Back to Journals » Risk Management and Healthcare Policy » Volume 16
Contemporary Universal Health Coverage in India – The Case of Federal State of Odisha (Orissa)
Authors Sahoo PM , Rout HS , Jakovljevic M
Received 21 February 2023
Accepted for publication 7 June 2023
Published 22 June 2023 Volume 2023:16 Pages 1131—1143
DOI https://doi.org/10.2147/RMHP.S406491
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Pragyan Monalisa Sahoo,1 Himanshu Sekhar Rout,2 Mihajlo Jakovljevic3–5
1Department of Analytical & Applied Economics, Utkal University, Bhubaneswar, Odisha, India; 2Department of Analytical and Applied Economics & RUSA Centre of Excellence in Public Policy and Governance, Utkal University, Vani Vihar, Bhubaneswar-751 004, Odisha, India; 3Institute of Advanced Manufacturing Technologies, Peter the Great St. Petersburg Polytechnic University, St Petersburg, Russia; 4Institute of Comparative Economic Studies, Hosei University, Tokyo, Japan; 5Department of Global Health Economics and Policy, University of Kragujevac, Kragujevac, Serbia
Correspondence: Pragyan Monalisa Sahoo, Department of Analytical & Applied Economics, Utkal University, Vanivihar, Bhubaneswar, Odisha, 751004, India, Tel +918895667710, Email [email protected]
Purpose: The present study assessed the awareness of the public about Biju Swasthya Kalyan Yojana (BSKY), which is a flagship public-funded health insurance scheme of the Government of Odisha. The study also identified its determinants and examined utilisation of the scheme among households in Khordha district of Odisha.
Materials and Methods: Primary data were collected from randomly chosen 150 households using a pretested structured questionnaire from Balipatana block of Khordha district, Odisha. Descriptive statistics and binomial logistic regression were used to substantiate the objectives.
Results: The study found that even though 56.70% of the sample households had heard about BSKY, procedure-specific awareness was low. State government organised BSKY health insurance camp was found to be a major source of knowledge among the sample. The regression model had an R2 of 0.414. The Chi2 value showed that the model with predictor variables was a good fit. Caste, gender, economic category, health insurance, and awareness about insurance were significant determinants of BSKY awareness. A majority (79.30%) of the sample had the scheme card with them. However, only 12.60% of the cardholders used the card and only 10.67% received benefits. Mean out-of-pocket expenditure (OOPE) faced by the beneficiaries is Rs. 15743.59. Among the beneficiaries, 53.80% financed the OOPE from their savings, 38.50% by borrowing, and 7.70% financed the OOPE by both means.
Conclusion: The study found that even though majority of people had heard about BSKY, they were not aware of its nature, features, and operational procedures. The trend of low benefit received and higher OOPE among the scheme beneficiaries hampers the economic health of the poor. Finally, the study highlighted the need to increase the magnitude of scheme coverage and administrative efficiency.
Keywords: out-of-pocket payments, health insurance, awareness, BSKY, India, emerging markets
Introduction
Healthcare in India has become expensive due to four major causes. They are a) medical inflation, b) high out-of-pocket expenditure (OOPE), c) low public health expenditure on health and healthcare, and d) unfolding of particularly communicable diseases.1 India here presents a unique case among the leading BRICS Emerging Markets for two causes. First is that its population still has a distinctive advantage of early stage of population aging which is about to bring the harvest of 150 million young educated and capable labour force expansion as we approach 2050.2 Another crucial fact is that India’s total health expenditure unlike that of the other BRICS nations remains steady at approximately 4% of its GDP share for almost two and a half decades.3 Due to the abundance of India’s welfare and prosperity at the federal level, its health spending per capita in absolute terms, both expressed in nominal and purchasing power parity continues to grow substantially over the same time horizon.4 These disparities among India and other BRICS as the engine of Global South development are likely to increase further as documented by 20255 and 2030 forecasts.6 Despite the growth in total health spending, spending allocation remains inefficient and regressive in India which is also common in its BRICS counterparts.7–11 India’s high OOPE lead people to take high-interest debt, sell their assets and pull-out resources from their basic necessities like food, cloth, shelter, and education,12–14 making the short-term health shock a cause behind long-term poverty. At times when the households fail to borrow, they are most likely to forego seeking high-value care, which leads them to poor health outcomes that ultimately degrade their work capacity pushing them further into poverty.12,15 A study conducted across an array of Global South countries found that health shocks are one of the major causes of impoverishment among people.6 The risk of impoverishment due to health shock for India is even more serious with its existing large-scale poverty; state-specific economic and social factors also play a significant role in it. The ever-rising cases of non-communicable diseases also contribute to the increased OOPE and catastrophic health expenditure (CHE).7,16,17 Thus, to protect the poor from incurring high OOPE, CHE and treat their health-related suffering, health insurance has become a necessity for the poor people, as a good insurance program protects people from the financial consequences related to the utilisation of medical care.18,19
United Nations in its sustainable development goal (SDG) 3.8 talks about universal health coverage (UHC). Achieving the UHC target is not only influenced by increased spending but also by country-specific structural factors.20 Almost all the member countries are putting their efforts towards achieving UHC. Different countries have made different progress toward UHC, with different service coverage and financial protection mechanisms.21 In the absence of a uniform approach to achieving UHC, countries have chosen different paths.
India started its UHC initiative in 2004 with its Universal Health Insurance Scheme (UHIS) way before the SDG targets and has introduced several other measures since then. In 2008, Rashtriya Swasthya Bima Yojana (RSBY) (National Health Insurance Scheme) was introduced by the Indian government as a cashless scheme to cover the hospitalization expenses of the BPL families. The scheme covered hospital admissions and surgical procedures for up to Rs. 30,000 yearly for families of up to five members. While some studies found that the beneficiaries of the RSBY scheme were satisfied with the scheme and willing to renew their enrolment with the scheme,22,23 some other studies also found that the scheme so far has been successful in reducing or keeping constant the treatment cost of inpatient and outpatient care. The scheme has been also criticized for some of its features, namely, focusing only on the BPL population and leaving out the APL population who are equally in danger of being impoverished due to healthcare expenses, of its complex administrative system, resulting in higher management cost, lack of utilisation of the scheme among users and narrow focus of the scheme on secondary and tertiary healthcare.24
To address the short-comings with RSBY and fill the healthcare financing gap, the union government established the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB PM-JAY) (Prime Minister’s People’s Health Scheme) in 2018, which aims to cover 40% of the vulnerable households with financial coverage up to Rs. 5,00000 for secondary and tertiary care hospitalisation. The majority of the Indian states have adopted the AB PM-JAY scheme. However, there are some states that have not joined the scheme and introduced their own state-led health coverage program. Odisha is one of those states having its own health insurance program called Biju Swasthya Kalyan Yojana (BSKY) (Biju Health Welfare Scheme).
Context and Framework
Odisha is an eastern state in India, whose 42 million population25 is mostly dominated by the poor, scheduled castes, scheduled tribes, and other vulnerable sections of the society. The state suffers from a high disease burden, both communicable and non-communicable.26 Poor health indicators and occasional health hazards contribute to the financial vulnerability of the people of Odisha. Rout and Choudhury27 found that “in Odisha, about 25% of the households reported hardship financing during the year 2012 due to healthcare expenditure”.
In 2018, the union government announced the PM-JAY health insurance scheme. However, Odisha chose to opt out of the scheme as several rounds of negotiations failed to provide a solution to the differences between the union and state government regarding the population covered under the scheme. The state government considered including 710 thousand of its economically weaker and vulnerable families, who are already enrolled under the existing state health schemes in PM-JAY. However, the union government criteria projected only 610 thousand families to be eligible for PM-JAY. Due to a lack of mutual consensus between both governments, the Odisha government announced its own scheme BSKY on 15 August 2018, by combining all the existing state schemes. The BSKY scheme details are given in Figure 1.
 |
Figure 1 BSKY scheme details. Reproduced with permission from Chandrashekar S, Dhananjay N, Rout S, et al. Biju Swasthya Kalyan Yojana (BSKY) Odisha Learnings and way forward. Bhubaneswar: Indian Institute of Public Health. Available from: https://www.hstp.org.in/wp-content/uploads/2021/03/bsky-policy-brief.pdf.28 Abbreviations: BKKY, Biju Krushak Kalyan Yojana (Previous version of BSKY); BPL, Below Poverty Line; AAY, Antyodaya/Annapurna cards (A food security program for the poorest segment of the BPL population in India); MCH, Medical College Hospital. |
Earlier studies done on public health insurance schemes in Odisha and India found that one of the major hurdles in the way of effective utilisation of the schemes and achieving its goal of providing affordable and risk-free health coverage for the vulnerable was a lack of awareness about them.1,14,29,30 The Odisha government launched a BSKY awareness drive in 2018 to raise program usage and public awareness. However, apart from some vague state government statistics, nothing is known about the scheme’s utilisation and awareness level among the population yet. In Odisha, while only one scoping study has been published on BSKY by Rout et al,31 no study has been conducted on the factors determining awareness and utilisation of the BSKY scheme. The present study is the first of its kind towards such an attempt. The study focuses on analysing the BSKY awareness in the study area and finding out the factors determining the awareness. It also analyses the extent of scheme utilisation among the beneficiaries.
Materials and Methods
Study Design, Setting and Data Collection
The study is based on primary data. As the main objective of this study was to analyse the awareness of BSKY and its utilisation, Khordha being the district recorded for having the highest health expenses per medical case (NSS 71st round) was purposively selected for the study. Khordha is one of the centrally located districts of Odisha state with a total area of 2813 sq km and a population of 2,251,673. It also has the highest literacy rate among the other districts in Odisha.25 Multistage random sampling was carried out to select two representative sample villages. Out of 10 blocks of the district, Balipatana was selected by following the chit lottery method. Balipatna has 16 gram-panchayats (village councils) out of which Garadia Panchana and Pampalo were selected. Out of the 8 villages in Garadia Panchana, Garedi Panchana, and out of the 9 villages in Pampalo, Nuapara was selected, respectively. Seventy-five households from each village – making total of 150 sample households – were selected randomly. Data were collected between January and February 2021 by conducting direct personal interviews using pre-structured schedules. Data were tested for any typographical errors and missing values using SPSS, whatever errors found were corrected.
Statistical Analysis
Descriptive analysis was carried out using percentages, averages, standard deviations, tables and graphs. BSKY awareness of the households was recorded in a discrete binary response format and to identify its determining factors, a binomial logistic regression model of the following form was used.
Yi= Awareness on BSKY
Yi = 1, If Aware
= 0; Otherwise
Xi= Selected Independent Variables; i= 1…10
ui= Idiosyncratic Error Term
Multicollinearity test was carried out using variance inflation factor (VIF) to test for any linear autocorrelations among the independent variables.
Results
BSKY Awareness Among Households
Table 1 displays the awareness of the BSKY programme and health insurance among various socioeconomic groups. Out of the total sample, 56.70, 47.30, 14.70, 40.70 and 52.70% were aware of insurance as a concept, health insurance, existing local health insurance, health insurance benefits, and BSKY, respectively. Among the socio-economic groups, male-headed households, general or OBC caste stratum, and APL households had the highest awareness in case of insurance, health insurance, benefits of health insurance and BSKY. While the awareness level on existing health insurance schemes among the total sample is low (14.70%), the awareness percentage was higher among female-headed households (18.20%) than in male-headed households. The local insurance scheme awareness percentage among other socio-economic stratums repeated the above discussed pattern. The statistical significance of the results is given with p-values. For BSKY awareness, only the results for gender of the households and caste category were significant at 5% and 1% levels, respectively.
 |
Table 1 Household Awareness of Health Insurance in the Study Area |
Source of Information for Health Insurance and BSKY Awareness
Figure 2 demonstrates that the majority of the sample’s knowledge about health insurance came through peer groups (26.80%), followed by SHGs (19.70%). Figure 3 demonstrates that the majority of people who were aware of BSKY did so through the BSKY insurance camp (34.20%), followed by peer groups (16.50%). In both situations, other mediums mostly include awareness from village panchayat offices.
 |
Figure 2 Source of information for general awareness on health insurance. Note: Primary Data. |
 |
Figure 3 Source of information for BSKY awareness. Note: Primary Data. |
Awareness of Pre-Hospitalisation Procedures Under BSKY
Table 2 provides information on pre-hospitalisation procedures under BSKY. Pre-hospitalisation steps include being aware of the sum assured (20.25%), hospitals on the panel (19%), and eligibility status (15.19%). While the statistics suggest poor procedural awareness throughout the sample, relative awareness was high for households headed by women, OBC and SC castes, BPL and AAY households (a counterintuitive conclusion given BSKY awareness findings). Only the economic category outcome, though, was statistically significant.
 |
Table 2 Household Awareness on Pre-Hospitalisation Procedures Under BSKY |
Awareness of Procedures During Hospitalisation Under BSKY
Table 3 provides awareness percentage on during-hospitalisation procedures under BSKY. The beneficiary proof requirement at the counter (24.05%), the card balance (7.60%), the fingerprint verification procedure at the counter (16.45%), and the supply of free medications and testing for patients (26.58%) are among the during-hospitalisation procedures for BSKY. Relative awareness of during-hospital procedures was also higher in families led by women. However, OBC and general caste groups exhibited more awareness than SCs. The level of awareness about during-hospitalisation procedures was highest among APL households among all economic groups. Findings for the gender of the household head were significant only in card balance awareness, and the findings for the economic category were significant in all the during-hospitalisation procedures except fingerprint verification.
 |
Table 3 Household Awareness on Procedures During-Hospitalisation Under BSKY |
Awareness of Post-Hospitalisation Procedures
Table 4 provides information on sample awareness of post-hospitalisation procedures under BSKY. Awareness of receiving a hospital discharge summary (7.60%), post-discharge fingerprint verification (17.72%), receiving the smart card back (16.46%), money remaining on the card (10.13%), coverage of 5-day post-hospitalisation expenses (8.86%), and provision of a travel allowance (7.60%) are among the post-hospitalization procedures. Only the findings for gender and economic categories were found to be statistically significant in some procedural awareness.
 |
Table 4 Household Awareness on Post-Hospitalisation Procedures |
Factors Affecting BSKY Awareness
The present study focuses on factors like caste category, gender, economic category, occupation, health insurance, and awareness of insurance to examine their influence on scheme awareness. The multicollinearity test showed no linear autocorrelation among the independent variables.
The output from logistic regression is given in Table 5. The table shows that the model has an R2 of 0.414, and the −2 log-likelihood or deviance is 151.808. The Chi2 value shows that the model with predictor variables is significant or a good fit.
 |
Table 5 Regression Output on Factors Determining BSKY Awareness |
The table shows that both general and OBC categories were more likely to be aware of the BSKY scheme than SC category, the former having eight times more likelihood and the latter with five times more likelihood than SC category. Both variables were significant at the 1% level. Male-headed households were twice more likely to be aware of BSKY than female-headed households. The difference was significant at the 10% level. The fifth variable Economic category shows Antyodaya/Annapurna cardholders were less likely to be aware of the scheme, and the result was significant at 5% level. The sixth variable Economic category being APL cardholder had a negative coefficient of −0.404 and an odds ratio of 0.668, which indicates that the APL category was less likely to be aware of BSKY. The variable Economic category being BPL cardholder had a positive coefficient of 0.206 and an odds ratio of 1.228. However, both the results were insignificant. Coefficient for occupation of the bread earner of the family indicates that having a formal occupation had a less likelihood of being aware of BSKY. However, the result was insignificant. Those who have health insurance were less likely to be aware of the BSKY than those who do not have any health insurance. Being aware of insurance had a coefficient of 2.163 and an odds ratio of 8.696 that indicates being aware of insurance increases the probability of being aware of BSKY by 8 times than those who do not know about insurance. Both the results were significant at the 1% level.
Utilisation of BSKY Card
The success of any welfare scheme is reflected in its mass utilisation. This section focuses on analysing the utilisation of BSKY in the study area.
Classification of families on the basis of the availability of BSKY card is given in Table 6. The table shows that 79.30% of the households had BSKY cards in the sample population. This indicates that a good percentage of population had the cards.
 |
Table 6 Utilisation of BSKY Card |
However, only 12.60% of the cardholders used the card for in-patient treatment and only 10.67% had received benefits from the card.
Table 7 shows the majority of the BSKY beneficiaries were from the general caste category followed by SC and OBC, respectively. The average income of the beneficiaries was Rs. 2,32,687.5 with a standard deviation of 348,434.35.
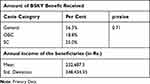 |
Table 7 Socio-Economic Profile of Beneficiaries |
Table 8 shows among BSKY hospitalisation cases, 80% went to private hospitals and 20% to public hospitals. This shows the high occurrence of BSKY hospitalisation in private hospitals. Around 20.1% of the beneficiaries received benefits amount under Rs. 10,000, 53.3% received between Rs. 10,000 and 20,000, 6.70% received above Rs. 20,000 and 20% of the beneficiary households did not know the amount of benefit received as they were not informed by the hospitals. After excluding the beneficiaries who were not aware of the benefit received, the mean amount of benefit received was estimated to be Rs. 25,566.67, with a standard deviation of 41,735.08 for the study period. The table depicts majority (35.40%) of the beneficiaries received only 0.20% of the Rs. 500,000 sum assured. About 5.90% of the beneficiaries received 0.30% and 1.40% of the sum assured. Majority (29.40%) of the households received 2%, 11.80% received 2.40% and 3% of the sum assured, and 5.90% beneficiaries received 4%, 20% and 30% of the sum assured. Among the card users, 86.70% had to pay extra OOPE. This shows that even after availing of insurance benefits under BSKY, the beneficiaries had to face out-of-pocket payment.
 |
Table 8 Card Use Details |
Among different reasons for paying out-of-pocket expenses, 7.70% stated that amount left in the card was insufficient, 15.30% stated that the hospital asked them to pay some amount in cash, 62% stated they had to pay for tests and medicines, and 15.38% had other reasons for paying OOPE.
Payment for medicines and tests was the major cause for out-of-pocket payment among the beneficiaries. All cases of extra out-of-pocket payment took place in private hospitals. Out of 46.1% paid below Rs. 10,000, 30.8% paid between Rs. 10,000 and 50,000 and 23.1% paid above Rs. 50,000. The mean OOPE paid by the beneficiaries are Rs. 15,743.59.
Regarding the source of financing of out-of-pocket payment, 53.80% of beneficiaries covered it on their own, 38.50% covered by borrowing, and 7.70% covered partly by both means. The present health status of the BSKY patients would indicate the quality of health service provided under the scheme. The findings showed 73.30% of BSKY patients had fully recovered, 6.70% of patients showed no improvement in their health, and 20% of patients had partially improved at the time of survey.
Discussion
Among the number of factors posing barriers to the success of public health insurance schemes, lack of scheme awareness plays a significant role in India.32 The present study showed that even though general awareness of BSKY was high among the sample, awareness of different procedures under schemes like pre-hospitalisation, during-hospitalisation, and post-hospitalisation was very low. Studies on RSBY in India also found that its beneficiaries had little knowledge about the benefits and services provided under the scheme,33–35 thus they continue to incur high out-of-pocket expenditures even after being enrolled in the scheme. The potential benefits of such schemes can only be realised by increasing awareness of such schemes among the population. Literature on factors determining health insurance awareness found variables like sex, socio-economic background, and education to have a dominant influence on the awareness level among people of various health insurance schemes.36,37 The present study conforms to the existing literature. It found female household heads, vulnerable social categories (OBC and SC), and lower economic class (BPL) had less probability of BSKY awareness than their affluent counterparts. These groups, which are likewise at the bottom of the social ladder, had lower annual incomes and were mostly less educated or illiterate. Understanding different government programs can be challenging for those who are illiterate or have low levels of education.
Economic literature typically generalises the same findings and justifications to households in lower economic categories.38 The case Antyodaya/Annapurna economic category household was special as they were more likely than both the APL and BPL categories to be aware of BSKY. One explanation for this finding is that because the Antyodaya/Annapurna category is among the lowest and weakest economically, it is frequently the target of government welfare programs. This is also true when it comes to providing healthcare. According to the initial survey, these families held several health scheme cards, including RSBY, BSKY, and Ayush scheme cards. However, such households could not differentiate among those schemes. Additionally, the survey discovered that people who privately bought health insurance were less likely to be familiar with BSKY. These were wealthier households that never had financial hardship paying for their healthcare. They never needed to search for any expense waivers, thus they may not have known about welfare programs like BSKY. Insurance awareness increased the probability of BSKY awareness by 8 times. The survey found that one of the main sources of insurance information was the SHG and bank loan meetings.
Besides the above variables, mistrust among people about their source of information about the scheme and language in a multilingual country like India also acts as a major barrier to the spread of awareness. The skeptical behaviour of people towards the scheme makes them hesitant in utilizing the scheme. The misunderstanding surrounding such schemes like mistaking the scheme as a complete cashless or credit card type program leads the beneficiaries further into debt. The solution to this problem can be given by educational intervention programmes by the government.39
The utilisation of the scheme showed only 12.60% of the cardholders had received any benefits and 10.67% had used the card for treatment. Low mean benefits received and benefits received as a percentage of the total sum assured show low utilisation of the scheme among beneficiaries. Scheme utilisation was particularly low among the socio-economically backward classes like OBC and SC. This low utilisation results from lack of awareness of the scheme as was also claimed by Shrisharath et al40 in their study on Ayushman Bharat in Karnataka.
There was a high occurrence of BSKY hospitalisation in private hospitals. This could either mean the low preference of people for the public hospitals or since the services in public hospitals are almost free, there was no need to use the card, hence cards were only used while availing treatment at the private hospitals.
Even after availing of insurance benefits under BSKY, the beneficiaries had to pay the mean OOPE of Rs. 15,743.59. The amount is burdensome if we see the economic condition of the cardholders, who were mostly farmers and BPL households. Paying for medicines and tests was the major cause for OOPE among the beneficiaries. This finding conforms to the findings of Garg and Karan,12 who stated that among the hospitalization expenses, OOPE on medicines alone occupies the largest share of the total OOPE in India. In LMICs, medicines contribute the largest proportion to OOPE for healthcare and this proportion is inversely associated with income quintile.31 The vast use of over-the-counter medication by the lower-income population can be a major cause behind such high OOPE on medicines.41 However, even though BSKY health insurance scheme covers expenses on medicines and tests in empannelled and government hospitals, often, the beneficiaries were told to buy medicines and to do the tests at other chemist stores and patholabs as some tests and medicines used to be unavailable at the hospital premises which ultimately contributed to high OOPE.
Own expenses and borrowing were the major source of financing for OOPE. This shows that even after being covered by BSKY, beneficiaries had to face the burden of borrowing, which limits BSKY’s achievement in protecting the poor from health-related impoverishment. Studies on the earlier version of BSKY called Biju Krushak Kalyan Yojana (BKKY) found similar results.1 The bearers of maximum damage for high out-of-pocket payment are the poor who are forced to use their savings, sell their assets, and even take unsecured loans with high-interest rates to cover the cost of care for which they later suffer to repay.1,28
Conclusions
The study concludes that even though general awareness on BSKY was more than 50%, when it comes to awareness of pre-hospitalisation, during-hospitalisation, and post-hospitalisation procedures, the awareness was very low. The disparity in awareness levels found between upper and lower socio-economic strata households is a cause of concern. Factors like caste, gender, economic category, having health insurance and being aware of insurance affect the awareness of BSKY. BSKY insurance camps, ASHA workers and SHGs were found to be significant and effective sources of information on the scheme. These mediums can be used for a further awareness drive. Having utilized the scheme benefit earlier also contributed to a great extent as a source of awareness. Evidence from the study also shows the trend of low benefit received and higher OOPE among the scheme beneficiaries, which hampers the economic health of the poor. The majority of the OOPE occurs for buying medicines and tests. To address the issue of card usability and IT failure, the government of Odisha has begun issuing smart cards to all BSKY users. However, much more needs to be done in terms of the magnitude of scheme coverage and administrative efficiency.
Based on the comprehensive analysis of study findings, which included both quantitative data and qualitative observations, several policy suggestions have been formulated. These recommendations are based on the understanding derived from the study and aim to address the identified issues effectively. For better awareness of the scheme, the awareness drive should be targeted at vulnerable sections of the society such as SC category and AAY cardholder category population in which the ASHA workers and SHGs can be used as awareness drivers. The WHO has also acknowledged the ASHA workers for connecting the communities to primary healthcare services and for playing an important part in raising the rate of COVID-19 vaccination in 2022.42 Greater focus should also be on encouraging cardholders to use the insurance benefits, and more private hospitals and nursing homes should be empanelled so that the patients do not have to waste their time in deciding which hospital to visit for availing the benefit. Also, they can approach any nearest health facility without having to travel long distances and occurring heavy transportation cost. A provision should be made to cover medicines and tests under the scheme benefits in the private facilities and strict inspection should be conducted from time to time to avoid any unfair practices by the hospitals. Last but not the least significance should be given for simplification of the scheme policy, procedures and approach. Future studies on BSKY should concentrate on how the scheme affects people’s health and economic wellbeing by using a broader, more representative sample of people.
Ethical Statement
The research was approved by the Departmental Research Committee (DRC) of the Department of Analytical & Applied Economics, Utkal University, Bhubaneswar, India. Informed consent was sought prior to conducting personal interviews with the sample households with the confirmation of maintaining data confidentiality. The study was performed in accordance with the principles stated in the World Medical Association – Declaration of Helsinki. Number of Decision: ECO/85(A)/2020. Date and place when Approval was issued: 21/03/2020 (Bhubaneswar).
Acknowledgments
The authors extend their appreciation to the journal editors and anonymous reviewers.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was not funded by any funding agency.
Disclosure
The authors declare no known competing interests for this work.
References
1. Panda B, Rout HS. Access, utilisation and challenges of Biju Krushak Kalyan Yojana (BKKY): a case study from Odisha, India. J Rural Dev. 2020;39(2):278–291. doi:10.25175/jrd/2020/v39/i2/127487
2. Chandrasekhar CP, Ghosh J, Roychowdhury A. The demographic dividend and young India’s economic future. Econ Polit Wkly. 2006;41(49):5055–5064.
3. Jakovljevic M, Timofeyev Y, Ranabhat CL, et al. Real GDP growth rates and healthcare spending–comparison between the G7 and the EM7 countries. Glob Health. 2020;16(1):1–13. doi:10.1186/s12992-020-00590-3
4. Mishra PK. The dynamics of relationship between exports and economic growth in India. Int J Econ Sci Appl Res. 2011;4(2):53.
5. Jakovljevic M, Potapchik E, Popovich L, et al. Evolving health expenditure landscape of the BRICS nations and projections to 2025. Health Econ. 2017;26(7):844–852. doi:10.1002/hec.3406
6. Jakovljevic M, Lamnisos D, Westerman R, et al. Future health spending forecast in leading emerging BRICS markets in 2030: health policy implications. Health Res Policy Syst. 2022;20(1):1–14.
7. Jakovljevic M, Ogura S. Health economics at the crossroads of centuries–from the past to the future. Front Public Health. 2016;4:115. doi:10.3389/fpubh.2016.00115
8. Jakovljevic M. Therapeutic innovations: the future of health economics and outcomes research–increasing role of the Asia-Pacific. J Med Econ. 2021;24(sup1):i–iii. doi:10.1080/13696998.2021.2014164
9. Jakovljevic M, Groot W, Souliotis K. Healthcare financing and affordability in the emerging global markets. Front Public Health. 2016;4:2. doi:10.3389/fpubh.2016.00002
10. Jakovljevic M, Sugahara T, Timofeyev Y, et al. Predictors of (in)efficiencies of healthcare expenditure among the leading asian economies–comparison of OECD and non-OECD nations. Risk Manag Healthc Policy. 2020;13:2261. doi:10.2147/RMHP.S266386
11. Jakovljevic M, Liu Y, Cerda A, et al. The Global South political economy of health financing and spending landscape–history and presence. J Med Econ. 2021;24(sup1):25–33. doi:10.1080/13696998.2021.2007691
12. Garg CC, Karan AK. reducing out-of-pocket expenditures to reduce poverty: a disaggregated analysis at rural-urban and state level in India. Health Policy Plan. 2009;24(2):116–128. doi:10.1093/heapol/czn046
13. Mohanty SK, Chauhan RK, Mazumdar S, et al. Out-of-pocket expenditure on healthcare among elderly and non-elderly households in India. Soc Indic Res. 2013;115(1):1137–1157. doi:10.1007/s11205-013-0261-7
14. Panda B, Rout HS. Extent of use of the government sponsored health insurance schemes: evidence from rural Odisha. Indian J Econ Dev. 2018;6(10):1–11.
15. Garg P, Nagpal J. A review of literature to understand the complexity of equity, ethics and management for achieving public health goals in India. J Clin Diagnostic Res. 2014;8(2):1–6.
16. Jakovljevic M, Jakab M, Gerdtham U, et al. Comparative financing analysis and political economy of non-communicable diseases. J Med Econ. 2019;22(8):722–727. doi:10.1080/13696998.2019.1600523
17. Menon G, Yadav J, John D. Burden of non-communicable diseases and its associated economic costs in India. Soc Sci Humanit Open. 2022;5(1):1–8.
18. Aggarwal A. Impact evaluation of India’s ‘YESHASVINI’ community-based health insurance programme. Health Econ. 2010;19(S1):5–35. doi:10.1002/hec.1605
19. Devadasan N, Criel B, Damme WV, et al. Open access performance of community health insurance in India: findings from empirical studies. BMC Proc. 2012;6(1):9. doi:10.1186/1753-6561-6-S1-P9
20. Ranabhat CL, Jakovljevic M, Dhimal M, et al. Structural factors responsible for universal health coverage in low-and middle-income countries: results from 118 countries. Front Public Health. 2020;7:414. doi:10.3389/fpubh.2019.00414
21. World Health Organization. Global monitoring report on financial protection in health. World Health Organisation. Available from: https://www.who.int/healthinfo/universal_health_coverage/report/fp_gmr_2019.pdf?ua=1.
22. Rao MG, Choudhury M Healthcare financing reforms in India. New Delhi: National Institute of Public Finance and Policy; 2012. Available from: https://www.nipfp.org.in/media/medialibrary/2013/04/wp_2012_100.pdf.
23. Kamath R, Sanah N, Machado LM, et al. Determinants of enrolment and experiences of Rashtriya Swasthya Bima Yojana (RSBY) beneficiaries in Udupi district, India. Int J Med Public Health. 2014;4(1):82–88. doi:10.4103/2230-8598.127164
24. Selvaraj S, Karan A. Why publicly-financed health insurance schemes are ineffective in providing financial risk protection. Econ Polit Wkly. 2012;47(11):60–68.
25. Census of India. New Delhi: government of India. Available from: https://censusindia.gov.in/census.website/.
26. Rout HS, Hota AK. Health and Healthcare in Odisha. In: Nayak PB, Panda SC, Pattanaik PK, editors. The Economy of Odisha: A Profile. New Delhi: Oxford University Press; 2016:350–381.
27. Rout SK, Choudhury S. Does public health system provide adequate financial risk protection to its clients? Out of pocket expenditure on inpatient care at secondary level public health institutions: causes and determinants in an Eastern Indian State. Int J Health Plann Manage. 2018;33(2):1–12. doi:10.1002/hpm.2490
28. Chandrashekar S, Dhananjay N, Rout S, et al. Biju Swasthya Kalyan Yojana (BSKY) Odisha Learnings and way forward. Bhubaneswar: Indian Institute of Public Health. Available from: https://www.hstp.org.in/wp-content/uploads/2021/03/bsky-policy-brief.pdf.
29. Panda B, Rout HS. Does public health system provide adequate financial protection to its clients through RSBY? An exploratory study of tribal Odisha. J Health Manag. 2019;21(4):1–13. doi:10.1177/0972063419868555
30. Platteau J, Ontiveros D. Cognitive bias in insurance: evidence from a health scheme in India. World Dev. 2021;144(105498):1–24. doi:10.1016/j.worlddev.2021.105498
31. Rout SK, Ghosh U, Parhi A, et al. State led innovations for achieving universal health coverage in a low resource setting Odisha, India: opportunities and challenges. Int J Community Med Public Health. 2021;8(5):2338–2345. doi:10.18203/2394-6040.ijcmph20211755
32. Kansra P, Pathania G. A study of factors affecting the demand for health insurance in Punjab. J Manag Sci. 2012;2(4):281–290.
33. Nandi S, Nundy M, Prasad V, et al. The Implementation of RSBY in Chhattisgarh, India. Health Cult Soc. 2012;2(1):41–70. doi:10.5195/HCS.2012.61
34. Vasisht S, Pandit N. Experiences of RSBY beneficiaries in a district of Western India –A Qualitative study. Int J Eng Manag Res. 2012;2(7):1–8.
35. Patel V, Parikh R, Nandraj S, et al. Assuring health coverage for all in India. Lancet. 2015;386(10011):2422–2435. doi:10.1016/S0140-6736(15)00955-1
36. Choudhary ML, Goswami KI, Khambhati SB, et al. Awareness of Health insurance and its related issues in rural areas of Jamnagar district. Natl J Community Med. 2013;4(2):267–271.
37. Yellaiah J, Ramakrishna G. Socio economic determinants of health insurance in India: the case of Hyderabad City. Int J Dev Sust. 2012;1(2):111–119.
38. Kusuma Y, Pal M, Babu B. Health insurance: awareness, utilization, and its determinants among the Urban Poor in Delhi, India. J Epidemiol Glob Health. 2018;8(1–2):69–76. doi:10.2991/j.jegh.2018.09.004
39. Puri R, Sun C. Increasing utilization of public health insurance programs: evidence from an experiment in India. World Dev. 2021;139(105321):1–8. doi:10.1016/j.worlddev.2020.105321
40. Shrisharath K, Hiremat S, Kumar S, et al. A study on the utilisation of Ayushman Bharat Arogya Karnataka (ABArK) among COVID patients admitted in a Tertiary Care Hospital. Clin Epidemiology Glob Health. 2022;15(101015):1–4.
41. Ghosh S. Catastrophic payments and impoverishment due to out-of-pocket health spending. Econ Polit Wkly. 2011;46:47.
42. Patel V, Bhagada S, Mazumdar-Shaw K, et al. A historic opportunity for universal health coverage in India. Lancet. 2022;400(10351):476–478. doi:10.1016/S0140-6736(22)01395-2
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

