Back to Journals » Therapeutics and Clinical Risk Management » Volume 15
Comprehensive evaluation of Manikin-based airway training with second generation supraglottic airway devices
Authors Schmutz A, Bohn E, Spaeth J, Heinrich S
Received 15 November 2018
Accepted for publication 23 January 2019
Published 1 March 2019 Volume 2019:15 Pages 367—376
DOI https://doi.org/10.2147/TCRM.S194728
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Garry Walsh
Axel Schmutz, Erich Bohn, Johannes Spaeth, Sebastian Heinrich
Department of Anesthesiology and Critical Care, Medical Center, Faculty of Medicine, University of Freiburg, 79106 Freiburg, Germany
Background: Supraglottic airway devices (SADs) are an essential second line tool during difficult airway management after failed tracheal intubation. Particularly for such challenging situations the handling of an SAD requires sufficient training. We hypothesized that the feasibility of manikin-based airway management with second generation SADs depends on the type of manikin.
Methods: Two airway manikins (TruCorp AirSim® and Laerdal Resusci Anne® Airway Trainer™) were evaluated by 80 experienced anesthesia providers using 5 different second generation SADs (LMA® Supreme™ [LMA], Ambu® AuraGain™, i-gel®, KOO™-SGA and LTS-D™). The primary outcome of the study was feasibility of ventilation measured by assessment of the manikins’ lung distention. As secondary outcome measures, oropharyngeal leakage pressure (OLP), ease of gastric tube insertion the insertion time, position and subjective assessments were evaluated.
Results: Ventilation was feasible with all combinations of SAD and manikin. By contrast, an OLP exceeding 10 cm H2O could be reached with most of the SADs in the TruCorp but with the LTS-D only in the Laerdal manikin. Gastric tube insertion was successful in above 90% in the Laerdal vs 87% in the TruCorp manikin (P<0.009). Insertion times differed significantly between manikins. The SAD positions were better in the Laerdal manikin for LMA, Ambu, i-gel and LTS-D. Participant’s assessments were superior in the Laerdal manikin for LMA, Ambu, i-gel and KOO-SGA.
Conclusions: Ventilation is possible with all combinations. However, manikins are variable in their ability to adequately represent additional functions of second generation SADs. In order to achieve the best performance during training, the airway manikin should be chosen depending on the SAD in question.
Keywords: emergency airway management, supraglottic airway device, SAD, airway training manikin, failed intubation, treatment, LMA, intubation guide
Introduction
Supraglottic airway devices (SADs) have become of increasing importance in recent years. Apart from their frequent use during elective surgery, SADs have become an essential part of difficult airway algorithms. When tracheal intubation and face mask ventilation fail, a temporary insertion of an SAD can enable ventilation, thus protecting the patient from hypoxemia.1 Moreover, the current European Resuscitation Council Guidelines recommend SADs as the device of choice for airway management by health care providers without expertise in tracheal intubation.2,3 In the recent years second generation SADs have been introduced with claims that ventilation and airway protection are improved. Second generation SADs include a lumen for insertion of a gastric tube in order to prevent gastric insufflation and pulmonary aspiration.4 Furthermore, several second generation SADs can be used as a conduit to facilitate tracheal intubation.1,5,6
Regarding the safe handling of an SAD, frequent airway trainings on SADs are essential, particularly for staff with limited experience.7 Effective airway training requires suitable airway manikins; however, due to limited experience, it is not well known which airway manikin is best suited for training of a specific skill related to ventilation and advanced techniques on second generation SADs.8,9
The most important characteristic of an airway manikin is to enable an authentic response to the trainee’s ventilation efforts after the insertion of the device. In a straightforward approach the device’s fit to the manikin’s airway can be estimated by the possibility of positive pressure ventilation and visual inspection of the expansion of the artificial lungs. A more sophisticated method for determining the seal of a respiratory system and thus to prove the possibility for clinically sufficient ventilation, is the oropharyngeal leakage pressure (OLP) test. Secondary requirements on airway manikins include the ability of accurate positioning of SADs as a prerequisite for tracheal intubation and the ability to insert a gastric tube. Airway manikins intended for airway training with second generation SADs should provide as many of these capabilities as possible. We hypothesized that the feasibility of training of the specific skills the second generation SADs allow for depends on the type of manikin.
In order to evaluate the qualities of two airway manikins intended for use with SADs we performed a series of skill tests using different second generation SADs with each manikin. Eighty anesthesia providers volunteered for the study. They were asked to insert five different types of second generation SADs in both the TruCorp AirSim® and the Laerdal Resusci Anne® Airway Trainer™. The primary outcome measure of the study is the feasibility of ventilation depending on the manikin type and type of SAD. As secondary objectives, the manikins’ qualities were evaluated by means of the seal to the SAD using the OLP test, the feasibility to insert a gastric tube and the accuracy of the SADs position relatively to the manikins’ airways. Additionally the insertion times and participants’ subjective ratings and preferences were evaluated.
Material and methods
Study institution and ethics
The study was conducted at the Department of Anesthesiology and Critical Care Medicine, University Medical Center, Freiburg, Germany after approval of the Ethics Committee of Freiburg University (May 12, 2016, Approval Number 235/16).
Airway manikins and supraglottic airway devices
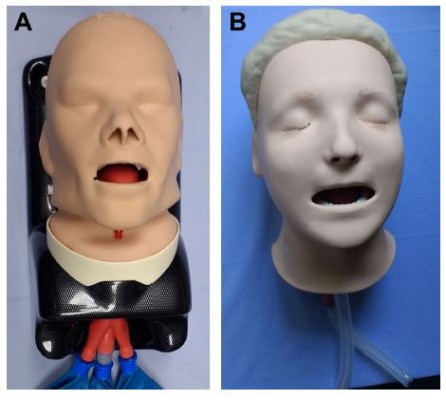
The two evaluated manikins were TruCorp AirSim® Advance (TruCorp, Belfast, UK) (TruCorp) and Laerdal Resusci Anne® Airway Trainer™ (Laerdal, Stavanger, Norway) (Laerdal) (Figure 1), both of comparable pricing. The TruCorp features an anatomically correct airway created from Digital Imaging and Communications in Medicine (DICOM) data. The Laerdal shows a complete anatomy of the vocal cords with elastic skin and tissue properties. According to the manufacturers’ recommendations, both airway manikins were dedicated for training with SADs and insertion of laryngeal masks. The chosen second generation SADs were LMA® Supreme™ (Teleflex, Athlone, Ireland), AuraGain™ (Ambu, Kopenhagen, Denmark), i-gel® (Intersurgical, Wokingham, UK), KOO™-SGA, a second generation prototype (KOO Medical Equipment, Tsuen Wan, China), and LTS-D™ (VBM GmbH, Sulz a.N. Germany) (Figure 2). Each device used was the model available in June 2016. In preliminary tests, we evaluated each SAD’s size to find the sizes that fitted best in both the included airway manikins. To that end, three anesthesiology consultants (blinded to the purpose of the study) were asked to use each SAD in each of the included airway manikins. The quality of fit between the SAD and airway manikins was evaluated by two independent experienced anesthesiologists with regard to the efficiency of ventilation, position, and ease of insertion of a gastric tube into the esophagus. Based on the experts’ ratings the LMA size 3, the AuraGain size 3, the i-gel size 5, the KOO-SGA size 4 and the LTS-D size four were included in the study. Oral cavities of the airway manikins were lubricated according to the manufacturers’ instruction manuals ahead of each individual test procedure.
  | Figure 1 Airway manikins. |
Participants
Eighty anesthesia residents, all staff of the Department of Anesthesia and Intensive Care of the University of Freiburg, gave written informed consent for voluntary participation. The inclusion criterion was a clinical experience of more than 100 SAD insertions. The participants’ individual demographic data, professional experience, and experience with airway management, in both numbers of SAD insertions and tracheal intubations, were recorded.
Study protocol
Every participant inserted each of the five SADs in both airway manikins. The sequence of airway manikins and SADs was randomised by drawing lots ahead of the study.
The study’s protocol is shown in Figure 3. First, participants were asked to insert the respective SAD. After insertion, the participants were asked to apply a standardized cuff pressure of 60 mbar with a cuff pressure gage (Covidien, Plymouth, MN, USA). Ventilation was achieved by connecting a self-inflating bag (Ambu SPUR II, Ambu, Copenhagen, Denmark) and confirmed by visual assessment of the manikins’ lungs’ distention. Following successful ventilation, the SAD’s position was determined by a bronchoscopic view of the hypopharynx. Thereafter, oropharyngeal leakage pressure was determined. Finally, participants were asked to insert a 14 Charrière gastric tube (Dahlhausen, Cologne, Germany) into the manikins’ esophagus through the additional lumen of their SAD. In all cases, the success of ventilation, the OLP, the evaluation of the position, and success of gastric tube insertion were assessed by the same individual, an experienced anesthesiologist.
  | Figure 3 Design and course of the study. |
Oropharyngeal leakage pressure (OLP) measurement
After insertion of the SAD the OLP was tested by occlusion of the breathing system and subsequent inflation of the closed system with a gas flow of 3 L min−1.10 Under continuous gas inflation the pressure in the breathing system was expected to exceed a threshold of 10 cm H2O, according to existing literature.11,12 If this objective has been reached we rated the OLP test passed and the ventilation to be clinically sufficient. If the threshold of 10 cm H2O could not be reached, ie, the leakage of the breathing system exceeded 3 L min−1, the OLP was rated failed. The pressure was measured using a differential pressure sensor (PasCal PC 100, Hoffrichter, Schwerin, Germany). Pressure signals were visualized and recorded using Labview 7.1 software (National Instruments, Austin, TX, USA).
Insertion time measurement
The participants’ performances were video-recorded using a camera (LifeCam Studio, Microsoft™, Redmond, WA, USA) giving a complete top-down view of the test setup. Using these recordings, insertion time was assessed as time from hands on SAD until onset of manual ventilation.
Accuracy of position
The positions of the SADs were evaluated for accuracy using a flexible bronchoscope (Ambu® aScope™ 3, Ambu, Kopenhagen, Denmark) which was introduced into the SAD through the mask’s oropharyngeal aperture. The bronchoscopic view was recorded and scored according to Brimacombe and Berry13: only vocal cords seen (4), vocal cords plus posterior epiglottis seen (3), vocal cords plus anterior epiglottis seen (2), vocal cords not seen but adequate function (1) and vocal cords not seen and failure to function (0).
Success of gastric tube insertion
The positioning of the gastric tube was evaluated by direct visual inspection in the Laerdal manikin and by palpation in the TruCorp manikin.
Participants’ subjective ratings and preferences
After completion of the test protocol, participants were asked to rate the handling quality of each SAD depending on the airway manikin using a five-point Likert scale, ranging from excellent handling (5) to poor handling (1). Beyond that, the participants were asked to indicate their preferred SAD in use with the respective airway manikin.
Data processing and statistical analysis
Data were collected in an Excel™ (Microsoft, Redmond, WA, USA) sheet and transferred to SPSS™ (version 25; IBM Corp., Armonk, NY, USA) for statistical processing. Statistical testing included basic descriptive statistics, Student’s t-test, Mann–Whitney U-test and Wilcoxon signed-rank test to compare non-parametric data (participants’ subjective rating). Normal distribution of continuous variables was tested using the Kolmogorov–Smirnov Test.
Results
All of the 80 anesthesia providers gave written informed consent to the study’s purpose. The participants’ characteristics are shown in Table 1. Initial ventilation was feasible in all combinations of SADs and airway manikins. The results of the secondary outcome measures are given in Table 2.
  | Table 1 Participants’ characteristics |
  | Table 2 Main results of the study |
Oropharyngeal leakage pressure
The highest rate of OLP exceeding 10 cm H2O could be observed in the combination of LTS-D and the TruCorp manikin (79%). With the i-gel the OLP could not be reached in any of the two manikins. In the Laerdal manikin OLP did not exceed 10 cm H2O in use with LMA, Ambu, KOO and i-gel; only with the LTS-D did the OLP exceed the threshold of 10 cm H2O, but this was seen only in a few cases (6%).
Insertion time
Insertion time was significantly shorter in the Laerdal manikin for all (all P<0.02) but the LMA SAD (P=0.315).
Accuracy of positioning (Brimacombe score)
In all SADs, except for the LTS-D, the recorded Brimacombe score was significantly higher in the Laerdal manikin. For the LTS-D the Brimacombe score was significantly higher in the TruCorp manikin.
Success of gastric tube insertion
The rate of successful gastric tube positioning was heterogeneous in the TruCorp manikin (Figure 4). The lowest rate of success was found with the i-gel (45%) and the highest rate of success with the LTS-D (86%). By contrast, in the Laerdal manikin the participants showed a success rate exceeding 90%, regardless of the SAD used.
Participants’ subjective ratings and preferences
Participants rated handling of all SADs better in the Laerdal manikin than in the TruCorp manikin (Figure 5). The ratings given as median (25%–75% quartiles) are stated in Table 2. In both manikins Ambu was the preferred device (Figure 6).
  | Figure 6 Participants’ ratings on the preferred supraglottic airway device for each airway manikin. |
Discussion
The most important finding of our study is that ventilation is possible with all SADs, regardless of the manikin in use. However, we performed an oropharyngeal leakage pressure test to further evaluate the possibility of alveolar ventilation using an SAD with regard to clinical conditions. The oropharyngeal leakage pressure, a technical approach to evaluating the breathing system’s ability to be ventilated, gives the level of airway pressure which is considered necessary for clinically sufficient ventilation.14 In accordance with the existing literature, we chose this threshold at 10 cm H2O.11 This means a minimal positive inspiratory pressure of 10 cm H2O can be reached when accepting a leakage of 3 L min−1. Translating this method into clinical practice means that one can expect an inspiratory pressure equal to our OLP threshold to result in a tidal volume of 400 mL, assuming a compliance of the respiratory system under general anesthesia of 40 mL cm H2O−1 and linear conditions. Taking the OLP into account showed a more differentiated result regarding the favorable combinations of airway manikins and SADs. Clinically sufficient ventilation, estimated by the OLP, was possible in certain SADs only and depended on the type of airway manikin.
In the TruCorp AirSim Advance manikin, clinically sufficient ventilation could be achieved with all SADs except the i-gel. By contrast in the Laerdal Resusci Anne Airway Trainer manikin clinically sufficient ventilation could be reached with the LTS-D device only. We assume the overall better fit of the SADs in the TruCorp to be attributable to the more flexible material and apparently tighter hypopharynx in this type of manikin. The superior performance of the TruCorp manikin, however, could not be attributed to a better laryngeal position of the SADs. The Brimacombe scores were better in the Laerdal compared to the TruCorp manikin for all SADs except the LTS-D. Moreover, the overall easier to perform ventilation with the TruCorp manikin was not associated with a better subjective rating of the participants. They rated the SADs’ handling more convenient in the Laerdal manikin.
With the i-gel clinically sufficient ventilation, measured by means of the OLP, was possible in neither manikin. This was most likely due to the non-inflatable thermo-sensitive tightening system, unique in this type of SAD. However, our findings demonstrate that the insufficient ventilation with the i-gel does not negate the other aspects of training with this device. In accordance with previous studies evaluating SADs on airway manikins,15,16 we found the i-gel to be superior regarding ease of handling and time of insertion. Furthermore, the excellent performance of the i-gel in clinical and emergency settings is well documented.17–20
The evaluation of insertion of a gastric tube may gain importance during the training of additional capabilities of second generation SADs. Our results demonstrate that all combinations of SADs with the Laerdal manikin enabled an easy insertion of a gastric tube. Similar success rates could be found in studies evaluating the extended capabilities of second generation SADs in humans.21,22 In these studies, gastric tube insertion was found to be successful in more than 91% of all cases. Therefore, we think that the high success rates found for gastric tube insertion are not due to the artificial situation of training with an airway manikin. However, gastric tube insertion seems more difficult in the TruCorp manikin.
Regarding the times required from hands on SAD to onset of manual ventilation, the differences between the TruCorp and the Laerdal manikin were statistically significant in four of the five SADs. The time required for insertion may support the provider’s decision on a preferable type of SAD. However, with respect to the small differences ranging from 3 to 12 seconds in our study and the fact that times required for SAD insertion in manikins are poorly correlated to those found in anesthetized patients,23 we consider our findings regarding the insertion time to be of limited clinical relevance.
The main findings of our study demonstrate that the airway models’ suitability for training with second generation SADs depends on the task in question. The TruCorp AirSim Advance manikin’s strength lies in its ability to be reliably ventilated with most of the SADs, particularly with the LTS-D. The strength of the Laerdal Resusci Anne Airway Trainer manikin is the overall good acceptance by the providers. Neither of the manikins is suitable for training with the i-gel concerning the performance of positive pressure ventilation. Insertion of a gastric tube is possible in both types. The potential clinical implications of these results rest on the benefits an ideal airway model can have on the feasibility of training. The most important quality of a manikin is the ability to simulate the real-world conditions and thus to give the trainee an authentic feedback. Moreover a working connection of a manikin and an airway device may motivate the trainee toward an achievable goal. Likewise, a manikin’s limitations should be known in order to avoid frustration due to multiple unsuccessful attempts. Although there is only weak evidence in support of simulation-based technical skill training on patient safety,24 demonstrable benefits in select clinical outcomes have been shown.25,26 We therefore assume that the selection of a suitable airway manikin based on the knowledge of the respective pros and cons can improve the quality of training and thus the clinical performance of the provider and potentially the patient’s safety.
Limitations
Some of our measurements may be subjective and open to bias in terms of familiarity and preference. However, the regular airway training of our department’s staff uses other manikins than those included in our study. Moreover, our findings are in consensus with those of previous studies, including those by health care providers with different experience.27–29 Therefore, we do not feel that the experience of our participants biased the findings of our study to a relevant extent.
We used a TruCorp AirSim Advance Manikin ordered in 2016. We are not aware of modifications applied to the inlay of the manikin by the manufacturer since the evaluation by Silsby et al.8 Furthermore, other newly developed airway manikins are unknown to us. We have compared how both airway training manikins perform with each second generation SAD. This study does not claim equivalent findings in clinical patient care.
Conclusion
Our study proves the existence of favorable combinations of manikins and second generation SADs, with regard to airway training. We therefore suggest selecting an appropriate manikin depending on the SAD and the training task in question. If, however, the training comprises multiple SADs or tasks, the trainer should be aware of the limitations of the respective pairings. In the light of the increasing spectrum of available SAD types and associated functions, it appears desirable that the development of airway manikins keeps pace with this technical progress.
Abbreviations
SAD, supraglottic airway device; TruCorp, TruCorp AirSim® Advance airway manikin; Laerdal, Laerdal Resusci Anne® Airway Trainer™; LMA, LMA® Supreme™ supraglottic airway device; Ambu, AuraGain™ supraglottic airway device; i-gel, i-gel® Intersurgical supraglottic airway device; KOO, KOO™-SGA second generation prototype supraglottic airway device; LTS-D™, laryngeal tube supraglottic airway device; OLP, oropharyngeal leakage pressure.
Data sharing statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgment
Thanks to Daniel P Reynolds for language editing and proofreading the manuscript.
Author contributions
AS and JS developed the design of the study. AS and EB collected the data. SH supported the design of the study and gave advice for interpreting the results. SH performed the statistical analysis. SH and AS wrote the manuscript, JS revised the manuscript. All authors contributed substantially to this work and all of them revised and agreed to the final version of the manuscript with full access to all data. They all agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Disclosure
The authors report no conflicts of interest in this work.
References
Frerk C, Mitchell VS, Mcnarry AF, et al. Difficult airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827–848. | ||
Soar J, Nolan JP, Böttiger BW, et al. European Resuscitation Council Guidelines for resuscitation 2015: Section 3. Adult advanced life support. Resuscitation. 2015;95:100–147. | ||
Cook TM, Kelly FE. Time to abandon the “vintage” laryngeal mask airway and adopt second-generation supraglottic airway devices as first choice. Br J Anaesth. 2015;115(4):497–499. | ||
Länkimäki S, Alahuhta S, Silfvast T, Kurola J. Feasibility of LMA Supreme for airway management in unconscious patients by ALS paramedics. Scand J Trauma Resusc Emerg Med. 2015;23(1):24. | ||
Shimizu M, Yoshikawa N, Yagi Y, et al. Fiberoptic-guided tracheal intubation through the i-gel supraglottic airway. Masui. 2014;63:841–845. | ||
Landsdalen HE, Berge M, Kristensen F, Guttormsen AB, Søfteland E. Continuous ventilation during intubation through a supraglottic airway device guided by fiberoptic bronchoscopy: a observational assessment. Acta Anaesthesiol Scand. 2017;61(1):23–30. | ||
Davis D. Paramedic intubation. Scand J Trauma Resusc Emerg Med. 2014;22(S1):A2. | ||
Silsby J, Jordan G, Bayley G, Cook TM. Evaluation of four airway training manikins as simulators for inserting the LMA Classic*. Anaesthesia. 2006;61(6):576–579. | ||
Cook TM, Green C, Mcgrath J, Srivastava R. Evaluation of four airway training manikins as patient simulators for the insertion of single use laryngeal mask airways. Anaesthesia. 2007;62(7):713–718. | ||
Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999;82(2):286–287. | ||
Brimacombe J, Berry A, Brain AI. Optimal intracuff pressures with the laryngeal mask. Br J Anaesth. 1996;77(2):295–296. | ||
Futier E, Constantin J-M, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369(5):428–437. | ||
Brimacombe J, Berry A. A proposed fiber-optic scoring system to standardize the assessment of laryngeal mask airway position. Anesth Analg. 1993;76:457. | ||
Zhang L, Seet E, Mehta V, et al. Oropharyngeal leak pressure with the laryngeal mask airway Supreme™ at different intracuff pressures: a randomized controlled trial. Can J Anesth/J Can Anesth. 2011;58(7):624–629. | ||
An J, Nam SB, Lee JS, et al. Comparison of the i-gel and other supraglottic airways in adult manikin studies: systematic review and meta-analysis. Medicine. 2017;96(1):e5801. | ||
Lee DW, Kang MJ, Kim YH, et al. Performance of intubation with 4 different airway devices by unskilled rescuers: manikin study. Am J Emerg Med. 2015;33(5):691–696. | ||
Gatward JJ, Cook TM, Seller C, et al. Evaluation of the size 4 i-gel™ airway in one hundred non-paralysed patients*. Anaesthesia. 2008;63(10):1124–1130. | ||
Choi GJ, Kang H, Baek CW, Jung YH, Woo YC, Cha YJ. A systematic review and meta-analysis of the i-gel® vs laryngeal mask airway in children. Anaesthesia. 2014;69(11):1258–1265. | ||
Lai C-J, Liu C-M, Wu C-Y, Tsai F-F, Tseng P-H, Fan S-Z. I-Gel is a suitable alternative to endotracheal tubes in the laparoscopic pneumoperitoneum and Trendelenburg position. BMC Anesthesiol. 2017;17(1):3. | ||
Gabbott DA, Beringer R. The iGEL supraglottic airway: a potential role for resuscitation? Resuscitation. 2007;73(1):161–162. | ||
Shariffuddin Ii TWH, Tang E, Hashim N, Loh PS. Ambu® AuraGain™ versus LMA Supreme™ second Seal™: a randomised controlled trial comparing oropharyngeal leak pressures and gastric drain functionality in spontaneously breathing patients. Anaesth Intensive Care. 2017;45:244–250. | ||
Liew GH, Yu ED, Shah SS, Kothandan H. Comparison of the clinical performance of i-gel, LMA Supreme and LMA ProSeal in elective surgery. Singapore Med J. 2016;57(8):432–437. | ||
Misiak M, Osadziñska J, Jarosz J, Czapliñska M. Simulation vs clinical practice – airway management with the laryngeal tube (LT). Eur J Anaesthesiol. 2004;21(Supplement 32):71–285. | ||
Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306:978–988. | ||
Ma IW, Brindle ME, Ronksley PE, Lorenzetti DL, Sauve RS, Ghali WA. Use of simulation-based education to improve outcomes of central venous catheterization: a systematic review and meta-analysis. Acad Med. 2011;86(9):1137–1147. | ||
Vanderbilt AA, Grover AC, Pastis NJ, et al. Randomized controlled trials: a systematic review of laparoscopic surgery and simulation-based training. Glob J Health Sci. 2014;7(2):310–327. | ||
Kim MH, Lee JH, Choi YS, Park S, Shin S. Comparison of the laryngeal mask airway Supreme and the i-gel in paralysed elderly patients. Eur J Anaesthesiol. 2018;35(8):598–604. | ||
Gill RK, Tarat A, Pathak D, Dutta S. Comparative study of two laryngeal mask airways: proseal laryngeal mask airway and Supreme laryngeal mask airway in anesthetized paralyzed adults undergoing elective surgery. Anesth Essays Res. 2017;11(1):23–27. | ||
Moser B, Audigé L, Keller C, Brimacombe J, Gasteiger L, Bruppacher HR. A prospective, randomised trial of the Ambu AuraGain laryngeal mask versus the LMA protector airway in paralysed, anaesthetised adult men. Minerva Anestesiol. 2018;84(6):684–692. |
 © 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2019 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



