Back to Journals » Pediatric Health, Medicine and Therapeutics » Volume 13
Congenital Hydrocephalus and Associated Risk Factors: An Institution-Based Case–Control Study, Dessie Town, North East Ethiopia
Authors Abebe MS , Seyoum G, Emamu B, Teshome D
Received 28 February 2022
Accepted for publication 9 May 2022
Published 11 May 2022 Volume 2022:13 Pages 175—182
DOI https://doi.org/10.2147/PHMT.S364447
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Roosy Aulakh
Melese Shenkut Abebe,1 Girma Seyoum,2 Bahru Emamu,3 Demissie Teshome4
1Department of Anatomy, School of Medicine, College of Health Science, Wollo University, Dessie, Ethiopia; 2Department of Anatomy, School of Medicine, College of Health Sciences, Addis Ababa University, Addis Ababa, Ethiopia; 3Department of Radiology, School of Medicine, College of Medicine and Health Science, Wollo University, Dessie, Ethiopia; 4Department of Radiography, Dessie Health Science College, Dessie, Ethiopia
Correspondence: Melese Shenkut Abebe, Department of Anatomy, School of Medicine, College of Health Science, Wollo University, Dessie, Ethiopia, Email [email protected]
Introduction: Congenital hydrocephalus is one of the commonest congenital anomalies of the central nervous system. It is characterized by extensive accumulation of cerebrospinal fluid within the ventricles of the brain due to an imbalance between synthesis and absorption of cerebrospinal fluid. This study was planned to investigate the incidence and associated risk factors of congenital hydrocephalus.
Methods: Unmatched case–control study was conducted in 34 (cases) and 104 (controls) pregnant women. Maternal data were collected from a structured questionnaire, and fetal-related data were recorded from obstetric ultrasound. Epi-info 7 and SPSS version 24 were used for data entry and analysis, respectively. The association between congenital hydrocephalus and risk factors was evaluated using binary logistic regression.
Results: The incidence of congenital hydrocephalus was 2.67 per 1000 pregnancies. The result of multivariate logistic regression indicated that alcohol use and iron with folic acid supplementation during pregnancy were significantly associated with the development of congenital hydrocephalus (OR: 7.64, 95% CI: 1.97– 29.66 and p-value: 0.003 and OR: 0.186, 95% CI: 0.07– 0.49 and p-value: 0.001, respectively). Maternal exposure to typhus and typhoid and use of antibiotics during early pregnancy were also significantly associated with congenital hydrocephalus. Moreover, significant association was also observed between the simultaneous development of spina bifida and congenital hydrocephalus (p-value 0.03).
Conclusion: In conclusion, alcohol consumption, unprescribed use of antibiotics and infection during pregnancy as well as absence of folic acid supplementation may predispose to congenital hydrocephalus.
Keywords: case control, congenital anomaly, hydrocephalus, nervous system
Introduction
Hydrocephalus is one of the commonest central nervous system anomalies manifested by excessive cerebrospinal fluid (CSF) accumulation within the ventricular system of the brain. It occurs due to the abnormalities in the CSF circulation, ie imbalance between the site of production (choroid plexus) and its sites of absorption.1,2
Hydrocephalus may present at birth (congenital) or develop in later life (acquired). However, some forms of hydrocephalus can be seen at birth, but they are due to another problem. Such type of hydrocephalus remains hidden until aging or the pathology causes it to become symptomatic.1,2
The pathological accumulations of CSF in the ventricular system exert pressure on the surrounding developing brain. If left untreated, the condition leads to various degrees of cognitive impairment, cerebral palsy and visual deficit. In severe case, the condition may be fatal.3
A report from Zhang et al4 investigation depicted that mild-to-moderate hydrocephalus causes structural brain deficit mainly in the middle temporal and middle frontal gyri. In another study, severe hydrocephalus produces compression on the cerebral cortex, with reduction of an overall brain mass and cortical thickness, particularly in the parieto-occipital lobe.5 The cortical tissues are affected by the mechanical injury of the high CSF pressure, secondary changes associated with increased interstitial edema, ischemia and oxidative stress.6
The causes of hydrocephalus are genetic factors, premature birth, infection, intraventricular hemorrhage and structural anomalies of the brain such as neural tube defects, agenesis of the corpus callosum and cerebral aqueduct stenosis.7 From these causes, abnormal brain development, blockage of the cerebral aqueduct, Chiari malformations, and Dandy–Walker malformation are the leading causes of congenital hydrocephalus (CHC).8
The incidence of congenital hydrocephalus differs worldwide. However, it falls in the range between 2.2 and 18 per 10,000 live births. From different types of hydrocephalus, CHC accounts around 50%.9,10
Ultrasound screening has been allowing ever earlier intrauterine diagnosis of congenital hydrocephalus and has been used as the primary diagnostic method for tracking CHC within the population. It is readily available at low cost especially for the developing world where advanced radiologic techniques are insufficient. In addition to this, it has no danger of ionizing radiation. Ultrasound can detect CHC with 90% accuracy even if it is associated or not with other anomalies.11–13
Congenital hydrocephalus is one of the greatest burdens in developing countries, especially in East Africa, with more than 6000 new cases estimated per year. It is a major public health concern.6 Worldwide, more than 300,000 new cases of CHC are reported each year.14
The prevalence of CHC is varied in different population. In California, an overall population prevalence of CHC is to be 5.9 per 10,000 live births.15 In Saudi Arabia, the prevalence of CHC is 1.6 per 1000 live births,16 while in Egypt it is 6.76/1000 live births.14 In addition, based on the study conducted in Denmark, the incidence of CHC is 0.062/1000 live births.17
Several children and maternal-related risk factors have been associated with the development of congenital hydrocephalus. Consanguinity, maternal diabetes, pregnancy-induced hypertension, oligohydramnios, family history of hydrocephalus, drugs intake during pregnancy, lack of prenatal care, multiparous gestation and alcohol use during pregnancy are some reported risk factors associated with the occurrence of CHC.2,14,17,18 Timely and accurate evaluation of risk factors of CHC is a crucial step for the evaluation of prevention programs and to influence public health policy and resource allocation.19,20
In developing countries, including Ethiopia, studies on such topics are limited. Thus, the aim of this study was to investigate the incidence and associated risk factors of CHC in Dessie town, North East Ethiopia.
Subjects and Methods
Study Setting
The study was conducted in the Ultrasound center of Ethiopian Family Guidance Association (EFGA) North East Model Clinics in Dessie Town. The town is located 400 kms North East to Addis Ababa, the capital city of Ethiopia. The ultrasound center is used as a diagnostic center for many patients including pregnant women either coming to the clinics or referred from different health centers in Dessie town.
Study Design
An unmatched case–control study was utilized to investigate the incidence and associated risk factors of CHC.
Sample Size and Sampling Technique
The sample size was calculated using Epi info version 7 considering the following assumptions: proportion of mothers who had a family history of CHC and gave birth to a baby with hydrocephalus were 15% and those who did not were 2%,16 95% confidence interval, 80% power and case to control ratio of 1:3. This gave a total sample size of 124 (31:93). Considering 10% non-response rate, the final sample size was 136. Conveniently, the data were collected prospectively from March 2019 to February 2020. In this study, cases and control were pregnant women who conceived fetus with hydrocephalus or not, respectively. For every diagnosis of congenital hydrocephalus by ultrasound (case), the next three women with non-hydrocephalus pregnancies were considered as controls.
Data Collection Tools and Techniques
Maternal related data (risk factors of CHC) were collected by a Midwife using pretested structured questionnaire and fetal related data (number, sex and gestational age of the fetuses as well as the presence of congenital anomalies) were taken from Ultrasound reading. Ultrasound findings were interpreted by a senior radiologist. We have excluded refusers and seriously ill women.
Data Analysis
Data entry and analysis were done by Epi info 7 and SPSS 24. Binary logistic regression with descriptive statistics was conducted. Univariate analysis was performed to check the association between the dependent variable and each independent variable. Then each predictor variable with a p-value less than 0.2 was selected for multivariate analysis. Finally, variables with p-value <0.05 were taken as statistically significant in the multivariate logistic regression. Odds ratio (OR) and 95% confidence interval (CI) were used to express the strength of association. The results are presented in text, tables and figures.
Results
In the study period, the total number of pregnant women who visited the ultrasound center of EFGA Dessie Clinics was twelve thousand seven hundred thirteen (12,713). Obstetric ultrasound was prescribed as routine antenatal care (ANC) service. During the study period, 34 pregnant women were diagnosed as conceiving a fetus with CHC and 102 pregnant women were taken as control. In this research, the incidence of CHC was 2.67 per one thousand pregnancies.
Regarding the different sociodemographic characteristics of the cases and controls, their values were respectively 50% and 45.1% in the age range of 21–25 years, 41.2% and 43.1% completed high school education, 91.2% and 92.1% Amhara in ethnicity, 73.5% and 76.5% lived in the urban area and 88.2% and 94.1% did not work in factories (Table 1). With regard to the sex distribution of fetuses with CHC, 58.8% were females and the rest males (Table 2).
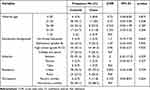 |
Table 1 Univariate Analysis of the Association Between CHC and Sociodemographic Factors (Cases N = 34) and (Controls n = 102) |
 |
Table 2 Univariate Analysis of the Association of Risk Factors and Occurrence of CHC (Cases N = 34) and (Controls n = 102) |
The result of univariate logistic regression reported that all maternal sociodemographic characteristics, sex of the fetuses, khat chewing during pregnancy, ANC follow-up and consanguinity did not show significant correlation with the development of congenital hydrocephalus (Tables 1 and 2).
Three congenital anomalies/clinical conditions were simultaneously detected in 23.5% of the fetuses with CHC. These were spina bifida (11.8%), polyhydramnios (8.8%) and oligohydramnios (2.9%). Among these, spina bifida was significantly associated with CHC, p = 0.03 (Figure 1).
 |
Figure 1 Congenital anomalies/clinical conditions present in association with case and control fetuses, respectively. Numbers indicate relative percentage for the occurrence of each anomaly. |
In addition to univariate analysis, some of the independent variables were entered into multivariate logistic regression (rejection level, p-value < 0.2). The result of multivariate logistic regression analysis indicated that alcohol use as well as iron with folic acid supplementation during pregnancy was significantly associated with the occurrence of CHC (OR: 7.64, 95% CI: 1.97–29.66 and p = 0.003 and OR: 0.186, 95% CI: 0.07–0.49 and p-value; 0.001 respectively) (Table 3).
 |
Table 3 Multivariate Analysis of the Association Between Risk Factors and Presence of Congenital Hydrocephalus (Cases N = 34) and (Controls n = 102) |
From the different diseases present during pregnancy, only typhus and typhoid infection were associated with CHC (OR: 5.03, 95% CI: 1.48–17.11 and p = 0.01). While from the drugs used during pregnancy, undocumented antibiotic use was correlated with CHC (OR: 5.69, 95% CI: 1.28–25.26 and p = 0.02) (Table 4).
 |
Table 4 Association Between Congenital Hydrocephalus and Exposure to Risk Factors During Pregnancy (Cases N = 34) and (Controls n = 102) |
Discussion
Recently, the advancement of prenatal screening and diagnostic tools for pregnant women ameliorates early detection of congenital anomalies. Literatures reported that hydrocephalus is the easiest congenital anomaly to be diagnosed using ultrasonographic examination.12 Following diagnosis, severe anomalies are usually terminated. This early termination will decrease its prevalence at birth. The use of imaging techniques is an important method for accurate investigation of congenital anomalies, especially for countries with poor patient profile documentation. This study investigated the incidence of CHC in prenatally diagnosed fetuses using obstetric ultrasound and associated maternal and fetal risk factors.
The incidence of CHC has been reported worldwide differently; 5.9 per 10,000 births in California,15 0.81 per 1000 pregnancies in France,21 0.062 per 1000 births in Denmark,17 1.47 per 1000 live births in rural tertiary care center in India,22 1.6 per 1000 live births in Saudi Arabia,16 6.76 per 1000 live births in Sohag, Egypt and 0.4% per 5000 pregnancies in Sudan.23 Based on ultrasound diagnosis, the incidence of CHC in the current study was 2.67 per one thousand pregnancies. The difference in terms of case definition, type of study and the nature of cases included makes incidence comparison of CHC difficult bearing in mind the geographical and ethnic disparities.23
In our study, most (58.8%) of the affected fetuses were female (Table 2). Such finding is also mentioned by Stoll et al 1992, Jeng et al 2014, and Kadian et al 2017.15,21,22 In contrast to this finding, a higher prevalence of CHC was reported in male fetuses in Sudan,23 Denmark,17 and Jordan.24 This disparity may be due to the variation in the overall birth ratio and ethnic difference.18,23
In the current investigation, maternal use of alcohol during early pregnancy was a significant risk factor for the development of CHC. The result is consistent with the following researches: Van Landingham et al, 2009, Clarren et al, 1978 and Swayze et al, 1997.2,25,26 This finding supported the idea that alcohol can disturb neurodevelopment since ethanol exposure affected cellular differentiation during neurulation.26,27
A plenty of research finding indicated that lack of folic acid use during pregnancy predisposes to the development of neural tube defects.28–30 On the other hand, the current study revealed significant protective effect of iron with folic acid supplementation during early pregnancy against the occurrence of CHC (p-value 0.001). This is also reported by Qadir et al 201731 as lack of folic acid supplementation is one of the commonest causes of congenital anomalies. This finding may uphold the idea that anomalies of the neural tube can be the cause of CHC. Because, in this finding, spina bifida simultaneously occurred with CHC in a significant manner.
Unprescribed/undocumented use of antibiotics during pregnancy was more common in pregnant women who conceived fetus with CHC than the controls. This use of antibiotics was a significant factor for the occurrence of CHC (p-value 0.02). Different reports indicated this association for a variety of drugs: antidepressant by Munch et al, 2014,17 a drug for the treatment of hemorrhoid by Kubicsek et al, 2011,32 and vaginal use of metronidazole by Kazy et al, 2005.33
The other risk factor that showed significant correlation with CHC development was exposure to typhus and typhoid illness during pregnancy. Multiple maternal illnesses like hypertension, diabetes, cytomegalovirus and Toxoplasma gondii infections had been reported as risk factors of congenital anomalies.2,17,34 The variation in terms of illness indicates the level of health care coverage in Ethiopia. Because typhus and typhoid illnesses are diseases of poor hygiene.
In the current study, only 76.5% of the cases were isolated CHC. The rest cases were presented with spina bifida, oligohydramnios and polyhydramnios. Among the three, spina bifida was significantly correlated with the occurrence of CHC at p = 0.03. In line with this finding, many central nervous system anomalies are associated with CHC commonly spina bifida and also Arnold-Chiari malformation and Dandy–Walker malformation.15,23
Even though not statistically significant, the blood relationship between the fetus parents was seen in 5.9% of the cases. However, this percentage was reported very high in Egypt (58%),14 Saudi Arabia (73%),16 Arar city, Northern Saudi Arabia (60.9%).35 This disparity may be due to cultural and religious differences.
Conclusion
The incidence of CHC was 2.67 per one thousand pregnancies which is relatively higher than the prevalence in European countries and lower than in Egypt. Significant risk factors identified were alcohol and antibiotics use during pregnancy, maternal exposure to typhus and typhoid infection and lack of iron and folic acid supplementation during pregnancy. Spina bifida was a commonly associated central nervous system anomaly with congenital hydrocephalus.
Finally, we recommend continued investigation on risk factors of CHC and appropriate preventive methods should be designed. In addition, antenatal care services should include health education on maternal risk factors.
Abbreviations
ANC: antenatal care, AOR: adjusted odds ratio, CI: confidence interval, CHC: congenital hydrocephalus, COR: crude odds ratio, EFGA: Ethiopian Family Guidance Association, OR: odds ratio, SPSS: Statistical Package for Social Science.
Data Sharing Statement
All data are included in the manuscript.
Ethical Approval and Informed Consent
The entire activities of this research work including verbal informed consent process were approved by departmental ethical review board of Wollo University and EFGA Clinic. This study was carried out in accordance with the Declaration of Helsinki. Informed verbal consent was also obtained from the participant mothers. All data collection tools were made anonymously to keep confidentiality of data. Participation in the study was made fully voluntary based.
Acknowledgment
We valued the support of staff members of Ethiopian Family Guidance Association Dessie Clinic. We also extend our thanks to the participant pregnant mothers who volunteered to take part in the study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
No specific grant was obtained for this research.
Disclosure
All authors declare that they have no conflicts of interest in this work.
References
1. Tully HM, Capote RT, Saltzman BS. Maternal and infant factors associated with infancy-onset hydrocephalus in Washington State. Pediatr Neurol. 2015;52(3):320–325. doi:10.1016/j.pediatrneurol.2014.10.030
2. Van Landingham M, Nguyen TV, Roberts A, Parent AD, Zhang J. Risk factors of congenital hydrocephalus: a 10 year retrospective study. J Neurol Neurosurg Psychiatry. 2009;80(2):213–217.
3. Christensen J, Hansen L, Garne E. Congenital hydrocephalus-prevalence and prognosis. Mortality and morbidity in a population-based study. Ugeskr Laeger. 2003;165(5):466–469.
4. Zhang S, Ye X, Bai G, et al. Alterations in Cortical Thickness and White Matter Integrity in Mild-to-Moderate Communicating Hydrocephalic School-Aged Children Measured by Whole-Brain Cortical Thickness Mapping and DTI. Neuralplasticity. 2017;4:1–6.
5. Fletcher JM, McCauley SR, Brandt ME, et al. Regional brain tissue composition in children with hydrocephalus: relationships with cognitive development. Arch Neurol. 1996;53(6):549–557.
6. Castejon O. Transmission electron microscope study of human hydrocephalic cerebral cortex. J Submicrosc Cytol Pathol. 1994;26(1):29–39.
7. Zhang J, Williams MA, Rigamonti D. Genetics of human hydrocephalus. J Neurol. 2006;253(10):1255–1266.
8. Huang Y-H, Wu Q-J, Chen Y-L, et al. Trends in the prevalence of congenital hydrocephalus in 14 cities in Liaoning province, China from 2006 to 2015 in a population-based birth defect registry from the Liaoning Women and Children’s Health Hospital. Oncotarget. 2018;9(18):14472–14480.
9. Garne E, Loane M, Addor M-C, Boyd PA, Barisic I, Dolk H. Congenital hydrocephalus-prevalence, prenatal diagnosis and outcome of pregnancy in four European regions. Eur j Paediatric Neurol. 2010;14(2):150–155.
10. Schrander-Stumpel C, Fryns J-P. Congenital hydrocephalus: nosology and guidelines for clinical approach and genetic counselling. Eur J Pediatr. 1998;157(5):355–362.
11. Cavalcanti DP, Salomão MA. Incidence of congenital hydrocephalus and the role of the prenatal diagnosis. J Pediatr (Rio J). 2003;79(2):135–140.
12. Nyberg D, Mack L, Hirsch J, Pagon R, Shepard T. Fetal hydrocephalus: sonographic detection and clinical significance of associated anomalies. Radiology. 1987;163(1):187–191.
13. Pober B, Greene M, Holmes L. Complexities of intraventricular abnormalities. J Pediatr. 1986;108(4):545–551.
14. Ali M, Abdelaal M. Epidemiological study of Congenital Hydrocephalus in Sohag Governorate. Egyptian J Commun Med. 2015;33(2):49–55.
15. Jeng S, Gupta N, Wrensch M, Zhao S, Wu YW. Prevalence of congenital hydrocephalus in California, 1991-2000. Pediatr Neurol. 2011;45(2):67–71.
16. Murshid WR, Jarallah JS, Dad MI. Epidemiology of infantile hydrocephalus in Saudi Arabia: birth prevalence and associated factors. Pediatr Neurosurg. 2000;32(3):119–123.
17. Munch TN, Rasmussen M-LH, Wohlfahrt J, Juhler M, Melbye M. Risk factors for congenital hydrocephalus: a nationwide, register-based, cohort study. J Neurol Neurosurg Psychiatry. 2014;85(11):1253–1259.
18. Tully HM, Dobyns WB. Infantile hydrocephalus: a review of epidemiology, classification and causes. Eur J Med Genet. 2014;57(8):359–368.
19. Kalyvas AV, Kalamatianos T, Pantazi M, Lianos GD, Stranjalis G, Alexiou GA. Maternal environmental risk factors for congenital hydrocephalus: a systematic review. Neurosurg Focus. 2016;41(5):E3 1–7.
20. Sun G, Xu Z-M, Liang J-F, Li L, Tang D-X. Twelve-year prevalence of common neonatal congenital malformations in Zhejiang Province, China. World j Pediatrics. 2011;7(4):331–336.
21. Stoll C, Alembik Y, Dott B, Roth M. An epidemiologic study of environmental and genetic factors in congenital hydrocephalus. Eur J Epidemiol. 1992;8(6):797–803.
22. Kadian YS, Verma A, Kajal P, Duhan N. Congenital hydrocephalus-An epidemiological study of maternal characteristics in a tertiary care center. J Evolution Med Dent Sci. 2017;6(75):5393–5396.
23. Mahmoud MZ, Dinar HA, Abdulla AA, Babikir E, Sulieman A. Study of the association between the incidences of congenital anomalies and hydrocephalus in Sudanese fetuses. Glob J Health Sci. 2014;6(5):1–8.
24. Alebous HDA, Hasan AA. Prevalence of congenital hydrocephalus in the Hashemite kingdom of Jordan: a hospital-based study. Natural Sci. 2012;4(10):789–791.
25. Clarren SK, Alvord JEC, Sumi SM, Streissguth AP, Smith DW. Brain malformations related to prenatal exposure to ethanol. J Pediatr. 1978;92(1):64–67.
26. Swayze VW, Johnson VP, Hanson JW, et al. Magnetic resonance imaging of brain anomalies in fetal alcohol syndrome. Pediatrics. 1997;99(2):232–240.
27. Bearer CF. L1 cell adhesion molecule signal cascades: targets for ethanol developmental neurotoxicity. Neurotoxicology. 2001;22(5):625–633.
28. Centers for Disease Control Prevention. Spina bifida and anencephaly before and after folic acid mandate-United States, 1995-1996 and 1999-2000. MMWR Morb Mortal Wkly Rep. 2004;53(17):362–365.
29. Klusmann A, Heinrich B, Stopler H, Gartner J, Mayatepek E, Von Kries R. A decreasing rate of neural tube defects following the recommendations for periconceptional folic acid supplementation. Acta Paediatrica. 2005;94(11):1538–1542.
30. Parker SE, Mai CT, Canfield MA, et al. Updated national birth prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Research Part A. 2010;88(12):1008–1016.
31. Qadir M, Amir S, Bano S. Prevalence and Associated Risk Factors of Congenital Anomalies at a tertiary care hospital. Pakistan J Med Health Sci. 2017;11(3):942–945.
32. Kubicsek T, Kazy Z, Czeizel AE. Teratogenic potential of tribenoside, a drug for the treatment of haemorrhoids and varicose veins-a population-based case-control study. Reproduct Toxicol. 2011;31(4):464–469.
33. Kazy Z, Puhó E, Czeizel AE. Teratogenic potential of vaginal metronidazole treatment during pregnancy. Eur J Obstetrics Gynecol Reproductive Biol. 2005;123(2):174–178.
34. Simeone RM, Rasmussen SA, Mei JV, et al. A pilot study using residual newborn dried blood spots to assess the potential role of cytomegalovirus and Toxoplasma gondii in the etiology of congenital hydrocephalus. Birth Defects Res a Clin Mol Teratol. 2013;97(7):431–436.
35. Alenezi AT, El-Fetoh NMA, Hussain MA, et al. Congenital Hydrocephalus in Arar, Northern Saudi Arabia. Egyptian J Hospital Med. 2018;71(3):2651–2656.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
