Back to Journals » Clinical Ophthalmology » Volume 18
Conformation of Horizontal Extraocular Muscle Insertions in Acute Acquired Concomitant Esotropia Induced by Excessive Digital Device Usage
Authors Hayashi R, Hayashi S, Nishimura T, Machida S
Received 14 September 2023
Accepted for publication 2 December 2023
Published 6 January 2024 Volume 2024:18 Pages 41—47
DOI https://doi.org/10.2147/OPTH.S440322
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Rijo Hayashi,1 Shimmin Hayashi,1,2 Tomoharu Nishimura,1 Shigeki Machida1
1Department of Ophthalmology, Saitama Medical Center, Dokkyo Medical University, Koshigaya, Saitama, Japan; 2Lively Eye Clinic, Soka, Saitama, Japan
Correspondence: Rijo Hayashi, Department of Ophthalmology, Saitama Medical Center, Dokkyo Medical University, 2-1-50, Minamikoshigaya, Koshigaya, Saitama, 3438555, Japan, Tel/Fax +81-48-965-8659, Email [email protected]
Purpose: Acute acquired concomitant esotropia induced by excessive digital device usage, especially smartphones (SAACE), has been increasing over the past few years. Convergence spasm induced by excessive near work has been suggested as a mechanism. Anatomical differences could also potentially contribute to SAACE onset. The present study investigated the conformation of horizontal recti between SAACE patients and normal subjects.
Patients and Methods: In 15 SAACE patients (SAACE group), the distances between the limbus and insertion of the horizontal recti (LI distance) and the widths of horizontal recti on the insertion (insertion width) were measured. The control group consisted of 30 patients who underwent retinal detachment surgery. Differences in LI distances and insertion widths were compared between SAACE and control groups.
Results: While there were no differences between the two groups for LI distances and insertion widths of lateral recti, there were significantly shorter LI distances for the medial recti in the SAACE group (P< 0.05). Moreover, the SAACE group tended to exhibit larger insertion widths of the medial recti. Medial/lateral ratio of LI distances were significantly lower and insertion widths were significantly higher in the SAACE compared to the control group (P< 0.05).
Conclusion: Based on the observations of more anterior insertion and larger muscle widths, this suggests there are stronger forces of medial recti in SAACE. In addition to excessive accommodation followed by increases in medial recti tonus, the results also suggest that an anatomical imbalance between lateral and medial recti contributes to esotropia onset following excessive near work.
Keywords: acute acquired concomitant esotropia, digital devices, extraocular muscles, insertion distance, insertion width
Introduction
Acute acquired concomitant esotropia (AACE) is known as an acute onset of esotropia characterized by an equal angle of deviation in all fields of gaze.1,2 Many etiologies have been considered to cause AACE. Several studies have suggested an association between intracranial disorders and AACE.3,4 Excessive accommodation is also one of the suggested etiologies.5 Increases in AACE have been reported,6 of which a large proportion were due to excessive usage of digital devices7–9 including smartphones, tablets and computers. This special type of AACE,10–14 which is called smartphone-associated AACE (SAACE) herein, is thought to be induced by convergence spasm that follows excessive near work, with refraining from excessive near work suggested to be effective in helping to decrease the degree of esodeviation.10 Several factors, such as uncorrected myopia,1,15 accommodative spasm1,16 and intracranial diseases,5,17 are considered to play important roles in SAACE. Few studies have evaluated the possible association with the anatomical peculiarities of the horizontal recti. During patient surgery, enlargement of the medial rectus in some of our SAACE patients was observed.18 In the present study, we measured the conformation of the horizontal recti and evaluated the possible association with the onset of SAACE.
Materials and Methods
Among the patients who had not been previously diagnosed with any type of strabismus or amblyopia, and exhibited onset of esotropia shortly after exceeding 4 hours of digital device usage every day, 15 patients who underwent surgery were enrolled as the SAACE group. None of these patients had any history of ocular diseases, ocular surgery, or systemic diseases, including diabetes and neurologic diseases. There were no abnormal ocular movements among the included patients. All enrolled patients underwent brain and orbital computed tomography or magnetic resonance imaging in order to exclude intracranial and extraocular muscle abnormalities. After obtaining informed consent, all patients underwent baseline examinations, which included angles of esotropia, refraction errors and axial length. For the control group, we enrolled 30 patients who underwent buckling surgeries for retinal detachment. Patients in the control group also underwent baseline examinations similar to that for the SAACE group. None of the patients in the control group had strabismus or systemic diseases, which included diabetes and neurologic diseases.
After the isolation of the medial and lateral recti (MR and LR) during the surgery, the distances from the limbus to the middle of the muscle insertion (the distance between the limbus and insertion, LI distance) and the muscle width at its insertion point (insertion width) were measured with a caliper prior to the disinsertion. All procedures followed the tenets of the Declaration of Helsinki. Approval was granted by the Institutional Human Experimentation Committee of the Saitama Medical Center, Dokkyo Medical University (Approval number: 21098).
LI distances and insertion widths of the MR and LR were compared between the SAACE and control groups. The medial/lateral (ML) ratio of the LI distance and that of insertion widths were also calculated. The LI distances/axial length ratios were also calculated as the LI distances divided by the axial length. Furthermore, the MRw/in was defined as the values of the insertion width divided by the LI distances, with this calculation used to evaluate the strength of the MR. We also calculated the LRw/in, which was used for the LR. All of these values were compared between the two groups using a t-test, with the significance set at a P-value of 0.05. All statistical analyses were performed with IBM®SPSS Statistics 28.
Results
Table 1 presents the characteristics of the enrolled patients. Although patients in the SAACE group were younger than those in the control group (P=0.0003), there were no differences found between the two groups for the refraction errors and axial length. As compared to the control group, the LI distances of the MR were shorter (P=0.0161)) and there was a tendency for larger insertion widths in the SAACE group. However, there were no differences observed between the two groups for the LI distances and insertion widths of the LR.
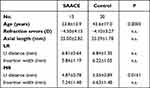 |
Table 1 Characteristics of Enrolled Patients |
As compared to the control group, there was a lower ML ratio for the LI distance (P=0.0068) and a higher ML ratio for insertion width (P=0.0412) in the SAACE group (Figure 1). Even though there was no difference in the LR between the two groups, the LI distances/axial length ratios of the MR were lower in the SAACE group (P=0.0164) (Figure 2). Furthermore, although the observed LRw/in did not differ between the two groups, the MRw/in was higher in the SAACE group (P=0.0046) (Figure 3).
Discussion
The results of this study showed that there was a shorter LI distance and a larger insertion width for the MR. In addition, the larger MRw/in, insertion width divided by LI distance, indicated stronger MR in SAACE compared to the control. However, there was no difference in measurements of LR. These results suggest that a stronger MR is one of the possible factors that can induce SAACE.
Three major types of AACE have been defined:1 (1) Swan type, which is esotropia due to the disruption of fusion following monocular occlusion or vision loss in young children; (2) Burian-Franceschetti, which is esotropia associated with physical or psychological stress in young patients; and (3) Bielschowsky type, which is esotropia in young uncorrected myopia with excessive near work. Excessive near work with excessive accommodation followed by convergence spasm has been suggested to be the mechanism of this esotropia.19 Since the convergence spasm in this condition cannot be relaxed during distance fixation, there is development of esotropia with diplopia. The imbalance between the convergence and divergence forces also leads to the development of increases in the tonus of the medial rectus, which leads to esotropia. Patients enrolled in our current study exhibited the onset of SAACE after several hours of digital device usage. Only 1 out of the 15 patients had emmetropia. The other 14 patients had myopia, with 8 of these patients exhibiting high myopia over −6.0 D. The characteristics found in our patients indicated that there was equal deviation at the near and distance fixation, myopia and adolescent onset after excessive near work, which are similar to that for Bielschowsky esotropia.
Over the last few decades, the usage of handheld devices, which includes smartphones and tablets, has increased, especially during lockdowns due to the COVID-19 pandemic. Binocular disabilities have also been reported after excessive usage of handheld devices.20,21 When using a smartphone, working distances are shorter than that found for typical near working distances,22 with these distances becoming even shorter when there is over 60 minutes of usage.23 Furthermore, some subjects will view text on their smartphones using a smaller font size.22 The smaller visual font size and the shorter visual distances can lead to increases in the demands on the accommodation and convergence, which can cause the spasm of the near reflex. Changes in the tonus of accommodation and binocular vergence have been reported to occur after near work,24 especially after hours of working with these digital devices.24,25 In addition, it has also been suggested that spasm of the near reflex with dynamic activations of the MR could be one of the causes in patients who present with AACE.26
Measuring the characteristics of extraocular muscles is valuable when investigating anomalies in ocular alignment. It has been reported that there were no differences in the LI distances of the MR between esotropia and normal controls, or in exotropia.27,28 However, Cai et al reported finding shorter LI distances for the MR in AACE patients with different causes as compared to exotropia.29 In addition, hypertrophic MR was also observed during surgery in some of our SAACE patients.18 In our present study, we first measured the characteristics of the horizontal extraocular muscles in AACE induced by excess usage of digital devices, ie, SAACE. The results demonstrated that there were shorter LI distances and larger insertion widths for the MR in SAACE as compared to the normal control. However, there were no differences noted for the LR measurements. These results suggest the possibility that SAACE could be also induced by the anatomical characteristics observed in the MR. As compared to the normal controls, there was a lower ML ratio of the LI distance and a higher ML ratio of the insertion width in the SAACE group. Furthermore, there was a higher MRw/in in the SAACE group, while there was no difference noted in the LRw/in between the two groups. These measurements suggest that the imbalance between the MR and LR could also possibly contribute to the onset of SAACE.
Myopia is one risk factor of Bielschowsky type AACE and SAACE. A few studies revealed abnormal fusional amplitude in AACE patients with myopia.30,31 However, it was reported that uncorrected myopia does not occur with AACE30 onset. Although most of our patients in the SAACE group were myopic, as described above, there were no differences between either group for refraction error and axial length since all of the patients in the RD group were myopic. Therefore, the intergroup differences could not attributable to myopia.
Concerning the hours of digital device usage, several patients in our SAACE group reported diplopia occurring after more than 4 hours of continuous smartphone usage, and most of these patients reported using digital devices for more than 4 hours every day. Among our control group, most reported 3 hours of digital device usage every day, which is similar to the 2022 Report on Current Status of Information and Communications by the Ministry of Internet Affairs and Communications.32 There was longer usage of digital device in the SAACE group compared to RD group, and there were differences in the MR measurements. Collectively, these results suggested that the anatomical peculiarities of MR were triggered by excessive usage of digital devices leading to the onset of SAACE.
There were several limitations in this study. The younger age of patients in the SAACE group was the first limitation. The LI distance of the extraocular muscles might be dependent on the refraction errors and axial lengths, which could differ according to age. Thus, it should be taken into consideration that our current results, which showed there was a shorter LI distance of MR, could have potentially been due to the inclusion of younger patients in our SAACE group. However, it has been reported that the LI distances for both the LR and MR were not different between children and adults.33,34 In addition, our present study also found that there were no differences between the SAACE and control groups for the refraction errors and axial lengths. Furthermore, the current results indicated that there were lower LI distances/axial length ratios of the MR in the SAACE group, while no differences were observed in the LR between the two groups. Furthermore, similar results were revealed when data for the 12 patients from the control group, who were in the same age range as the test groups, were analyzed. Therefore, this suggests that the differences between the SAACE and control groups are not due to the differences in age. Currently, the observed associations between the insertion width and age are controversial. The insertion width of the MR has been reported to be smaller in patients with intermittent exotropia who are under 5 years old,35 with no significant differences noted after reaching the age of 18 years and older.27 However, Niyaz et al reported that there was no correlation between the insertion width of the extraocular muscles and age.28 In our present study, we found that there was a larger insertion width of the MR in the SAACE group, even though they were younger than the subjects in the control group. Thus, these results suggest that it is not possible that the larger insertion width in SAACE is due to aging effects. Another limitation is the small study population. Most of the patients with SAACE who visited our clinic showed improvement after limiting their digital device usage and administration of topical cycloplegics,36 and only 15 patients underwent surgical treatment. Further evaluation of additional patients will be necessary to allow for better investigation of the characteristics of SAACE.
A previous study indicated that limiting the usage of digital devices led to good binocularity and an improvement in the esotropia.9 Based on the results of our previous study, we determined that in addition to limiting the usage of digital devices, the administration of topical cycloplegics was also found to be effective among SAACE subjects.36 Furthermore, Botox injections have also been reported to be effective in treating SAACE.37,38 In addition, improvement in the strabismus angles and restoration of binocularities were reported to occur after surgery in SAACE subjects,39 also in who were resistant to the treatment of topical cycloplegics and Botox.36–38 Thus, surgical intervention can be considered an effective treatment for SAACE. However, since different satisfactory outcomes have occurred after the same surgical formula with different LI distances,27 this suggests that the anatomical characteristics of the MR need to be taken into consideration during the surgical intervention for SAACE.
Conclusion
In SAACE, the more anterior insertion and larger muscle widths suggested stronger forces of the MR. In addition to excessive accommodation followed by increases in the tonus of the MR, the anatomical imbalance between the LR and MR also appears to contribute to the onset of esotropia following excessive near work. These results suggest that the characteristic conformation of the horizontal extraocular muscles should be taken into consideration when designing the surgical formula for SAACE.
Disclosure
The authors declare that they have no competing interests and this research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
1. Burian HM, Miller JE. Comitant convergent strabismus with acute onset. Am J Ophthalmol. 1958;45(4):55–64. doi:10.1016/0002-9394(58)90223-X
2. Clark AC, Nelson LB, Simon JW, Wagner R, Rubin SE. Acute acquired comitant esotropia. Br J Ophthalmol. 1989;73(8):636–638. doi:10.1136/bjo.73.8.636
3. Nouraeinejad A. Neurological pathologies in acute acquired comitant esotropia. Graefes Arch Clin Exp Ophthalmol. 2023;5:1–8.
4. Hu Y, Wang S, Wu L, Xi S, Wen W, Zhao C. Deficits of visual cortex function in acute acquired concomitant esotropia patients. Invest Ophthalmol Vis Sci. 2023;64(13):46. doi:10.1167/iovs.64.13.46
5. Buch H, Vinding T. Acute acquired comitant esotropia of childhood: a classification based on 48 children. Acta Ophthalmol. 2015;93(6):568–574. doi:10.1111/aos.12730
6. Lim CW, Lee J, Kim WJ. Changes in the number and characteristics of patients with acute acquired concomitant esotropia over time: an 8-year retrospective study. Medicine. 2023;102(22):e33986. doi:10.1097/MD.0000000000033986
7. Zhu M, Tang Y, Wang Z, et al. Clinical characteristics and risk factors of acute acquired concomitant esotropia in last 5 years: a retrospective case-control study. Eye. 2023;37(2):320–324. doi:10.1038/s41433-022-01939-1
8. Roda M, Di Geronimo N, Valsecchi N, et al. Epidemiology, clinical features, and surgical outcomes of acute acquired concomitant esotropia associated with myopia. PLoS One. 2023;18(5):e0280968. doi:10.1371/journal.pone.0280968
9. Okita Y, Kimura A, Masuda A, et al. Yearly changes in cases of acute acquired comitant esotropia during a 12-year period. Graefes Arch Clin Exp Ophthalmol. 2023;261(9):2661–2668. doi:10.1007/s00417-023-06047-8
10. Lee HS, Park SW, Heo H. Acute acquired comitant esotropia related to excessive smartphone use. BMC Ophthalmol. 2016;16:37.
11. Mehta A, Greensher JE, Dahl GJ, Miller KE. Acute onset esotropia from excessive smartphone use in a teenager. J Pediatr Ophthalmol Strabismus. 2018;55(6):e42–e44. doi:10.3928/01913913-20181017-01
12. Vagge A, Giannaccare G, Scarinci F, et al. Acute acquired concomitant esotropia from excessive application of near vision during the COVID-19 lockdown. J Pediatr Ophthalmol Strabismus. 2020;57(6):e88–e91. doi:10.3928/01913913-20200828-01
13. Mohan A, Sen P, Mujumdar D, Shah C, Jain E. Series of cases of acute acquired comitant esotropia in children associated with excessive online classes on smartphone during COVID-19 pandemic; digital eye strain among kids (DESK) study-3. Strabismus. 2021;29(3):163–167. doi:10.1080/09273972.2021.1948072
14. Neena R, Remya S, Anantharaman G. Acute acquired comitant esotropia precipitated by excessive near work during the COVID-19-induced home confinement. Indian J Ophthalmol. 2022;70(4):1359–1364. doi:10.4103/ijo.IJO_2813_21
15. Zhang J, Chen J, Lin H, Huang L, Ma S, Zheng W. Independent risk factors of type III acute acquired concomitant esotropia: a matched case-control study. Indian J Ophthalmol. 2022;70(9):3382–3387. doi:10.4103/ijo.IJO_318_22
16. Kaur S, Sukhija J, Khanna R, Takkar A, Singh M. Diplopia after excessive smart phone usage. Neuroophthalmology. 2018;43(5):323–326. doi:10.1080/01658107.2018.1518988
17. Williams AS, Hoyt CS. Acute comitant esotropia in children with brain tumors. Arch Ophthalmol. 1989;107(3):376–378. doi:10.1001/archopht.1989.01070010386029
18. Hayashi R, Hayashi S, Machida S. The treatment of acute acquired comitant esotropia persist over one year. Jpn J Ophthalmol Surg. 2022;35(1):148–153.
19. Campos EC. Why do the eyes cross? A review and discussion of the nature and origin of essential infantile esotropia, microstrabismus, accommodative esotropia, and acute comitant esotropia. J AAPOS. 2008;12(4):326–331. doi:10.1016/j.jaapos.2008.03.013
20. Jaiswal S, Asper L, Long J, Lee A, Harrison K, Golebiowski B. Ocular and visual discomfort associated with smartphones, tablets and computers: what we do and do not know. Clin Exp Optom. 2019;102(5):463–477. doi:10.1111/cxo.12851
21. De-Hita-Cantalejo C, García-Pérez Á, Sánchez-González JM, Capote-Puente R, Sánchez-González MC. Accommodative and binocular disorders in preteens with computer vision syndrome: a cross-sectional study. Ann N Y Acad Sci. 2021;1492(1):73–81. doi:10.1111/nyas.14553
22. Bababekova Y, Rosenfield M, Hue JE, Huang RR. Font size and viewing distance of handheld smart phones. Optom Vis Sci. 2011;88(7):795–797. doi:10.1097/OPX.0b013e3182198792
23. Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom. 2017;100(2):133–137. doi:10.1111/cxo.12453
24. Owens DA, Wolf-Kelly K. Near work, visual fatigue, and variations of oculomotor tonus. Invest Ophthalmol Vis Sci. 1987;28(4):743–749.
25. Gratton I, Piccoli B, Zaniboni A, Meroni M, Grieco A. Change in visual function and viewing distance during work with VDTs. Ergonomics. 1990;33(12):1433–1441. doi:10.1080/00140139008925344
26. Goldstein JH, Schneekloth BB. Spasm of the near reflex: a spectrum of anomalies. Surv Ophthalmol. 1996;40(4):269. doi:10.1016/S0039-6257(96)82002-9
27. Lai YH, Wu WC, Wang HZ, Hsu HT. Extraocular muscle insertion positions and outcomes of strabismus surgery: correlation analysis and anatomical comparison of Western and Chinese populations. Br J Ophthalmol. 2012;96(5):679–682. doi:10.1136/bjophthalmol-2011-300632
28. Niyaz L, Yucel OE, Gul A. Medial and lateral rectus muscle insertion distance and width in esotropia and exotropia patients. Curr Eye Res. 2017;42(9):1245–1247. doi:10.1080/02713683.2017.1313429
29. Cai C, Dai H, Shen Y. Clinical characteristics and surgical outcomes of acute acquired comitant esotropia. BMC Ophthalmol. 2019;19(1):173. doi:10.1186/s12886-019-1182-2
30. Ruatta C, Schiavi C. Acute acquired concomitant esotropia associated with myopia: is the condition related to any binocular function failure? Graefes Arch Clin Exp Ophthalmol. 2020;258(11):2509–2515. doi:10.1007/s00417-020-04818-1
31. Zhao S, Hao J, Liu J, Cao K, Fu J. Fusional vergence dysfunctions in acute acquired concomitant esotropia of adulthood with myopia. Ophthalmic Res. 2022. doi:10.1159/000527884
32. Ministry of internet Affairs and Communications. 2022 report on current status of information and communications. Available from: http://www.soumu.go.jp/main_content/000887660.pdf.
33. Ocak OB, İnal A, Yilmaz İ, et al. Measurement of extraocular horizontal muscle insertion distance via anterior segment optical coherence tomography of healthy children and comparison with healthy adults. Int Ophthalmol. 2019;39(5):1037–1042. doi:10.1007/s10792-018-0903-5
34. De-Pablo-Gómez-de-Liaño L, Fernández-Vigo JI, Ventura-Abreu N, et al. Spectral domain optical coherence tomography to assess the insertion of extraocular rectus muscles. APOS. 2016;20(3):201–205.
35. Yun CM, Kim SH. The tendon width of lateral rectus muscle in predicting the effect of recession: is it just age-related artifact? Eye. 2011;25(19):1356–1359. doi:10.1038/eye.2011.178
36. Hayashi R, Hayashi S, Machida S. The effects of topical cycloplegics in acute acquired comitant esotropia induced by excessive digital device usage. BMC Ophthalmol. 2022;22(1):366. doi:10.1186/s12886-022-02590-w
37. Suwannaraj S, Rojanasaksothron C, Methapisittikul Y, Wongwai P, Yospaiboon Y. Botulinum toxin injection versus extraocular muscle surgery for acute acquired comitant esotropia. Clin Ophthalmol. 2023;17:413–420. doi:10.2147/OPTH.S401019
38. Lang LJ, Zhu Y, Li ZG, et al. Comparison of botulinum toxin with surgery for the treatment of acute acquired comitant esotropia and its clinical characteristics. Sci Rep. 2019;9:13869. doi:10.1038/s41598-019-50383-x
39. Yagasaki T, Yokoyama Y, Yagasaki A, et al. Surgical outcomes with and without prism adaptation of cases with acute acquired comitant esotropia related to prolonged digital device use. Clin Ophthalmol. 2023;17:807–816. doi:10.2147/OPTH.S403300
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



