Back to Journals » Risk Management and Healthcare Policy » Volume 15
Concurrent Rising of Dry Eye and Eye Strain Symptoms Among University Students During the COVID-19 Pandemic Era: A Cross-Sectional Study
Authors Uwimana A , Ma C, Ma X
Received 8 September 2022
Accepted for publication 23 November 2022
Published 7 December 2022 Volume 2022:15 Pages 2311—2322
DOI https://doi.org/10.2147/RMHP.S388331
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Alexandre Uwimana,* Cong Ma,* Xiang Ma
Department of Ophthalmology, the First Affiliated Hospital of Dalian Medical University, Dalian, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiang Ma, Department of Ophthalmology, the First Affiliated Hospital of Dalian Medical University, 222 Zhongshan Road, Xigang District, Dalian, 116044, People’s Republic of China, Tel +8618098876399, Fax +8641183622844, Email [email protected]
Purpose: Students spend extended hours using electronic devices due to online teaching. Digital eye strain (DES) and dry eye disease (DED) symptoms are both associated with prolonged screen exposure time and may co-occur. This study aimed to evaluate the correlation between DES and DED symptoms and determine the prevalence of DED according to the severity of DES.
Patients and Methods: This cross-sectional study was conducted among international students in Chinese universities. The survey was built using Wenjuan Mini Program and distributed using the WeChat platform. The questionnaire assessed participants’ screen exposure, the 20-20-20 rule, ED practices, and DED awareness. Computer Vision Syndrome Questionnaire (CVS-Q) and Dry Eye Questionnaire (DEQ-5) were used to diagnose DES and DED symptoms, respectively.
Results: 498 students completed the survey, but 452 were considered for the study. Predictors of DES and DED symptoms were conjunctivitis, eye allergy, glares, tired eye, neck pain, back pain, PhD students, and daily spending > 9h on screen (P < 0.05 for all). We observed that an increase in DES scores also exponentially increases DED scores. Among students diagnosed with DES symptoms, 26.5% had mild to moderate DED symptoms, and 8.2% had severe DED symptoms. In contrast, only 8.4% and 0.9% of those with asymptomatic DES had mild to moderate and severe DED symptoms, respectively (P < 0.000). A strong and significant positive correlation (r = 0.695, P < 0.000) between DES and DED scores was found.
Conclusion: We found an extremely high prevalence of DES and DED symptoms compared to the previous studies with a similar population group. We believe that the prevalence of DED may be underestimated in the young population. Training about proper ED practices is mandatory to prevent these deleterious ocular surface conditions.
Keywords: COVID-19 pandemic, digital eye strain, dry eye disease, electronic device, online study, university students
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic has changed our former overall way of living, driving us to a new normal lifestyle. Almost all sectors were affected; however, the present study will focus on the deterioration of students’ ocular health due to online classes. Several universities are still implementing online teaching platforms in order to limit COVID-19 spread in campus environments; as a result, students spend extended hours daily using electronic devices. However, although China is in the recovery process and some universities are slowly reintroducing physical teaching, most international students are still using online education, mainly because they share classes with their peers who left China at the beginning of the pandemic. Since then, they have been unable to come back due to the borders closure policy.
Digital eye strain (DES), also called computer vision syndrome (CVS), is a major global health concern of the 21st century.1 It affects nearly 70–75% of all electronic device (ED) users, with a worldwide estimation of 60 million people and millions of new cases each year.1,2 According to the American Optometric Association (AOA), DES is a set of visual and ocular discomforts occurred after extended exposure to an ED screen. The risk factors of DES include poor brightness and luminosity, glares, inappropriate screen distances, improper ergonomics and postures, non-corrected refractive errors, and environmental factors.3
Excessive use of ED is the leading risk of exposure to DED.4 The blinking rates are 22 blinks/min while relaxing, 10 blinks/min while reading on a paper, and 7 blinks/min while viewing on a digital screen.5 This causes poor dispersion of tear film, which leads to inadequate lipid layer, unstimulated meibomian glands, and ocular surface evaporation; thus, eyestrain symptoms such as eye dryness, burning, itching, and grittiness.6
DED is among the most common reasons for ophthalmology visits.4 As reported by the Tear Film Ocular Surface Society (TFOS) Dry Eye Workshop (DEWS) II, DED is the frequently complex disorder of tear film and ocular surface (cornea and conjunctiva) defined by alteration of lacrimal dynamics and hyperosmolarity.7 DED significantly affects the quality of life (QoL) of affected people and reduces their productivity.8 In the United States, the total loss of productivity due to DED was estimated to be $55,4 billion per year.9
DES and DED symptoms are both associated with screen exposure time and may co-occur; thus, some DED symptoms can be attributed to DES and vice versa.10 For instance, in the CVS-Q, there are also questions about dry eye symptoms, such as burning, itching, feeling of a foreign body, tearing, excessive blinking, eye redness, eye pain, heavy eyelids, and dryness.
Most previous studies have separately investigated DES and DED symptoms; however, the concurrence of these two conditions has not yet been given an important evaluation. Therefore, based on the definite paucity of literature about the correlation between DES and DED, the present study aimed to evaluate this correlation and determine the prevalence of DED symptoms according to the severity of DES. In addition, this study provides recommendations from our experts regarding safer practices while extensively using ED.
Materials and Methods
Design
A cross-sectional study was conducted among international students in Chinese universities. The survey was built using Wenjuan Mini Program (hosted by WeChat Survey). The questionnaire was distributed using the WeChat tool, the leading social media platform in China, for a period of four weeks. The survey link was randomly posted to groups of international students, and the responding time was limited to 15 minutes to ensure the reliability of the answers. A group of ophthalmologists from a single hospital conducted the study and provided recommendations regarding safer practices while extensively using ED. The study was conducted in accordance with the Declaration of Helsinki and approved by the Ethics Committee of the First Affiliated Hospital of Dalian Medical University. Detailed informed consent has been obtained from the students to participate and publish this paper.
Questionnaire
Socio-demographic information was assessed by asking questions such as age, gender, marital status, learning system, major, level of education, university, and city in China. A history of any general and ocular disorder or surgery was requested. Two questions were asked to assess participants’ screen exposure: 1) how many hours per day do you spend on electronic devices for studying? (Including online studying, e-book reading, academic or research writing), and 2) how many hours per day do you spend on electronic devices for entertainment? (Including social networks, movies, online videos, and games). Moreover, questions were asked to know whether the participant wore eyeglasses or contact lenses. We then collected information on ED usage by asking questions regarding the practice of the 20-20-20 rule, distance from ED, break time when using ED, and usage of antiglare or protective glasses, among others.
Dry Eye Disease
DED was determined by the dry eye questionnaire (DEQ-5). This assessment scale has five questions, represented by the following five symptoms: the frequency of discomfort, dryness, and watery eye, and the intensity of discomfort and dryness. The frequency of symptoms was scored as follows (0 = never, 1 = rarely, 2 = sometimes, 3 = frequently, 4 = constantly), while the intensity was scored as follows (0 = never have it, 1 = not at all intense, 5 = very intense). DEQ-5 total score was calculated by summing the points obtained for each question (1a +1b +2a +2b +3).10 The highest score is 22 points and is interpreted as follows: < 6 points are asymptomatic, 6–11 points indicate mild to moderate DED symptoms, and ≥ 12 points indicate severe DED symptoms.11,12
Digital Eye Strain
DES was assessed by using the computer vision syndrome questionnaire (CVS-Q). The frequency of symptoms was scored as follows: 0 = never, 1 = occasionally, and 2 = often or always, while the intensity was scored as 1 = moderate and 2 = intense. The total score was determined by the formula: ∑ (frequency) × (intensity) and recoded as (0 → 0, 1 or 2 → 1, 4 → 2).13 The maximum score is equal to 32 points, and a score ≥ 6 points indicate that the individual suffers from DES. Scores of DES symptoms are considered mild (6–12), moderate (13–18), and severe (19–32).13,14
Statistical Analysis
Data analyses were performed with IBM SPSS Statistics 25.0 software (SPSS Inc., Chicago, USA). Data were presented by mean ± SD (standard deviation) and number, percentage (n, %). Pearson’s correlation analysis and scatterplots were used to determine the relationship between DES and DED symptoms. The Chi-square test was calculated to establish the association between categorical variables. Univariate logistic regression was performed to identify potential predictors of DES and DED symptoms, and P < 0.15 was selected and used in the multivariate analysis. Multivariate logistic regression was calculated using odd ratios (OR) and 95% confidence intervals (CI). The Cronbach’s alpha test of reliability was conducted to determine the internal consistencies of CVS-Q and DEQ-5. The statistical significance of P < 0.05 was used throughout the analyses.
Results
A total of 498 students completed the survey, of which 46 (9.2%) were excluded; therefore, 452 (90.8%) were analyzed for this study. Out of the excluded participants, 15 did not consent to participate, 12 provided incomplete answers, 13 had preexisting major ocular and/or systemic diseases, and 6 had past ocular surgery.
Students were from 66 countries, located in 82 cities, and enrolled in 176 universities within mainland China. The mean age was 27.25 ± 5.62. The majority of students were male (65.9%). A total of 200 (44.2%) students were studying through online platforms. 170 (37.6%) students were aware of DES and DED symptoms, and 89 (19.7%) were aware of the 20-20-20 rule, while only 18 (4%) practiced it. The description of the sample is summarized in Table 1. Cronbach’s alpha was 0.886 and 0.862 for CVS-Q and DEQ-5, respectively.
 |
Table 1 Socio-Demographic Information |
The mean total score of DES was 6.1 ± 5.1, and the prevalence was 226 (50%) (Figure 1A) at the cut point of 6, with mild DES (38.5%), moderate DES (9.7%), and severe DES (1.8%). The most reported symptoms of DES were headache (62.2%), eye pain (50.8%), tearing eyes (48.4%), itching eyes (45.7%), and eye redness (43.2%). A significant association was found between overall DES score and gender (P = 0.026), wearing eyeglasses (P < 0.000), wearing contact lenses (P < 0.000), and daily time on ED (P = 0.042). Moreover, DES scoring was associated with other ocular disorders: myopia (P = 0.024), astigmatism (P = 0.034), eye allergy (P < 0.000), and conjunctivitis (P < 0.000). Furthermore, factors linked with higher DES and DED scores are highlighted in Table 2.
 |
Table 2 Factors Linked with Higher DES and DED Mean Scores |
 |
Figure 1 Prevalence of (A) digital eye strain (DES) and (B) dry eye disease (DED) symptoms among participants. |
On the other hand, the overall DED mean score was 5.4 ± 4.8. Participants diagnosed with DED symptoms were 199 (44.1%) (Figure 1B), of which 35% had mild to moderate DED, and 9.1% had severe DED (cutoff = 6 points). The frequency of DED symptoms was watery eyes (57.8%), eye discomfort (47.5%), and eye dryness (45.9%). The results showed an association between DED total scores and level of education (P = 0.013), wearing eyeglasses (P = 0.002), wearing contact lenses (P < 0.000), myopia (P = 0.031), hypermetropia (P = 0.001), astigmatism (P < 0.000), eye allergy (P < 0.000), and conjunctivitis (P < 0.000). Additionally, asymptomatic DED predominated among students who studied from classrooms (4.75 ± 4.14), aged between 18–24 (4.69 ± 4.21), undergraduate (4.77 ± 4.19), non-eyeglasses nor contact lens wearers (4.82 ± 4.15; 5.27 ± 4.26, respectively), readers at an arm’s distance or within 25–40cm (4.71 ± 4.05; 5.36 ± 4.22, respectively), who use ED for < 3h/day to study (4.74 ± 4.13) and to entertain (4.62 ± 3.98), and who take a break every 20 minutes (4.52 ± 3.97) and every 1h (5.37 ± 4.16).
Univariate and multivariate odds ratios of DES and DED symptoms by demographic and clinical characteristics are presented in Tables 3 and 4. Sensitivity analysis was conducted by incorporating all confounding predictors of DES and DED symptoms with univariate logistic regression P < 0.15 in the multivariate logistic regression model. Multivariate logistic regression was performed based on the observation that conjunctivitis, eye allergy, glares, tired eye, neck pain, back pain, PhD students, and daily spending > 9h on screen could significantly explain the model (P < 0.05).
 |
Table 3 Univariate Logistic Regression of Associated Factors for Severe DES and DED Symptoms |
 |
Table 4 Multivariate Logistic Regression for Predicting Severe DES and DED Symptoms |
In addition, we observed that an increase in DES scores also exponentially increases DED scores. The prevalence of DED symptoms was extremely high in participants with DES symptoms compared to asymptomatic DES participants (Figure 2A). Among students diagnosed with DES symptoms, 120 (26.5%) had mild to moderate DED symptoms, and 37 (8.2%) had severe DED symptoms. In contrast, in those with asymptomatic DES, only 38 (8.4%) and 4 (0.9%) had mild to moderate and severe DED symptoms, respectively (P < 0.000). Thus, asymptomatic, mild, moderate, and severe DES symptoms were respectively equivalent to the mean DED of 2.97 ± 3.22, 6.71 ± 3.28, 10.45 ± 3.81, and 16.75 ± 2.49 (Figure 2B). Moreover, Pearson’s correlation analysis showed a strong and significant positive correlation (r = 0.695, P < 0.000) between DES and DED scores (Figure 2C). Furthermore, DES and DED scores showed a weak but significant correlation with age, distance from ED, screen hours for studying, and screen hours for entertainment (Table 5).
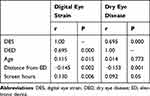 |
Table 5 Correlation (r) Between DES and DED, and Various Factors |
Discussion
Covid-19 is easily spread in university environments due to the challenges of maintaining social distancing policies among students. For this reason, education has shifted from physical teaching to online teaching, and therefore, the prevalence of DES and DED symptoms has significantly risen among university students.10 Participants in our study showed a high prevalence of DES and DED symptoms compared to the previous studies with a similar population group.10 In our analysis, CVS-Q results showed that 50% of students had higher DES symptoms, whereas DEQ-5 diagnosed DED symptoms in 44.1%. The present study aimed to analyze the correlation between DES and DED symptoms and examine the prevalence of severe dry eye disease among patients with digital eye strain.
As was expected, our results revealed that students with higher DES symptoms were exposed to developing severe DED symptoms. Moreover, the prevalence of DED symptoms was extremely high in participants with DES symptoms compared to asymptomatic DES participants. The most acute symptoms of DED (mean DEQ-5: 16.75 ± 2.49) were observed among students with severe DES. This may explain the strong positive correlation (r = 0.695, P < 0.000) observed between DES and DED mean scores. DES and DED symptoms usually coincide and may be difficult to differentiate, as both conditions share some common symptoms.10
The risk factors associated with higher DES and DED symptoms were age (≥ 35 years old), online studying, spending > 9h/day on screen, screen distance < 25 cm, wearing eyeglasses or contact lenses, and taking breaks after ≥ 2 hours of intensive ED use. However, being female, not practicing the 20-20-20 rule, and using the screen in the dull mode were risk factors for higher DES symptoms but not DED symptoms. In contrast, the TFOS DEWS II Epidemiology Report related DED symptoms to females.4 The same report reported a high prevalence of DED symptoms in older individuals. Similarly, our study found that DED symptoms predominated in older students (≥ 35 years old), though very low and insignificant correlations were observed between DED and age.
A study by Salinas-Toro et al (2019)12 found higher DED symptoms among the younger population than the older one. This difference may be attributed to the nature of their study sample, in which older participants spent fewer hours using ED than younger participants. Normally, the sensitivity of the cornea and conjunctiva decreases with age,15 which can explain a lesser eye discomfort in older individuals. However, our results evidenced that time spent on the ED screens has more influence on DED than age. Moreover, this can be justified by the higher mean scores and prevalence of DES and DED symptoms in our PhD participants because the intensity of their work requires them to stay on screens for many hours.
Furthermore, the distance from ED was significantly correlated with DES and DED symptoms. It was previously demonstrated that the optimum focus distance is 30–40 cm when reading or writing using a computer and 20–30 cm when using small ED such as telephones or tablets.16 The distance of 50–70 cm, which can correspond to the arm’s distance, was recommended by several studies as the ideal viewing distance to avoid the onset of ocular complaints.17,18 Habitually, most people tend to use smartphones closely to their eyes; however, studies reported severe eyestrain symptoms after closer viewing of telephones for at least one hour.19 For explanation, when the ED is close to the eyes, there will be an excess accommodation, resulting in the eye’s ciliary muscles overworking, contributing thus to the development of visual discomfort, eye fatigue, and headache.18 Moreover, constant focus on the ED screen decreases the blinking rates, leading to increased evaporation of tears, and thus inducing the eye’s redness, burning, and tiredness.17
The use of contact lenses exacerbates screen ocular discomfort.20 The same to our findings, severe DES and DED symptoms were found among contact lens wearers. This can be explained by the fact that wearing contact lenses decreases the frequency of blinking and lacrimal dynamics due to meibomian gland alteration, contributing thus to eye discomfort and ocular surface instability.21 Moreover, the comfort of the contact lens depends on lubrication in the eyes, which promotes the slip of the contact lens without resistance, otherwise, if the cornea becomes dry, the contact lens dehydrates and clings to the upper eyelid, and therefore the eye’s discomfort occurs,22 with a risk to develop serious corneal disorders such as keratitis.
Our multivariate logistic regression analysis revealed that none of the refractive errors was a predictor of the DES and DED symptoms. Similarly, a long-term follow-up study showed that there was no relationship between refractive disorders and extensive ED screen exposure symptoms.23 Nevertheless, although there is an onset of transient myopic shift after extended ED use, no persuasive evidence is present in the literature for the permanence of this myopia.24 In terms of the predicting factors associated with the DED condition, we found that conjunctivitis (OR = 0.22; P = 0.002), eye allergy (OR = 0.25; P = 0.008), glares (OR = 0.20; P = 0.000), tired eye (OR = 0.30; P = 0.000), neck pain (OR = 0.17; P = 0.001), back pain (OR = 0.13; P = 0.012), and daily spending > 9h on screen (OR = 0.05; P = 0.005) were predictors of DED symptoms.
In addition to ocular factors, physical and environmental factors, such as posture, screen brightness, glare, room temperature, and illumination, also play a significant role in the development of DES and DED symptoms by inducing corneal drying. Poor lighting results in the tiredness of the eyes; however, bright illumination produces transitory visual disturbance due to screen reflection and glare. Thus, appropriate lighting and proportional brightness must be maintained in the visual field to avoid ocular discomfort.25 Moreover, lower humidity or higher temperature accelerates the evaporation of tears and results in hyperosmolarity and ocular dryness.26 It has been shown that inappropriate ergonomic posture tenses the eye muscles and leads to visual and musculoskeletal discomfort. This could be explained by overactivity of the orbicularis oculi muscles and increased trapezius blood flow.27 It has been reported that ocular discomfort is more severe when the viewing angle is over 15°.2 This is explained by the fact that a greater viewing angle exposes a wider ocular surface to the air, thus increasing dryness and tear evaporation.
Strengths and Limitations
The primary limitation of this study was its cross-sectional setting. This was a DED symptoms study with self-assessed severity of dry eye symptoms. Further clinical testing for DED may have been very beneficial to patients who had severe DED symptoms. The questionnaires were distributed using the WeChat platform, which could influence selection bias as higher symptomatic patients are more prone to participate. Also, this study did not evaluate presbyopia status, although 9.5% of participants were around 40s. Other limitations included the difference in race, the disproportion of male/female ratio, unequally distributed age groups, and the uniquely student-based study sample; therefore, results may not represent the whole population. Moreover, despite our reasonable efforts to exclude all students with vision impairment pathologies, including those with refractive errors may have had an impact on the prevalence of visual symptoms even though they wore optical correction eyeglasses. There is a possibility that the spectacle corrections worn were outdated. We should have asked a question to know if the students had a recent ophthalmic check. Furthermore, as we did not clinically test our participants, we cannot fully ascertain their understanding of refractive errors. Lastly, psychosocial factors and psychological variables were not considered in the present study, even though previous studies have related severe DES and DED symptoms to stress, anxiety, depression, and somatic disorders such as headache and insomnia.28,29
However, this study contributes significantly to the literature despite the above limitations. We showed a rising concurrent correlation between DES and DED symptoms and first revealed that patients with higher digital eye strain symptoms are exposed to developing more severe dry eye disease. This may further lead clinicians to ameliorate their diagnosis and management approaches toward patients with DES and DED symptoms. Misdiagnosis or confounding these conditions can lead to inappropriate management, thus contributing to severe ocular symptoms. In addition, this study alarmed that although there is an increased prevalence of DES and DED symptoms among university students during this COVID-19 era, only 37.6% of students were aware of these conditions. It is evident that one cannot take preventive measures while unmindful of the risks. We recommended an urgent propagation of DES and DED symptoms awareness among university students. Appropriate patterns of using ED and preventive measures must be customized; otherwise, an epidemic of ocular surface instability may surge, which can affect future learning capability and labor productivity.
Recommendations
The risk factors of DED and advice to avoid them are provided below. Frequent voluntary blinking is urged to ensure proper tears dispersion and to prevent evaporative dry eye. Daily screen exposure must be limited as much as possible by avoiding unnecessary tasks. Teaching institutions are advised to consider resuming offline classes (Figure 3A); if not, it is necessary to maintain online classes duration under 6 hours per day (Figure 3B) and advocate the habit of frequent breaks (Figure 3C). For this, we promote the practice of the 20-20-20 rule (every 20 minutes, look at least 20 feet away for 20 seconds) (Figure 3D) and keep 25–40 cm or arm’s distance away from the ED screen (Figure 3E). Of note, some apps do exist to remind ED users to take a break at a fixed time interval. The viewing angle of 15° or lower is encouraged because this only exposes the inferior ocular surface to the air, and thus the dryness and tear evaporation decrease.
Furthermore, it is mandatory to establish appropriate physical and environmental outputs such as proper screen lighting, ergonomic posture, room temperature, humidity, and illumination. In addition, relieving symptoms by using artificial tears, blue light filters, antiglare, and protective glasses might help; however, this practice does not reduce ocular symptoms but masks them to improve ocular comfort. Finally, it is highly recommended to avoid wearing contact lenses (Figure 3F) while experiencing eyestrain symptoms; instead, switching to eyeglasses is more coherent if this is for optical correction purposes. Also, once there is persistent ocular discomfort due to excessive use of ED, it is necessary to consult an ophthalmic clinic for a proper diagnosis to prevent ocular casualties that may develop if they stay untreated.
Conclusion
The impact of COVID-19 will probably stay for many years. Special attention was paid to university students due to the growing extent of online classes, excessive use of electronic devices, and an increased prevalence of DES and DED symptoms. Our study showed that students with higher DES symptoms were exposed to developing severe DED symptoms. We believe that the prevalence of DED may be underestimated in the young population. It is necessary to consider it an emerging public health problem associated with lifestyle changes during the COVID-19 pandemic. Further studies and substantial clinical attention are needed to corroborate these hypotheses and better understand their impact on the ocular health of students. Universities should provide a comfortable study environment and educational training about proper ED practices to prevent these deleterious ocular surface conditions. Clinical studies to evaluate DED among university students are highly recommended for future research. In addition, concerned experts such as optometrists, ergonomists, and ophthalmologists must collaborate to design more practical and effective guidelines for the safer usage of digital screens.
Data Sharing Statement
The data are available from the corresponding author upon reasonable request.
Acknowledgments
The authors thank all participants for their participation.
Funding
This study was supported by grants from the National Key R&D Program of China (Grant Number: 2017YFA0105301); and the National Natural Science Foundation of China (Grant Number: 81770970).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Coronel-Ocampos J, Gómez J, Gómez A, Quiroga-Castañeda PP, Valladares-Garrido MJ. Computer visual syndrome in medical students from a private university in Paraguay: a Survey Study. Front Public Health. 2022;10:935405. doi:10.3389/fpubh.2022.935405
2. Kumar N, Sharma N. To determine the prevalence of computer vision syndrome among computer users: a descriptive study. EJMCM. 2020;7(10):3933–3938.
3. Sánchez-Brau M, Domenech-Amigot B, Brocal-Fernández F, Quesada-Rico JA, Seguí-Crespo M. Prevalence of computer vision syndrome and its relationship with ergonomic and individual factors in presbyopic VDT workers using progressive addition lenses. Int J Environ Res Public Health. 2020;17(3):1003. doi:10.3390/ijerph17031003
4. Stapleton F, Alves M, Bunya VY, et al. TFOS DEWS II Epidemiology Report. Ocul Surf. 2017;15(3):334–365. doi:10.1016/j.jtos.2017.05.003
5. Talens-Estarelles C, García-Marqués JV, Cervino A, García-Lázaro S. Use of digital displays and ocular surface alterations: a review. Ocul Surf. 2021;19:252–265. doi:10.1016/j.jtos.2020.10.001
6. Bahkir FA, Grandee SS. Impact of the COVID-19 lockdown on digital device-related ocular health. Indian J Ophthalmol. 2020;68(11):2378–2383. doi:10.4103/ijo.ijo_2306_20
7. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf. 2017;15(3):276–283. doi:10.1016/j.jtos.2017.05.008
8. Morthen MK, Magno MS, Utheim TP, et al. The vision-related burden of dry eye. Ocul Surf. 2022;23:207–215. doi:10.1016/j.jtos.2021.10.007
9. McDonald M, Patel DA, Keith MA, Snedecor SJ. Economic and humanistic burden of dry eye disease in Europe, North America, and Asia: a systematic literature review. Ocul Surf. 2016;14(2):144–167. doi:10.1016/j.jtos.2015.11.002
10. Cartes C, Segovia C, Salinas-Toro D, et al. Dry eye and visual display terminal-related symptoms among university students during the coronavirus disease pandemic. Ophthalmic Epidemiol. 2022;29(3):245–251. doi:10.1080/09286586.2021.1943457
11. Chalmers RL, Begley CG, Caffery B. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Cont Lens Anterior Eye. 2010;33(2):55–60. doi:10.1016/j.clae.2009.12.010
12. Salinas-Toro D, Cristian Cartes C, Segovia C, et al. High frequency of digital eye strain and dry eye disease in teleworkers during the coronavirus disease (2019) pandemic. Int J Occup Saf Ergon. 2021:1–6. doi:10.1080/10803548.2021.1936912
13. Seguí MM, Cabrero-García J, Crespo A, Verdú J, Ronda E. A reliable and valid questionnaire was developed to measure computer vision syndrome at the workplace. J Clin Epidemiol. 2015;68(6):662–673. doi:10.1016/j.jclinepi.2015.01.015
14. Cantó-Sancho N, Sánchez-Brau M, Ivorra-Soler B, Seguí-Crespo M. Computer vision syndrome prevalence according to individual and video display terminal exposure characteristics in Spanish university students. Int J Clin Pract. 2021;75(3):e13681. doi:10.1111/ijcp.13681
15. Barabino S. Is dry eye disease the same in young and old patients? A narrative review of the literature. BMC Ophthalmol. 2022;22(1):85. doi:10.1186/s12886-022-02269-2
16. Ichhpujani P, Singh RB, Foulsham W, Thakur S, Lamba AS. Visual implications of digital device usage in school children: a cross-sectional study. BMC Ophthalmol. 2019;19(1):76. doi:10.1186/s12886-019-1082-5
17. Rempel D, Willms K, Anshel J, Jaschinski W, Sheedy J. The effects of visual display distance on eye accommodation, head posture, and vision and neck symptoms. Hum Factors. 2007;49(5):830–838. doi:10.1518/001872007X230208
18. Wang J, Zeng P, Deng XW, et al. Eye habits affect the prevalence of asthenopia in patients with myopia. J Ophthalmol. 2022;2022:8669217. doi:10.1155/2022/8669217
19. Long J, Cheung R, Duong S, Paynter R, Asper L. Viewing distance and eyestrain symptoms with prolonged viewing of smartphones. Clin Exp Optom. 2017;100(2):133–137. doi:10.1111/cxo.12453
20. Tauste A, Ronda E, Molina MJ, Seguí M. Effect of contact lens use on computer vision syndrome. Ophthalmic Physiol Opt. 2016;36(2):112–119. doi:10.1111/opo.12275
21. Francés AT, Ronda-Pérez E, Crespo MS. Ocular and visual alterations in computer workers contact lens wearers: scoping review. Rev Esp Salud Publica. 2014;88(2):203–215. doi:10.4321/s1135-57272014000200004
22. Kojima T. Contact lens-associated dry eye disease: recent advances worldwide and in Japan. Invest Ophthalmol Vis Sci. 2018;59(14):DES102–DES108. doi:10.1167/iovs.17-23685
23. Keshavarz B, Novak AC, Hettinger LJ, Stoffregen TA, Campos JL. Passive restraint reduces visually induced motion sickness in older adults. J Exp Psychol Appl. 2017;23(1):85–99. doi:10.1037/xap0000107
24. Foreman J, Salim AT, Praveen A, et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit Health. 2021;3(12):e806–e818. doi:10.1016/S2589-7500(21)
25. Lin KH, Su CC, Chen YY, Chu PC. The effects of lighting problems on eye symptoms among cleanroom microscope workers. Int J Environ Res Public Health. 2019;16(1):101. doi:10.3390/ijerph16010101
26. Parihar JK, Jain VK, Chaturvedi P, Kaushik J, Jain G, Parihar AK. Computer and visual display terminals (VDT) vision syndrome (CVDTS). Med J Armed Forces India. 2016;72(3):270–276. doi:10.1016/j.mjafi.2016.03.016
27. Mork R, Bruenech JR, Thorud HM. Effect of direct glare on orbicularis oculi and trapezius during computer reading. Optom Vis Sci. 2016;93(7):738–749. doi:10.1097/opx.0000000000000855
28. Dragano N, Lunau T. Technostress at work and mental health: concepts and research results. Curr Opin Psychiatry. 2020;33(4):407–413. doi:10.1097/YCO.0000000000000613
29. Hilty DM, Armstrong CM, Smout SA, et al. Findings and guidelines on provider technology, fatigue, and well-being: scoping review. J Med Internet Res. 2022;24(5):e34451. doi:10.2196/34451
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


