.
Keywords: awareness, attitude, contraceptives, pharmacy students
Introduction
Unintended pregnancy is a serious global health problem.1 It is estimated that about 121 million unintended pregnancies occur worldwide yearly, and around 61% of these are ended in abortion.2 The unintended pregnancies are associated with many negative consequences for the family members, such as abortion-related morbidity and mortality,3 increased risks of parental stress, and maternal depression.4 In addition, the high percentages of unintended pregnancies negatively affect mothers and their families, health care systems, and the economy.5
Contraception, on the other hand, contributes greatly to the reduction of unintended pregnancies, with more than 300 million unintended pregnancies prevented in 2017 by the utilization of modern contraceptives.6 Moreover, contraception is vital in lowering the need for elective abortions and can prevent up to 15% of maternal fatalities caused by unsafe abortions.7 However, incorrect use of contraceptives may result in many unintended pregnancies.8 Several factors contribute to the underutilization and inadequate use of contraceptives. These include a lack of awareness, access challenges, insufficient information, erroneous beliefs, misconceptions about contraception techniques and services, and social restraints.9
Pharmacists contribute significantly to the safe and effective administration of medications, and they are frequently the first healthcare providers consulted by people seeking medical guidance.10 Pharmacists are also becoming increasingly important providers of family planning services. Pharmacists are not only responsible for dispensing contraceptives but, more importantly, for providing adequate consultations about them for the patients. As a result, good knowledge of future-to-be pharmacists about contraceptive methods is of vital importance for adequate practice.
Few studies have assessed medical students’ awareness of contraceptive options.11–13 However, data regarding pharmacy students’ knowledge in the Middle East is scarce, with no studies conducted in Jordan. Consequently, this study aimed to evaluate the senior pharmacy students’ knowledge, awareness, and perceptions of contraceptive methods. Additionally, we assessed the factors affecting knowledge, awareness, and perceptions among the study population. Senior pharmacy students were selected for this research as they are future-to-be pharmacists. Assessing their knowledge and perception of contraception at this stage can provide insight into their readiness to advise patients about contraception once they enter the field. Moreover, as future pharmacists, they will play a significant role in disseminating correct information about contraceptive methods. Therefore, understanding their current knowledge and perception of contraception could help educators and policymakers identify any knowledge gaps or misconceptions that need to be addressed in their education. Furthermore, in Jordan, discussing contraception can be considered sensitive. Young pharmacists need to be culturally sensitive and non-judgmental while providing contraceptive information and services. Identifying the knowledge gaps and assessing the students’ perceptions can help identify any biases or misconceptions that may affect their interactions with clients.
Methods
Design and Study Setting
This is a cross-sectional study conducted among the senior pharmacy students (fourth and fifth year) at four universities in Jordan: two private and two governmental universities. Data was collected over three months. A convenience sampling method was used to disseminate a structured, validated questionnaire. Respondents completed the questionnaire immediately and in the presence of researchers to ensure that their responses reflected their current knowledge and that the questions were understood.
Ethical Considerations
The institutional review board at Jordan University of Science and Technology granted ethical approval (82/126). Students were assured that their involvement in the study was entirely voluntary and their responses would remain anonymous. Written informed consent was obtained from participants before filling out the questionnaire.
Sample Size and Participants
In 2017, over 7000 undergraduates were enrolled in pharmacy programs throughout all Jordan universities at all levels.14 So assuming 40% of them (2800) are in the 4th and 5th years of study (our target population of senior pharmacy students), and using the Daniel’s sample size formula,15 at 95% confidence interval and 5% precision, and based on the assumption that 70% of senior pharmacy students will have optimal knowledge regarding contraception, the calculated sample size is 290. The targeted senior pharmacy students were categorized based on their level of study (4th and 5th year of study). Also, senior pharmacy students were classified according to their university into private and governmental universities.
Data Collection Tool and Scoring
For data collection, a self-validated questionnaire was utilized (S1 File). The questionnaire was adapted from a previous relevant study, and permission to use and modify was obtained from the authors.11 The questionnaire was content validated by three experts. These experts have substantial professional experience in various areas within clinical pharmacy, health education, questionnaire design, and validation, which enabled them to provide a comprehensive evaluation of the questionnaire. Minor suggestions were made to the original questionnaire. For validity, the questionnaire was given to 6 of the target participants (senior pharmacy students) to make sure the questions were clear and understandable. Finally, a pilot test was done among 25 pharmacy students. The reliability coefficient (Cronbach alpha) was acceptable (0.71).
The survey was made of four sections and was described in Table 1. Inferential analysis was used to see whether there was any difference in the scores of knowledge, awareness, and perception between the different demographic groups.
 |
Table 1 Description of the Questionnaire |
Statistical Analysis
The data analysis was performed using SPSS (version 25, IBM Corp., New York, USA). In this study, both inferential and descriptive analyses were employed. For categorical variables, frequency (percentages) was utilized; for continuous data, the median (IQR) was reported, as the data were not normally distributed. In order to analyze if there is any difference in knowledge scores between the groups of demographic data, the Mann–Whitney and Kruskal–Wallis tests were utilized. The data for these tests was presented as mean rank because the distribution of knowledge scores among groups of the independent variables is of different shapes.16 Significant differences were defined as those with P values < 0.05.
Results
Demographic Characteristics of Participants
A total of 310 (88.6%) participants completed the survey out of 350 distributed questionnaires. More than half of the senior students were final-year students (N= 172, 55.5%), and female participants represented almost two-thirds of the recruited sample (N= 200, 64.5%) (Table 2). The majority of participants were from private universities (N= 196, 63.2%), and most of them had community pharmacy training (N= 237, 76.5%).
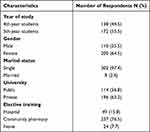 |
Table 2 The Sociodemographic Characteristics of the Study’s Participants |
The General Knowledge About Contraceptives
For the general knowledge about contraceptives, all participants have heard of contraceptives. Less than one-third (N= 98, 31.6%) of them thought that contraceptives could not reduce the risk of certain types of cancer (Table 3). Furthermore, 30.6% (N= 95) of participants believed that the effect of contraceptives or birth control pills could last for several months after discontinuation. Less than one-fifth of the participants (19%) had incorrect answers in relation to the effectiveness of male condoms in protecting against sexually transmitted diseases (STDs). Surprisingly, over half of the included subjects (56.1%) believed that a woman must have a pelvic exam before taking contraceptive pills. Other knowledge findings are presented in Table 3.
 |
Table 3 Knowledge Measurement of Contraceptive Methods |
Awareness of Contraception Methods
Table 4 shows the participants’ responses regarding the awareness of contraception methods. More than two-thirds of the included subjects believed that the responsibility for using contraceptive methods does not solely rest on women (N= 218, 70.3%). Furthermore, more than half of the participants (N= 174, 56.1%) disagreed or strongly disagreed that contraceptive methods had adverse effects on the health of individuals that outweighed their benefits. However, just over two-fifths (N= 132, 42.6%) were unsure about the false statement that utilizing contraceptive methods in young individuals may elevate the likelihood of future infertility. Surprisingly, a minority of the study’s participants (15.4%) were either not sure or disagreed with changing the contraception method in case of existing adverse effects. Other findings are presented in Table 4.
 |
Table 4 Awareness Measurement of Contraception Methods |
Perception of Contraception Methods
Regarding the perceptions, less than half of the students agreed or strongly agreed that contraceptives are permitted in Islam when needed (N= 143, 46.1%) (Table 5). In addition, more than half of students thought it was unnecessary to purchase contraceptives (N= 182, 58.7%). Less than two-fifths of the students agreed that it needs some courage to buy contraceptives (N= 116, 37.4%). Over 90% of students thought that education about contraceptives should be introduced in the early years of education in the medical fields, and the majority expressed strong agreement that healthcare providers should offer comprehensive counseling on contraceptives, including methods, mechanisms, optimal usage, and potential side effects (N= 196, 63.2%). Other perceptions are described in Table 5.
 |
Table 5 Perception Measurement of Contraception Methods |
Comparison of Knowledge, Awareness, and Perception Scores Between the Different Sociodemographic Groups
Table 6 presents the statistical analysis results for the differences in the knowledge, awareness, and perception scores between the different sociodemographic groups. Final-year students had significantly better knowledge (Mean rank =169.42 vs 138.16, p= 0.002) and awareness (Mean rank =167.73 vs 140.26, p=0.007) compared to fourth-year students. No significant difference was observed in gender and the type of university. The type of training (Hospital, Community, None) had a statistically significant impact on awareness scores (p<0.001).
 |
Table 6 Differences in Knowledge, Awareness, and Perception Scores Among the Participants Using the Mann–Whitney U-Test and Kruskal–Wallis Test |
Discussion
In this study, we assessed the knowledge, awareness, and perception of contraception among senior pharmacy students. Two-thirds of students thought that contraceptives could reduce the risk of ovarian and endometrial cancer. Karlsson et al found that the risk for ovarian and endometrial was lower among those who used contraceptive pills in the UK ((OR = 0.72; 95% CI, 0.65–0.81), and (OR = 0.68; 95% CI, 0.62–0.75), respectively), and the association was stronger with longer use (P < 0.001). However, unfortunately, they also found that the risk of breast cancer was slightly increased with no significant difference in prolonged use.17
Knowledge about the utilization of contraceptives plays a major role in preventing unwanted outcomes due to contraceptive failure. Our study suggested that the senior pharmacy students knew fairly about condoms and contraceptive pills. The results of our work were in line with a study from Malaysia that assessed the knowledge among pharmacy students, where 80% of subjects knew that male condoms protect against STDs. Additionally, the same study found that students were knowledgeable about intrauterine devices (IUDs) and their use.11 In another study, standardized interviews were used to assess the knowledge about contraceptives, and found that the use of hormonal contraception and emergency contraception were not as common. Furthermore, 70% of participants thought that a standardized contraceptive curriculum should be added to the university curriculum in Malaysia.18 This was less than our finding, where around 90% agreed on this topic. A study from the University of Alabama showed that there is a gap in women’s knowledge and attitude toward hormonal contraception and concluded that prescription counseling about contraception should be incorporated into pharmacy school curricula.19 However, unlike our study, they assessed the knowledge and attitudes among first-year students instead of the senior ones. Most of our respondents wrongly thought that a pelvic exam is required before taking contraceptives, reflecting the need for contraceptive education at the university level.
As stated in the contraceptives fact sheet, contraceptive pills do not offer 100% protection against unwanted pregnancies (around 95%),20 this was reflected by our students’ knowledge responses about this topic. Also, many of our senior pharmacy students were either unsure or had a false idea that contraceptives might cause infertility in the future. Sedlander et al has found the misconception that modern contraceptives could cause infertility is widespread among African women and the most frequently mentioned side effect among them.21 Although almost all participants have stated that contraceptives could cause infertility, some of them stated that they do not personally believe it, but they believe it is present in the community and might have some truth to it. Furthermore, some participants said that they witnessed someone in the community take birth control pills and could not conceive later. Additionally, this study has indicated that the fear of becoming infertile exists not only among the public but also among senior pharmacy students. This is mainly based on anecdotal stories rather than scientific evidence. In a large systematic review of 121 studies, the authors found that most participants received information about oral contraceptives from the internet, media, and friends. Additionally, a negative attitude toward oral contraceptives was present in more than one-quarter of the participants.22
The vast majority of participants agreed that education about contraceptives should be implemented in the university curriculum. A Thai study assessed the implementation of educational courses at the university level and found that the students’ knowledge scores statistically improved after the courses. However, the students’ attitude toward using condoms and emergency contraceptive pills was not significantly changed.23 On the other hand, another Thai study reported that Thai pharmacists had average knowledge, poor attitude, and average practice related to emergency oral contraceptives (median scores = 51.02%, 21.81%, and 60.0%, respectively).24 A recent study from the University of Botswana found that although 95% of the 371 students knew about contraception, only 53% had good knowledge, and 55% had negative attitudes toward its use.25 Furthermore, similar to our study, higher-year students had better knowledge and a more positive attitude towards contraceptives.
In our study, the respondents thought that providing proper counseling about contraceptives is vital. Mobark and her colleagues found that the dispensing and counseling on hormonal contraceptives in the UAE was suboptimal among community pharmacists.26 And Barakat et al found that around 53% of community pharmacists encountered improperly used oral contraceptives.27 These findings suggest that there is an urgent need for proper contraceptive counseling. Similar to our findings, previous studies reported a great interest among community pharmacists and pharmacy students in the idea of providing direct contraceptive consultation to patients; such a direct approach model was also supported by physicians and clinicians.28,29
A few limitations should be addressed for this study. First, data gathering was limited to four Jordanian universities. This might restrict how far the data can be generalized. Second, because convenience sampling was used, it is probable that survey respondents were more enthusiastic than non-respondents, which would have led to an exaggerated perception of contraception. Therefore, additional research with a larger sample size, encompassing more cities and universities, and involving graduate pharmacists is recommended. Despite these limitations, the study included participants from both governmental and private universities from different major cities. Also, it is the first study from Jordan to assess the knowledge and perception of senior pharmacy students regarding contraception.
Conclusion
Final-year students were associated with better knowledge and awareness about contraceptives compared to fourth-year students. Students who had community pharmacy training were more aware of contraceptives compared to those who did not train at all and those who had hospital pharmacy training. Future studies should explore the impact of incorporating more targeted contraceptive education into earlier years of pharmacy education to bridge the knowledge gap observed between final-year and fourth-year students. Additionally, research should also investigate the effectiveness of specific community pharmacy training modules on contraceptive awareness.
Acknowledgments
The authors would like to thank Saifullah Al-Sammaraee, Baker Ali, and Sara Hafed for helping with the questionnaire distribution.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Kang HS, Moneyham L. Use of emergency contraceptive pills and condoms by college students: a survey. Int J Nurs Stud. 2008;45(5):775–783. doi:10.1016/j.ijnurstu.2007.01.008
2. Bearak J, Popinchalk A, Ganatra B, et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990–2019. Lancet Glob Health. 2020;8(9):e1152–e1161. doi:10.1016/S2214-109X(20)30315-6
3. Haddad LB, Nour NM. Unsafe Abortion: unnecessary Maternal Mortality. Rev Obstet Gynecol. 2009;2(2):122–126.
4. Bahk J, Yun SC, Kim Y, Khang YH. Impact of unintended pregnancy on maternal mental health: a causal analysis using follow up data of the Panel Study on Korean Children (PSKC). BMC Pregnancy Childbirth. 2015;15(1):85. doi:10.1186/s12884-015-0505-4
5. Blumenthal PD, Voedisch A, Gemzell-Danielsson K. Strategies to prevent unintended pregnancy: increasing use of long-acting reversible contraception. Hum Reprod Update. 2011;17(1):121–137. doi:10.1093/humupd/dmq026
6. World Health Organization. Contraception: Evidence Brief. World Health Organization; 2019. Available from: https://apps.who.int/iris/handle/10665/329884.
7. Tsui AO, McDonald-Mosley R, Burke AE. Family planning and the burden of unintended pregnancies. Epidemiol Rev. 2010;32(1):152–174. doi:10.1093/epirev/mxq012
8. Tanne JH. Problems with contraception play big part in unplanned pregnancies, study says. BMJ. 2008;336(7653):1095. doi:10.1136/bmj.39576.554699.DB
9. Chigbu B, Onwere S, Aluka C, Kamanu C, Okoro O, Feyi-Waboso P. Contraceptive choices of women in rural Southeastern Nigeria. Niger J Clin Pract. 2010;13(2):195–199.
10. Fathelrahman AI, Ibrahim MIM, Wertheimer AI. McCalley Chair Virginia Commonwealth University Richmond. In: Joseph T, editor. Pharmacy Practice in Developing Countries. Virginia USA: Academic Press; 2016:xxiii–xxiv. doi:10.1016/B978-0-12-801714-2.06001-9
11. Elkalmi RM, Khan MU, Ahmad A, et al. Knowledge, awareness, and perception of contraception among senior pharmacy students in Malaysia: a pilot study. J Res Pharm Pract. 2015;4(2):94–98. doi:10.4103/2279-042X.155760
12. Oo MS, Ismail NBM, Ean WR, Hamid HA. Knowledge, Attitude And Perception Of Contraception Among Medical Students In Universiti Putra Malaysia. Malays J Public Health Med. 2019;19(2):11–19. doi:10.37268/mjphm/vol.19/no.2/art.165
13. Fatimah SR. Knowledge, Awareness and Perception of Contraception among Students in a Public University. KnE Life Sci. 2019;34–43. doi:10.18502/kls.v4i13.5223
14. Nazer LH, Tuffaha H. Health Care and Pharmacy Practice in Jordan. Can J Hosp Pharm. 2017;70(2):150–155. doi:10.4212/cjhp.v70i2.1649
15. Daniel WW, Cross CL. Biostatistics: a Foundation for Analysis in the Health Sciences. Wiley; 2018.
16. Rutledge L ULibraries Research Guides: introduction to SPSS: Mann-Whitney U Test; 2022. Available from: https://campusguides.lib.utah.edu/c.php?g=160832&p=6707563.
17. Karlsson T, Johansson T, Höglund J, Ek WE, Johansson Å. Time-Dependent Effects of Oral Contraceptive Use on Breast, Ovarian, and Endometrial Cancers. Cancer Res. 2021;81(4):1153–1162. doi:10.1158/0008-5472.CAN-20-2476
18. Rim C, El-Ibiary SY, Rafie S, Borgelt LM. Assessment of contraceptive curricula in US pharmacy programs. Curr Pharm Teach Learn. 2020;12(4):395–399. doi:10.1016/j.cptl.2019.12.025
19. Hohmann N, Kavookjian J. Using the Theory of Planned Behavior to determine pharmacy students’ intention to participate in hormonal contraception counseling services. Curr Pharm Teach Learn. 2018;10(11):1488–1495. doi:10.1016/j.cptl.2018.08.005
20. University of Iowa Hospitals & Clinics. Birth control pill fact sheet; 2014. Available from: https://uihc.org/educational-resources/birth-control-pill-fact-sheet.
21. Sedlander E, Bingenheimer JB, Thiongo M, et al. “They Destroy the Reproductive System”: exploring the Belief that Modern Contraceptive Use Causes Infertility. Stud Fam Plann. 2018;49(4):345–365. doi:10.1111/sifp.12076
22. Leelakanok N, Parmontree P, Petchsomrit A, Methaneethorn J. A systematic review and meta-analysis of attitude and knowledge involving emergency oral contraceptive use in patients and healthcare providers. Int J Clin Pharm. 2022;44(4):873–893. doi:10.1007/s11096-022-01445-0
23. Thongnopakun S, Pumpaibool T, Somrongthong R. The effects of an educational program on knowledge, attitudes and intentions regarding condom and emergency contraceptive pill use among Thai female university students. J Health Res. 2018;32(4):270–278. doi:10.1108/JHR-05-2018-033
24. Leelakanok N, Kangwanrattanakul K, Petchsomrit A, Sapapsap B, Siritientong T, Methaneethorn J. After morning, phew! A knowledge, attitudes, and practices survey related to emergency oral contraception in Thai pharmacists. J Pharm Policy Pract. 2023;16(1):97. doi:10.1186/s40545-023-00601-9
25. Kgosiemang B, Blitz J. Emergency contraceptive knowledge, attitudes and practices among female students at the University of Botswana: a descriptive survey. Afr J Prim Health Care Fam Med. 2018;10(1):e1–e6. doi:10.4102/phcfm.v10i1.1674
26. Mobark DM, Al-Tabakha MM, Hasan S, Mobark DM, Al-Tabakha MM, Hasan S. Assessing hormonal contraceptive dispensing and counseling provided by community pharmacists in the United Arab Emirates: a simulated patient study. Pharm Pract Granada. 2019;17(2). doi:10.18549/pharmpract.2019.2.1465
27. Barakat M, Al-Qudah R, Akour A, Al-Qudah N, Bashi YHD. Unforeseen uses of oral contraceptive pills: exploratory study in Jordanian community pharmacies. PLoS One. 2020;15(12):e0244373. doi:10.1371/journal.pone.0244373
28. Landau S, Besinque K, Chung F, et al. Pharmacist interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. J Am Pharm Assoc JAPhA. 2009;49(1):43–50. doi:10.1331/JAPhA.2009.07154
29. Rafie S, El-Ibiary SY. Student pharmacist perspectives on providing pharmacy-access hormonal contraception services. J Am Pharm Assoc JAPhA. 2011;51(6):762–765. doi:10.1331/JAPhA.2011.10094
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
