Back to Journals » Clinical Ophthalmology » Volume 16
Compliance with Lid Hygiene in Patients with Meibomian Gland Dysfunction
Authors Chuckpaiwong V, Nonpassopon M , Lekhanont K, Udomwong W, Phimpho P, Cheewaruangroj N
Received 10 February 2022
Accepted for publication 1 April 2022
Published 19 April 2022 Volume 2022:16 Pages 1173—1182
DOI https://doi.org/10.2147/OPTH.S360377
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Varintorn Chuckpaiwong, Manachai Nonpassopon, Kaevalin Lekhanont, Weerapat Udomwong, Prae Phimpho, Nontawat Cheewaruangroj
Department of Ophthalmology, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Bangkok, Thailand
Correspondence: Manachai Nonpassopon, Department of Ophthalmology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, Bangkok, Thailand, Tel +662-201-1560, Fax +662-201-1516, Email [email protected]
Purpose: To evaluate the level and predictor of compliance with lid hygiene of the patients with meibomian gland dysfunction (MGD) by a specially designed and validated questionnaire.
Patients and Methods: A cross-sectional, descriptive study was conducted among patients with symptomatic meibomian gland dysfunction visiting at Ramathibodi Hospital from April 2019 to December 2020. Dry eye symptom, fluorescein tear breakup time (TBUT), ocular surface staining, lid morphology, meibum quality, and meibum expressibility were evaluated. All patients were instructed to perform lid hygiene two times daily. Eight weeks after receiving the instruction, the patients were asked to complete a newly developed seven-item questionnaire to assess compliance. The associated factors limiting treatment adherence were evaluated. Proper statistical analyses were used to determine the relationships between compliance and non-compliance and a group of relevant baseline variables. P < 0.05 was considered to be statistically significant.
Results: A total of 77 patients were recruited into the study. Sixty-three patients (81.8%) were female. The mean age was 66.71 ± 8.17 years old (42– 87 years). Good compliance with lid hygiene was reported by 42 patients (54.6%). Patient demographic factors or the number of concurrent systemic or ophthalmic drugs were not significantly different between the compliance and non-compliance groups. Some clinical signs, including the higher scores of meibomian gland expressibility and moderate to severe ocular surface staining, were significantly positively associated with lid hygiene compliance (χ2 = 10.13, P = 0.001 and χ2 = 10.48, P = 0.001, respectively). A lack of time was the most notable reason for non-compliance.
Conclusion: Approximately half of the patients with symptomatic MGD had good compliance with lid hygiene by the specific questionnaire. Appropriate patient education and optimization methods of lid hygiene may promote patient compliance.
Keywords: lid hygiene, meibomian gland dysfunction, compliance, adherence
Introduction
Meibomian gland dysfunction (MGD) is a chronic, diffuse abnormality of the meibomian glands, commonly characterized by terminal duct obstruction and/or qualitative/quantitative changes in glandular secretion.1 It appears to be a frequent ophthalmic condition, particularly in Asians, with prevalence in the general population varying from 31% to 70% and is considered to be a major contributor of evaporative dry eye, which is the most common subtype of dry eye disease.1–4 Although several treatment modalities are available, lid hygiene, consisting of eyelid warming, massaging, and cleaning, is the cornerstone of MGD treatment.5 Lid hygiene has been shown to decrease dry eye symptoms, reestablish tear film stability, improve meibomian gland secretion, increase tear film lipid layer thickness, and reverse meibomian gland dropout.5,6 However, similar to long-term treatment adherence for other chronic asymptomatic conditions, the compliance with everyday lid hygiene could be a demanding task for many MGD patients.5 Multiple new treatment modalities, ie, the thermal pulsatile system or Lipiflow® (TearScience ®, Morrisville, NC), intense pulse light therapy(IPL), or Quantum Molecular Resonance-based electrotherapy (QMR-ET) might help improve treatment result and fixed this problem.7–10 There have been few studies primarily evaluating the compliance with lid hygiene in patients with MGD, despite the recognition of this issue in MGD treatment.6,11–14 Several methods have recently been utilized for the assessment of compliance, including indirect measures such as self-report, electronic drug monitoring, pill counts, and pharmacy refill records; and direct measures, including detection of drugs or drug metabolites in plasma and examination of the intended effect.15 As lid hygiene regimens do not involve medications, the assessment can only rely on self-report or examination of an intended effect. Nonetheless, the use of intended effects as the measure of lid hygiene compliance may not be appropriate because there might be a weak link between the prescribed regimen and the desired outcomes.16 Additionally, most MGD patients tend to receive combination therapy, and multiple factors could be related to the therapeutic results.5 Therefore, self-report obtained through a questionnaire, which is the most preferred strategy for assessing compliance behavior, has been mainly used in previous studies.6,11–14 However, there were no standardized questions, so either a follow-up single question or a telephone 1- or 2-item questionnaire was administered to determine patient compliance.11,13 Although single-item questionnaires have been found to be valid ways to analyze patient compliance,17 they still overestimate treatment compliance compared with multiple questions.15 A simple self-report form was applied in one study. The patients were instructed to sign the form every day if they performed the lid hygiene.13 Nonetheless, the possibility of having distrustful answers might be a major disadvantage.18 In another study investigating the efficacy of lid hygiene using a specialized commercial product, the compliance was evaluated via a product questionnaire at the follow-up visits.14 Nevertheless, details of the product questionnaire were unavailable in that study. This study aimed to assess levels and predictors of compliance with lid hygiene among patients with MGD in real life, using a specifically designed and validated seven-item questionnaire, and to identify reasons for non-compliance.
Materials and Methods
Study Design
This single-center cross-sectional study was conducted at the Department of Ophthalmology, Ramathibodi Hospital, Bangkok, Thailand, between April 2019 and December 2020. The study protocol and consent form were reviewed and approved by the Institutional Review Board/Ethics Committee of Faculty of Medicine Ramathibodi Hospital, Mahidol University (MURA2019/1200). The study adhered to the tenets of the Declaration of Helsinki. Written informed consent was obtained from all participants before enrollment.
Study Questionnaire
Based on the various tools used for measuring the patient’s adherence to prescribed medications,19,20 we developed a new seven-item questionnaire to assess lid hygiene compliance (Table 1). Eight weeks after receiving instructions of lid hygiene, a single independent interviewer (WU) assessed the real-life patient’s compliance. Before administering the questionnaire, the interviewer reiterated that all responses were completely anonymous and their treating ophthalmologist would not be able to access any information given to the interviewer. A blame-free environment was created as much as possible to make patients feel comfortable providing honest responses and revealing non-compliance. If any patients had specific concerns that the interviewer could not answer, they were encouraged to discuss these problems with their cornea specialist. Response choices were “yes” or “no”. Ideally, five questions (questions 2, 3, 5–7) must have been answered positively and 2 (question 1, 4) negatively to receive one score for each question. The total score was the sum of all the scores and ranged from 0 to 7, with scores of 7 reflecting high adherence, 6 or 5 reflecting medium adherence, and ≤4 reflecting low adherence. In this study, patients were considered well compliant when they had medium to high adherence to their lid hygiene (a score of 5–7). Patients with poor compliance (total scores of ≤4) were asked about the most crucial reason or factor limiting their adherence.
 |
Table 1 Seven-Item Questionnaire Lid Hygiene Compliance Scale |
The validity and reliability of the questionnaire were examined by the index of Item-Objective Congruence (IOC) and internal consistency methods using Cronbach’s Alpha Coefficient, respectively. Four cornea specialists were asked to judge each item whether it really measures the expected attribute to determine content validity. All items had the IOC greater than 0.5, indicating the qualified items. A pilot test was performed on 15 subjects to ensure comprehension of the questions, and there were no significant inconsistencies in test scores over different parts of the questionnaire. The Cronbach’s alpha values were above 0.75 (0.76–1.00), indicating the high reliability of the questionnaire.21 Therefore, this questionnaire was created and considered valid and reliable based on an index of item objective congruence from four specialists (>0.75) and a pilot of 15 subjects (Cronbach alpha, 0.83–1.00).
Study Population
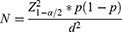
The amount of study population was calculated based on the sample size calculation formula.22
N = number of sample size, Alpha (α) = 0.05, Z = 1.959964
p = likely proportion of sample size, d = error
According to the formula, we assumed that the proportion of good compliance was 0.55 (reference from the previous study),12 and the acceptance of error was 0.11. A sample size of 78 patients was required. Then, the patients with symptomatic MGD were recruited from general ophthalmology outpatient and cornea clinics during the study period. Eligible participants were at least 18 years old, diagnosed with MGD stage 2 to 4 by a cornea specialist (KL, PP, NC, VC, MN), according to the 2011 Tear Film and Ocular Surface Society (TFOS) International Workshop on MGD.1 The subjects had not been trained in lid hygiene. Other inclusion criteria were an absence of active ocular surface inflammation, physical ability to follow the regimen, and willingness to attend a scheduled follow-up visit and undergo study assessments. Patients with MGD stage 1 were excluded from the study because they had no symptoms. Thus, they might not seek medical assistance and be less likely to adhere to their treatment.6 Patients with exacerbated inflammatory ocular surface were not suitable for lid hygiene until the inflammation was well controlled.5,6 Additional exclusion criteria comprised ocular surgeries or trauma within the previous six months, active ocular infection, other anatomical or functional eyelid or eyelash abnormalities such as mucosal keratinization or trichiasis, dermatologic disorders affecting eyelids, hypersensitivity to any composition of substances used in the regimen, monocular participants, and pregnancy, potential of becoming pregnant, or breastfeeding during the study.
Study Protocol
The patient information regarding demographics data, past ocular and medical history, and the number of systemic and topical medications were surveyed and collected. Education levels were classified into four classes; no education, primary education, secondary education/vocational certificate/vocational diploma, and bachelor’s degree/higher bachelor’s degree. Then, enrolled patients underwent a subjective evaluation of MGD-related symptoms,1,23,24 including ocular fatigue, foreign body sensation, dryness, discomfort, itching, photophobia, burning, fluctuating/blur vision, and soreness, to re-confirm that the patients still had symptomatic MGD before receiving instructions for lid hygiene. Subsequently, basic ocular surface examinations were carried out in the following manner: fluorescein tear breakup time (TBUT), ocular surface fluorescein staining (Oxford scale),25 and meibomian gland expression. Ocular surface staining was divided into two categories: grade 0 to 3; absent to mild staining and grade 3 to 5; moderate to severe staining. Meibomian gland secretion was assessed using firm digital pressure. Five glands in the center of the upper tarsus were expressed using a thumb to grade the meibum expressibility semi-quantitatively. A scale of 0 to 3 based on the number of glands expressible was used as follows: 0, all glands; 1, three to four glands; 2, one to two glands; 3, no glands.1 Meibum quality was evaluated on a scale of 0 to 3 as well: 0, clear; 1, cloudy; 2, cloudy with particulate matter (granular); 3, inspissated, like toothpaste.26
After the initial clinical evaluation, all patients were given a detailed instruction brochure and were instructed in lid hygiene by the same instructor team. The sequence of self-treatment regimen was as follows: (1) lid warming: warm the eyelids using either warm towel compresses/warm eye masks/a heated rice bag delivered approximately 40–42°C heat applied to the skin of closed eyelids or a commercial warm moist air device (Blephasteam®, Spectrum Thea Pharmaceuticals LTD, Macclesfield, UK) for 10 minutes; (2) lid massaging: apply traction on the lateral canthus to immobilize the upper and lower eyelids, followed by downward (for upper eyelids) or upward (for lower eyelids) mild compression of the eyelids with the finger of the opposite hand beginning at the nasal canthus and moving laterally toward the lateral canthus; (3) lid cleansing: scrub the eyelid margin with moistened cotton buds and dilute infant shampoo or commercial specifically formulated lid scrubs/wipes.5 Lid hygiene must be performed twice daily, in the morning and at night.
In addition to receiving instructions, patients were briefly told about the pathophysiology, the natural history, and the need for long-term treatment of MGD using simple and clear language. They are also reassured that they would notice an improvement in their symptoms if they complied with the instructions. Patients were allowed to continue their eye drops, including artificial tears as usual. Eight weeks after receiving complete instructions, a new seven-item questionnaire was used to assess the patient’s compliance.
Statistical Analysis
Statistical analyses were conducted using STATA version 16 (Stata Corp, College Station, TX, USA). The data from the worse eye, defined as having higher meiboscores of each patient, were used for analysis. For continuous data, normally distributed variables were presented as mean and standard deviation (SD); non-normally distributed variables were presented as median and range. Frequency and percentage were used for categorical data. Pearson chi-square (χ2) test, t-test, Fisher’s exact test, and Wilcoxon rank-sum test were used to evaluate the relationships between compliance and non-compliance and a group of relevant baseline variables. P < 0.05 was considered to be statistically significant. Factors that were significant at p < 0.10 in univariate analysis were considered for multivariate analysis. Multiple logistic regression was used to predict factors associated with compliance. P values <0.05 were considered statistically significant.
Results
Eighty-two eligible patients were enrolled in this study. Seventy-seven (94%) of 82 patients were completed with all inclusion criteria and included in the study. Two and three of the patients were excluded due to physical inability to do lid hygiene and active ocular surface inflammation, respectively. Most of the consecutively enrolled patients were female (63/77; 81.8%). The mean age was 66.7 ± 8.2 years (range, 42–87 years). Sixty-six patients (85.7%) had completed secondary school or higher (no education = 2, primary education = 9, secondary education/vocational certificate/vocational diploma = 21, and bachelor’s degree/higher bachelor’s degree = 45). Nearly half (32/77; 41.6%) were retired or unemployed. Almost all patients who had a job (45/77) worked in an office (Table 2). The majority of patients (81.8%) were taking at least one chronic systemic medication. The median number of systemic drugs used per patient was 4 (range, 0–16). The median number of ophthalmic prescriptions per patient was 2 (range, 1–5). A small proportion of patients (10.4%) had glaucoma requiring anti-glaucoma agents. Baseline ocular surface and meibomian gland characteristics are summarized in Table 2.
 |
Table 2 Patient Demographic and Baseline Characteristics of the Study Population (N = 77) |
Overall, 2, 40, and 35 patients (2.6%, 51.9%, 45.5%) had high adherence (score = 7), medium adherence (scores 5 to 6), and low adherence (scores ≤4) respectively. Four patients had a score of zero. The number of patients classified as being compliant (scores 5 to 7) was 42 patients (54.6%). By univariate analysis, there was no significant difference between compliance and non-compliance groups regarding age, sex, education, employment status, number of concurrent medications, systemic or ophthalmic drugs, history of glaucoma, fluorescein TBUT and meibum quality (Table 3). Only the ocular surface staining scores and meibomian gland expressibility were significantly positively associated with lid hygiene compliance (χ2 = 10.13, P = 0.001 and χ2 = 10.48, P = 0.001, respectively). However, after multivariate analysis, only the higher ocular surface staining scores were significantly positively associated with lid hygiene compliance (Odds ratio (OR) = 14.12, 95% confident interval (CI)=1.67–118.80, P < 0.05) (Table 3). Diverse reasons for poor compliance are presented in Table 4. A lack of time was the most notable reason for non-compliance in this study (18/35, 51.4%).
 |
Table 3 Univariate and Multivariate Analysis of Patient Demographic and Baseline Characteristics Comparing Between Good and Poor Compliance Measured by the Newly Developed Questionnaire |
 |
Table 4 Reasons of Poor Compliance with Lid Hygiene (N = 35) |
Discussion
Although lid hygiene is a routinely recommended first-line therapy for MGD, the variability among clinicians on what to use and the nature of instructions given to patients for lid hygiene could result in the lack of standardization of the technique and the uncertainty about patient compliance. This study aimed to investigate the compliance of the patients with MGD after they were given the same detailed instruction leaflet, verbally instructed and demonstrated the technique by the single instructor team to perform lid hygiene.
Overall, the compliance rate of lid hygiene in the current study was 54.6%. This rate was slightly lower than those of other prior studies (range, 55–67%).6,12,27 This might be explained by the differences in lid hygiene technique and regimen between studies along with various methods and criteria used to access the compliance. We proposed that using a specifically designed seven-item questionnaire in our study should improve the reliability of the compliance rate. More importantly, five of the seven questions had high sensitivity to determine good compliance; meanwhile, three had high specificity to define poor compliance (Table 5). As question 1 had 100% specificity, it might be a valid question when a clinician needs to detect patients with poor compliance correctly. Question 5 had a relatively high positive likelihood ratio and low negative likelihood ratio when compared with the others. Therefore, this question could be the most reasonable screening question to estimate patient compliance, especially when patient overload does not allow a clinician ample time to spend with patients in real-life practice.
 |
Table 5 Sensitivity, Specificity, Positive Likelihood Ratio, and Negative Likelihood Ratio of Each Questionnaire Item |
In addition, we found that demographic factors including age, sex, education, employment status, and the number of systemic or topical ophthalmic drugs did not influence therapy compliance. The literature review by Jin et al demonstrated that general demographic factors might not be good predictors of therapeutic compliance because some of them are related to patients’ various cultural, socioeconomic, and psychological backgrounds. Hence, they may not be genuinely independent factors affecting compliance.28 Previous studies showed that older age might be associated with poorer compliance in lid hygiene. Conversely, no significant relationships between the other demographic factors, including sex, race, ethnicity, and patient compliance were observed.12,27,29 Similar to the previous study,12 our study revealed that history of glaucoma did not appear to be a variable influencing the compliance. Although the presence of disease symptoms has generally been associated with better compliance,30,31 no consistent evidence demonstrated that patients with greater disease severity based on clinical signs would correlate with having better compliance.32–34 One previous study reported that the patients with lid margin disease who self-reported dry eye symptom were more likely to be compliant with lid hygiene than those who did not.12 In this study, we included only patients with symptomatic MGD. Hence, the compliance rate might be lowered if patients with asymptomatic MGD were also recruited into the study. Interestingly, we found that higher severity of some clinical signs of dry eye and MGD, including ocular surface staining and meibomian gland expressibility, were significantly positively associated with good lid hygiene compliance. It possibly implies that more severe clinical signs of MGD could lead to worse symptoms, contributing to better compliance. The results of a recent study support our hypothesis, showing that MGD patients with severe symptoms had worse meibomian gland characteristics, including meibum quality, meibomian gland expressibility, and meiboscore.30 Nonetheless, further investigations to assure this association are warranted.
In patients with poor lid hygiene compliance, we used opened-end questions to explore the main reasons for non-compliance. Broadly, the causes of poor compliance in this study were categorized into two themes: patient-centered factors and procedure-related factors (Table 4). Almost three-fourths of all reasons were related to patient-centered factors, whereas the rest were associated with procedure-related factors. Regarding patient-centered factors, a lack of time was the most common reason, followed by uncomprehending the disease and the necessity of the recommended treatment; too many concerns about other systemic conditions; and simply forgetting to do lid hygiene. To the best of our knowledge, only a few studies specifically mentioned the reasons for poor compliance with lid hygiene.12,35 Similarly, patient-centered factors, such as forgetfulness and carelessness, were the major causes of poor compliance in those studies. Thus, patient education to increase illness and consequence perceptions and emphasize the importance of proper treatment would enhance patient compliance to long-term lid hygiene.
As for procedure-related factors, complexity of the regimen, inconvenience of preparing things required for lid hygiene, and difficulty in remembering the steps of the regimen were the primary reasons. Theoretically, a straightforward and undemanding technique should provide better lid hygiene compliance. Therefore, the compliance rate would be improved if the lid hygiene protocol is modified appropriately to obtain the simplest effective regimen. Multiple eyelid-warming devices, ie, a steam-based system goggle: Blephasteam® (Spectrum Thea Pharmaceuticals LTD, Macclesfield, UK), heat-generating chemicals system eyemask: EyeGiene® (Eyedetec Medical Inc., Danville, CA, USA), or gel-bead heat delivery system eyemask: TheraPearl® (Bausch & Lomb Inc., New York, USA) might facilitate eyelid warming process and keep more consistent delivery of heat over the time when applying these devices on eyelid.36,37 One previous research demonstrated the favorable effect of Blephasteam over the conventional method in terms of the better improvement of symptoms.37 Future studies are required to identify the best ways to perform lid hygiene to optimize patient compliance and treatment outcomes.
This study has some limitations. First, the sample size was small and the study duration was short. This might overestimate the actual long-term compliance. Second, the disadvantages inherent to self-report measures of treatment adherence tend to overestimate compliance compared with other assessment approaches as well.38 However, the structured questionnaire measure, which is superior to in-person interviews in terms of their correspondence to objective adherence measures,38 was used in this study. It helped collect and analyze quantitative data, making the study more reliable and accurate. Third, the severity of dry eye symptoms related to MGD was not evaluated. Lastly, there was still a variation in the equipment used for lid warming and lid cleansing, potentially affecting the compliance.
Conclusion
The compliance rate assessed by a specifically designed seven-item questionnaire in this study was 54.6%. Patient-centered factors were significant causes of poor compliance with lid hygiene. Raising patient awareness of MGD and its impact and emphasizing the need to maintain lid hygiene and long-term benefits of therapy, along with appropriate regimen modification, could be strategies for improving patient compliance with lid hygiene.
Informed Consent
Written informed consent was obtained from all patients.
Funding
Supported by a research grant from the Faculty of Medicine, Ramathibodi hospital, Mahidol University.
Disclosure
The authors report no conflicts of interest for this work and have no proprietary or commercial interest in any materials discussed in this article.
References
1. Nichols KK, Foulks GN, Bron AJ, et al. The international workshop on meibomian gland dysfunction: executive summary. Invest Ophthalmol Vis Sci. 2011;52(4):1922–1929. doi:10.1167/iovs.10-6997a
2. Schaumberg DA, Nichols JJ, Papas EB, Tong L, Uchino M, Nichols KK. The international workshop on meibomian gland dysfunction: report of the subcommittee on the epidemiology of, and associated risk factors for, MGD. Invest Ophthalmol Vis Sci. 2011;52(4):1994–2005. doi:10.1167/iovs.10-6997e
3. Basak SK, Pal PP, Basak S, Bandyopadhyay A, Choudhury S, Sar S. Prevalence of dry eye diseases in hospital-based population in West Bengal, Eastern India. J Indian Med Assoc. 2012;110(11):789–794.
4. Lekhanont K, Rojanaporn D, Chuck RS, Vongthongsri A. Prevalence of dry eye in Bangkok, Thailand. Cornea. 2006;25(10):1162–1167. doi:10.1097/01.ico.0000244875.92879.1a
5. Geerling G, Tauber J, Baudouin C, et al. The international workshop on meibomian gland dysfunction: report of the subcommittee on management and treatment of meibomian gland dysfunction. Invest Ophthalmol Vis Sci. 2011;52(4):2050–2064. doi:10.1167/iovs.10-6997g
6. Yin Y, Gong L. Reversibility of gland dropout and significance of eyelid hygiene treatment in meibomian gland dysfunction. Cornea. 2017;36(3):332–337. doi:10.1097/ICO.0000000000001042
7. Villani E, Marelli L, Dellavalle A, Serafino M, Nucci P. Latest evidences on meibomian gland dysfunction diagnosis and management. Ocul Surf. 2020;18(4):871–892. doi:10.1016/j.jtos.2020.09.001
8. Arita R, Fukuoka S, Morishige N. Therapeutic efficacy of intense pulsed light in patients with refractory meibomian gland dysfunction. Ocul Surf. 2019;17(1):104–110. doi:10.1016/j.jtos.2018.11.004
9. Blackie CA, Coleman CA, Holland EJ. The sustained effect (12 months) of a single-dose vectored thermal pulsation procedure for meibomian gland dysfunction and evaporative dry eye. Clin Ophthalmol. 2016;10:1385–1396. doi:10.2147/OPTH.S109663
10. Ferrari G, Colucci A, Barbariga M, Ruggeri A, Rama P. High frequency electrotherapy for the treatment of meibomian gland dysfunction. Cornea. 2019;38(11):1424–1429. doi:10.1097/ICO.0000000000002063
11. Lee L, Garrett Q, Flanagan JL, Vaddavalli PK, Papas EB. Treatment practices and outcomes of meibomian gland dysfunction at a tertiary center in Southern India. Eye Contact Lens. 2018;44(Suppl 1):S138–s43. doi:10.1097/ICL.0000000000000356
12. Alghamdi YA, Camp A, Feuer W, Karp CL, Wellik S, Galor A. Compliance and subjective patient responses to eyelid hygiene. Eye Contact Lens. 2017;43(4):213–217. doi:10.1097/ICL.0000000000000258
13. Aryasit O, Uthairat Y, Singha P, Horatanaruang O. Efficacy of baby shampoo and commercial eyelid cleanser in patients with meibomian gland dysfunction: a randomized controlled trial. Medicine. 2020;99(19):e20155. doi:10.1097/MD.0000000000020155
14. Guillon M, Maissa C, Wong S. Symptomatic relief associated with eyelid hygiene in anterior blepharitis and MGD. Eye Contact Lens. 2012;38(5):306–312. doi:10.1097/ICL.0b013e3182658699
15. Berg KM, Arnsten JH. Practical and conceptual challenges in measuring antiretroviral adherence. J Acquir Immune Defic Syndr. 2006;43(Suppl1):S79–S87. doi:10.1097/01.qai.0000248337.97814.66
16. DiNicola DM. Practitioners, Patients, and Compliance with Medical Regimens: A Social Psychological Perspective. New York: Routledge; 2020.
17. Feldman BJ, Fredericksen RJ, Crane PK, et al. Evaluation of the single-item self-rating adherence scale for use in routine clinical care of people living with HIV. AIDS Behav. 2013;17(1):307–318. doi:10.1007/s10461-012-0326-7
18. Demetriou C, Özer B, Essau C. Self-report questionnaires. 2015.
19. Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens. 2008;10(5):348–354. doi:10.1111/j.1751-7176.2008.07572.x
20. Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (Mars) for the psychoses. Schizophr Res. 2000;42(3):241–247. doi:10.1016/S0920-9964(99)00130-9
21. Taber KS. The use of cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Educ. 2018;48(6):1273–1296. doi:10.1007/s11165-016-9602-2
22. Daniel EG, Wayne W. Biostatistics — a foundations for analysis in the health sciences. Wiley & Sons, New York—Chichester—Brisbane—Toronto—Singapore, 6th ed. 1995, 780 S., £58.—, ISBN 0–471–58852-0 (cloth). Biometrical J. 1995;37(6):744. doi:10.1002/bimj.4710370610
23. Arita R, Itoh K, Maeda S, et al. Proposed diagnostic criteria for obstructive meibomian gland dysfunction. Ophthalmology. 2009;116(11):2058–63.e1. doi:10.1016/j.ophtha.2009.04.037
24. Paugh JR, Kwan J, Christensen M, Nguyen AL, Senchyna M, Meadows D. Development of a meibomian gland dysfunction-specific symptom questionnaire. Eye Contact Lens. 2018;44(1):6–14. doi:10.1097/ICL.0000000000000294
25. Bron AJ, Evans VE, Smith JA. Grading of corneal and conjunctival staining in the context of other dry eye tests. Cornea. 2003;22(7):640–650. doi:10.1097/00003226-200310000-00008
26. Bron AJ, Benjamin L, Snibson GR. Meibomian gland disease. Classification and grading of lid changes. Eye. 1991;5(Pt 4):395–411. doi:10.1038/eye.1991.65
27. Kasetsuwan N, Suwajanakorn D, Tantipat C, Reinprayoon U. The efficacy between conventional lid hygiene and additional thermal pulsatile system in meibomian gland dysfunction patients treated with long-term anti-glaucoma medications in a randomized controlled trial. Clin Ophthalmol. 2020;14:2891–2902. doi:10.2147/OPTH.S259692
28. Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag. 2008;4(1):269–286. doi:10.2147/TCRM.S1458
29. Guillon M, Maissa C, Wong S. Eyelid margin modification associated with eyelid hygiene in anterior blepharitis and meibomian gland dysfunction. Eye Contact Lens. 2012;38(5):319–325. doi:10.1097/ICL.0b013e318268305a
30. Grant RW, Devita NG, Singer DE, Meigs JB. Polypharmacy and medication adherence in patients with type 2 diabetes. Diabetes Care. 2003;26(5):1408–1412. doi:10.2337/diacare.26.5.1408
31. Klauer T, Zettl UK. Compliance, adherence, and the treatment of multiple sclerosis. J Neurol. 2008;255(6):87–92. doi:10.1007/s00415-008-6016-8
32. Choudhry NK, Kronish IM, Vongpatanasin W, et al. Medication adherence and blood pressure control: a scientific statement from the American Heart Association. Hypertension. 2022;79(1):e1–e14. doi:10.1161/HYP.0000000000000203
33. Wild MR, Engleman HM, Douglas NJ, Espie CA. Can psychological factors help us to determine adherence to CPAP? A prospective study. Eur Respir J. 2004;24(3):461–465. doi:10.1183/09031936.04.00114603
34. Matthews D, Hingson R. Improving patient compliance: a guide for physicians. Med Clin North Am. 1977;61(4):879–889. doi:10.1016/S0025-7125(16)31304-9
35. Romero JM, Biser SA, Perry HD, et al. Conservative treatment of meibomian gland dysfunction. Eye Contact Lens. 2004;30(1):14–19. doi:10.1097/01.ICL.0000095229.01957.89
36. Olafsson J, Lai X, Landsend E, et al. TheraPearl Eye Mask and Blephasteam for the treatment of meibomian gland dysfunction: a randomized, comparative clinical trial. Sci Rep. 2021;11:22386. doi:10.1038/s41598-021-01899-8
37. Sim HS, Petznick A, Barbier S, et al. A randomized, controlled treatment trial of eyelid-warming therapies in meibomian gland dysfunction. Ophthalmol Ther. 2014;3(1–2):37–48. doi:10.1007/s40123-014-0025-8
38. Stirratt MJ, Dunbar-Jacob J, Crane HM, et al. Self-report measures of medication adherence behavior: recommendations on optimal use. Transl Behav Med. 2015;5(4):470–482. doi:10.1007/s13142-015-0315-2
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.