Back to Journals » Clinical Optometry » Volume 11
Contact lens-related visual loss in the context of microbial keratitis
Authors Mohammadpour M, Hosseini SS, Khorrami-Nejad M, Bazvand F
Received 29 October 2018
Accepted for publication 18 January 2019
Published 13 February 2019 Volume 2019:11 Pages 11—14
DOI https://doi.org/10.2147/OPTO.S192585
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Mr Simon Berry
Mehrdad Mohammadpour,1 Seyedeh Simindokht Hosseini,1 Masoud Khorrami-Nejad,1,2 Fatemeh Bazvand1
1Eye Research Center, Farabi Eye Hospital, Tehran University of Medical Sciences, Tehran, Iran; 2Department of Optometry, School of Rehabilitation, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Abstract: Microbial keratitis is a potentially blinding condition for those who do not receive rapid and proper treatment. The case of a healthy 26-year-old man who has worn extended-wear hydrogel soft contact lenses and developed a unilateral central corneal ulcer with underlying dense stromal infiltrates surrounded by subepithelial and superficial stromal opacity in a reticular pattern along with several complications is reported.
Keywords: infectious keratitis, contact lens, emergency penetrating keratoplasty
Introduction
Microbial keratitis is a rare and acute corneal disease, a potentially blinding condition for those who do not receive rapid and appropriate treatment. It has been shown that the use of contact lenses is recognized as one of the major risk factors for developing this condition in western and developing countries.1,2
Case report
A 26-year-old high-myopic man with a history of wearing soft extended-wear hydrogel contact lenses was referred for evaluation with complaints of decreased vision, photophobia, and pain in the left eye of 3 days’ duration as well as a history of using topical steroids and antibiotics prior to referral. The patient provided written informed consent for the case details and images to be published. The Ethics Committee of Tehran University of Medical Science approved the publication of the case details.
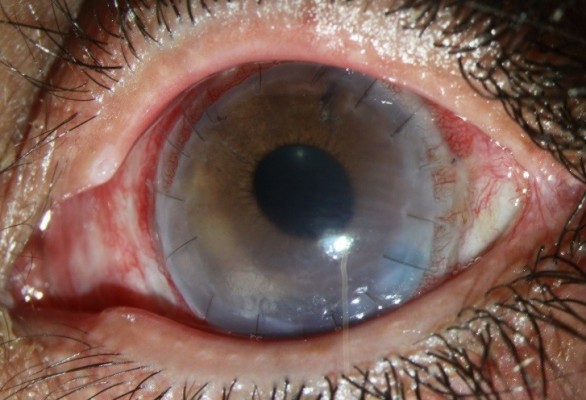
The patient’s ocular and systemic history was unremarkable. On ocular examination, the visual acuity was hand motion in the left eye and 2/10 in the right eye. The conjunctiva in the left eye was 3+ injected with a marked limbal flush. The corneal examination revealed an 8 mm inferior paracentral ulcer with 4 mm of central corneal thinning. The surrounding cornea was noted to have a marked stromal infiltration and a significant purulent discharge. These clinical features were most probably compatible with fulminant bacterial keratitis (Figures 1 and 2).
  | Figure 1 Left eye at presentation (down gaze). |
  | Figure 2 Left eye at presentation (primary position). |
The smear was Gram-negative bacilli, and culture revealed Pseudomonas aeruginosa. A few hours later, severe thinning of the descemetocele turned into a perforation. Based on the large affected area in the cornea by keratitis and severe infections, a large limbus to limbus tectonic graft was implemented with lateral tarsorrhaphy in the same setting (Figures 3 and 4).
  | Figure 3 Left eye post penetrating keratoplasty. |
  | Figure 4 Left eye post lateral tarsorrhaphy. |
Lateral tarsorrhaphy was performed to enhance reepithelialization after the limbus to limbus transplant. The patient was discharged from the hospital with close follow-up monitoring. One month later, uncorrected visual acuity increased to 4/10 in the involved eye. The graft was clear with no signs of early rejection (Figure 5).
  | Figure 5 Patient with considerably clear optical zone after penetrating keratoplasty. |
On subsequent follow-up, the patient developed a corneal epithelial defect increasing in size from the central cornea to the periphery (Figures 6 and 7).
  | Figure 6 Persistent epithelial defect 3 months after penetrating keratoplasty. |
  | Figure 7 Persistent epithelial defect, fluorescein staining. |
The patient was instructed to use copious lubrication, instill a lubricating ointment frequently, and tape the lids closed to minimize eyelid friction during the night. Cefazolin (50 mg/mL, 5%) eye drops and 2% fortified amikacin eye drops were prescribed every 1 hour. He was prescribed close follow-up. Three months later, the patient developed a total epithelial defect involving whole parts of the cornea. He traveled long distances to get to our hospital. Unfortunately, the patient was lost to follow-up for subsequent visits. Six months later, he returned with visual loss and perforation of the donor cornea as shown in Figure 8. The patient was admitted, and a concomitant corneal patch graft and a bipedicular conjunctiva flap were implanted. Subsequently, the patient experienced three episodes of graft rejection that were managed by topical and systemic steroids.
  | Figure 8 Corneal melting, 6 months later. |
Discussion
Microbial keratitis is a sight-threatening complication for contact lens wearers, affecting almost 5 per 10,000 wearers. The condition has been proposed as an ocular emergency, and prompt antimicrobial administration is imperative. With a massive number of contact lens wearers worldwide, corneal ulcer with its noteworthy morbidity has been considered as a public health consequence.3 If corneal perforation seems likely, urgent management is required. Although the mainstay of initial management of severe infective keratitis remains aggressive antimicrobial therapy to limit spread to the sclera and anterior chamber, the role of timely surgical intervention in the form of therapeutic keratoplasty should be considered in view of the relatively successful outcomes. The timing of surgery is critical for virtuous therapeutic outcomes.4
Perforated eyes need urgent treatment to protect the corneal anatomic integrity and avoid the development of complications such as endophthalmitis. Conservative management of corneal perforation such as therapeutic soft contact lenses, amniotic membrane graft, or surgical adhesive glue is recommended. However, the effect of adhesion is temporary. Corneal perforation ultimately may require therapeutic keratoplasty.5
On the other hand, success rates of therapeutic keratoplasty for desperate infectious keratitis fluctuate widely, influenced by organism virulence, predisposing factors, associated ocular surface inflammation, initial medical treatment, and surgical performance.6
Topical steroids are useful when the ulceration is secondary to inflammatory mediators, but they are contraindicated in corneal melts with inflammation.7 Unfortunately, our case received injudicious use of topical steroids prior to referral, which formulates more complications.
Although large grafts often are regarded as a risk factor for graft failure, a study in Singapore noted that in terms of graft clarity there was no statistical difference between penetrating grafts 9.0 mm or larger and those <9.0 mm in diameter.6 On the other hand, there are studies showing that small-diameter penetrating keratoplasty seems to be effective in treating various eccentric corneal perforations.8 Apart from the increased complication rate of large graft surgery resulting from loss of limbal support and subsequent protrusion of the lens–iris diaphragm during surgery, the risk of surgery – including surgical manipulation of inflamed, necrotic iris tissue, and copious hemorrhage – has been increased. Inflammatory debris may be associated with chronic graft edema, occlusio pupillae, and a high risk of angle damage causing glaucoma.6
In our patient, impression cytology was not performed; however, in view of the persistent characteristic of epithelial defect which was impervious to medical and surgical interventions, the probability of limbal stem cell deficiency has been proposed and thus supplementary complex suggested for its management.
Scheduled visits during the course of corneal ulcer are mandatory. All patients require frequent and close observation until they start responding to treatment.9,10 Regrettably, our case missed long-term follow-up, which exacerbates the patient’s poor prognosis.
In view of numerous complications in this case, more likely introducing a small corneal patch graft could produce better results. Moreover, compliance to follow-up as well as precise scheduled follow-up and deferring keratoplasty to a proper stage while the inflamed eye becomes settled would be beneficial.
Disclosure
The authors report no conflicts of interest in this work.
References
Musa F, Tailor R, Gao A, Hutley E, Rauz S, Scott RA. Contact lens-related microbial keratitis in deployed British military personnel. Br J Ophthalmol. 2010;94(8):988–993. | ||
Bourcier T, Thomas F, Borderie V, Chaumeil C, Laroche L. Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol. 2003;87(7):834–838. | ||
Stapleton F, Keay L, Edwards K, et al. The incidence of contact lens-related microbial keratitis in Australia. Ophthalmology. 2008;115(10):1655–1662. | ||
Sedghipour MR, Sorkhabi R, Shenasi A, Dehghan H. Outcome of penetrating keratoplasty in corneal ulcer: a single-center experience. Clin Ophthalmol. 2011;5:1265. | ||
Roozbahani M, Hammersmith KM, Nagra PK, Ma JF, Rapuano CJ. “Therapeutic penetrating keratoplasty: a retrospective review”. Eye Contact Lens. 2018;44(Suppl 2):S433–S441. | ||
Ti SE, Scott JA, Janardhanan P, Tan DT. Therapeutic keratoplasty for advanced suppurative keratitis. Am J Ophthalmol. 2007;143(5):755–762. | ||
Carnt N, Samarawickrama C, White A, Stapleton F. The diagnosis and management of contact lens-related microbial keratitis. Clin Exp Optom. 2017;100(5):482–493. | ||
Lohchab M, Prakash G, Arora T, et al. Surgical management of peripheral corneal thinning disorders. Surv Ophthalmol. 2019;64(1):67–78. | ||
Gokhale NS. Medical management approach to infectious keratitis. Indian J Ophthalmol. 2008;56(3):215. | ||
Mohammadpour M, Rahimi F, Khorrami-Nejad M. Total necrosis of cornea, iris and crystalline lens with exposure of vitreous hyaloid face in the context of recalcitrant Acanthamoeba keratitis. J Curr Ophthalmol. 2018;30(4):377–380. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
